Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
TAKAYASU’S ARTERITIS
Содержание
- 1. TAKAYASU’S ARTERITIS
- 2. EPIDEMIOLOGYMore case reports from Japan ,India, South-east
- 3. Age Mc-2nd
- 4. Слайд 4
- 5. HistopathologyIdiopathic c/c infla arteritis of elastic arteries
- 6. Слайд 6
- 7. Слайд 7
- 8. Wall thickening, Fibrosis, Stenosis, & Thrombus formation
- 9. Associated pathology-TB (LN)-55%
- 10. Clinical featuresEarly pre pulseless/gen manifFever,weight loss,headache, fatigue,malaise,night
- 11. Слайд 11
- 12. Coronary involvement in TAOccurs in 10~30%Often fatalClassified
- 13. Occular involvement-Amaurosis fugax, pain behind eye,
- 14. Слайд 14
- 15. HTN is the most characteristic manifestation in
- 16. Ishikawa clinical classification of Takayasu arteritis 19784 Complications Retinopathy, Secondary HTN, AR, & Aneurysm
- 17. Слайд 17
- 18. Cumulative survival 5years -91% (event free survival
- 19. Слайд 19
- 20. Слайд 20
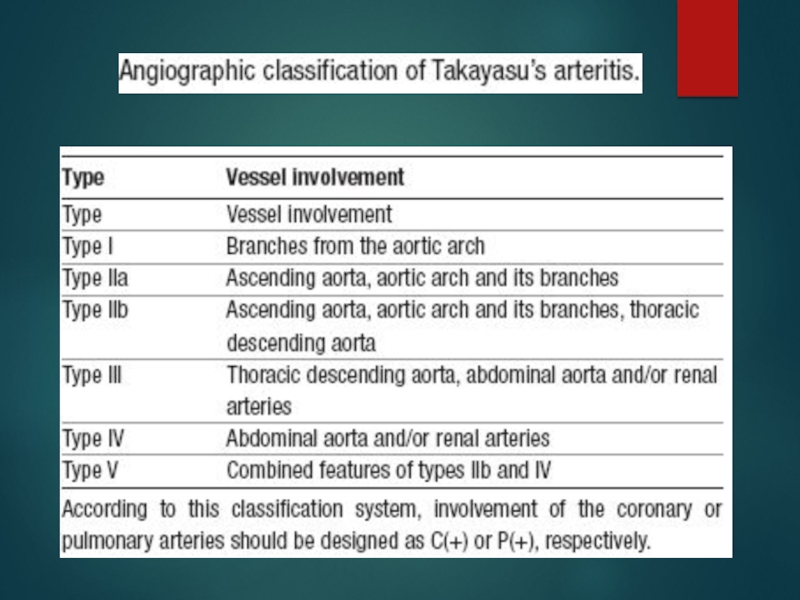
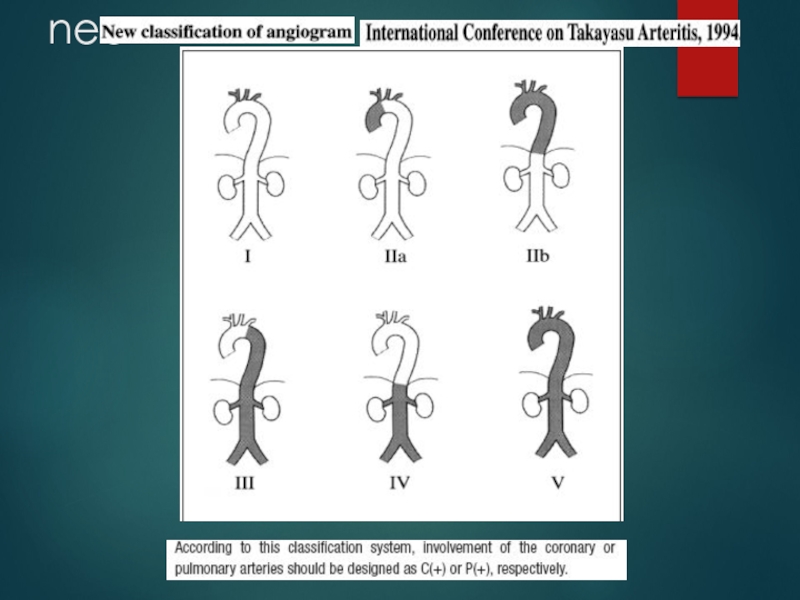
- 21. Sharma BK, Jain S, Suri S, Numano
- 22. Слайд 22
- 23. nee
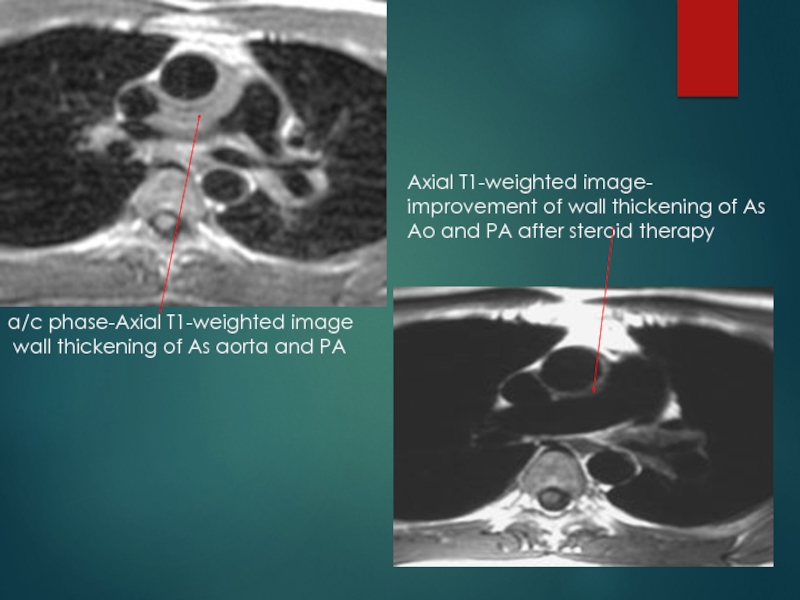
- 24. a/c phase-Axial T1-weighted image wall thickening
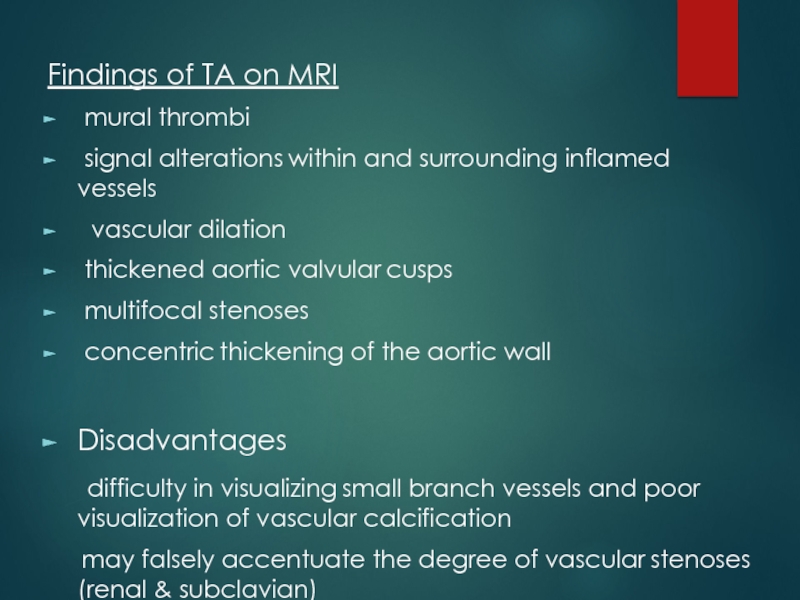
- 25. Findings of TA on MRI mural
- 26. [18F]fluorodeoxyglucose PET for diagnosing Takayasu’s arteritiscommon [18F]FDG
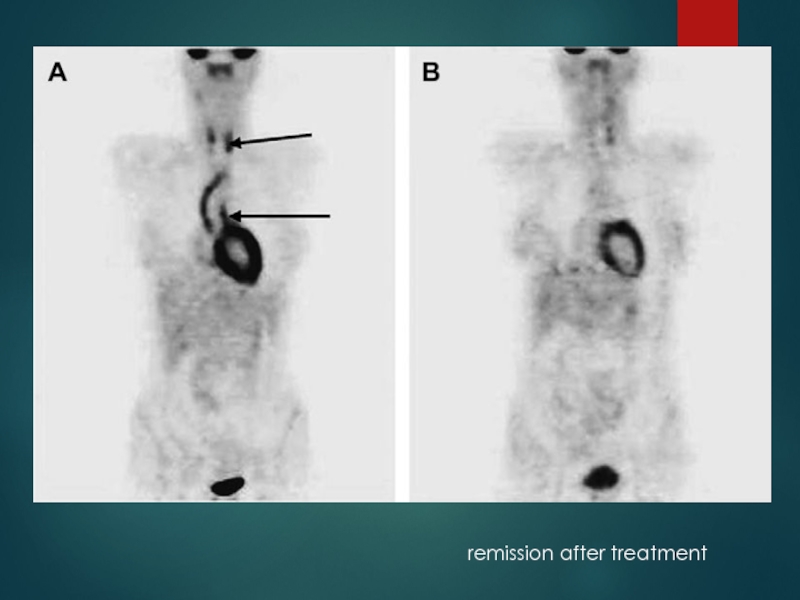
- 27. remission after treatment
