Слайд 2General characteristic of infectious diseases
with fecal-oral mechanism of transmission
specific localization of the causative agent in intestine (small or
large, rectum, mesenterium)
removing the agent with feces or vomiting mass
can penetrate into a susceptible organism by next ways of transmission (watery, alimentary, contact-household)
various factors of transmission (foodstuff, water, hands, insects, toys, soil)
in intestine causative agent can be: in the lumen of intestine, intestinal epithelium, mucous membrane, lymphatic tissue of intestine
causative agent can constantly be in intestine (cholera, dysentery, some helminthic invasion) or temporarily,
penetration from intestine in blood and other tissue (ascariasis, amebiasis, strongyloidiasis, trichinosis, echinococcosis)
Слайд 3 - Morbidity of intestinal infection is the highest:
- in warm and/or rainy period of year
(in moderate climatic zones is more often registered during
summer or autumn);
- in countries with low socio-economic level of development;
- among people of risk-groups:
- age - children and the elderly,
- chronic GIT-pathology - patients with
gastritis, duodenitis, peptic ulcer, cholecystitis;
- profession - sanitary workers, plumbers, teachers,
medical personal;
- occupation – fishermen, water-rescuers,
veterinarians, animal trainers
Слайд 4Definition
Typhoid fever – is an acute intestinal anthroponotic infection with
fecal - oral mechanism of transmission caused by S. typhi,
characterized by lesions of lymphatic apparatus of the small intestine and bacteremia, development of severe intoxication, hepatosplenomegaly and roseola rash.
The name of the disease came from the word «typhos», meaning «smoke» or «fog».
The disease has been referred to by various names, often associated with symptoms, such as gastric fever, enteric fever, abdominal typhus, infantile remittant fever, slow fever, nervous fever, and pathogenic fever.
Слайд 5 History
The first data on typhoid fever obtained from
the writings of the ancient historian Thucydides, who suffered this
disease.
In 430 BC in Athens lost one-third of the population of Athens, including their leader Pericles.
- Some historians believe that English colony of Jamestown, Virginia, died from typhoid. Typhoid fever killed more than 6000 settlers in the New World between 1607 and 1624.
- During the American Civil War 81 360 Union soldiers died of typhoid or dysentery, more than died of battle wounds.
Слайд 6 The most notorious carrier of
typhoid fever was Mary Mallon, also known as Typhoid Mary.
In 1907, she became the first carrier in the United States to be identified and traced. She was a cook in New York who is closely associated with 53 cases and 3 deaths.
Public health authorities told Mary to give up working as a cook or have her gall bladder removed, as she had a chronic infection that kept her active as a carrier of the disease.
Mary quit her job, but returned later under a false name. She was detained and quarantined after another typhoid outbreak.
She died of pneumonia after 26 years in quarantine.
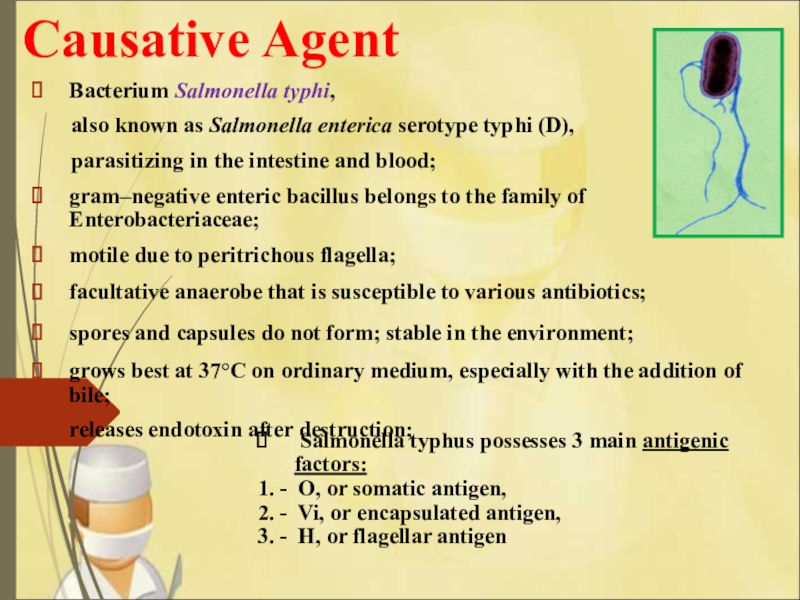
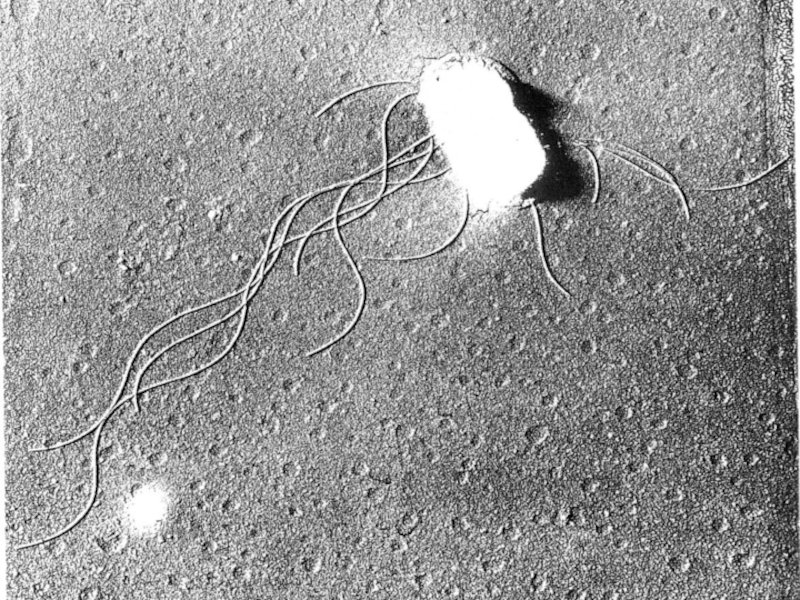
Слайд 7 Causative Agent
Bacterium Salmonella typhi,
also
known as Salmonella enterica serotype typhi (D),
parasitizing in the intestine and blood;
gram–negative enteric bacillus belongs to the family of Enterobacteriaceae;
motile due to peritrichous flagella;
facultative anaerobe that is susceptible to various antibiotics;
spores and capsules do not form; stable in the environment;
grows best at 37°C on ordinary medium, especially with the addition of bile;
releases endotoxin after destruction;
Salmonella typhus possesses 3 main antigenic factors:
1. - O, or somatic antigen,
2. - Vi, or encapsulated antigen,
3. - H, or flagellar antigen
Слайд 9Epidemiology
Source of infection: - bacilli- carrier:
the acute -
releases within 3 months, chronic – more than 6 months
(the most dangerous in epidemiological terms).
- patient discharges bacteria with feces, urine, saliva. (massive discharging starts from the 7th day of illness).
Mechanism of transmission: – fecal-oral implemented by – water, - food, - contact-household ways.
