Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
acquired heart defects
Содержание
- 1. acquired heart defects
- 2. Слайд 2
- 3. Valvular heart disease is any
- 4. MITRAL VALVE STENOSISMitral stenosis (MS) refers to
- 5. ETIOLOGYPrimarily a result of rheumatic fever.Infective endocarditis.Systemic
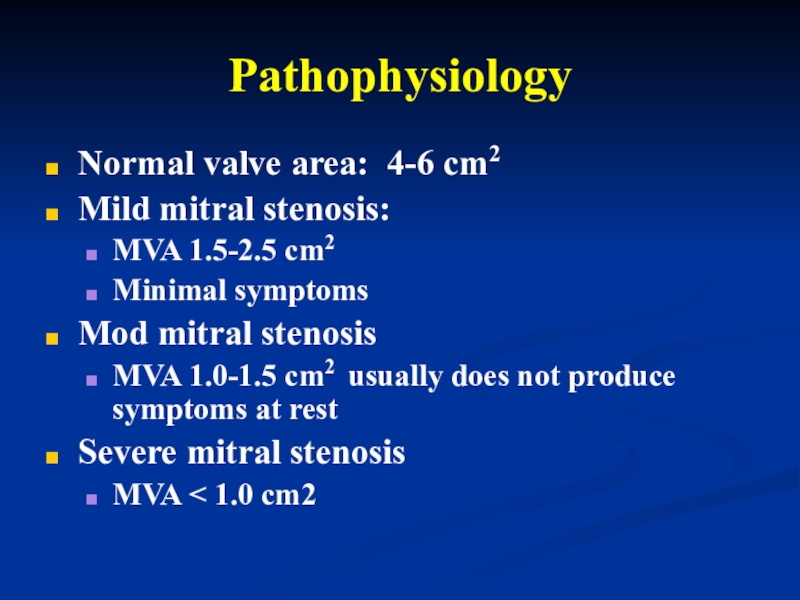
- 6. PathophysiologyNormal valve area: 4-6 cm2Mild mitral stenosis:
- 7. Pathophysiology Patients with MS typically present
- 8. Pathophysiology Elevated left atrial pressures lead
- 9. Слайд 9