- 28. Treatment of TA ・ Steroidsimmunosuppressants:Cyclosporine,Cyclophosphamide,Mtx,Mycophenolate mofetilAnti-platelet therapy(low-dose Aspirin)angioplasty/surgeryIf uncontrolledControl of vasculitisSymptomatic occlusionthrombosis
- 29. Medical treatment 0.7-1 mg/kg/day –prednisolone for 1-3
- 30. Steroids → 50% responseMethotrexate →further 50% respond25%
- 31. Critical issue is in trying to determine
- 32. chronic phase- persistent inflammation
- 33. Surgical treatmentHTN with critical RASExtremity claudication limiting
- 34. Surgical techniquesCarry high morbidity & mortalitySteno /aneurysm -anastomotic points Progressive nature of TADiffuse nature of TA
- 35. Renal artery involvementBest treated by PTAStent placement following PTAOstial lesionsLong segment lesionsIncomplete relief of stenoses Dissection
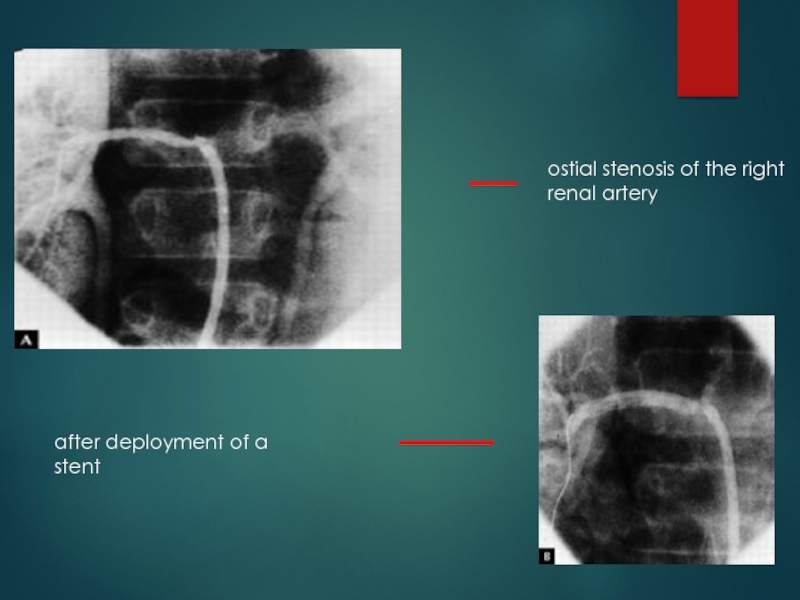
- 36. ostial stenosis of the right renal arteryafter deployment of a stent
- 37. Renal PTA - 33 stenoses (20 pts)
- 38. Aortoarteritic lesionsBalloon dilation safe & reasonably effectiveCan
- 39. Left subclavian angiograms- 95% stenosis with extensive collaterals Post angioplasty and stenting.
- 40. Joseph s et al, SCT J Vasc
- 41. Aortoplasty and StentingPTA -desc thoracic and/or abd
- 42. long-segment diffuse stenotic involvement of the DTAafter deployment of stents.
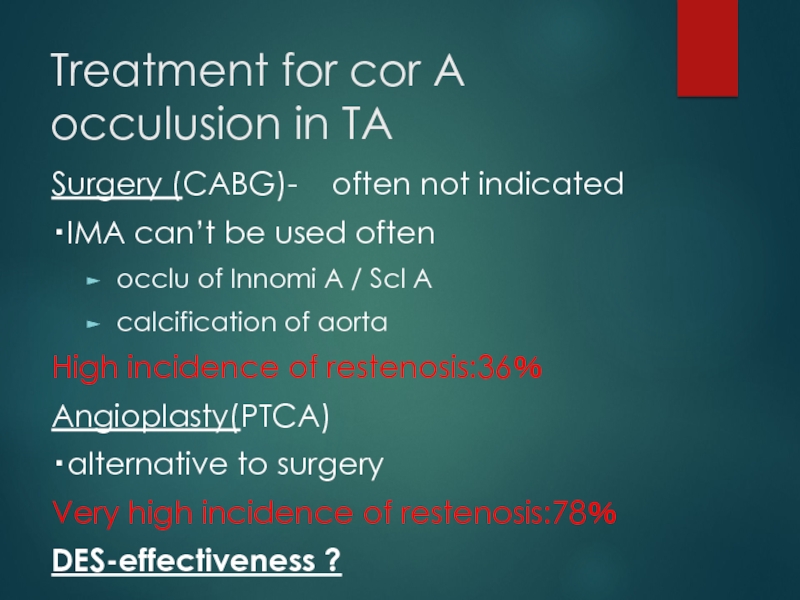
- 43. Treatment for cor A occulusion in TASurgery