Sensitivity: - children, young people, elderly,
54% of typhoid fever cases involved males;
patients with immunodeficiency and chronic diseases of the gastrointestinal tract;
After the disease develops persistent immunity.
Characterized by seasonality (summer, autumn).
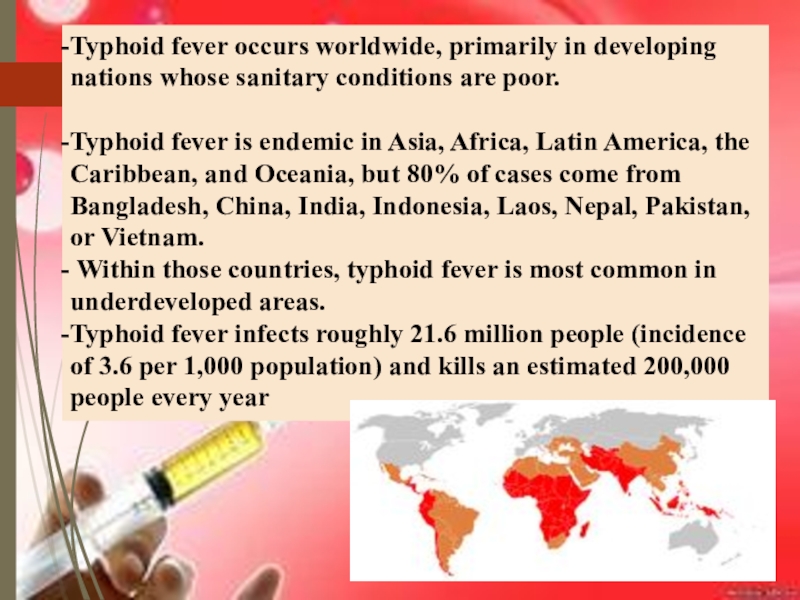
Слайд 10Typhoid fever occurs worldwide, primarily in developing nations whose sanitary
conditions are poor.
Typhoid fever is endemic in Asia, Africa,
Latin America, the Caribbean, and Oceania, but 80% of cases come from Bangladesh, China, India, Indonesia, Laos, Nepal, Pakistan, or Vietnam.
Within those countries, typhoid fever is most common in underdeveloped areas.
Typhoid fever infects roughly 21.6 million people (incidence of 3.6 per 1,000 population) and kills an estimated 200,000 people every year
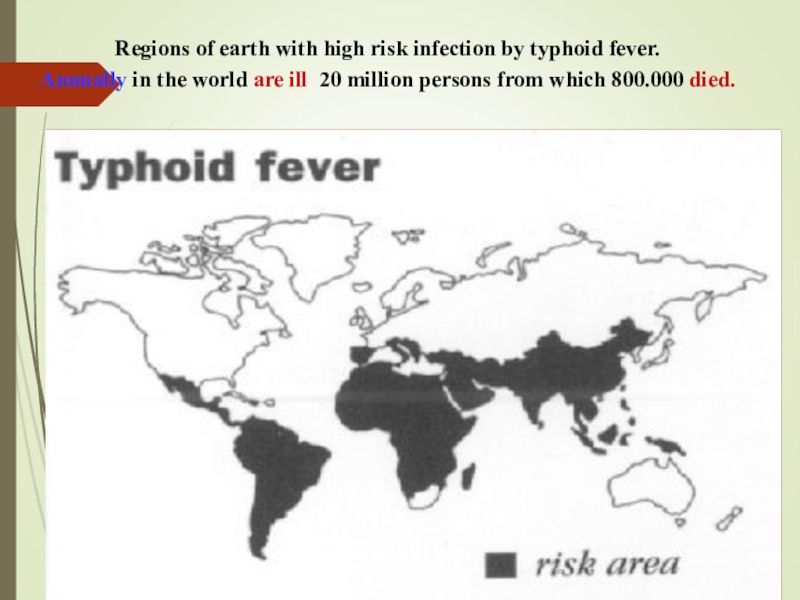
Слайд 11Regions of earth with high risk infection by typhoid fever.
Annually in the world are ill 20 million persons from
which 800.000 died.
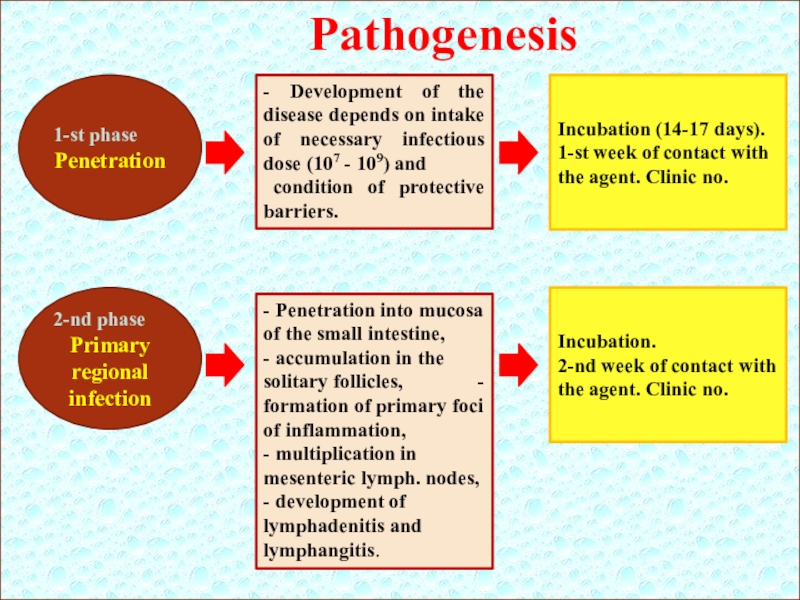
Слайд 12Pathogenesis
1-st phase
Penetration
- Development of the disease depends on intake of
necessary infectious dose (107 - 109) and
condition of protective
barriers.
Incubation (14-17 days).
1-st week of contact with the agent. Clinic no.
2-nd phase
Primary regional infection
- Penetration into mucosa of the small intestine, - accumulation in the solitary follicles, - formation of primary foci of inflammation,
- multiplication in mesenteric lymph. nodes,
- development of lymphadenitis and lymphangitis.
Incubation.
2-nd week of contact with the agent. Clinic no.
