Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
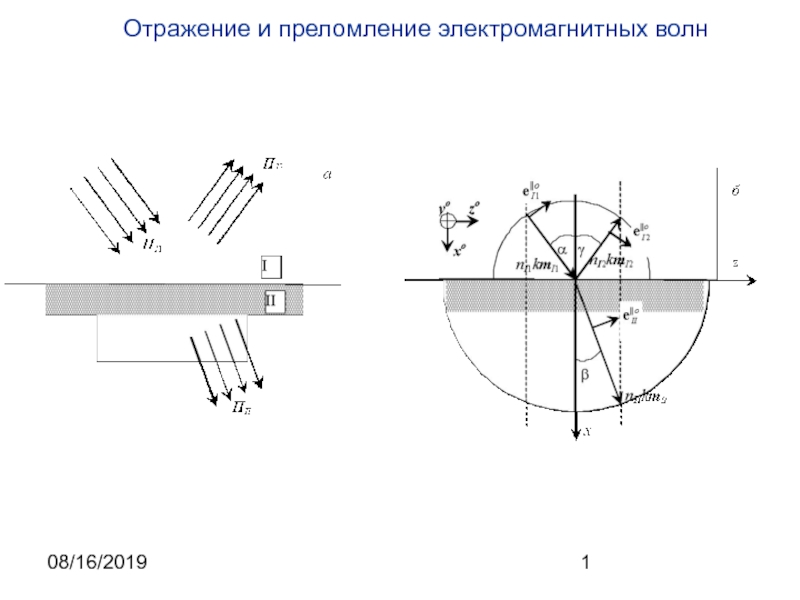
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Diseases of liver
Содержание
- 1. Diseases of liver
- 2. Слайд 2
- 3. Слайд 3
- 4. Слайд 4
- 5. Слайд 5
- 6. Clinical features of hepatic failureJaundiceHypoalbuminemiaCoagulopathyDICFetor hepaticusIncreased serum levels of hepatic enzymesGynecomastiaHepatic encephalopathyHepatorenal syndrome
- 7. Diseases of liverThe liver is vulnerable to
- 8. MORPHOLOGIC PATTERNS OF HEPATIC INJURYRegardless of cause, five general reactions may occur:Necrosis. Degeneration.Inflammation. Regeneration. Fibrosis.
- 9. Types of liver diseasesHepatosisHepatitisCirrhosisTumors of liver
- 10. Hepatoses
- 11. Hepatoses – group of diseases characterized
- 12. Massive progressive necrosis of liverEtiology: exogenous
- 13. Massive progressive necrosis of the liverMorphogenesis:Stage of
- 14. Слайд 14
- 15. Слайд 15
- 16. Massive hepatic necrosis with bleeding diathesis
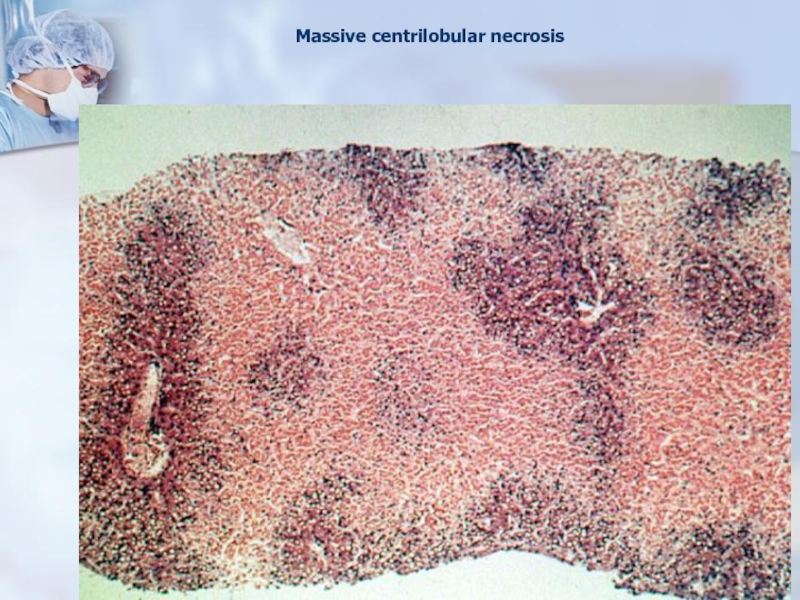
- 17. Massive centrilobular necrosis
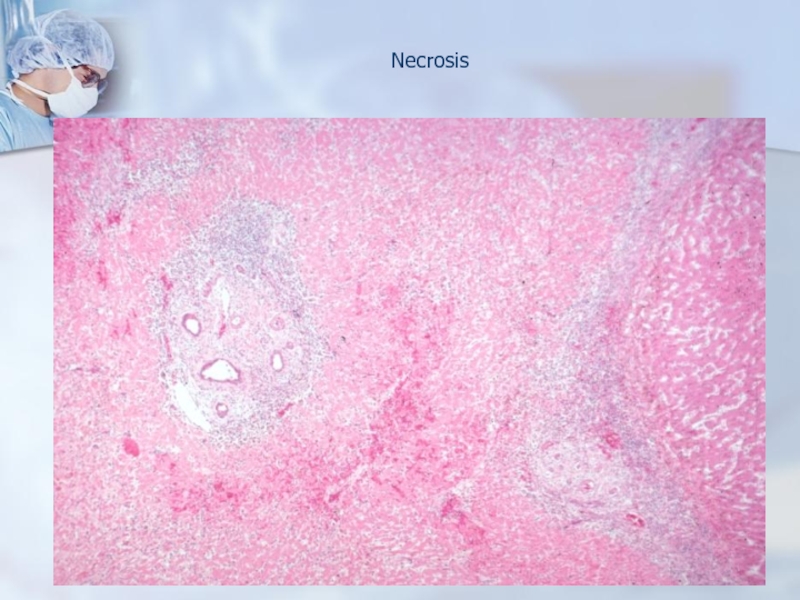
- 18. Necrosis
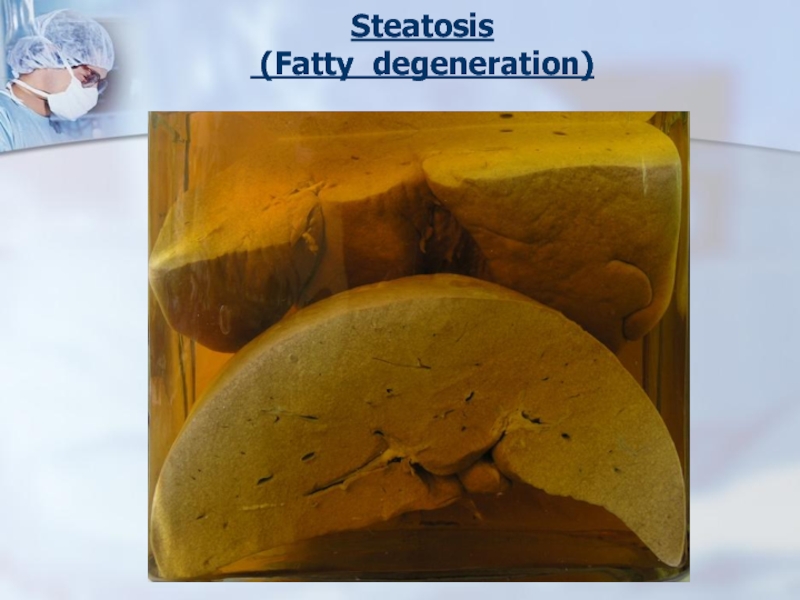
- 19. Steatosis (Fatty degeneration)