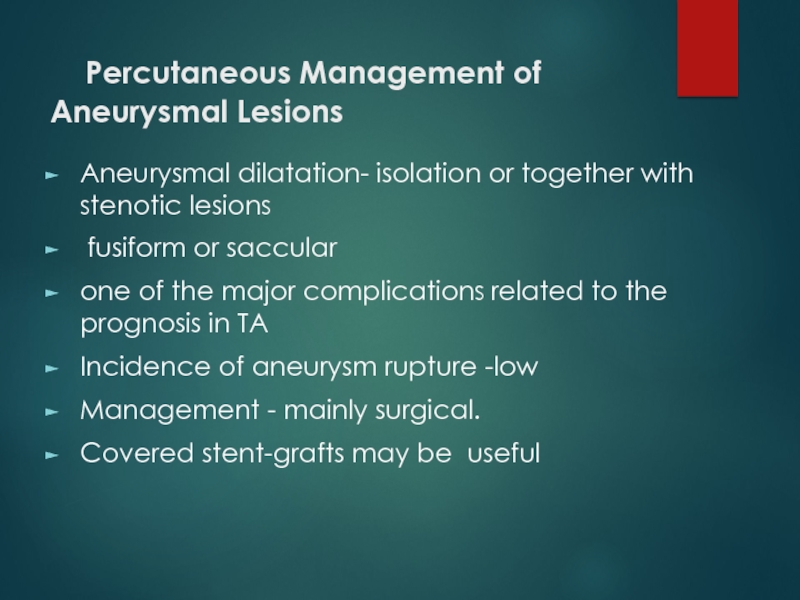
- 44. Percutaneous Management of Aneurysmal Lesions
- 45. Скачать презентанцию
Слайды и текст этой презентации
Слайд 2EPIDEMIOLOGY
More case reports from Japan ,India, South-east Asia, Mexico
No geographic
restriction
women.Слайд 3 Age
Mc-2nd & 3rd decade
May
range from infancy to middle age
Indian studies-age 3- 50 yrs
Gender diff Japan-F:M=8-9:1
India-F:M ratio varies from -1:1 - 3:1
( Padmavati S, Aurora AP, Kasliwal RR Aortoarteritis in India. J Assoc Physicians India 1987)
India=F:M- 6.4:1 (Panja et al, 1997 JACC)
Слайд 4
Genetics
Japan - HLA-B52 and B39
Mexican and Colombian patients - HLA-DRB1*1301 and HLA-DRB1*1602
India- HLA- B 5, -B 21
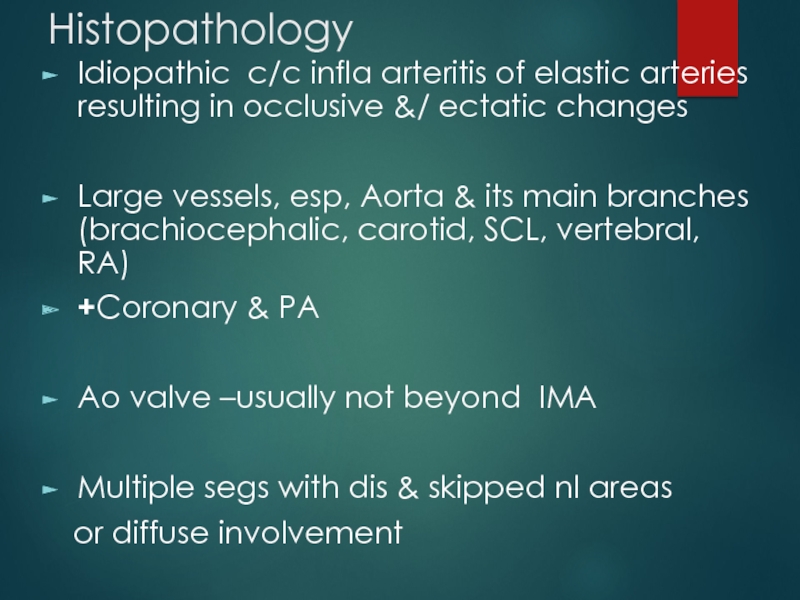
Слайд 5Histopathology
Idiopathic c/c infla arteritis of elastic arteries resulting in occlusive
&/ ectatic changes
Large vessels, esp, Aorta & its main branches
(brachiocephalic, carotid, SCL, vertebral, RA) +Coronary & PA
Ao valve –usually not beyond IMA
Multiple segs with dis & skipped nl areas
or diffuse involvement
Слайд 7
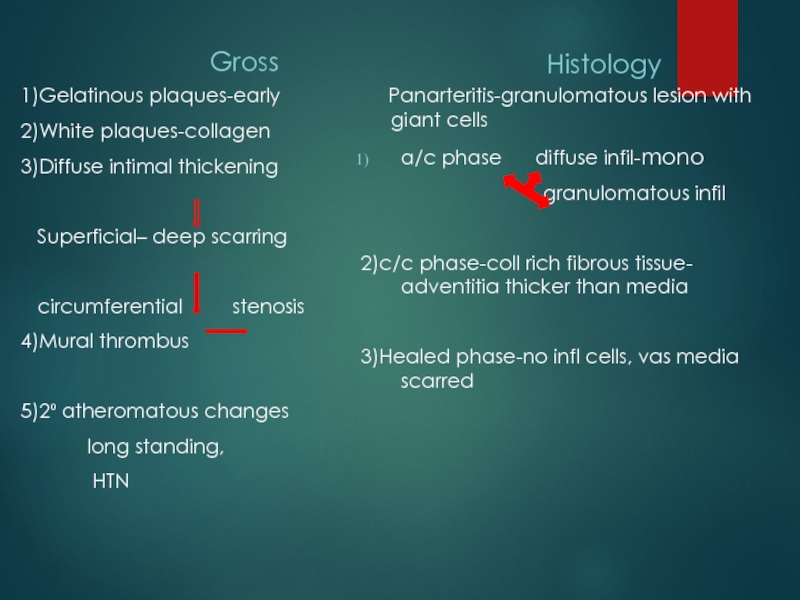
Gross
1)Gelatinous plaques-early
2)White plaques-collagen
3)Diffuse intimal thickening
Superficial– deep scarring
circumferential stenosis4)Mural thrombus
5)2⁰ atheromatous changes
long standing,
HTN
Histology
Panarteritis-granulomatous lesion with giant cells
a/c phase diffuse infil-mono
granulomatous infil