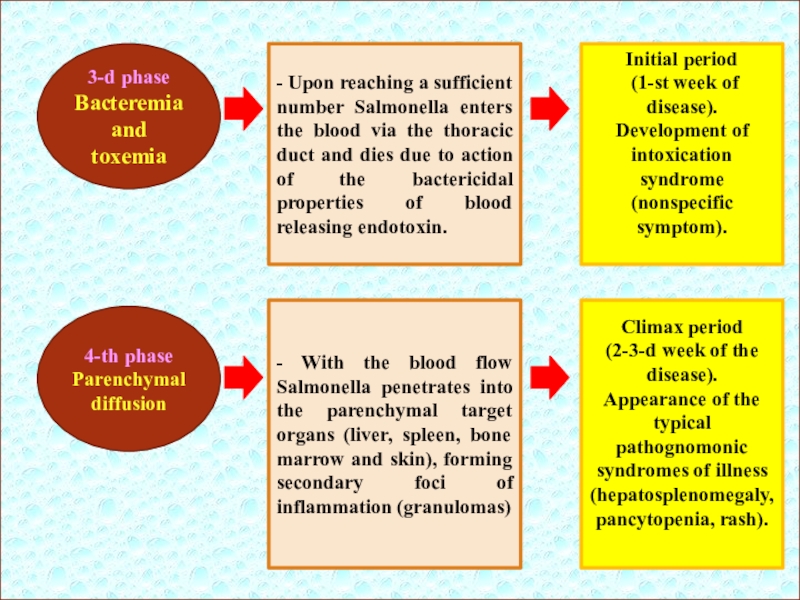
Слайд 133-d phase
Bacteremia and toxemia
4-th phase
Parenchymal diffusion
- Upon reaching a sufficient
number Salmonella enters the blood via the thoracic duct and
dies due to action of the bactericidal properties of blood releasing endotoxin.
- With the blood flow Salmonella penetrates into the parenchymal target organs (liver, spleen, bone marrow and skin), forming secondary foci of inflammation (granulomas)
Initial period
(1-st week of disease).
Development of intoxication syndrome (nonspecific symptom).
Climax period
(2-3-d week of the disease).
Appearance of the typical pathognomonic syndromes of illness (hepatosplenomegaly, pancytopenia, rash).
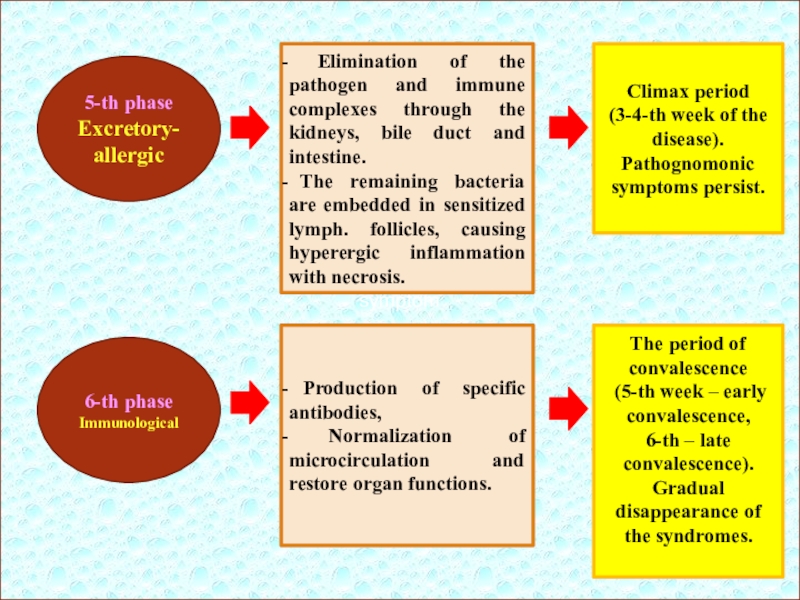
Слайд 14symptom
5-th phase Excretory- allergic
6-th phase Immunological
Elimination of the pathogen
and immune complexes through the kidneys, bile duct and intestine.
The remaining bacteria are embedded in sensitized lymph. follicles, causing hyperergic inflammation with necrosis.
Production of specific antibodies,
Normalization of microcirculation and restore organ functions.
Climax period
(3-4-th week of the disease).
Pathognomonic symptoms persist.
The period of convalescence
(5-th week – early convalescence,
6-th – late convalescence). Gradual disappearance of the syndromes.
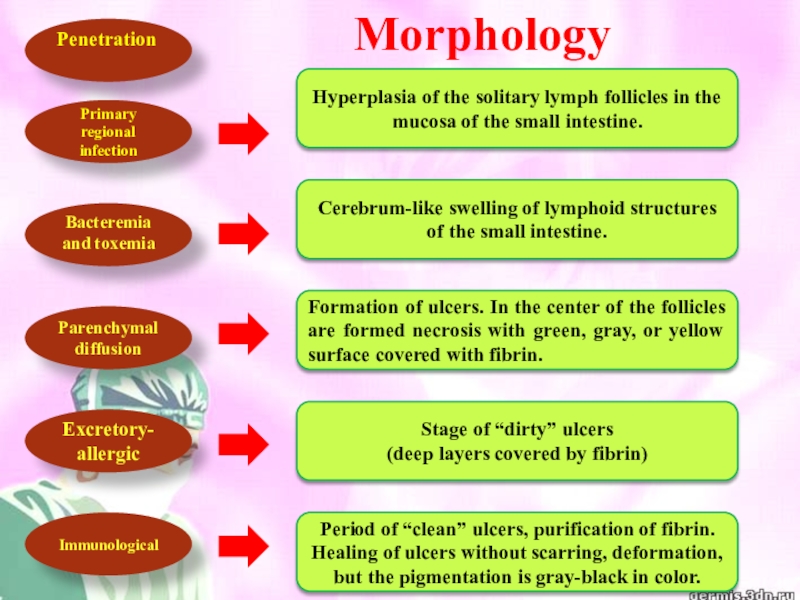
Слайд 15Morphology
Penetration
Bacteremia and toxemia
Parenchymal diffusion
Primary regional infection
Excretory- allergic
Immunological
Hyperplasia of the solitary
lymph follicles in the mucosa of the small intestine.
Cerebrum-like swelling
of lymphoid structures of the small intestine.
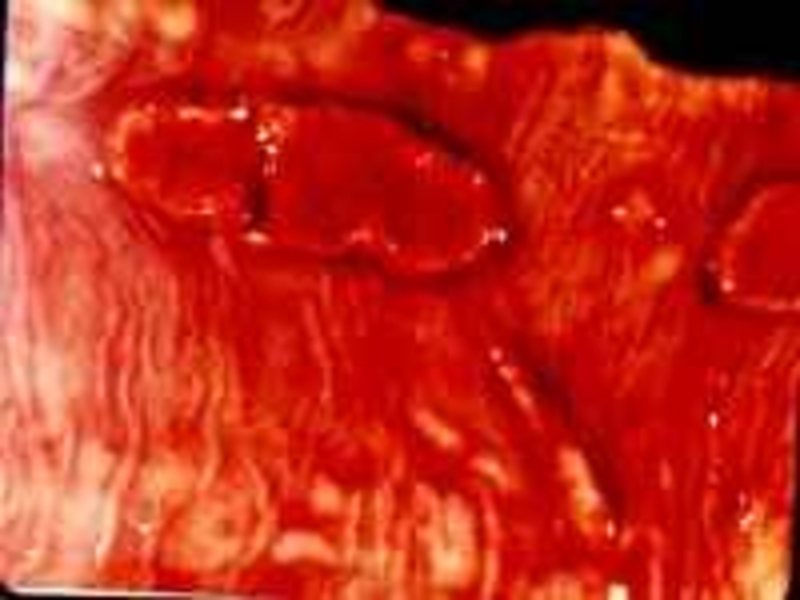
Formation of ulcers. In the center of the follicles are formed necrosis with green, gray, or yellow surface covered with fibrin.