- 20. Fatty hepatosisEtiology: alcohol, medicines, metabolic disorders (diabetes
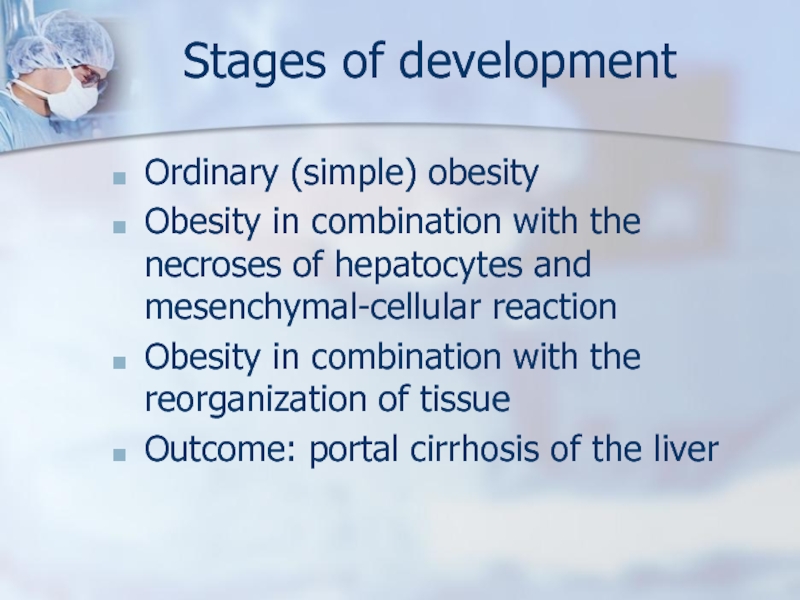
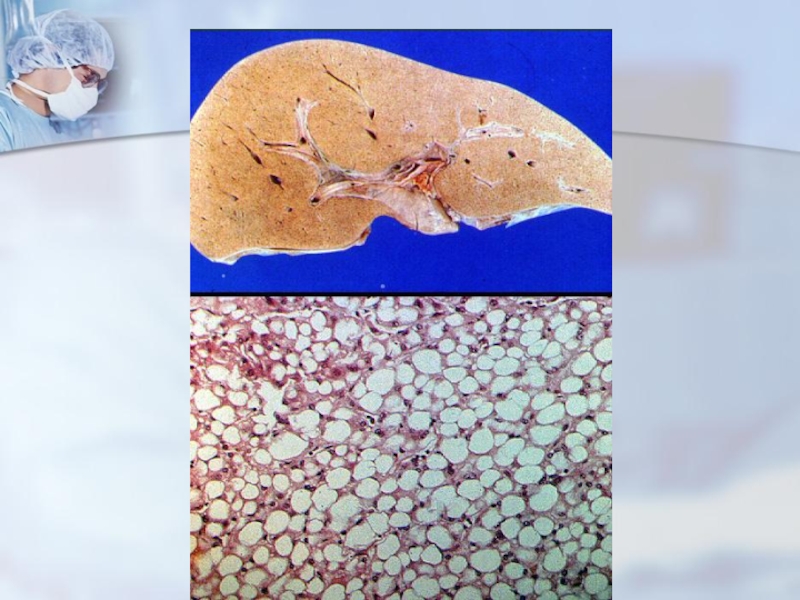
- 21. Stages of developmentOrdinary (simple) obesityObesity in combination
- 22. Слайд 22
- 23. Слайд 23
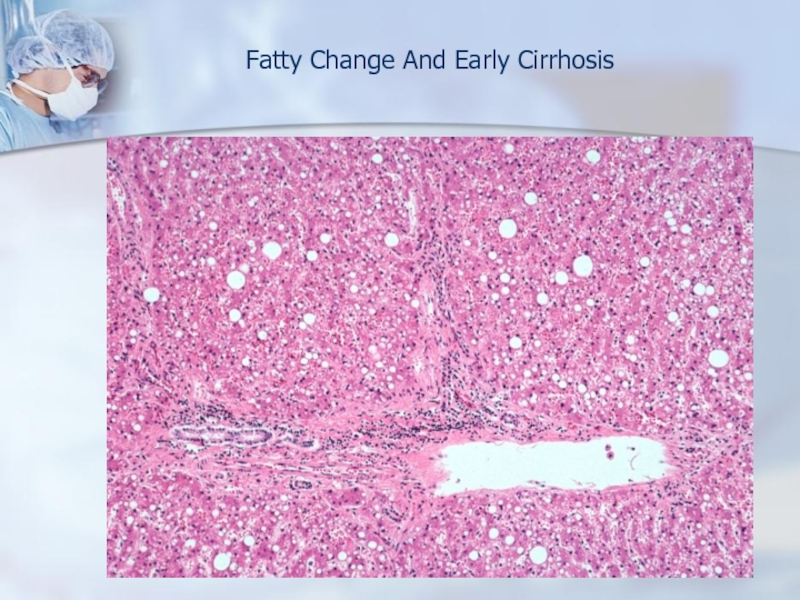
- 24. Fatty Change And Early Cirrhosis
- 25. Hepatitis
- 26. Viral hepatitisEtiology: Viruses hepatitis A,B,C,D…Viral hepatitis is
- 27. Hepatitis A Virus does not cause chronic
- 28. Transfusion, blood products, dialysis, needle-stick accidents among
- 29. Whatever the agent is, the disease is
- 30. Forms of viral hepatitisCyclic ictericNon-ictericCholestaticNecroticChronic (active and persistent)
- 31. Morphological signs Protein degenerationProliferation of Kupffer cellsLymphohistiocytic
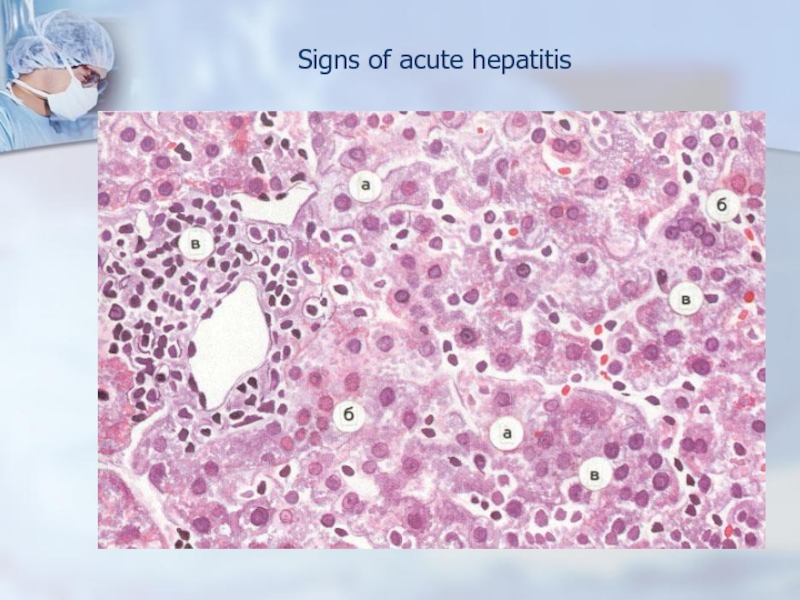
- 32. Signs of acute hepatitis
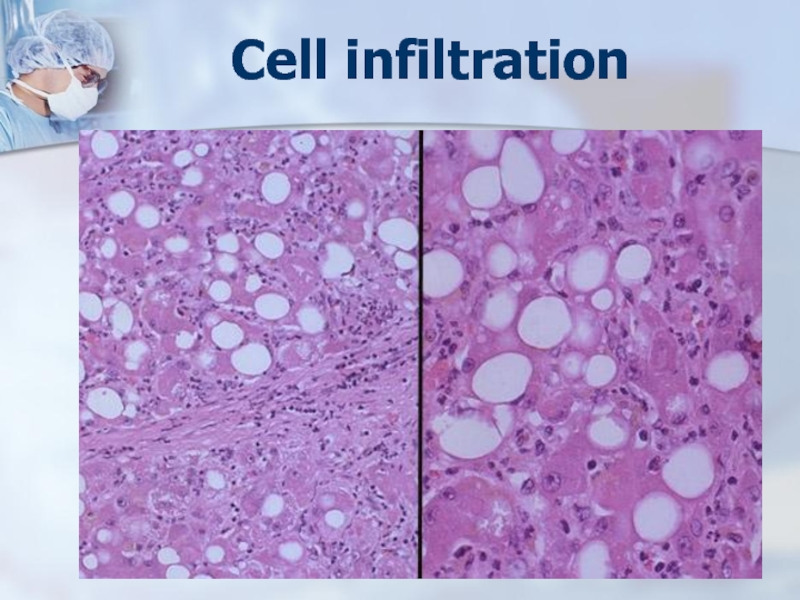
- 33. Cell infiltration
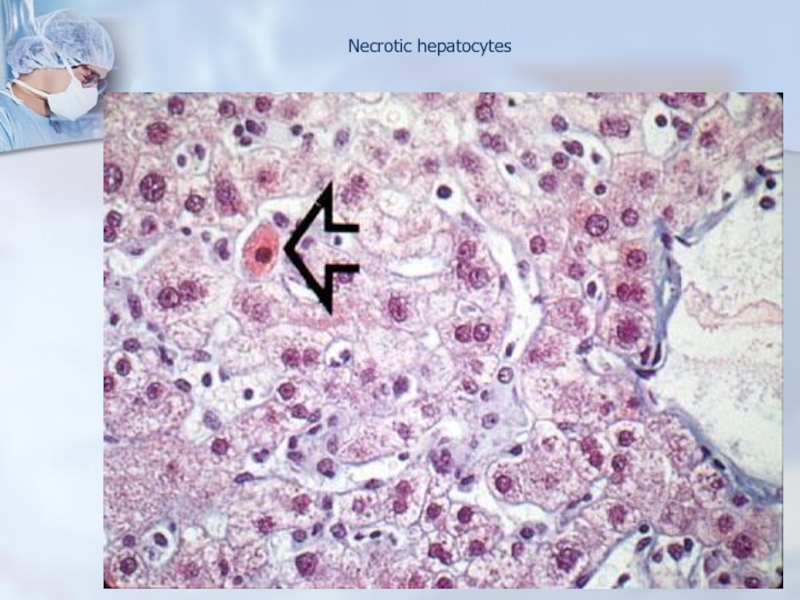
- 34. Necrotic hepatocytes
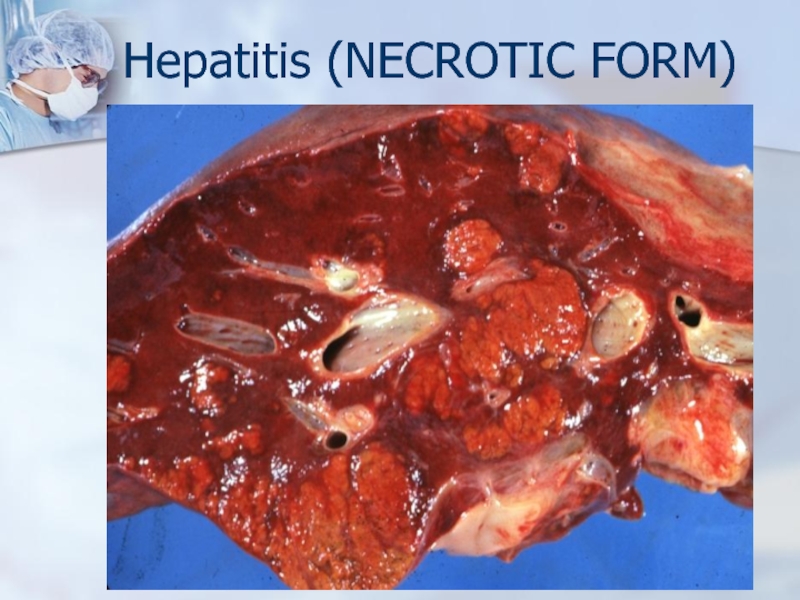
- 35. Hepatitis (NECROTIC FORM)
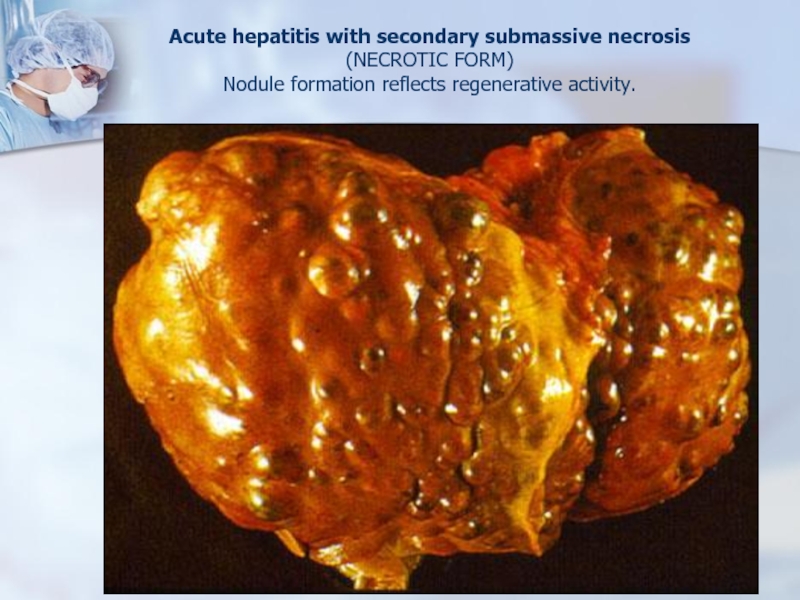
- 36. Acute hepatitis with secondary submassive necrosis (NECROTIC FORM) Nodule formation reflects regenerative activity.