2)c/c phase-coll rich fibrous tissue- adventitia thicker than media
3)Healed phase-no infl cells, vas media scarred
Слайд 8
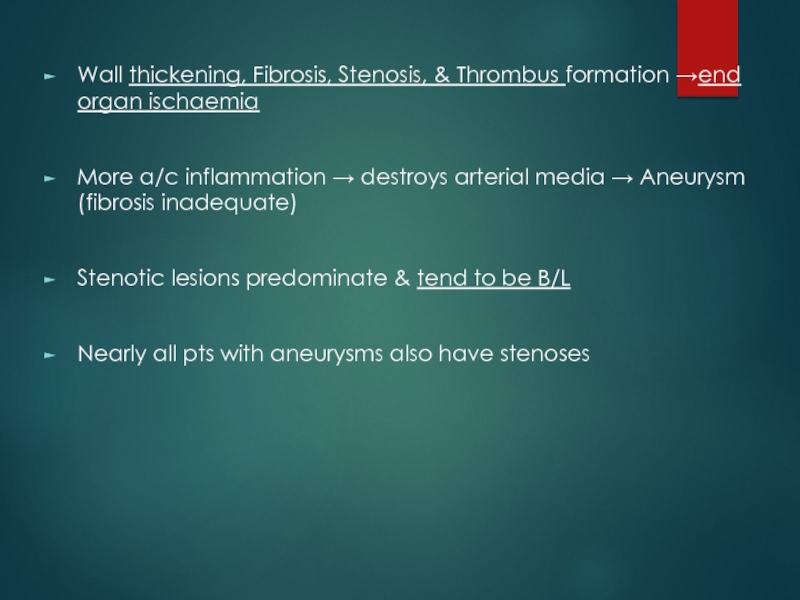
Wall thickening, Fibrosis, Stenosis, & Thrombus formation →end organ ischaemia
More
a/c inflammation → destroys arterial media → Aneurysm (fibrosis inadequate)
Stenotic
lesions predominate & tend to be B/LNearly all pts with aneurysms also have stenoses
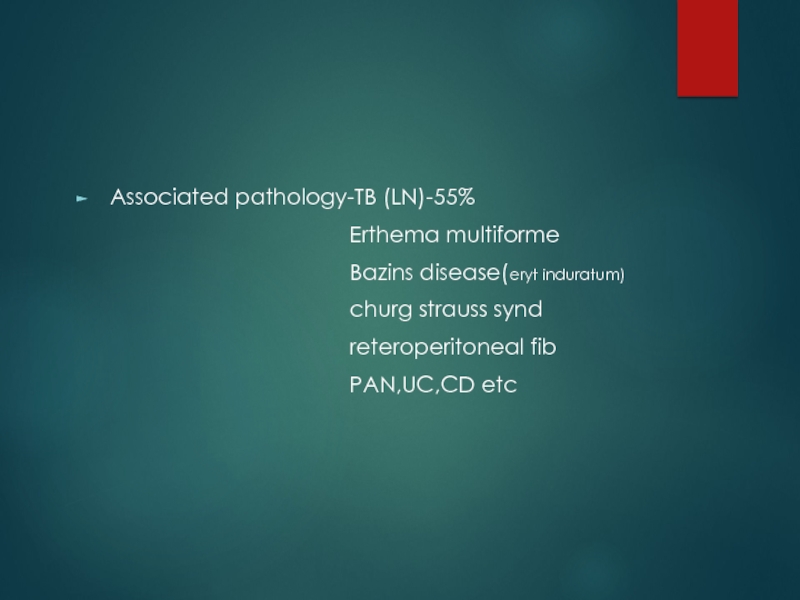
Слайд 9Associated pathology-TB (LN)-55%
Erthema multiforme
Bazins disease(eryt induratum)
churg strauss synd
reteroperitoneal fib
PAN,UC,CD etc
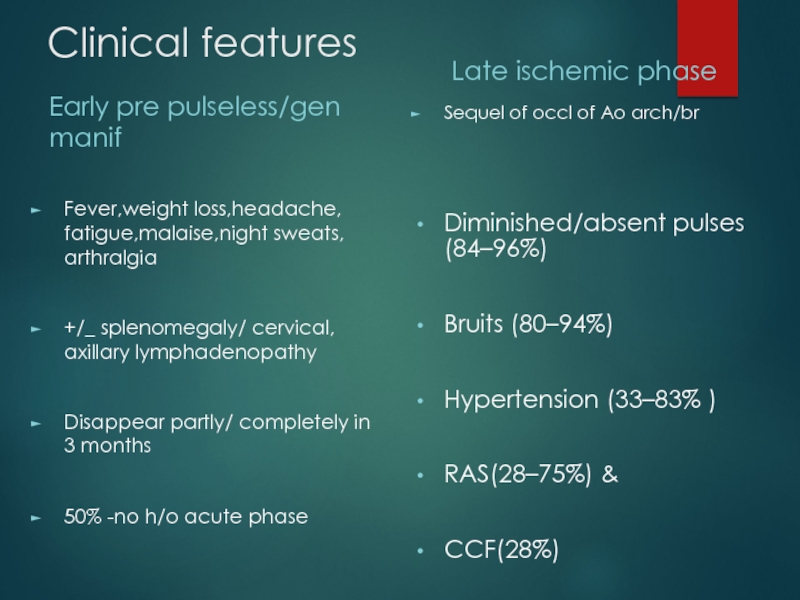
Слайд 10Clinical features
Early pre pulseless/gen manif
Fever,weight loss,headache, fatigue,malaise,night sweats, arthralgia
+/_ splenomegaly/
cervical, axillary lymphadenopathy
Disappear partly/ completely in 3 months
50% -no h/o
acute phase Late ischemic phase
Sequel of occl of Ao arch/br
Diminished/absent pulses (84–96%)
Bruits (80–94%)
Hypertension (33–83% )
RAS(28–75%) &
CCF(28%)
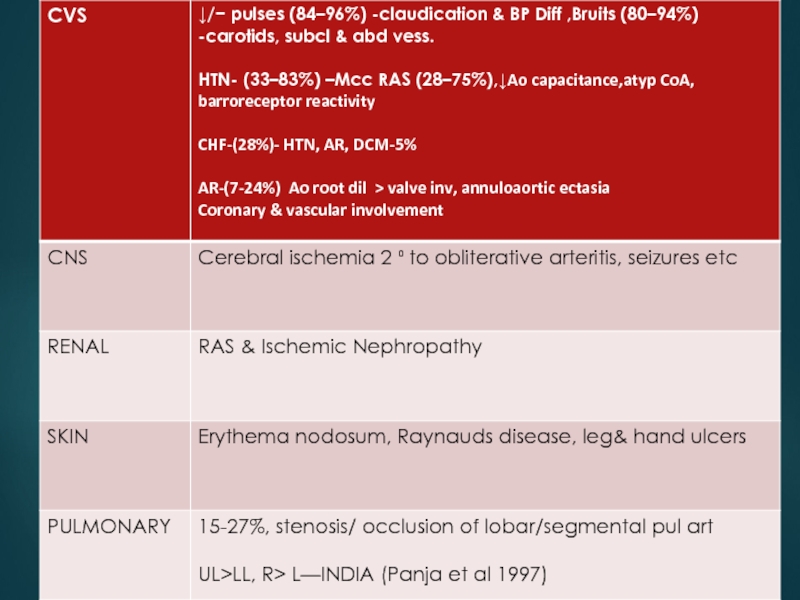
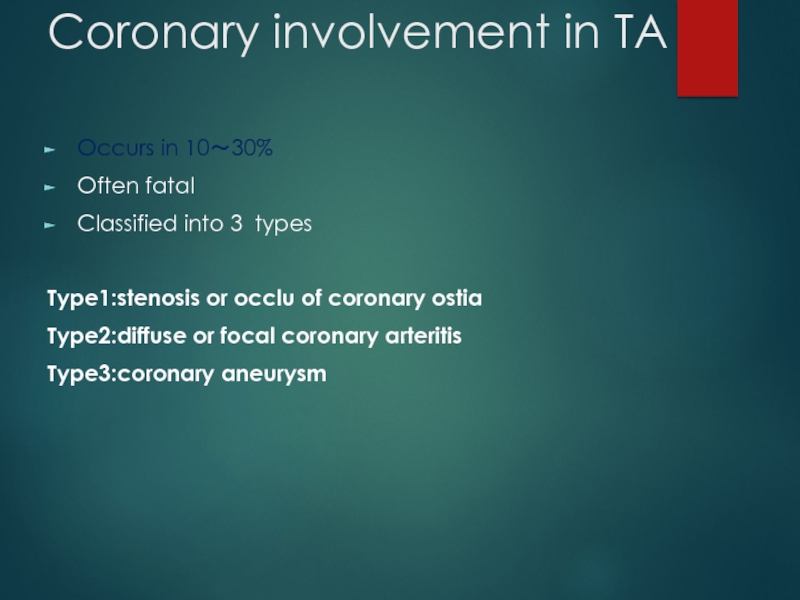
Слайд 12Coronary involvement in TA
Occurs in 10~30%
Often fatal
Classified into 3 types
Type1:stenosis
or occlu of coronary ostia
Type2:diffuse or focal coronary arteritis
Type3:coronary aneurysm
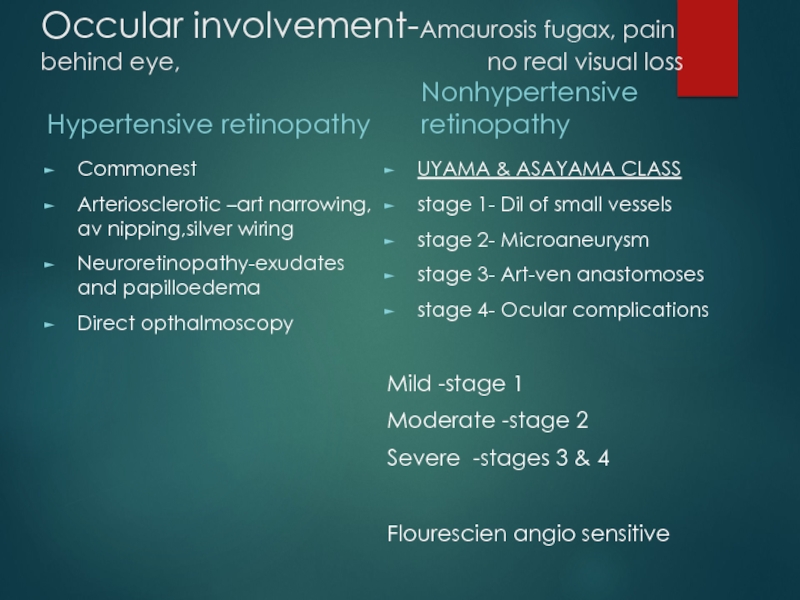
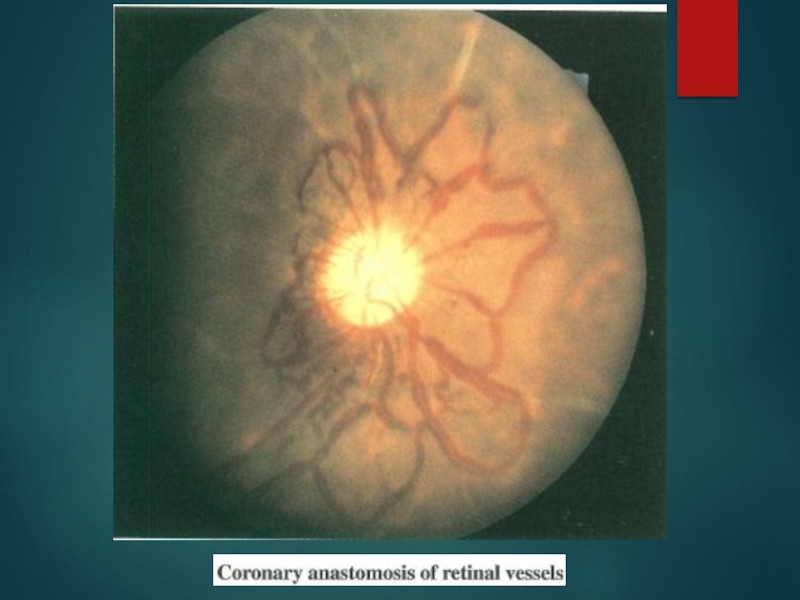