Stage of “dirty” ulcers
(deep layers covered by fibrin)
Period of “clean” ulcers, purification of fibrin.
Healing of ulcers without scarring, deformation, but the pigmentation is gray-black in color.
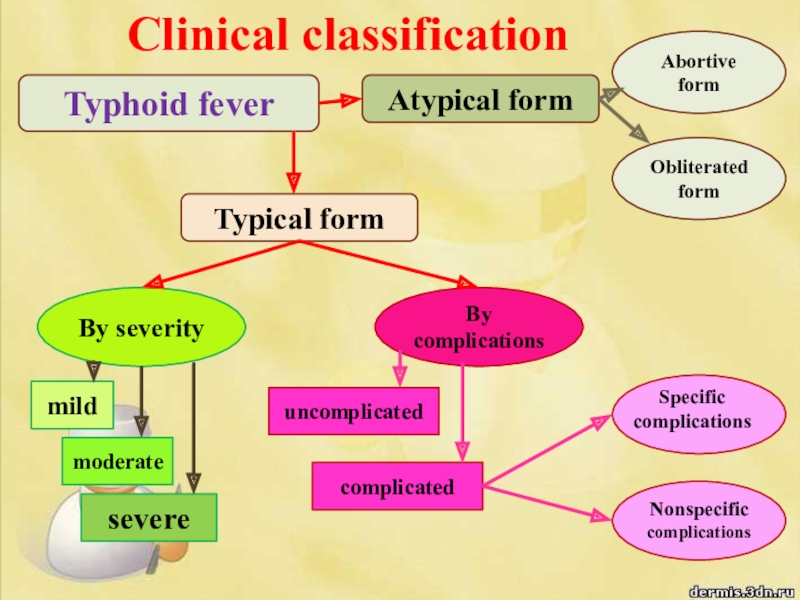
Слайд 19Clinical classification
Typhoid fever
Typical form
Atypical form
By severity
By complications
Obliterated form
Abortive form
moderate
mild
severe
uncomplicated
complicated
Nonspecific
complications
Specific
complications
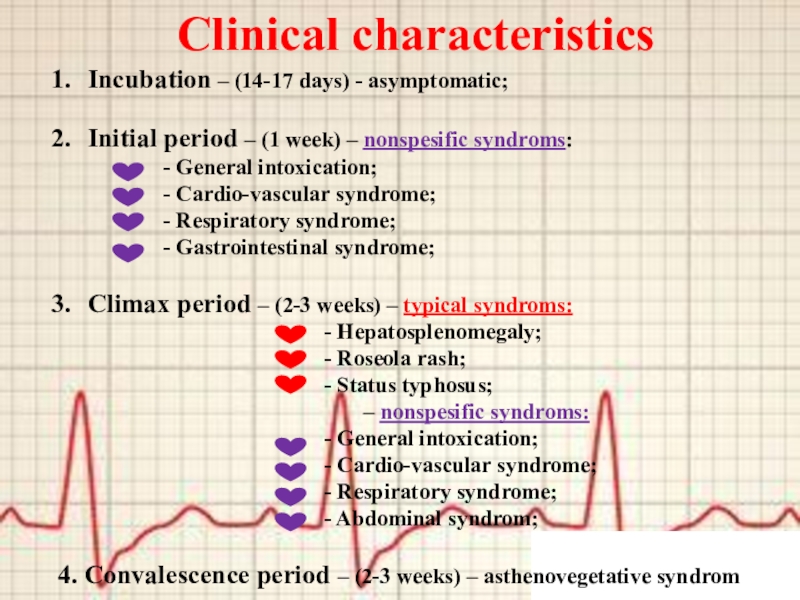
Слайд 20Clinical characteristics
Incubation – (14-17 days) - asymptomatic;
Initial period – (1
week) – nonspesific syndroms:
- General intoxication;
- Cardio-vascular syndrome;
- Respiratory syndrome;
- Gastrointestinal syndrome;
Climax period – (2-3 weeks) – typical syndroms:
- Hepatosplenomegaly;
- Roseola rash;
- Status typhosus;
– nonspesific syndroms:
- General intoxication;
- Cardio-vascular syndrome;
- Respiratory syndrome;
- Abdominal syndrom;
4. Convalescence period – (2-3 weeks) – asthenovegetative syndrom
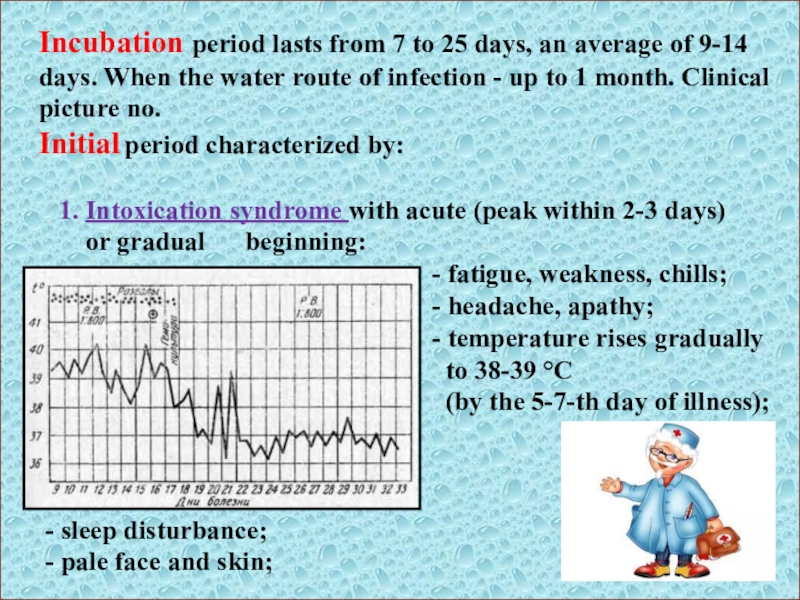
Слайд 21Incubation period lasts from 7 to 25 days, an average
of 9-14 days. When the water route of infection -
up to 1 month. Clinical picture no.