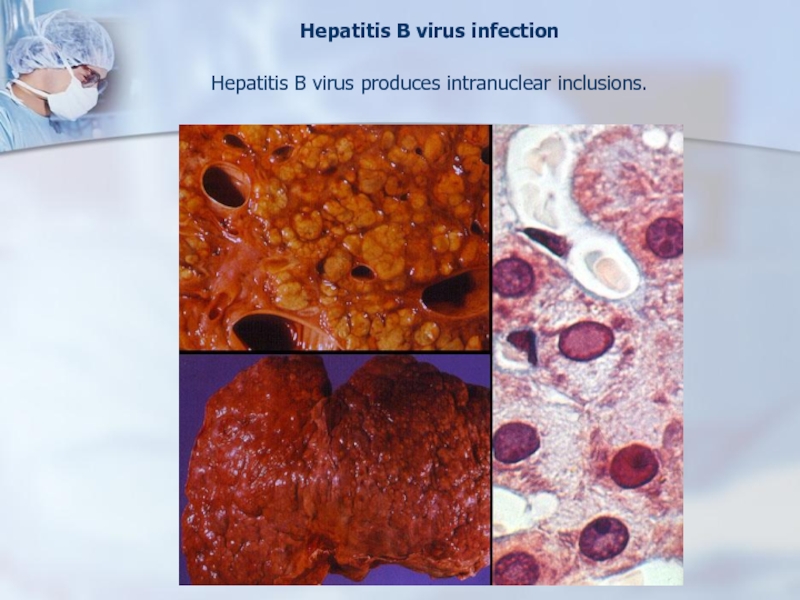
- 37. Hepatitis B virus infection Hepatitis B virus produces intranuclear inclusions.
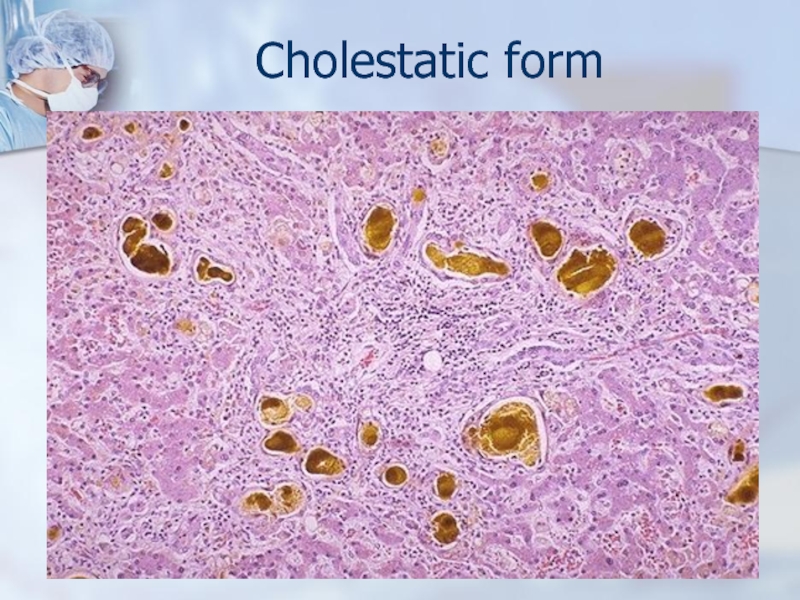
- 38. Cholestatic form
- 39. CHRONIC HEPATITISSymptomatic, biochemical or serologic evidence of
- 40. etiologic forms of hepatitis Hepatitis A Virus:
- 41. Since 1968, chronic hepatitis has been classified
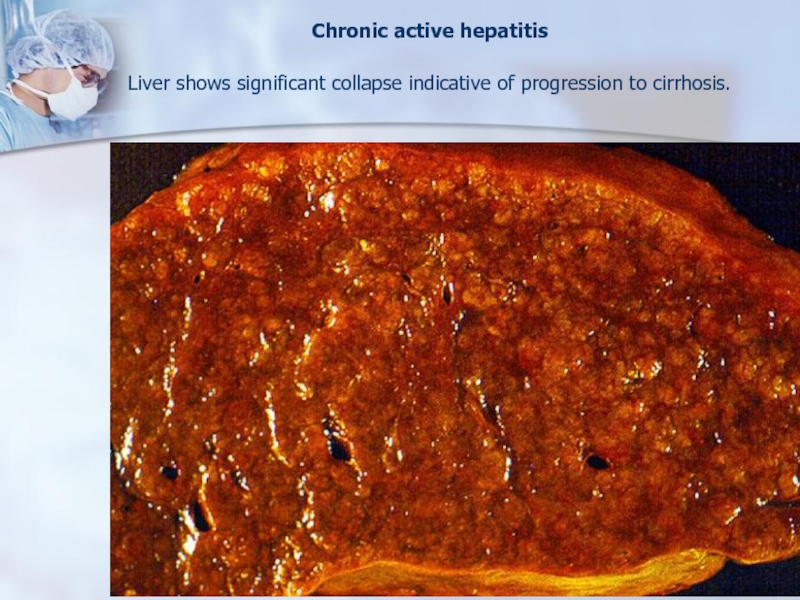
- 42. Chronic active hepatitis Liver shows significant collapse indicative of progression to cirrhosis.
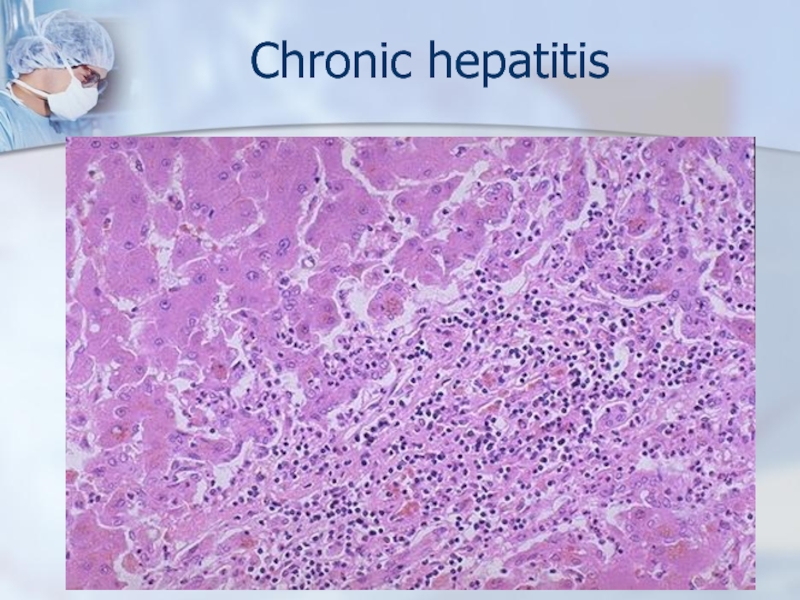
- 43. Chronic hepatitis
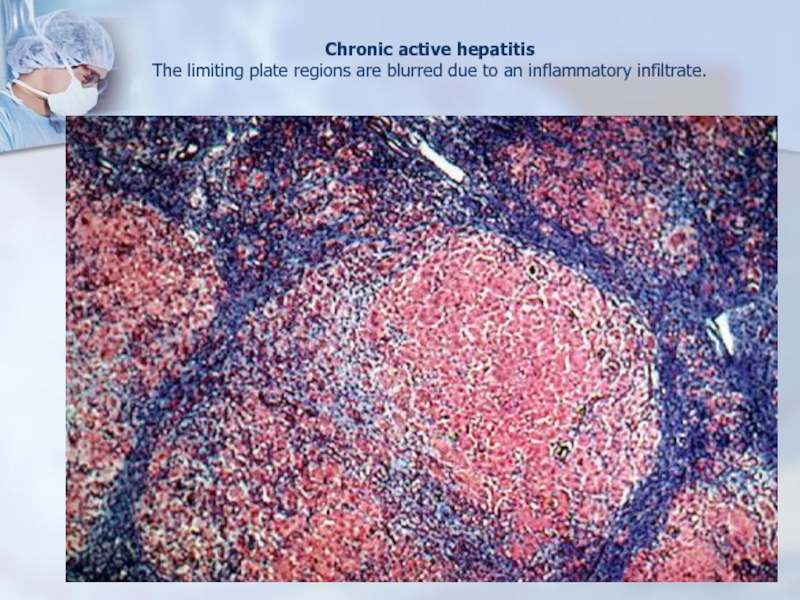
- 44. Chronic active hepatitis The limiting plate regions are blurred due to an inflammatory infiltrate.
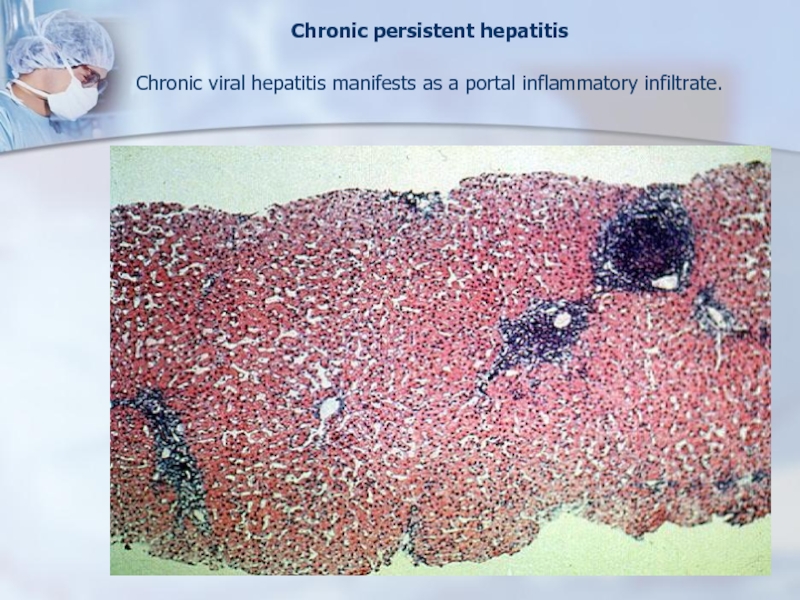
- 45. Chronic persistent hepatitis Chronic viral hepatitis manifests as a portal inflammatory infiltrate.