Слайд 13Occular involvement-Amaurosis fugax, pain behind eye,
no real visual
lossHypertensive retinopathy
Commonest
Arteriosclerotic –art narrowing, av nipping,silver wiring
Neuroretinopathy-exudates and papilloedema
Direct opthalmoscopy
Nonhypertensive retinopathy
UYAMA & ASAYAMA CLASS
stage 1- Dil of small vessels
stage 2- Microaneurysm
stage 3- Art-ven anastomoses
stage 4- Ocular complications
Mild -stage 1
Moderate -stage 2
Severe -stages 3 & 4
Flourescien angio sensitive
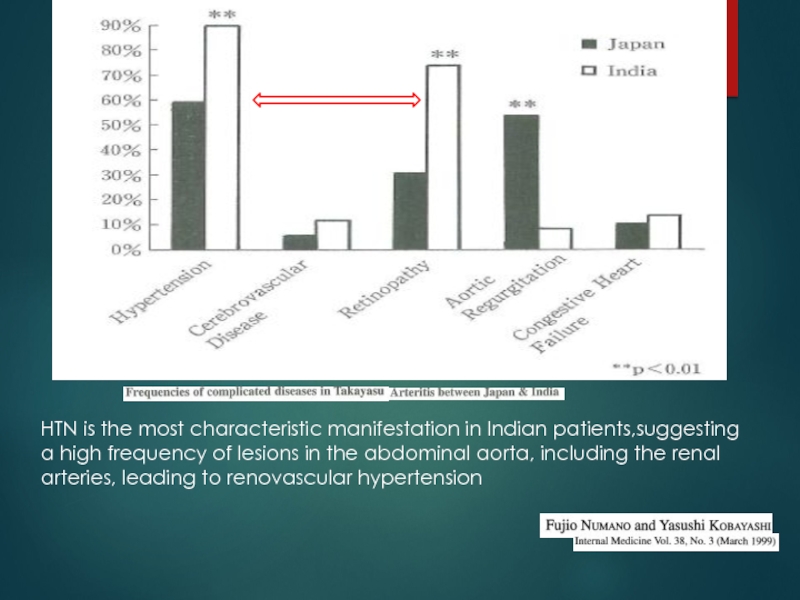
Слайд 15HTN is the most characteristic manifestation in Indian patients,suggesting a
high frequency of lesions in the abdominal aorta, including the
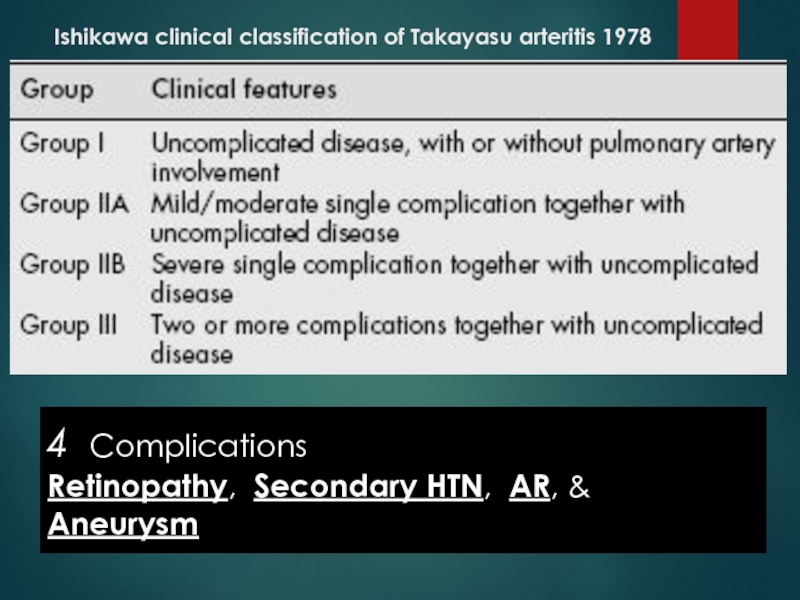
renal arteries, leading to renovascular hypertensionСлайд 16Ishikawa clinical classification of Takayasu arteritis 1978
4 Complications
Retinopathy, Secondary
HTN, AR, & Aneurysm
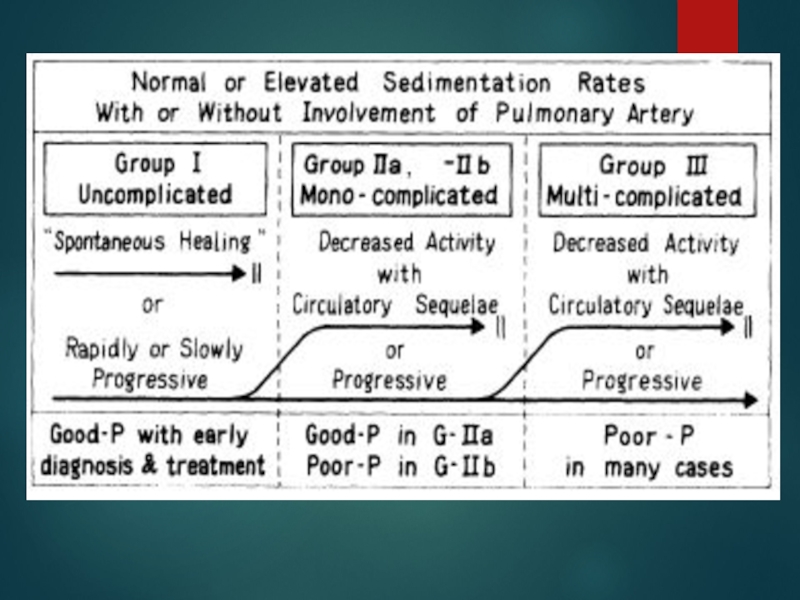
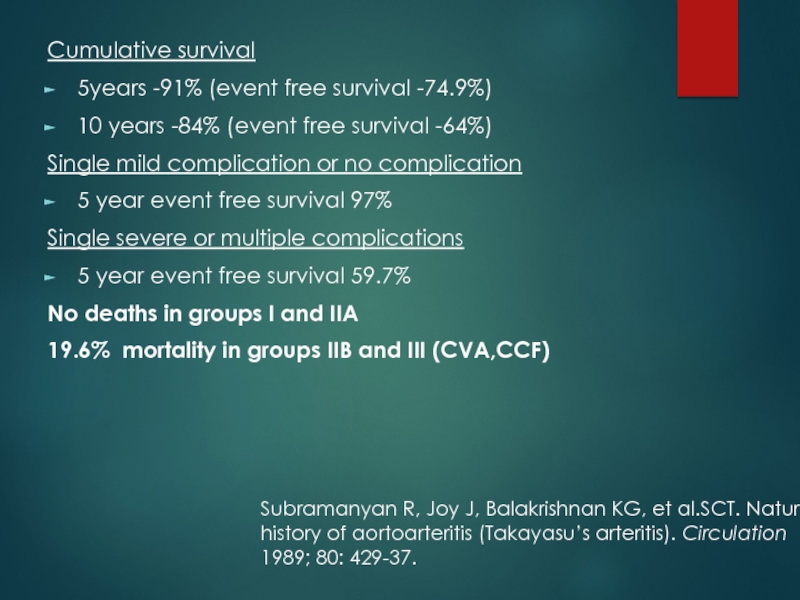
Слайд 18Cumulative survival
5years -91% (event free survival -74.9%)
10 years -84%
(event free survival -64%)
Single mild complication or no complication
5
year event free survival 97% Single severe or multiple complications
5 year event free survival 59.7%
No deaths in groups I and IIA
19.6% mortality in groups IIB and III (CVA,CCF)
Subramanyan R, Joy J, Balakrishnan KG, et al.SCT. Natural
history of aortoarteritis (Takayasu’s arteritis). Circulation
1989; 80: 429-37.