Initial period characterized by:
1. Intoxication syndrome with acute (peak within 2-3 days)
or gradual beginning:
- fatigue, weakness, chills;
- headache, apathy;
- temperature rises gradually
to 38-39 °C
(by the 5-7-th day of illness);
- sleep disturbance;
- pale face and skin;
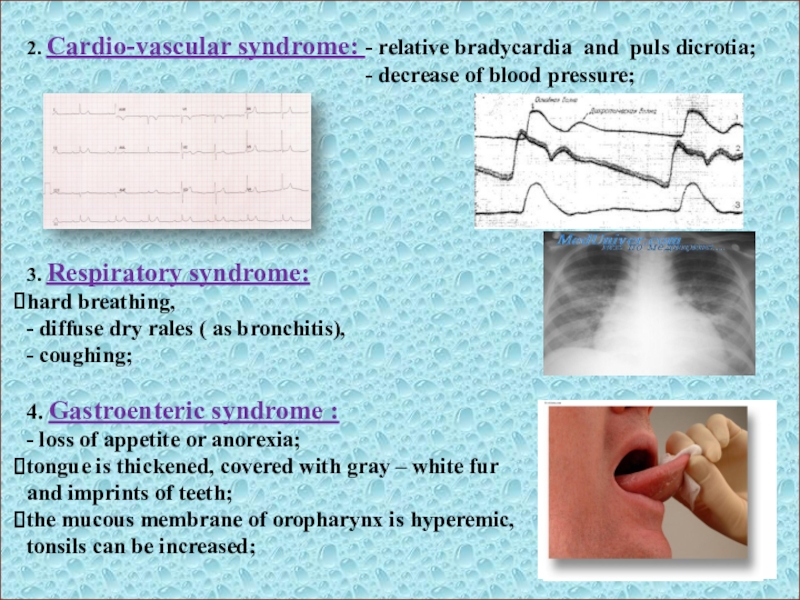
Слайд 222. Cardio-vascular syndrome: - relative bradycardia and puls dicrotia;
- decrease of blood pressure;
3. Respiratory syndrome:
hard breathing,
- diffuse dry rales ( as bronchitis),
- coughing;
4. Gastroenteric syndrome :
- loss of appetite or anorexia;
tongue is thickened, covered with gray – white fur
and imprints of teeth;
the mucous membrane of oropharynx is hyperemic,
tonsils can be increased;
Слайд 23 meteorism, abdomen distended, rumbling,
painful along the small intestine
at palpation ( ileitis);
- at percussion – is
a shortening of sound
in the right iliac area
(“+” Padalka – sign due to hyperplasia of the mesenteric lymph. nodes),
within 2-4 days of disease may be seen
diarrhea (stool is stinking with a sour
smell, up to 2 – 4 t/day, foamy, liquid,
greenish like pea soup.
enlargement of the spleen and liver
(at the end of 1st week),
Слайд 24Climax period
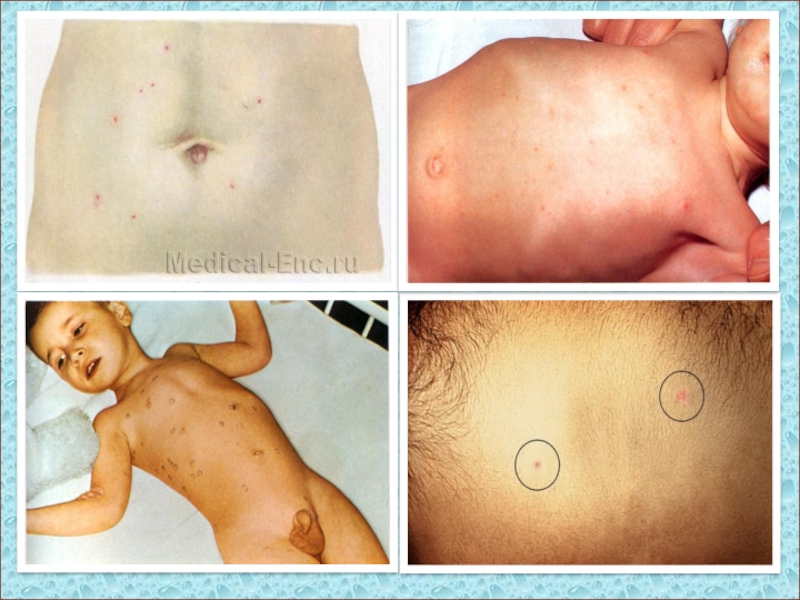
(begins with the appearance of the rash on
the 2-d week of the disease and lasts an average
of 2-3 weeks)
Intoxication syndrome:
- headache is the most expressed, not relieved by drugs;
- insomnia, drowsiness;
- chills, weakness;
- photophobia;
- status typhosus - delayed mental reactions,
sometimes prostration, stupor condition
and coma, tremor of fingers, chin and
tongue;
- apathy, adynamia;
- temperature is febrile or hectic (39-40ºC), increases every day
for 1-2ºC during the week and lasts for about 2 weeks.
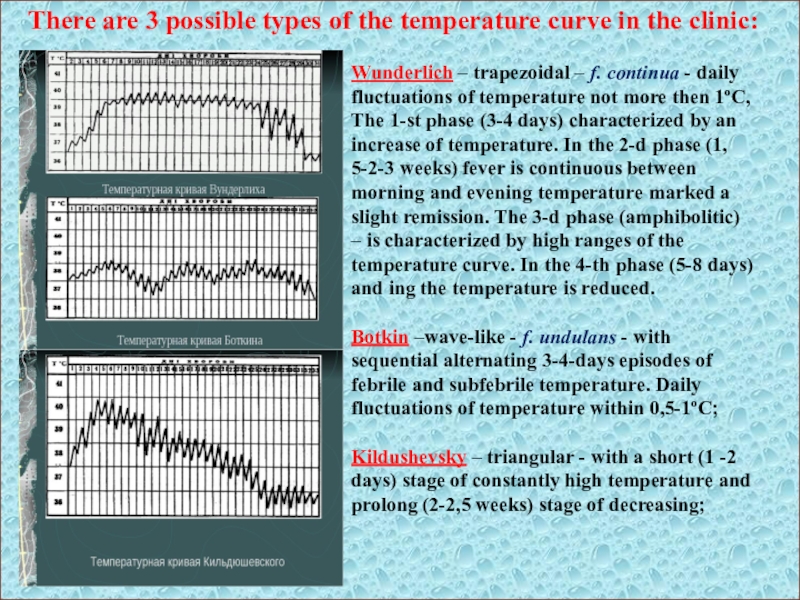
Слайд 26Wunderlich – trapezoidal – f. continua - daily fluctuations of
temperature not more then 1ºC,
The 1-st phase (3-4 days)
characterized by an increase of temperature. In the 2-d phase (1, 5-2-3 weeks) fever is continuous between morning and evening temperature marked a slight remission. The 3-d phase (amphibolitic) – is characterized by high ranges of the temperature curve. In the 4-th phase (5-8 days) and ing the temperature is reduced.