- 46. ALCOHOLIC LIVER DISEASE
- 47. Слайд 47
- 48. Alcoholic hepatitis
- 49. Markers of AHFatty dystrophy and necrosis of
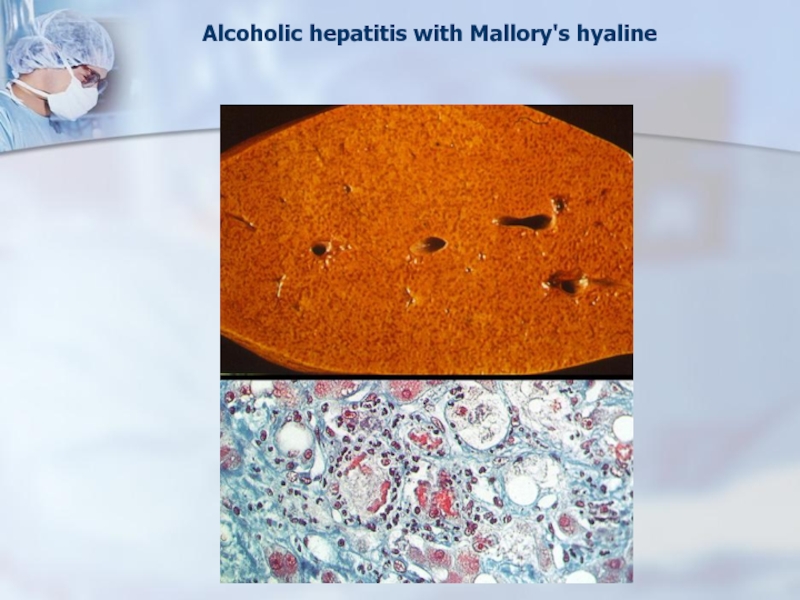
- 50. Alcoholic hepatitis with Mallory's hyaline
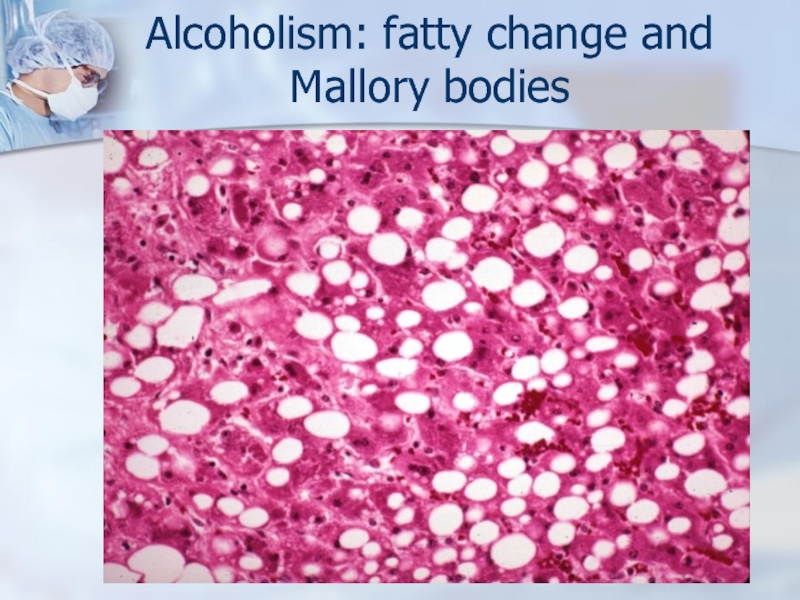
- 51. Alcoholism: fatty change and Mallory bodies
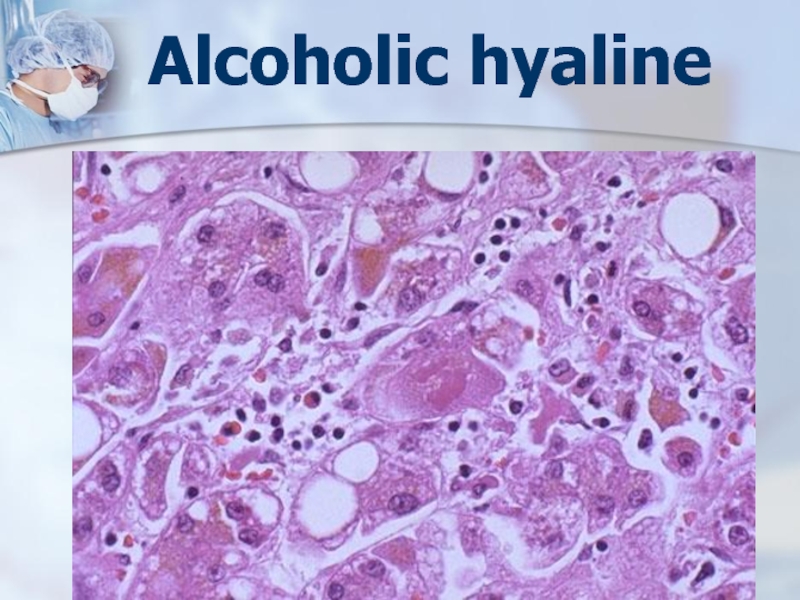
- 52. Alcoholic hyaline
- 53. Слайд 53
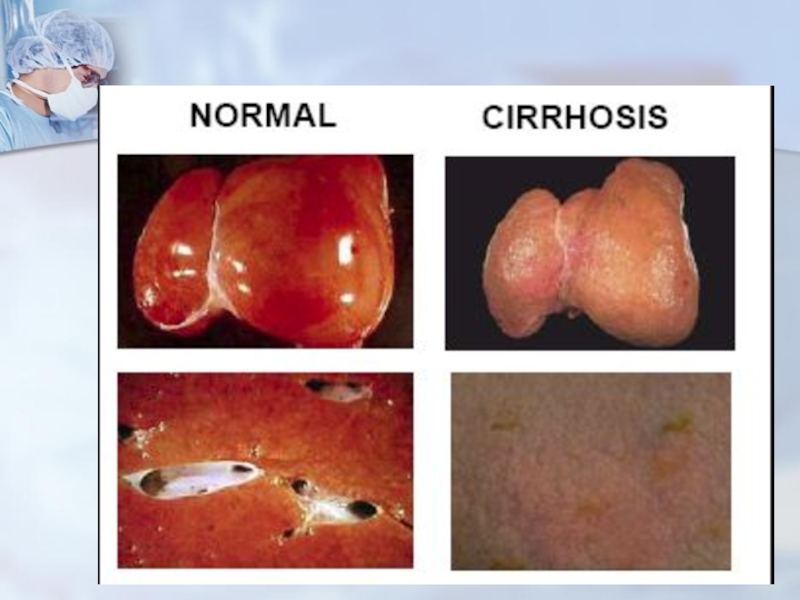
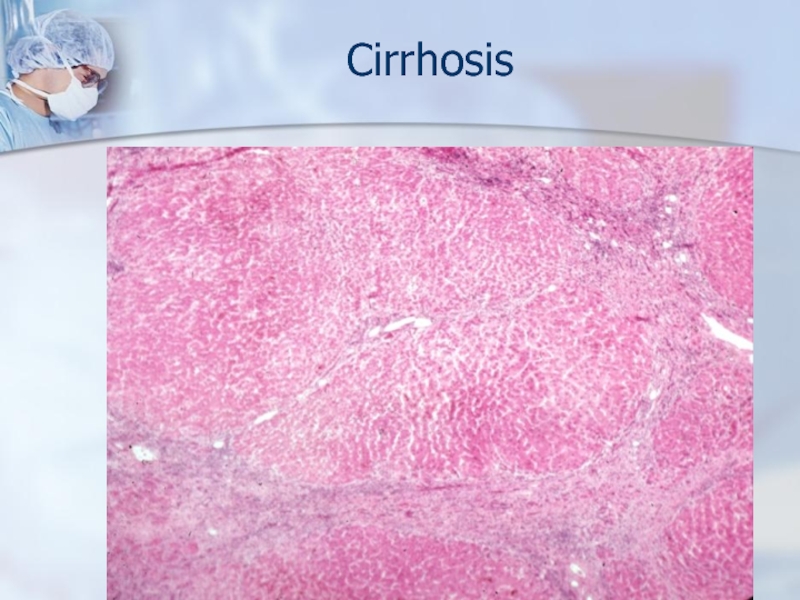
- 54. CirrhosisIs chronic disease of liver which is
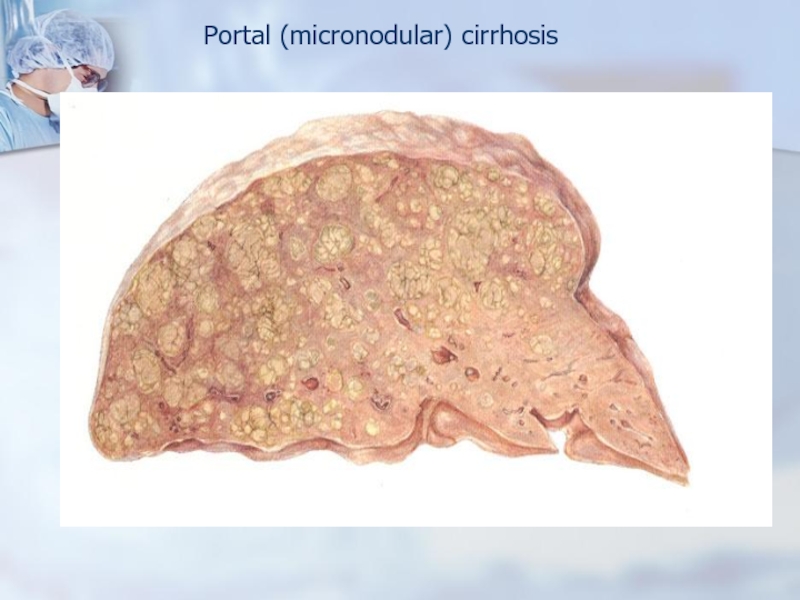
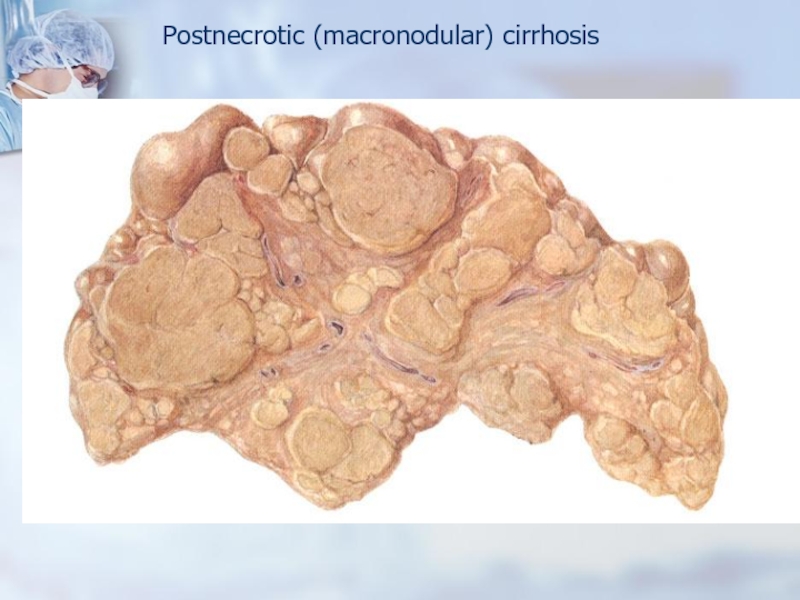
- 55. This end stage of liver disease is
- 56. Слайд 56
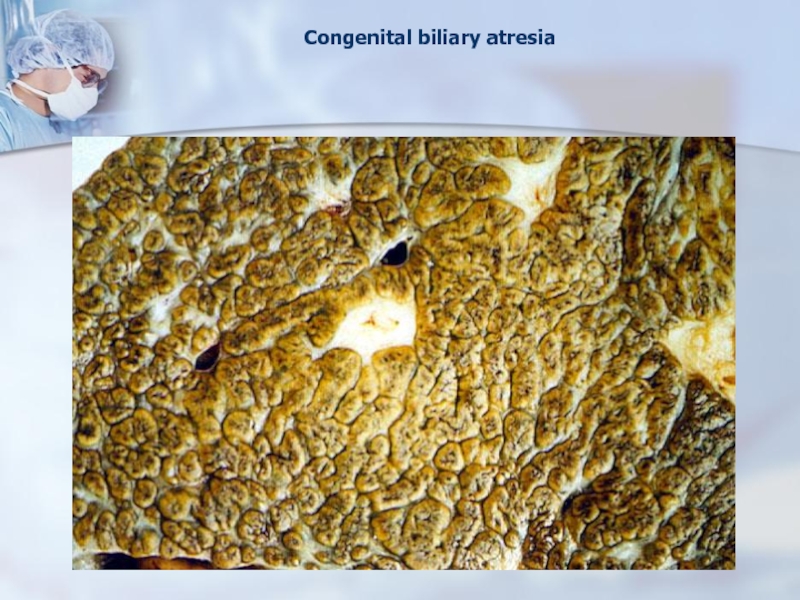