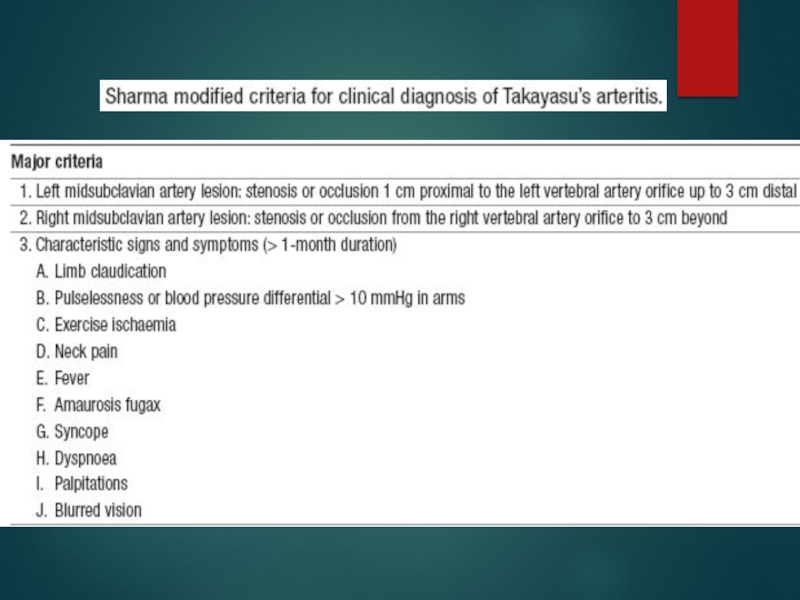
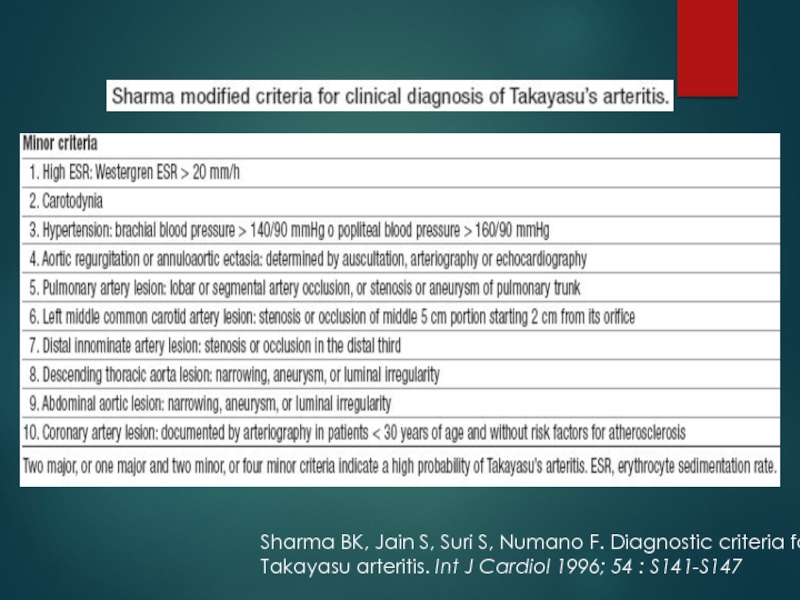
Слайд 21Sharma BK, Jain S, Suri S, Numano F. Diagnostic criteria
for
Takayasu arteritis. Int J Cardiol 1996; 54 : S141-S147
Слайд 24a/c phase-Axial T1-weighted image
wall thickening of As aorta
and PA
Axial T1-weighted image- improvement of wall thickening of As
Ao and PA after steroid therapyСлайд 25Findings of TA on MRI
mural thrombi
signal alterations
within and surrounding inflamed vessels
vascular dilation
thickened aortic
valvular cuspsmultifocal stenoses
concentric thickening of the aortic wall
Disadvantages
difficulty in visualizing small branch vessels and poor visualization of vascular calcification
may falsely accentuate the degree of vascular stenoses (renal & subclavian)
Слайд 26[18F]fluorodeoxyglucose PET for diagnosing
Takayasu’s arteritis
common [18F]FDG uptake pattern TA
early phase - linear and continuous
late phase-patchy rather than continuous ,linear
shown to identify more affected vascular regions than morphologic imaging with MRI
does not provide any information about changes in the wall structure or luminal blood flow
sensitivities of 83% and specificity 100%
( Meller Jet al. Value of F-18 FDG hybrid camera PET and MRI in earlyTakayasu aortitis. Eur Radiol 2003)
Sensitivity of 92%, specificity of 100% and a diagnostic accuracy of 94%
( Webb M et al. The role of 18F-FDG PET in characterising disease activity in Takayasu arteritis. Eur J Nucl Med Imaging 2004
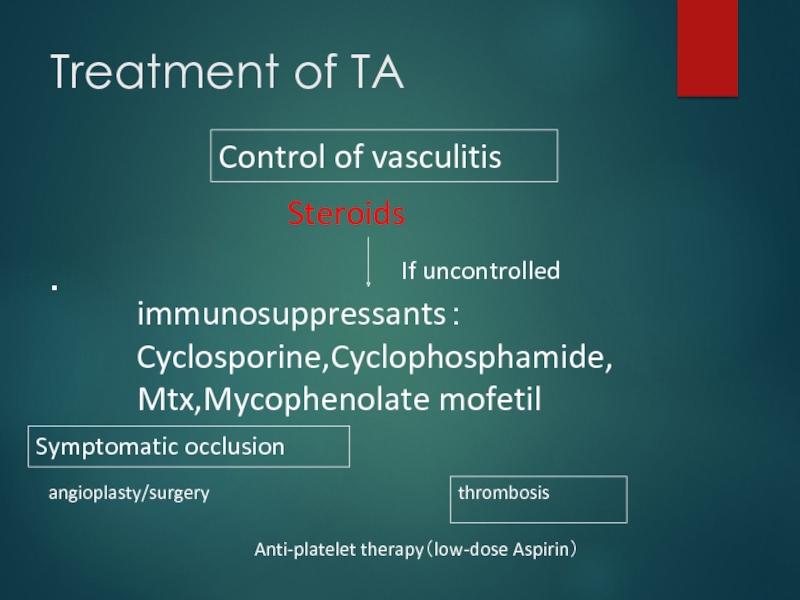
Слайд 28Treatment of TA
・
Steroids
immunosuppressants:
Cyclosporine,Cyclophosphamide,
Mtx,Mycophenolate mofetil
Anti-platelet therapy(low-dose Aspirin)
angioplasty/surgery
If uncontrolled
Control of vasculitis
Symptomatic occlusion
thrombosis
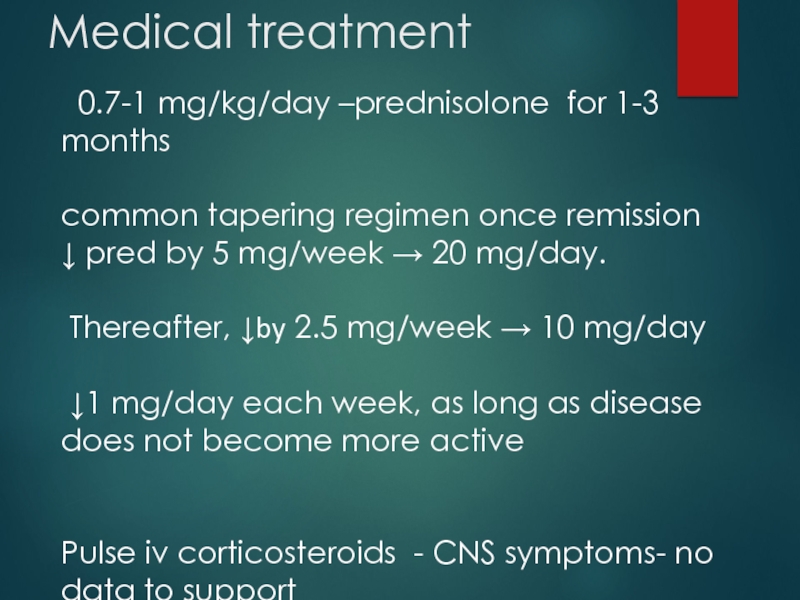
Слайд 29Medical treatment
0.7-1 mg/kg/day –prednisolone for 1-3 months
common tapering regimen
once remission
↓ pred by 5 mg/week → 20 mg/day.