Botkin –wave-like - f. undulans - with sequential alternating 3-4-days episodes of febrile and subfebrile temperature. Daily fluctuations of temperature within 0,5-1ºC;
Kildushevsky – triangular - with a short (1 -2 days) stage of constantly high temperature and prolong (2-2,5 weeks) stage of decreasing;
There are 3 possible types of the temperature curve in the clinic:
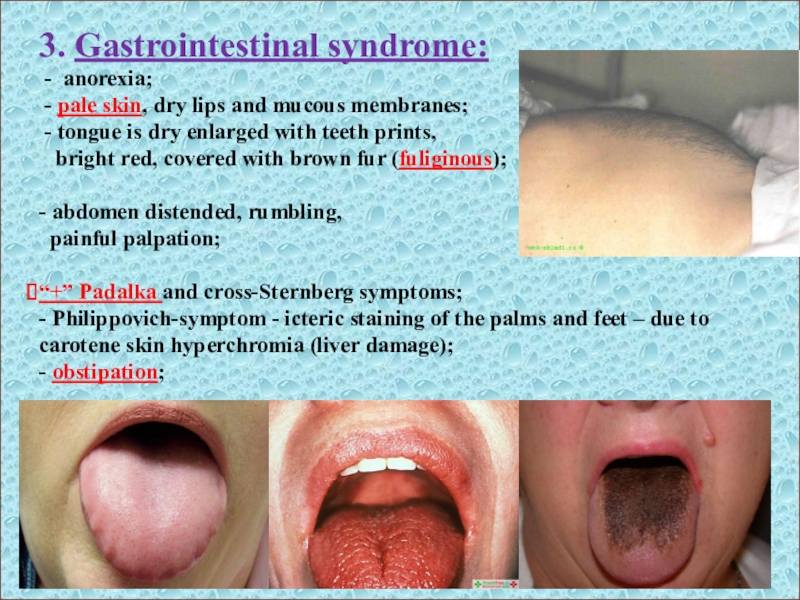
Слайд 293. Gastrointestinal syndrome:
- anorexia;
- pale skin, dry lips
and mucous membranes;
- tongue is dry enlarged with
teeth prints,
bright red, covered with brown fur (fuliginous);
- abdomen distended, rumbling,
painful palpation;
“+” Padalka and cross-Sternberg symptoms;
- Philippovich-symptom - icteric staining of the palms and feet – due to carotene skin hyperchromia (liver damage);
- obstipation;
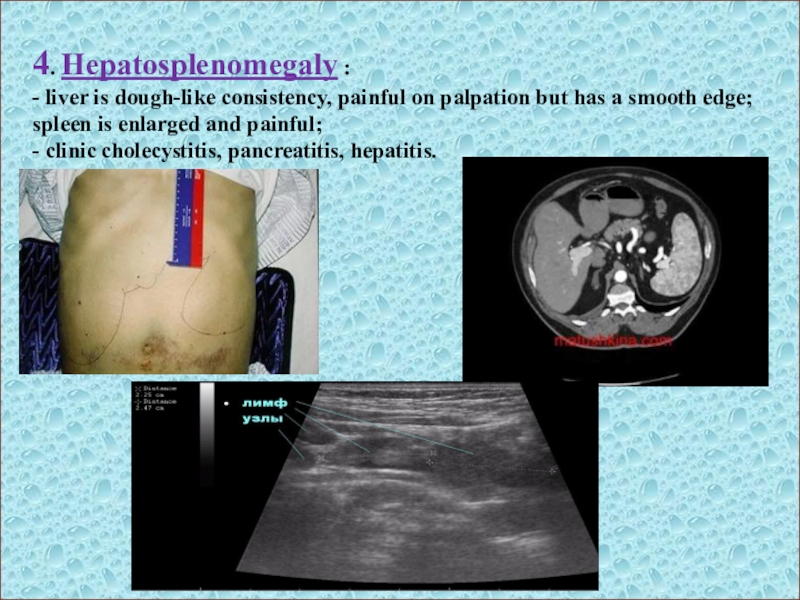
Слайд 304. Hepatosplenomegaly :
- liver is dough-like consistency, painful on palpation
but has a smooth edge; spleen is enlarged and painful;
-
clinic cholecystitis, pancreatitis, hepatitis.
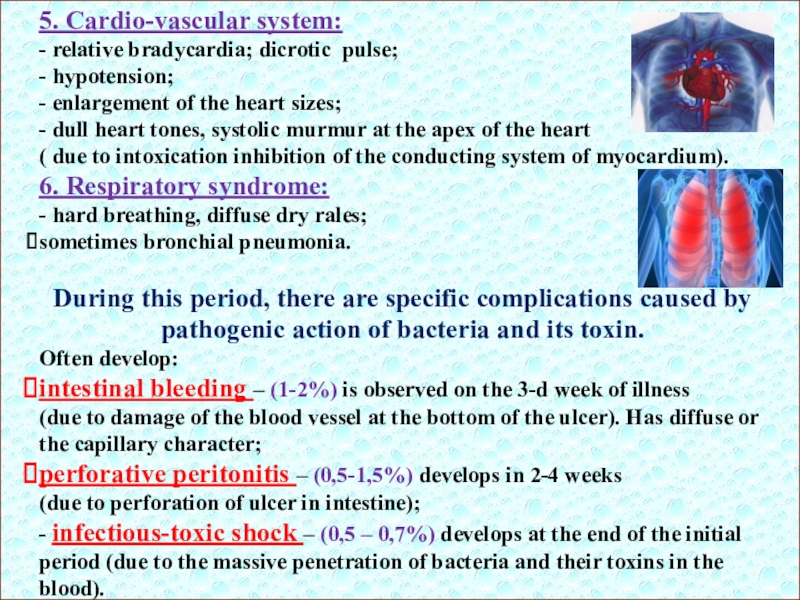
Слайд 315. Cardio-vascular system:
- relative bradycardia; dicrotic pulse;
- hypotension;
- enlargement of
the heart sizes;
- dull heart tones, systolic murmur at the
apex of the heart
( due to intoxication inhibition of the conducting system of myocardium).
6. Respiratory syndrome:
- hard breathing, diffuse dry rales;
sometimes bronchial pneumonia.
During this period, there are specific complications caused by pathogenic action of bacteria and its toxin.
Often develop:
intestinal bleeding – (1-2%) is observed on the 3-d week of illness
(due to damage of the blood vessel at the bottom of the ulcer). Has diffuse or
the capillary character;
perforative peritonitis – (0,5-1,5%) develops in 2-4 weeks
(due to perforation of ulcer in intestine);
- infectious-toxic shock – (0,5 – 0,7%) develops at the end of the initial period (due to the massive penetration of bacteria and their toxins in the blood).
Слайд 32Laboratory diagnostics
Specific studies (allow to confirm the diagnosis):
Bacteriologic analysis -
the main method of laboratory
diagnosis
of typho-paratyphoid diseases, allows to select and
determine the type of pathogen.
Bacteriological research is subjected to blood (52—78%), urine (0,7—2,1%),
feces (11—19%) , bile and scraping of the rash, bone marrow, pus, sputum.
The time of selection of the material:
- 1-2-d week – the blood; - 2-3-d week – the urine, stool;
- during the whole of the disease – the duodenal contents.
Blood should be taken from the first days of sickness and whole period of the fever in volume of 5-10ml on a nutrient medium containing a bile
(Rappoport-medium).