- 57. Congenital biliary atresia
- 58. Portal (micronodular) cirrhosis
- 59. Postnecrotic (macronodular) cirrhosis
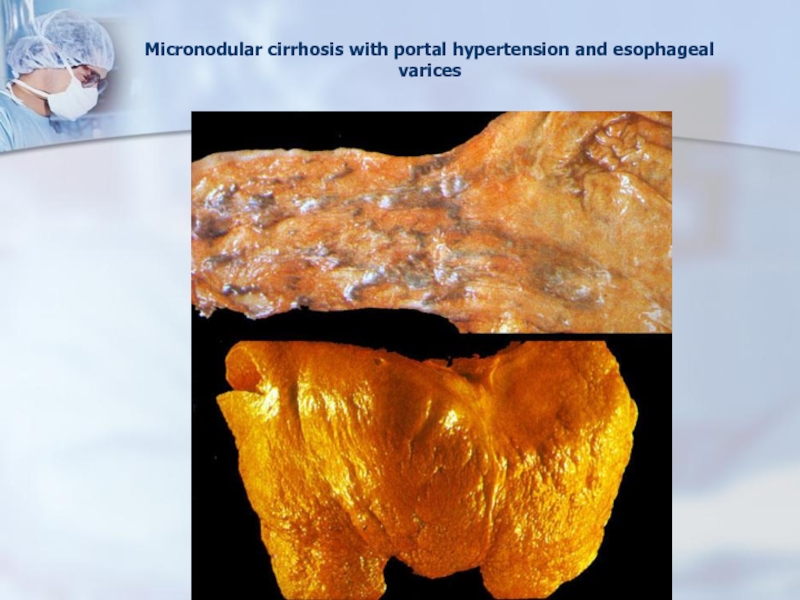
- 60. Micronodular cirrhosis with portal hypertension and esophageal varices
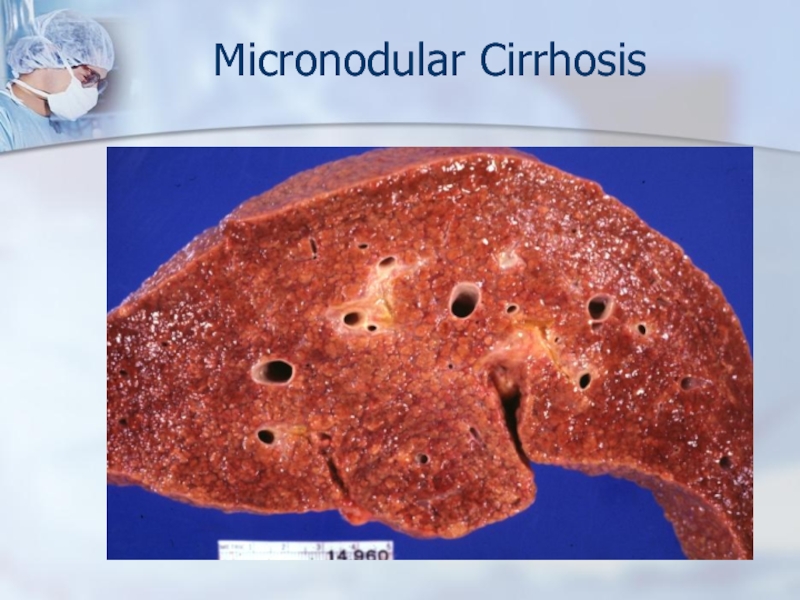
- 61. Micronodular Cirrhosis
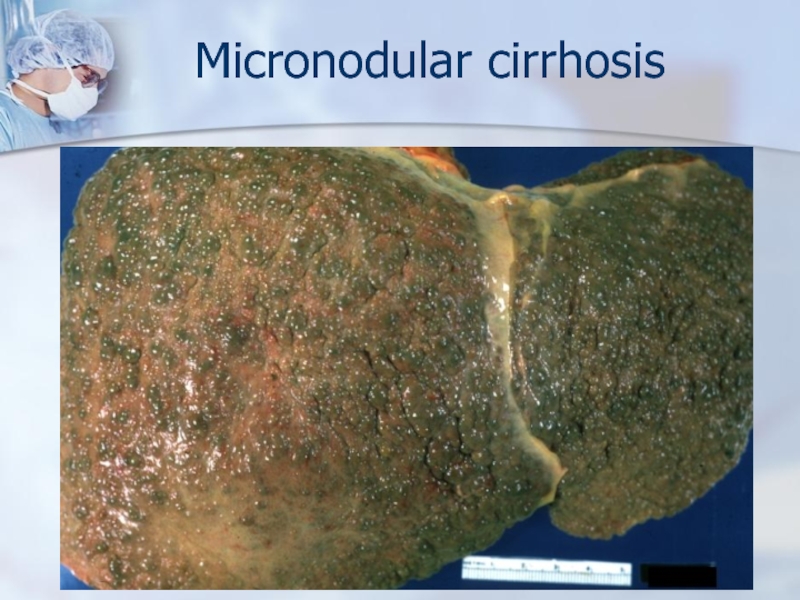
- 62. Micronodular cirrhosis
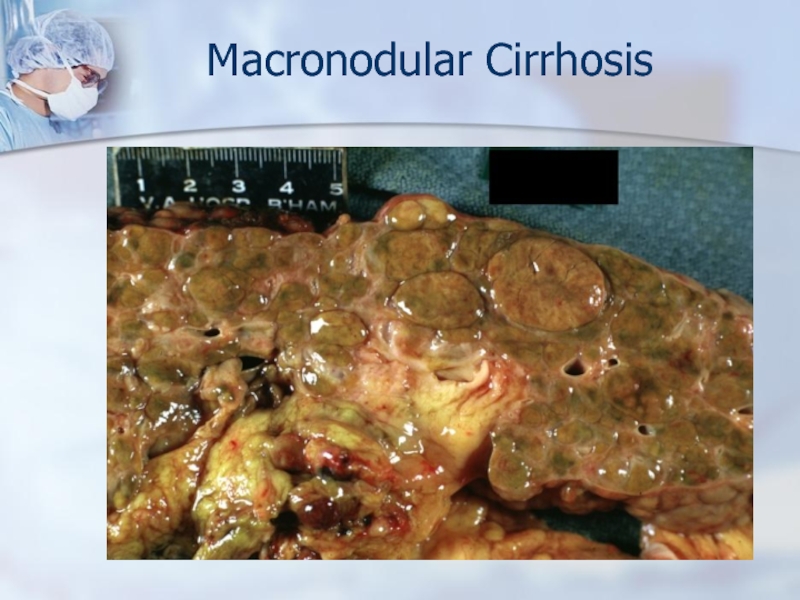
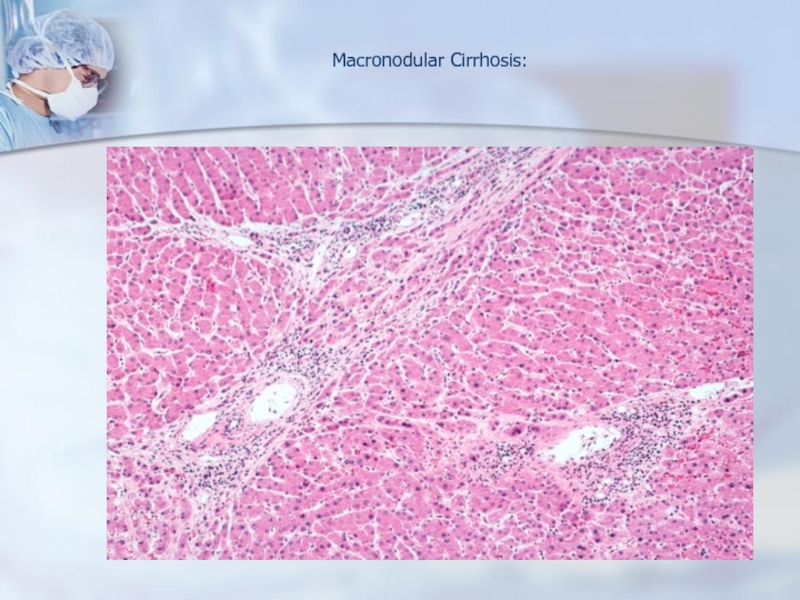
- 63. Macronodular Cirrhosis
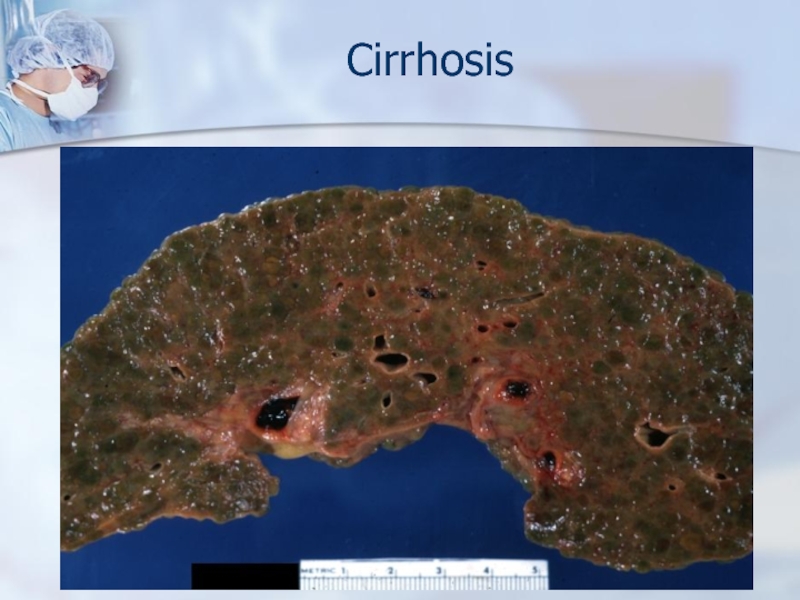
- 64. Cirrhosis
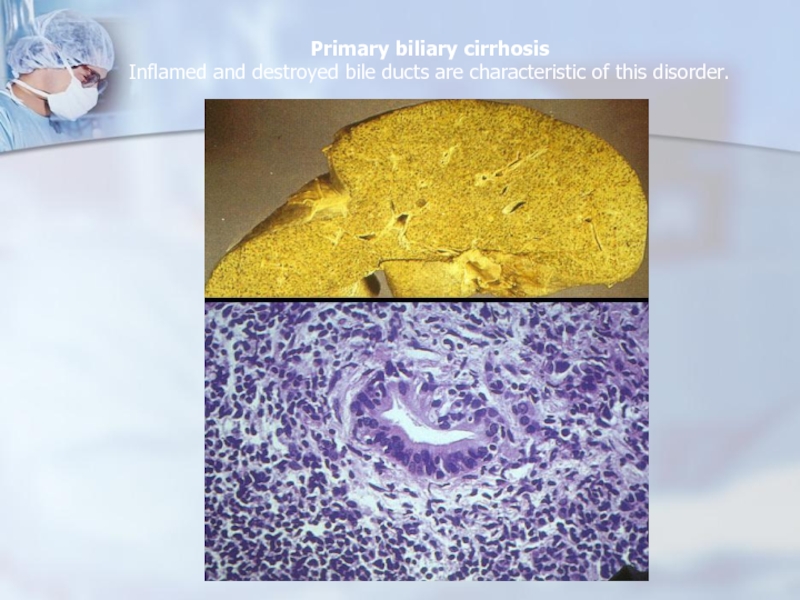
- 65. Primary biliary cirrhosis Inflamed and destroyed bile ducts are characteristic of this disorder.