Thereafter,
↓by 2.5 mg/week → 10 mg/day↓1 mg/day each week, as long as disease does not become more active
Pulse iv corticosteroids - CNS symptoms- no data to support
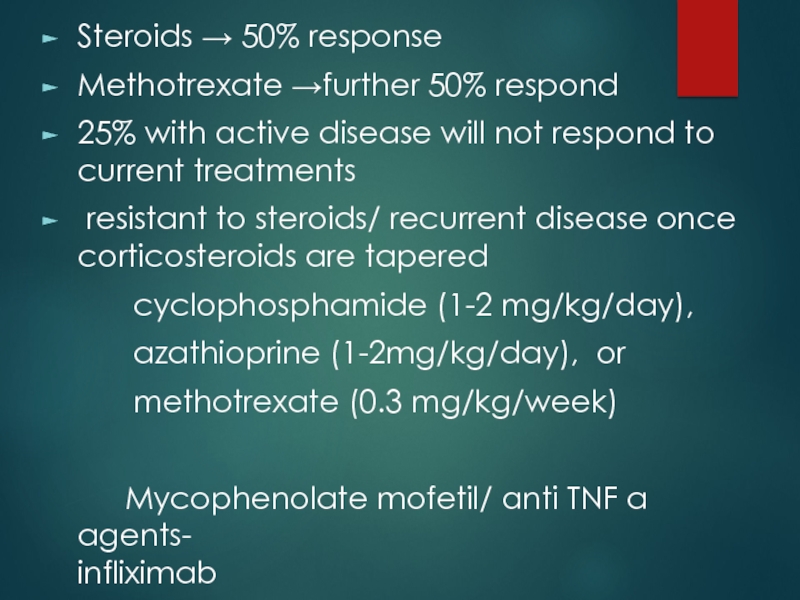
Слайд 30Steroids → 50% response
Methotrexate →further 50% respond
25% with active disease
will not respond to current treatments
resistant to steroids/ recurrent
disease once corticosteroids are taperedcyclophosphamide (1-2 mg/kg/day),
azathioprine (1-2mg/kg/day), or
methotrexate (0.3 mg/kg/week)
Mycophenolate mofetil/ anti TNF α agents- infliximab
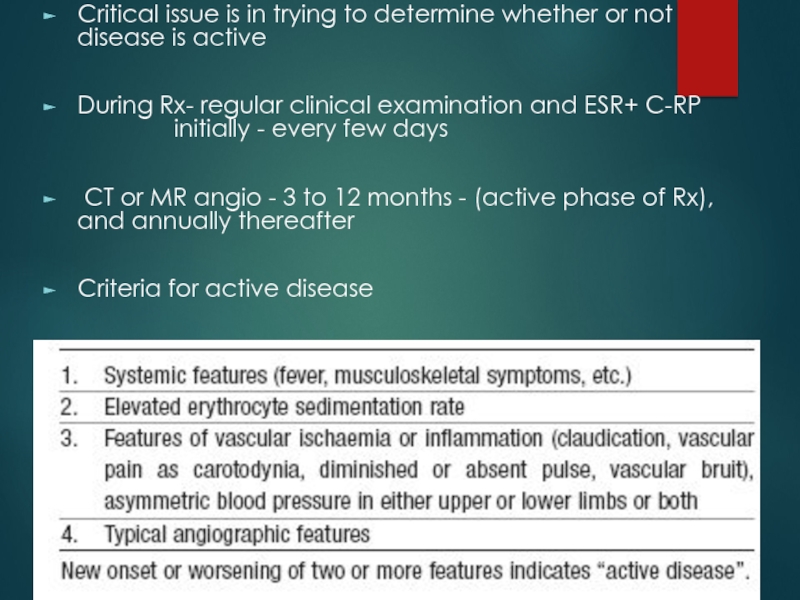
Слайд 31Critical issue is in trying to determine whether or not
disease is active
During Rx- regular clinical examination and ESR+ C-RP
initially - every few daysCT or MR angio - 3 to 12 months - (active phase of Rx), and annually thereafter
Criteria for active disease
Слайд 32
chronic phase- persistent inflammation
steroids should be
continued –
of s.C-RP and 20 mm/h of ESRСлайд 33Surgical treatment
HTN with critical RAS
Extremity claudication limiting daily activities
Cerebrovascular ischaemia
or critical stenoses of ≥3 cerebral vessels
Moderate AR
Cardiac ischaemia with
confirmed coronary involvement Aneurysms
Recommended at quiescent state-avoids compli
(restenosis, anastamotic failure, thrombosis, haemorrhage, & infection)
Слайд 34Surgical techniques
Carry high morbidity & mortality
Steno /aneurysm -anastomotic points
Progressive
nature of TA
Diffuse nature of TA
Слайд 35Renal artery involvement
Best treated by PTA
Stent placement following PTA
Ostial lesions
Long
segment lesions
Incomplete relief of stenoses
Dissection
Слайд 37Renal PTA - 33 stenoses (20 pts)
Indi-sev HTN,angio 70%
stenosis with pr grad 20mm,
nl-ESRTech success -28 lesions (85%) clin success-14(82%)
Failures - Coexistent abd Ao disease & tight, prox RAS
Tech diffi - tough, noncompliant stenoses, difficult to cross & resisted repeated, prolonged balloon inflations - backache & ↓SBP during balloon inflation
Follow-up –mean (8/12) -restenosis in 6 (21%)
Renal PTA in TA -tech difficulties; Short-term results - good, Complication rate-acceptable
Sharma s et al, AIIMS
Am J Roentgenol. 1992 Feb;158(2):417-22
Слайд 38Aortoarteritic lesions
Balloon dilation
safe & reasonably effective
Can be performed repeatedly
without any added risks
Balloon dilation diff from atherosclerotic lesions
Minimal
intimal involvement –permits easy wiring and balloon crossingResistance to dilation – high fibrotic element in the stenotic lesion
restenosis> frequent in TA - diffuse and long stenotic lesions
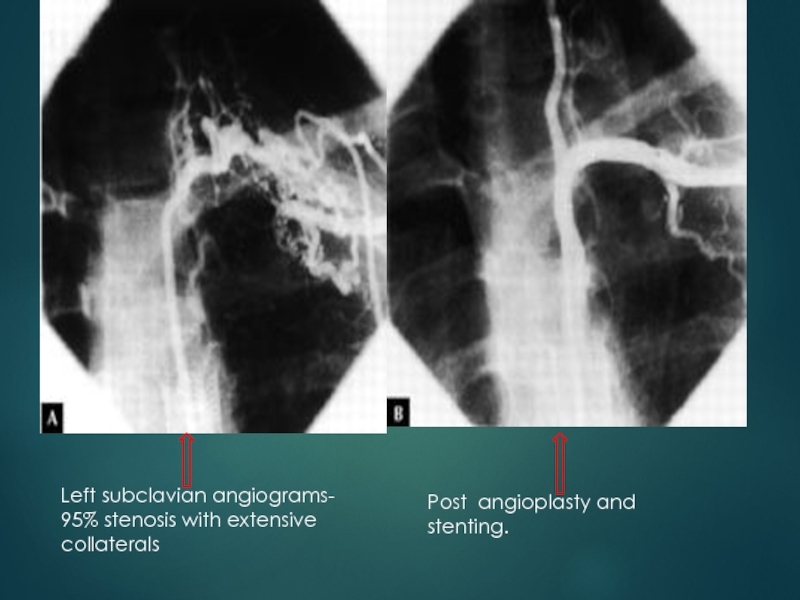
Слайд 39Left subclavian angiograms- 95% stenosis with extensive collaterals
Post angioplasty
and stenting.