The ratio between the blood and nutrition – 1:10
(because the blood has antibacterial properties
destroys the microbe).
Stool-, bile-, urin-culture can be obtained
on the nutrient medium called Ploskirev-medium.
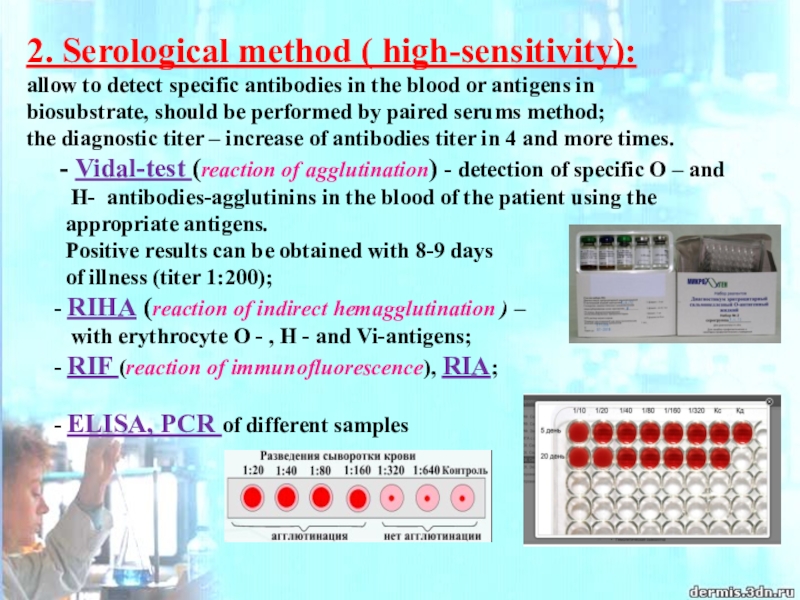
Слайд 332. Serological method ( high-sensitivity):
allow to detect specific antibodies in
the blood or antigens in
biosubstrate, should be performed by
paired serums method;
the diagnostic titer – increase of antibodies titer in 4 and more times.
- Vidal-test (reaction of agglutination) - detection of specific O – and
H- antibodies-agglutinins in the blood of the patient using the
appropriate antigens.
Positive results can be obtained with 8-9 days
of illness (titer 1:200);
- RIHA (reaction of indirect hemagglutination ) –
with erythrocyte O - , H - and Vi-antigens;
- RIF (reaction of immunofluorescence), RIA;
- ELISA, PCR of different samples
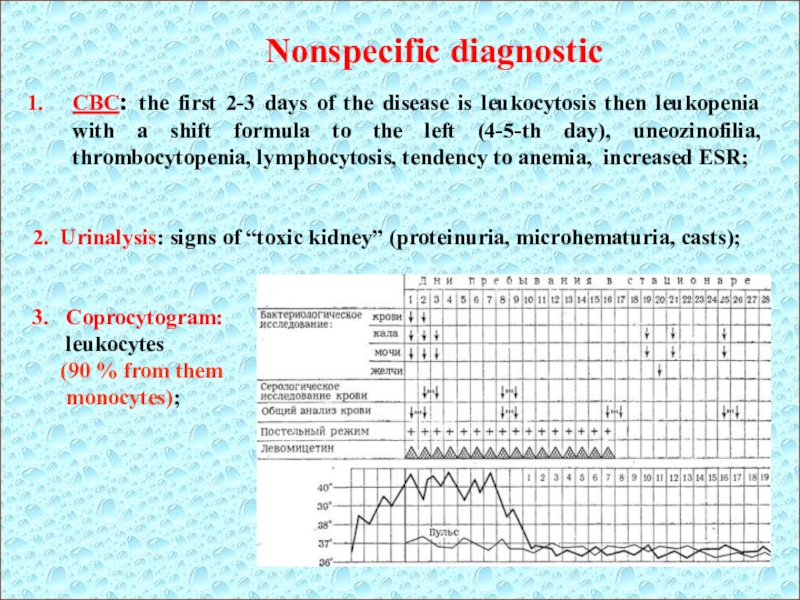
Слайд 34Nonspecific diagnostic
CBC: the first 2-3 days of the disease is
leukocytosis then leukopenia with a shift formula to the left
(4-5-th day), uneozinofilia, thrombocytopenia, lymphocytosis, tendency to anemia, increased ESR;
2. Urinalysis: signs of “toxic kidney” (proteinuria, microhematuria, casts);
3. Coprocytogram:
leukocytes
(90 % from them
monocytes);
Слайд 35Additional methods of diagnostics
1. Chest x-ray – to detect focal
changes in lungs (pneumonia).
2. Radiography of the abdomen - if
you suspect an intestinal perforation.
3. ECG, monitor heart activity - to diagnose myocarditis.
4. Spinal puncture - is performed when a positive meningeal signs,
suspicion for the development of meningitis.
5. Ultrasound of the abdomen - helps to determine the size of the liver and
spleen.
Слайд 36Diagnostic criteria for typhoid fever
epidemiological anamnesis (contact with the sick
person or carrier,
using of unboiled water and contaminated
food);
- gradual onset with a classic temperature curve;
chills and sweating, hot dry pale skin;
bloating (mainly in the classic version);
- tenderness on palpation of the abdomen and positive Padalka-symptom;
presence of watery stool a yellowish or greenish color without
pathological admixtures, transforming into constipation;
- tongue with prints of teeth on lateral surfaces;
- enlarged liver and spleen;
- symptoms of intoxication (headache, sleep disturbance and weakness);
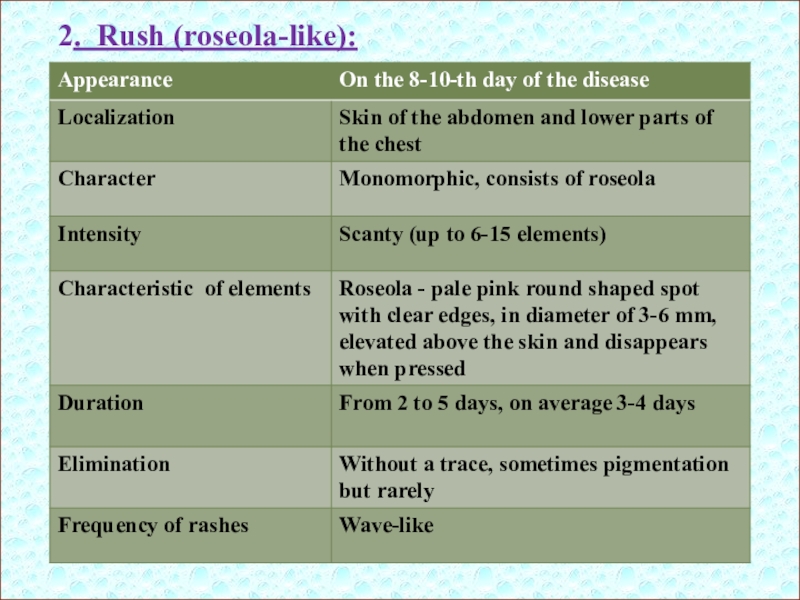
rash (roseola-like) on the skin of the abdomen and thorax on
the 8-9th day of illness;
- relative bradycardia.