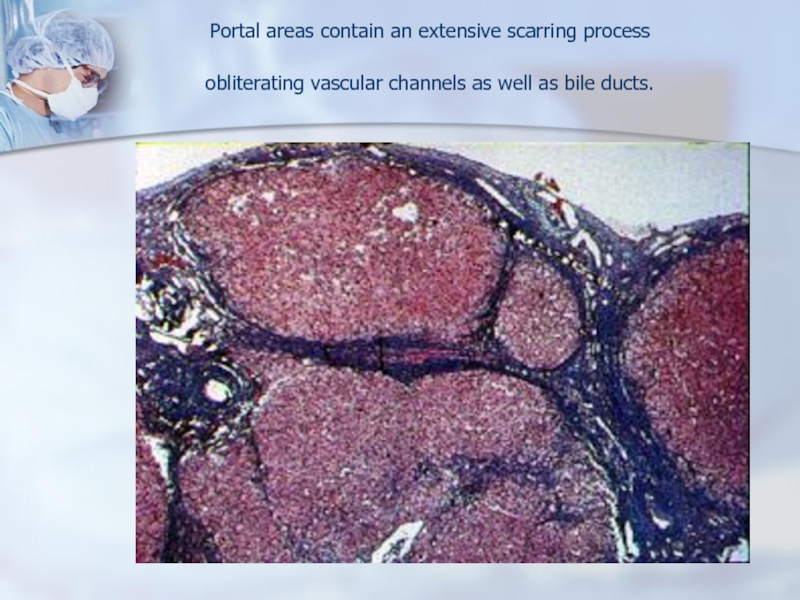
- 66. Portal areas contain an extensive scarring process obliterating vascular channels as well as bile ducts.
- 67. Several features should be understood:- The parenchymal
- 68. Several features should be understood:- Fibrosis, once
- 69. The ultimate mechanism of most cirrhotic
- 70. The four major clinical consequences are :1)
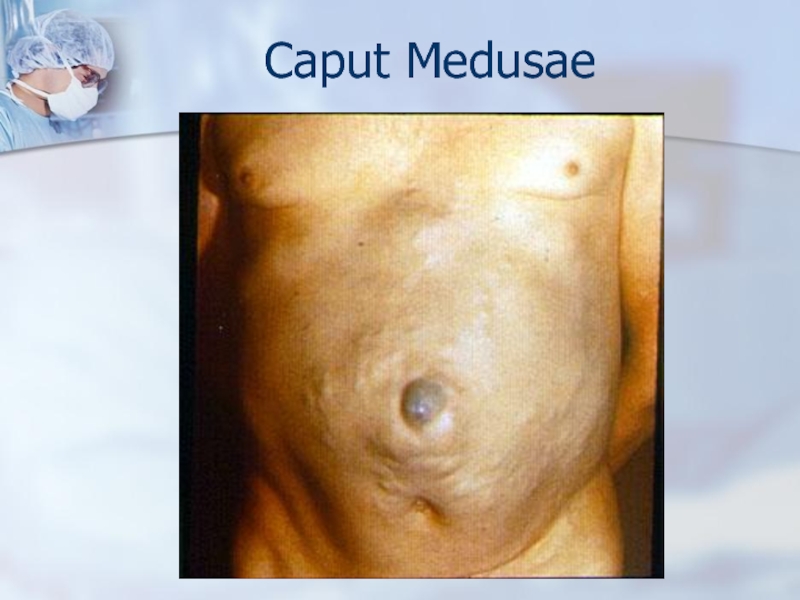
- 71. Caput Medusae
- 72. Esophageal varices
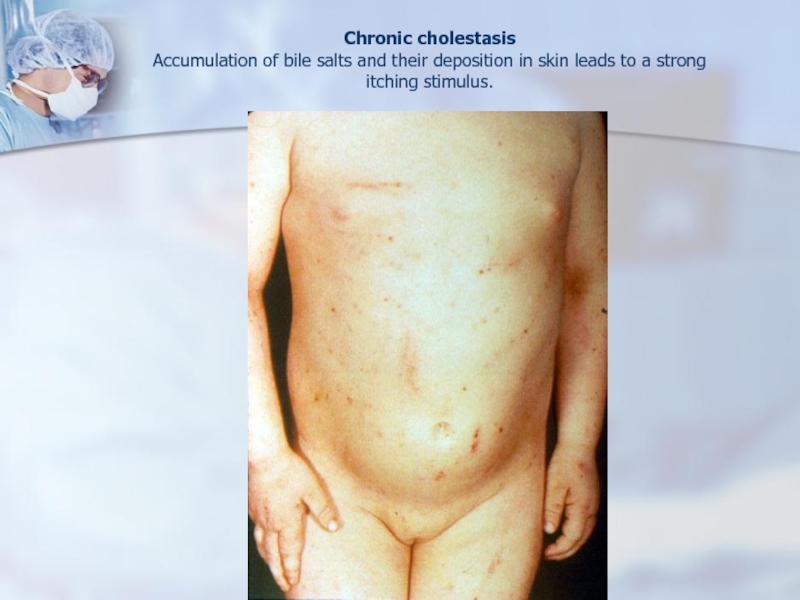
- 73. Chronic cholestasis Accumulation of bile salts and
- 74. Cirrhosis
- 75. Macronodular Cirrhosis:
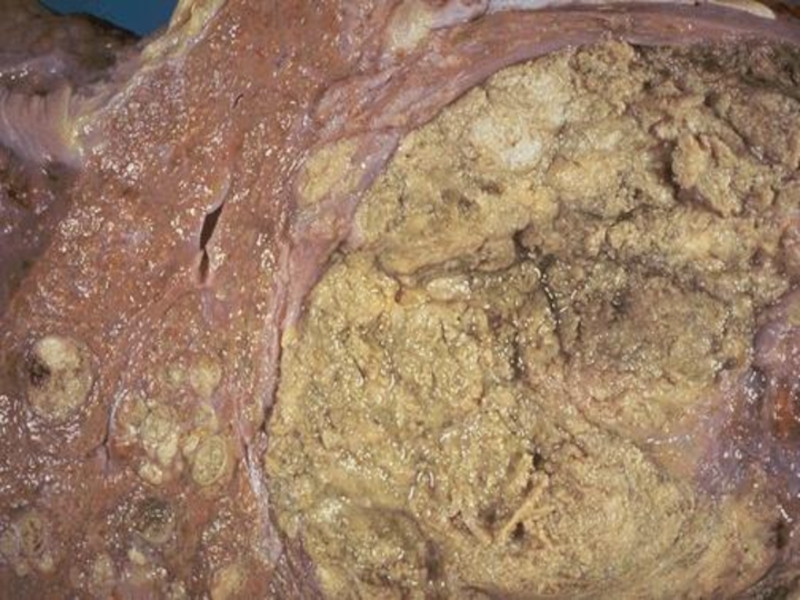
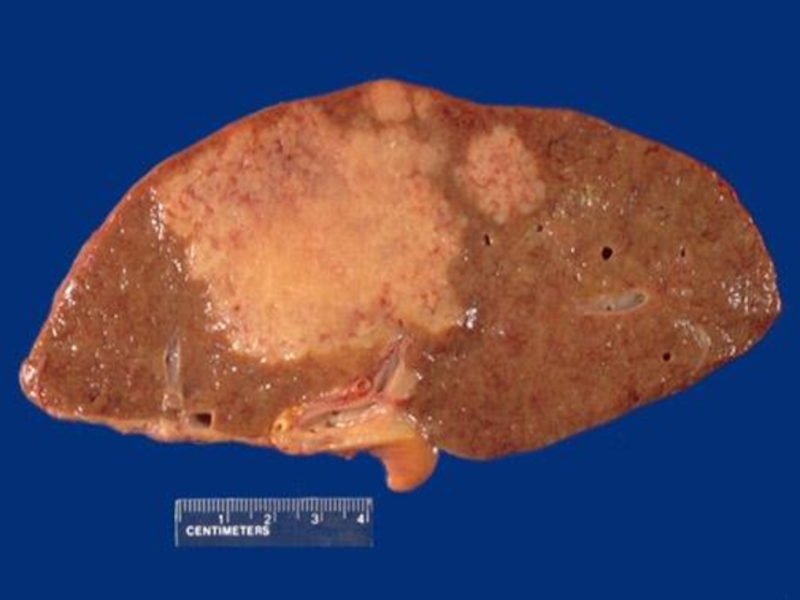
- 76. Liver cancerBackground disease – cirrhosis
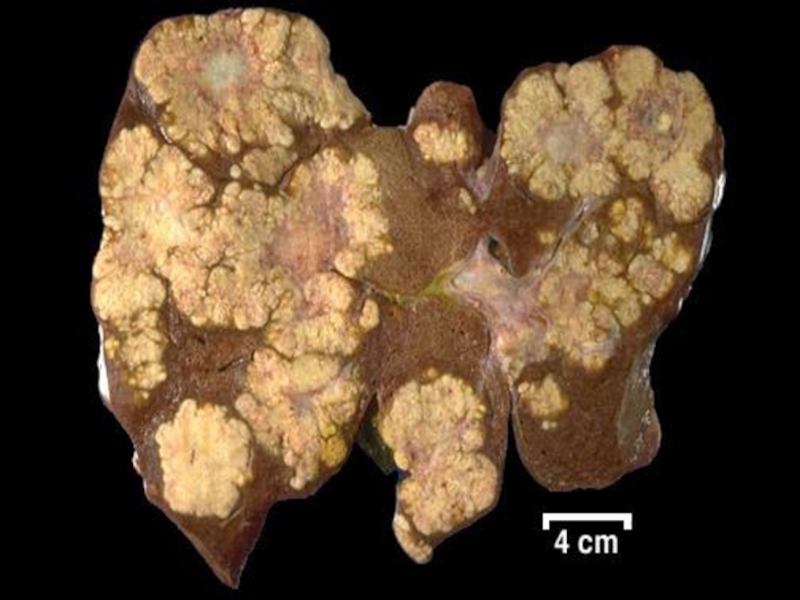
- 77. Anatomical formsNodularMassiveDiffuse
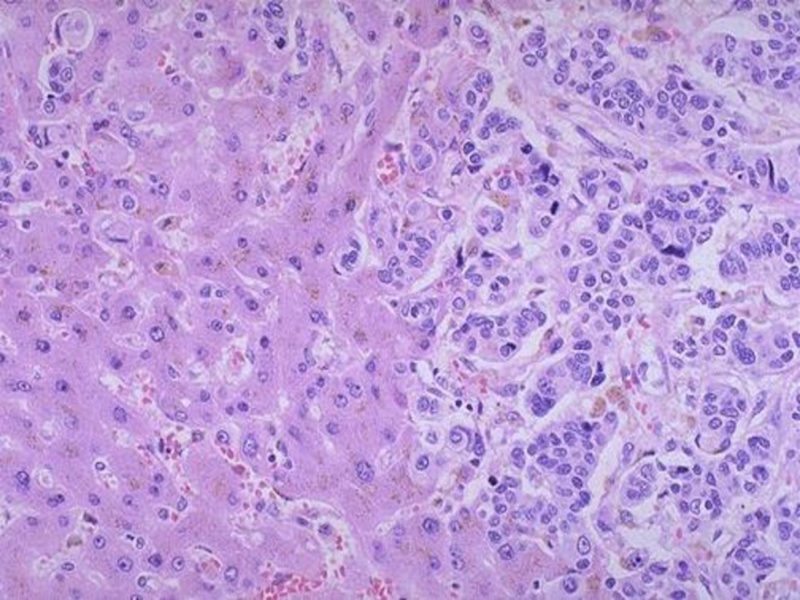
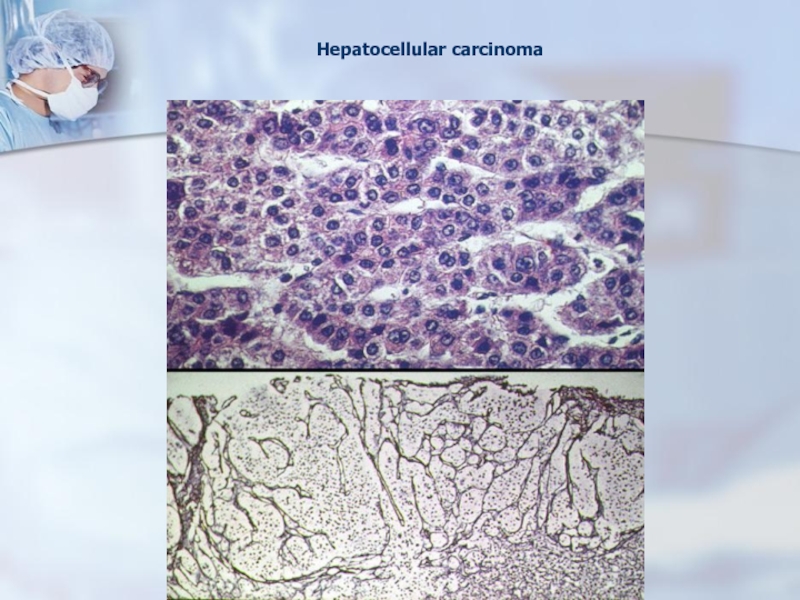
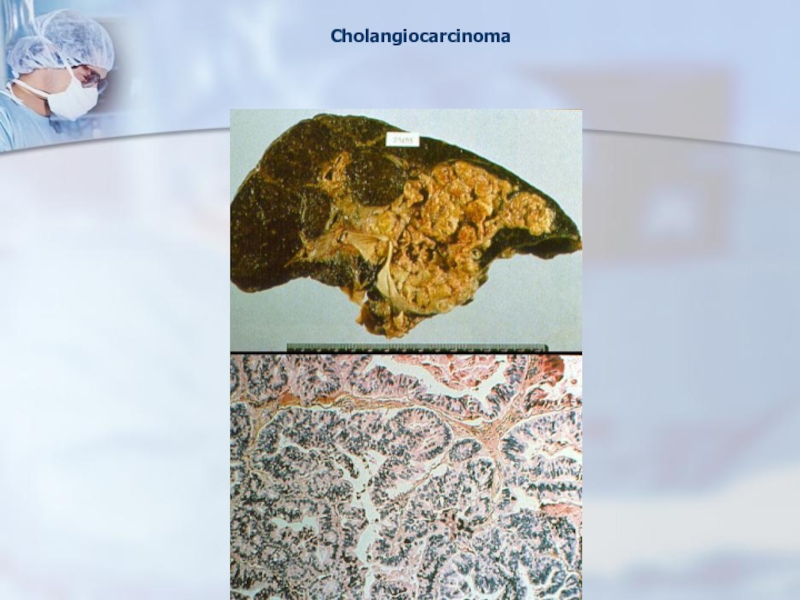
- 78. Histological formsHepatocellular carcinomaCholangiocellular carcinoma
- 79. Слайд 79
- 80. Слайд 80
- 81. Слайд 81
- 82. Слайд 82
- 83. Слайд 83
- 84. Слайд 84
- 85. Слайд 85
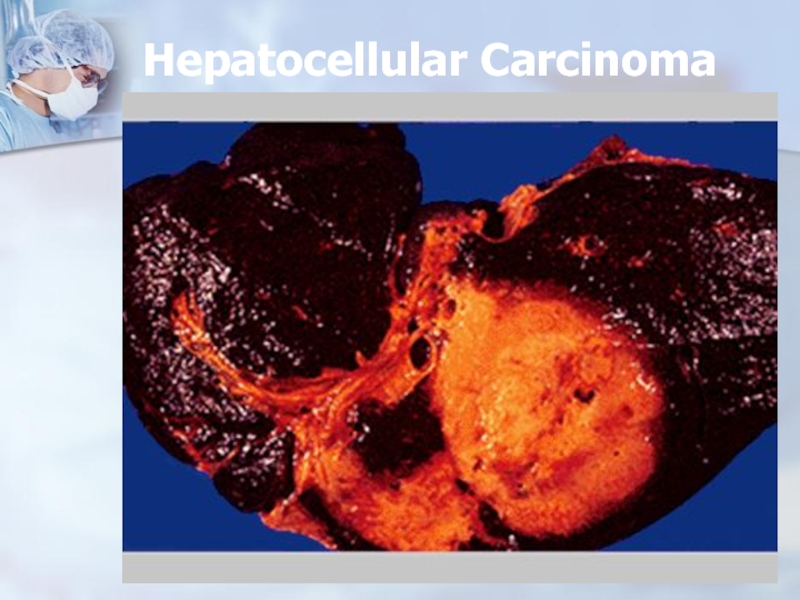
- 86. Hepatocellular Carcinoma
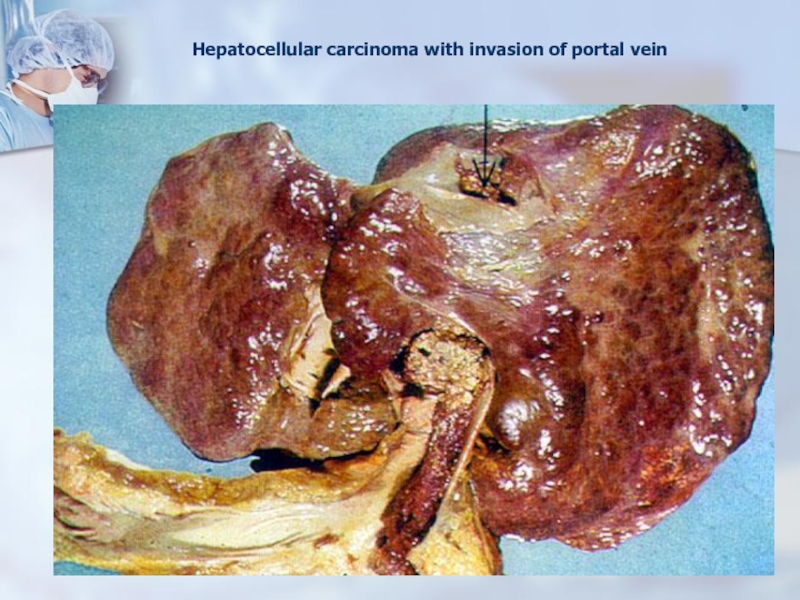
- 87. Hepatocellular carcinoma with invasion of portal vein
- 88. Hepatocellular carcinoma
- 89. Cholangiocarcinoma
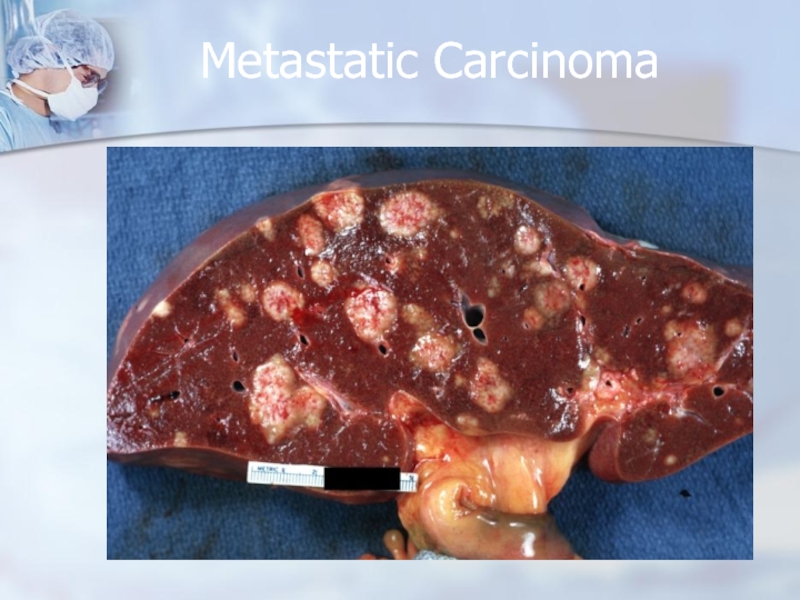
- 90. Metastatic Carcinoma
- 91. The end
- 92. Скачать презентанцию
Clinical features of hepatic failureJaundiceHypoalbuminemiaCoagulopathyDICFetor hepaticusIncreased serum levels of hepatic enzymesGynecomastiaHepatic encephalopathyHepatorenal syndrome
Слайды и текст этой презентации
Слайд 6Clinical features of hepatic failure
Jaundice
Hypoalbuminemia
Coagulopathy
DIC
Fetor hepaticus
Increased serum levels of hepatic
enzymes
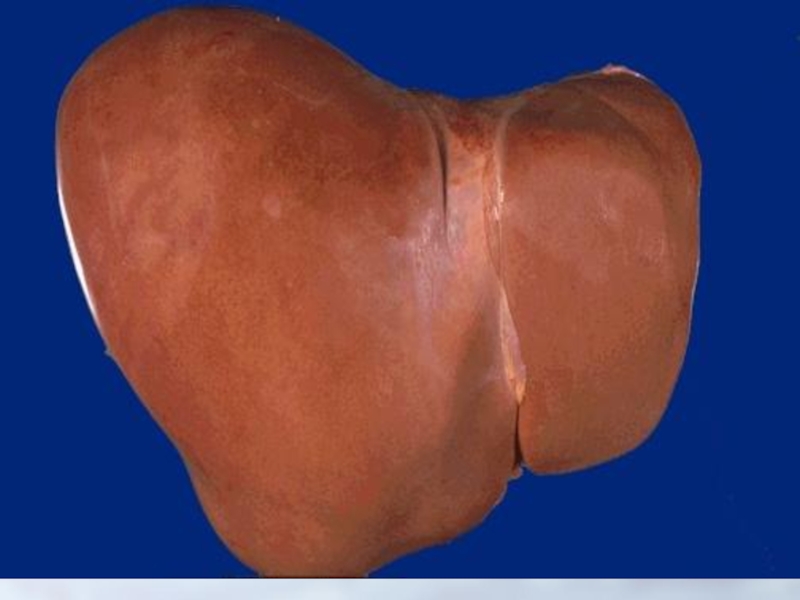
Слайд 7Diseases of liver
The liver is vulnerable to a wide variety
of metabolic, toxic, microbial, circulatory, and neoplastic insults. In some
instances, the disease is primary to the liver, as in viral hepatitis and hepatocellular carcinoma. More often the hepatic involvement is secondary, often to some of the most often diseases in humans, such as cardiac decompensation, disseminated cancer, alcoholism, and extrahepatic infections.Слайд 8MORPHOLOGIC PATTERNS OF HEPATIC INJURY
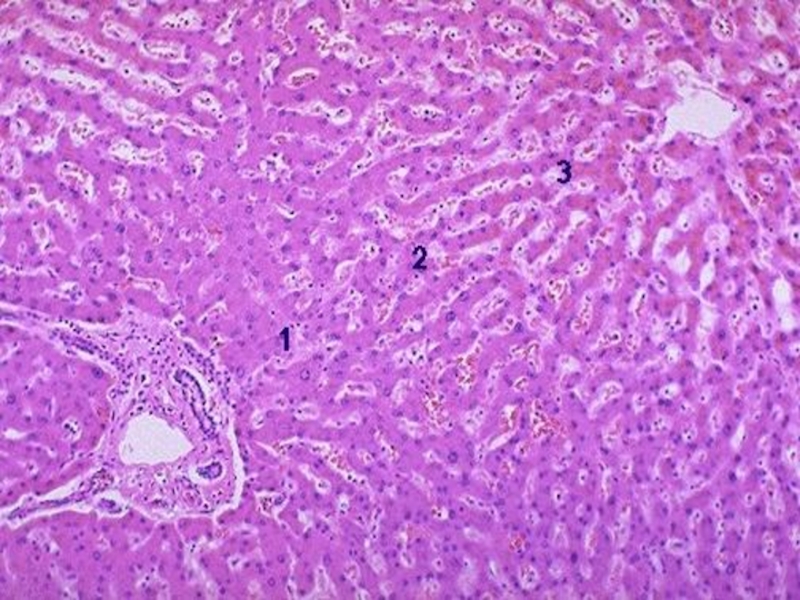
Regardless of cause, five general reactions
may occur:
Necrosis.
Degeneration.
Inflammation.
Regeneration.
Fibrosis.
Слайд 11Hepatoses – group of diseases characterized by dystrophy and necrosis
of hepatocytes
Chronic
Fatty degeneration
Hepatoses
Acute
Massive progressive necrosis
of the liver
(toxic dystrophy of
the liver)Слайд 12Massive progressive
necrosis of liver
Etiology:
exogenous factors-fungi, food toxins, arsenic.