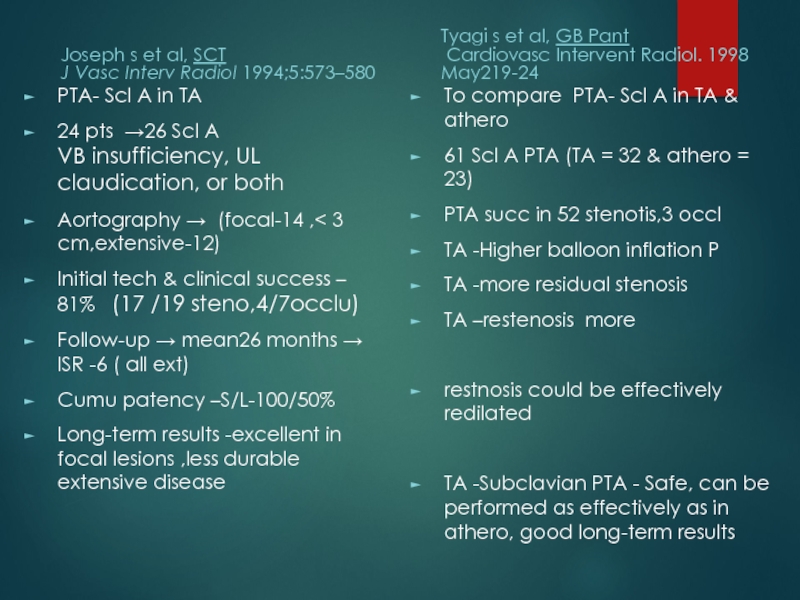
Слайд 40Joseph s et al, SCT
J Vasc Interv Radiol 1994;5:573–580
PTA- Scl
A in TA
24 pts →26 Scl A
VB insufficiency, UL claudication, or bothAortography → (focal-14 ,< 3 cm,extensive-12)
Initial tech & clinical success – 81% (17 /19 steno,4/7occlu)
Follow-up → mean26 months → ISR -6 ( all ext)
Cumu patency –S/L-100/50%
Long-term results -excellent in focal lesions ,less durable extensive disease
Tyagi s et al, GB Pant
Cardiovasc Intervent Radiol. 1998 May219-24
To compare PTA- Scl A in TA & athero
61 Scl A PTA (TA = 32 & athero = 23)
PTA succ in 52 stenotis,3 occl
TA -Higher balloon inflation P
TA -more residual stenosis
TA –restenosis more
restnosis could be effectively redilated
TA -Subclavian PTA - Safe, can be performed as effectively as in athero, good long-term results
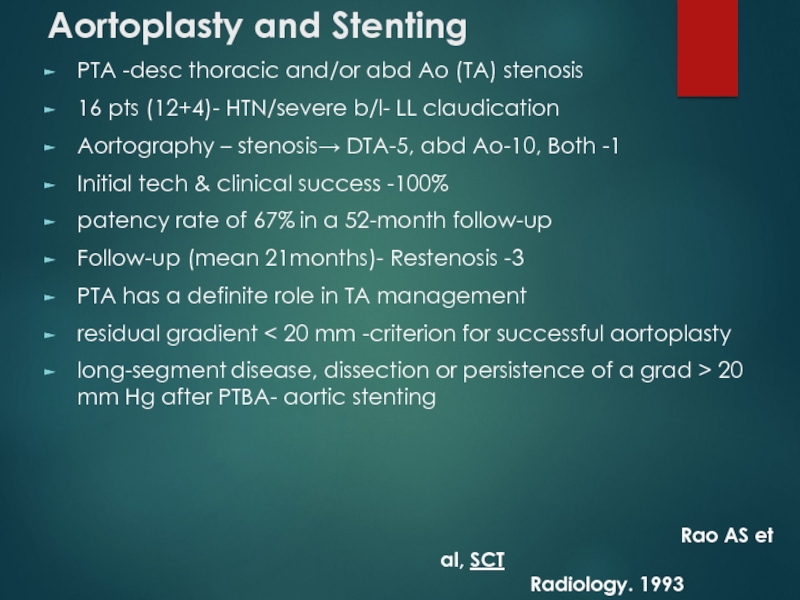
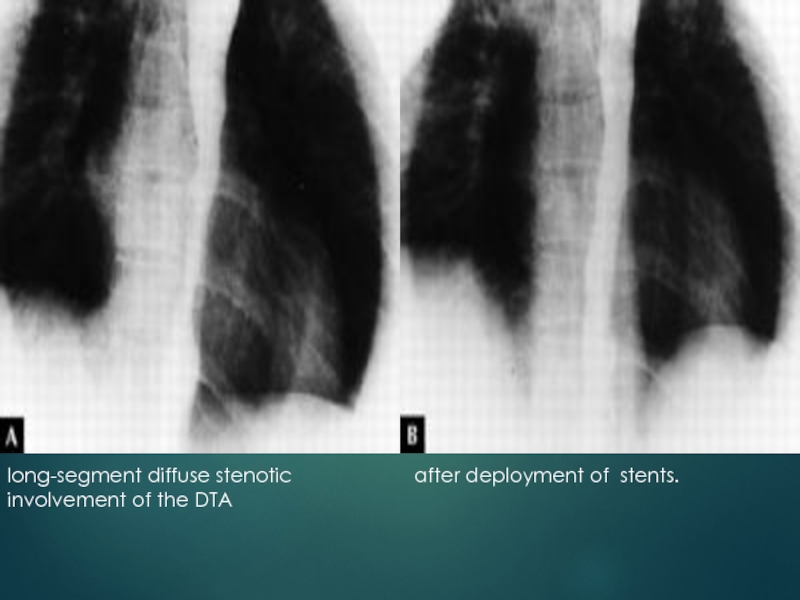
Слайд 41Aortoplasty and Stenting
PTA -desc thoracic and/or abd Ao (TA) stenosis
16
pts (12+4)- HTN/severe b/l- LL claudication
Aortography – stenosis→ DTA-5, abd
Ao-10, Both -1Initial tech & clinical success -100%
patency rate of 67% in a 52-month follow-up
Follow-up (mean 21months)- Restenosis -3
PTA has a definite role in TA management
residual gradient < 20 mm -criterion for successful aortoplasty
long-segment disease, dissection or persistence of a grad > 20 mm Hg after PTBA- aortic stenting
Rao AS et al, SCT
Radiology. 1993 Oct;189(1):173-9
Слайд 43Treatment for cor A occulusion in TA
Surgery (CABG)- often
not indicated
・IMA can’t be used often
occlu of Innomi A /
Scl Acalcification of aorta
High incidence of restenosis:36%
Angioplasty(PTCA)
・alternative to surgery
Very high incidence of restenosis:78%
DES-effectiveness ?
Слайд 44 Percutaneous Management of Aneurysmal Lesions
Aneurysmal dilatation- isolation or
together with stenotic lesions
fusiform or saccular
one of the
major complications related to the prognosis in TAIncidence of aneurysm rupture -low
Management - mainly surgical.
Covered stent-grafts may be useful

![TAKAYASU’S ARTERITIS [18F]fluorodeoxyglucose PET for diagnosing Takayasu’s arteritiscommon [18F]FDG uptake pattern TA [18F]fluorodeoxyglucose PET for diagnosing Takayasu’s arteritiscommon [18F]FDG uptake pattern TA](/img/thumbs/f85acfe7eb1f2faa294cc7851931f52c-800x.jpg)