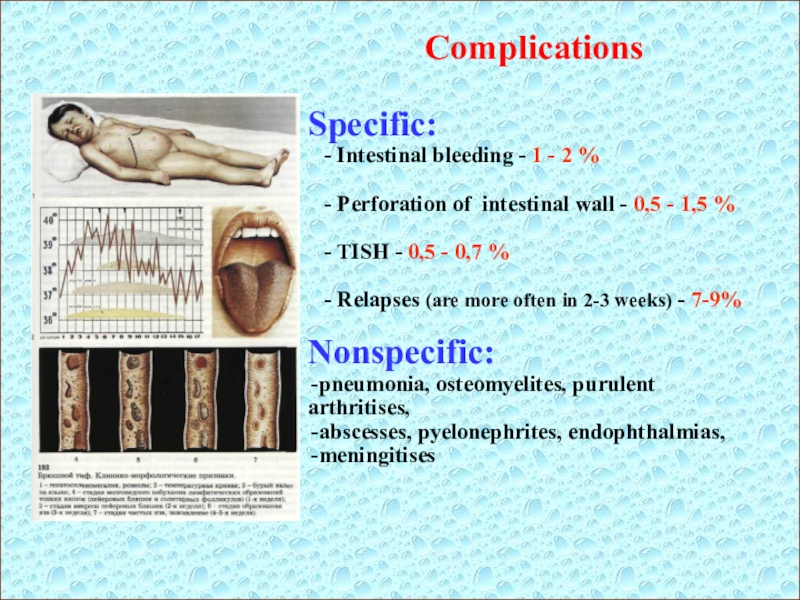
Слайд 37Complications
Specific:
- Intestinal bleeding - 1 - 2
%
- Perforation of intestinal wall - 0,5 -
1,5 %
- TISH - 0,5 - 0,7 %
- Relapses (are more often in 2-3 weeks) - 7-9%
Nonspecific:
pneumonia, osteomyelites, purulent arthritises,
abscesses, pyelonephrites, endophthalmias,
meningitises
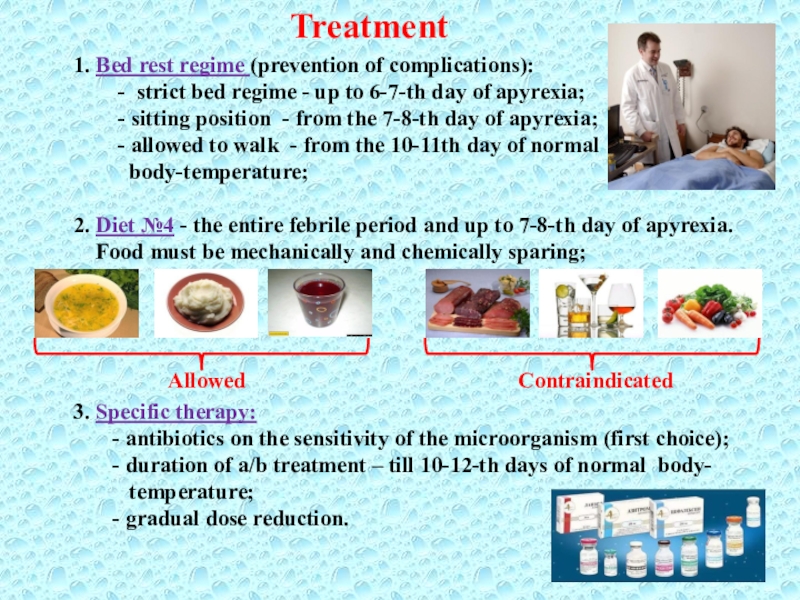
Слайд 38Treatment
1. Bed rest regime (prevention of complications):
- strict bed regime - up to 6-7-th day of
apyrexia;
- sitting position - from the 7-8-th day of apyrexia;
- allowed to walk - from the 10-11th day of normal
body-temperature;
2. Diet №4 - the entire febrile period and up to 7-8-th day of apyrexia.
Food must be mechanically and chemically sparing;
3. Specific therapy:
- antibiotics on the sensitivity of the microorganism (first choice);
- duration of a/b treatment – till 10-12-th days of normal body-
temperature;
- gradual dose reduction.
Allowed Contraindicated
Слайд 39Specific therapy
1. Chloramphenicol (first choice a/b):
- per os
- in mild and moderate severity (without vomiting)
0,5-1,0 g × 4 t/d (daily dose - 2-4g);
- parenteral (i/m or i/v) – in severe cases and vomiting
1-2 g × 2 t/d (daily dose - 2-4g);
On the 2nd day of normalization of body temperature the dose is reduced gradually and should be given per os in 0,5 g × 4 t/d 10 days of apyrexia.
2. Ampicillinum:
(effect is slower than of chloramphenicol, but relapse is less often)
- per os or parenteral (i/m) – 1-1,5 g × 4 t/d;
3. Ciprofloxacin:
- per os - 0,5 g × 4 t/d;
4. Trimethaprim – sulphamethoxazole:
- per os - 0,960 g × 2 t/d;
5. Alternative remedies: ceftriaxone - 2 g/day, ofloxacin - 0,8 g/day,
azitromicin - 0,25-0,5 g/day, cefoxim - 0,4 g/day.
For the treatment of a carrier:
- ampicillinum in a dose 40-50 mg/kg per os 4 t/d within 4 - 6 weeks
(efficiency 80 %).
Слайд 40 Nonspesific (supporting) therapy:
- desintoxication therapy (PO or
IV);
- sufficient hydration (PO or IV);
-
hemostatic therapy (intestinal bleeding);
- glucocorticoids (ТISH);
- antioxidants;
- antiferment drugs;
- probiotics, eubiotics.
Symptomatic therapy:
- analgetics, antipyretics, antiemetics;
Rules of discharging the patient out from the hospital:
Discharge the patient from the hospital is possible on 21-st day of normal
temperature, but not before the 4-th week of illness.
1. Clinical recovery;
2. 2 negative copro- and urine-cultures (5, 10 day of normal temperature);
4. 1 negative bile-culture (12-14-th day of normal temperature)
Слайд 41 Prophylaxis:
- immunity after T.F. is often intensive but the
relapse appears in 20-25 %
The vaccines do not form
a complete protection, but should be used:
- at close family contact with patient or carrier;
- during outbreaks of T.F.
- before visiting the areas endemic on T.F.
Basic preventive measures:
- keeping of rules of personal hygiene;
- control of cooking and storage of nutrition;
- registration, treatment and discharge from work carriers of S.t;
- careful clearing of the drynking water;
- desinfection of the sewers;
- constant medical control for decreed risk groups in population