Endogenous-gestosis
of pregnancy, thyrotoxicosis
Pathogenesis-toxic substances affect the hepatocytes direсtly, mainly in
the central part of lobules.Слайд 13Massive progressive necrosis of the liver
Morphogenesis:
Stage of yellow degeneration
1-
2 week
Stage of red degeneration –
3 week
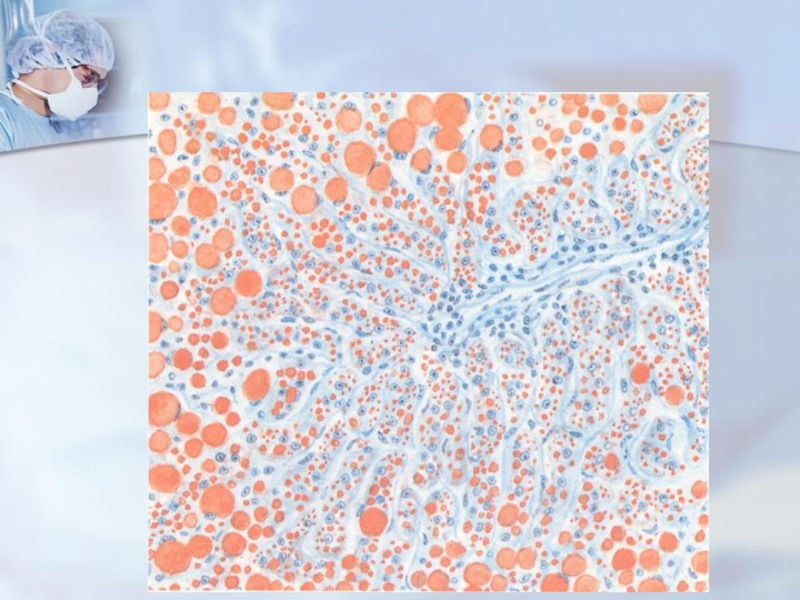
Слайд 20Fatty hepatosis
Etiology: alcohol, medicines, metabolic disorders (diabetes mellitus, defective protein
nutrition, excessive fat consumption), cardiac insufficiency, anemia.
Morphology: in hepatocytes
appear fat droplets, which can be small or big. Слайд 21Stages of development
Ordinary (simple) obesity
Obesity in combination with the necroses
of hepatocytes and mesenchymal-cellular reaction
Obesity in combination with the reorganization
of tissueOutcome: portal cirrhosis of the liver
Слайд 26Viral hepatitis
Etiology: Viruses hepatitis A,B,C,D…
Viral hepatitis is reserved for infection
of the liver caused by a small (but growing) group
of viruses having a particular affinity for the liver.Слайд 27Hepatitis A Virus does not cause chronic hepatitis or a
carrier state and only rarely causes fulminant hepatitis, and so
the fatality rate associated with Hepatitis A Virus is about 0.1 %.Hepatitis В Virus can produce 1) acute hepatitis, 2) chronic nonprogressive hepatitis, 3) progressive chronic disease ending in cirrhosis, 4) fulminant hepatitis with massive liver necrosis, and 5) an asymptomatic carrier state with or without progressive disease. Furthermore, Hepatitis В Virus plays an important role in the development of hepatocellular carcinoma.
Слайд 28Transfusion, blood products, dialysis, needle-stick accidents among health care workers,
intravenous drug abuse, and homosexual activity constitute primary risk categories
for Hepatitis В Virus infection.Hepatitis С Virus has a high rate of progression to chronic disease and eventual cirrhosis, exceeding 50 %.
Слайд 29Whatever the agent is, the disease is more or less
the same and can be divided into four phases:
1) an
incubation period,2) a symptomatic preicteric phase,
3) a symptomatic icteric phase, and
4) convalescence.
Слайд 30Forms of viral hepatitis
Cyclic icteric
Non-icteric
Cholestatic
Necrotic
Chronic (active and persistent)
Слайд 31Morphological signs
Protein degeneration
Proliferation of Kupffer cells
Lymphohistiocytic infiltration
Councilman bodies (
necrotic hepatocytes may be evident as fragmented, eosinophilic bodies оr
may be phagocytosed, leading to the accumulaton of clumps of lymphocytes and macrophages.Слайд 36Acute hepatitis with secondary submassive necrosis (NECROTIC FORM) Nodule formation reflects regenerative
activity.
Слайд 39CHRONIC HEPATITIS
Symptomatic, biochemical or serologic evidence of continuing or relapsing
hepatic disease for more than 6 months, optimally with histologically
documented inflammation and necrosis, is taken to mean chronic hepatitis.Слайд 40etiologic forms of hepatitis
Hepatitis A Virus: Extremely rare.
Hepatitis В
Virus: Develops in more than 90% of infected neonates and
5 % of infected adults, of whom one-fourth progresses to cirrhosis.Hepatitis С Virus: Develops in more than 50 % of infected patients, of whom half progresses to cirrhosis.
Hepatitis D Virus: Rare in acute Hepatitis D Virus/ Hepatitis В Virus coinfection; a more severe chronic hepatitis is the most frequent outcome of Hepatitis D Virus superinfection.
Hepatitis E Virus: Does not produce chronic hepatitis.
Слайд 41Since 1968, chronic hepatitis has been classified according to the
extent of inflammation:
1. Chronic persistent hepatitis, in which inflammation is
confined to the portal tracts.2. Chronic active hepatitis, in which portal tract inflammation spills into the parenchyma and surrounding regions of necrotic hepatocytes.
3. Chronic lobular hepatitis, in which persistent inflammation is confined to the lobule.
Слайд 42Chronic active hepatitis Liver shows significant collapse indicative of progression to
cirrhosis.
Слайд 44Chronic active hepatitis The limiting plate regions are blurred due to
an inflammatory infiltrate.
Слайд 45Chronic persistent hepatitis Chronic viral hepatitis manifests as a portal inflammatory
infiltrate.
Слайд 49Markers of AH
Fatty dystrophy and necrosis of hepatocytes
Alcoholic hyaline
( Mallory bodies)
Prevalence of neutrophils in the infiltrate
Слайд 54Cirrhosis
Is chronic disease of liver which is characterized by hepatic
failure due to structural reorganization of liver.
Cirrhosis is among
the top ten causes of death in the world, largely the result of alcohol abuse, chronic hepatitis and biliary disease. Слайд 55This end stage of liver disease is defined by three
characteristics:
- Fibrosis is present in the form of delicate bands
or broad scars replacing multiple adjacent lobules.- The parenchymal architecture of the entire liver is disruptured by interconnecting fibrous scars.
- Parenchymal nodules are created by regeneration of hepatocytes, The nodules may vary from micronodules (less than 3 mm in diameter) to macronodules (3 mm to several centimeters in diameter).
Слайд 65Primary biliary cirrhosis Inflamed and destroyed bile ducts are characteristic of
this disorder.
Слайд 66Portal areas contain an extensive scarring process obliterating vascular channels as
well as bile ducts.
Слайд 67Several features should be understood:
- The parenchymal injury and consequent
fibrosis are diffuse, extending throughout the liver; focal injury with
scarring does not constitute cirrhosis.- Nodularity is requisite for the diagnosis and reflects the balance between regenerative activity and constrictive scarring.