- 10. Symptoms and singsDyspnea , cough.Left sided failure.Hemoptysis.Palpitation, Atrial arrhythmias.Cardialgia.Systemic embolism.Right sided failure (Hepatic Congestion, Edema).
- 11. ObjectivelyAcrocyanosis , facies mitralis.Palpation - «purring thrill»
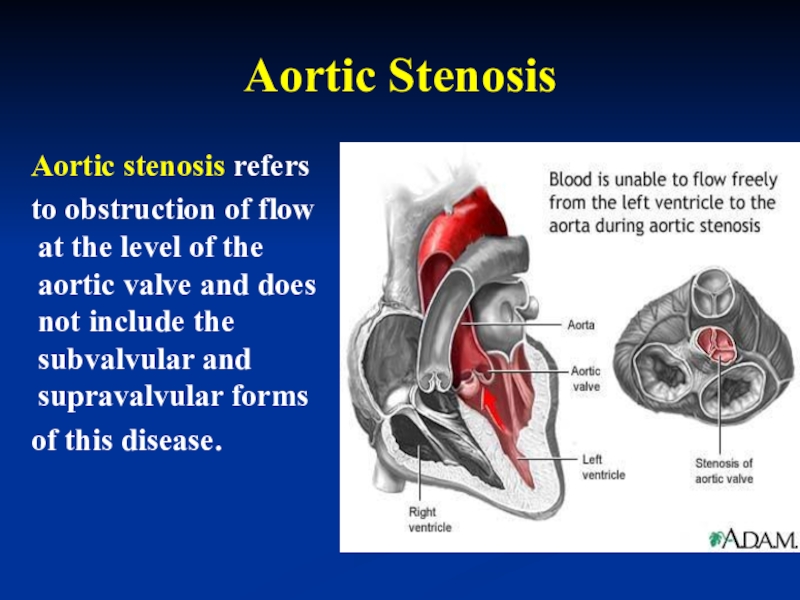
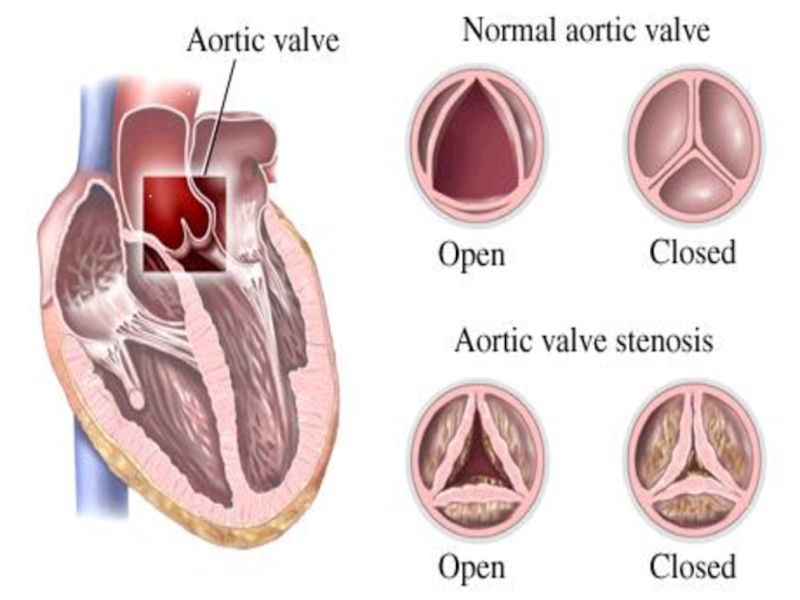
- 12. Слайд 12
- 13. Auscultation:The auscultatory findings characteristic of
- 14. Auscultation:3. The second heart sound is
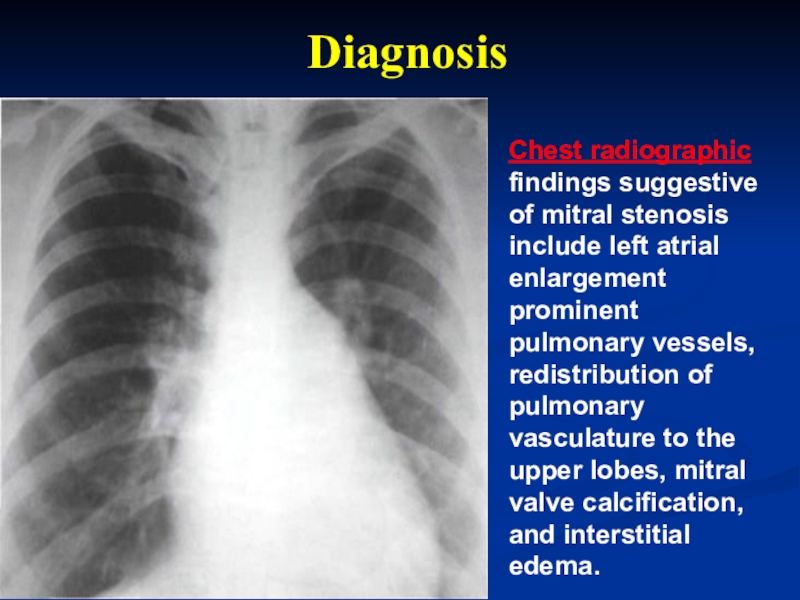
- 15. Chest radiographic findings suggestive of mitral stenosis
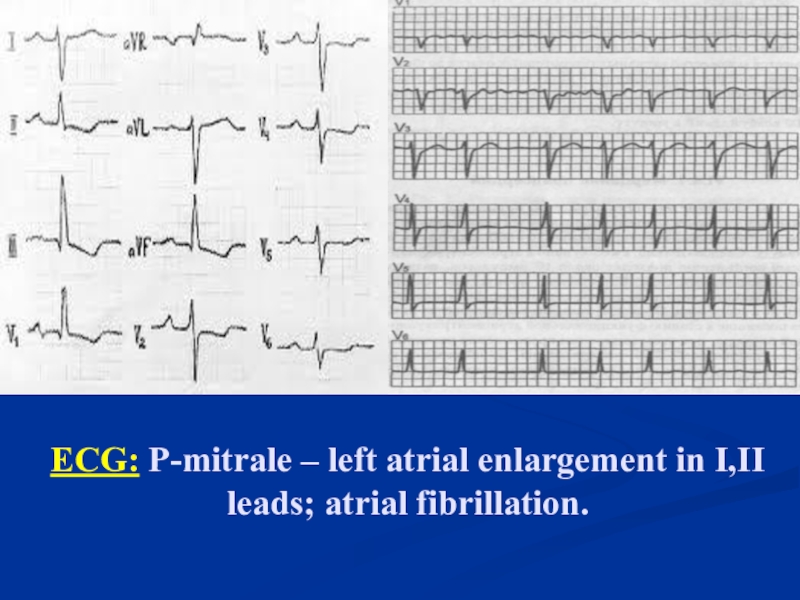
- 16. ECG: Р-mitrale – left atrial enlargement in I,II leads; atrial fibrillation.
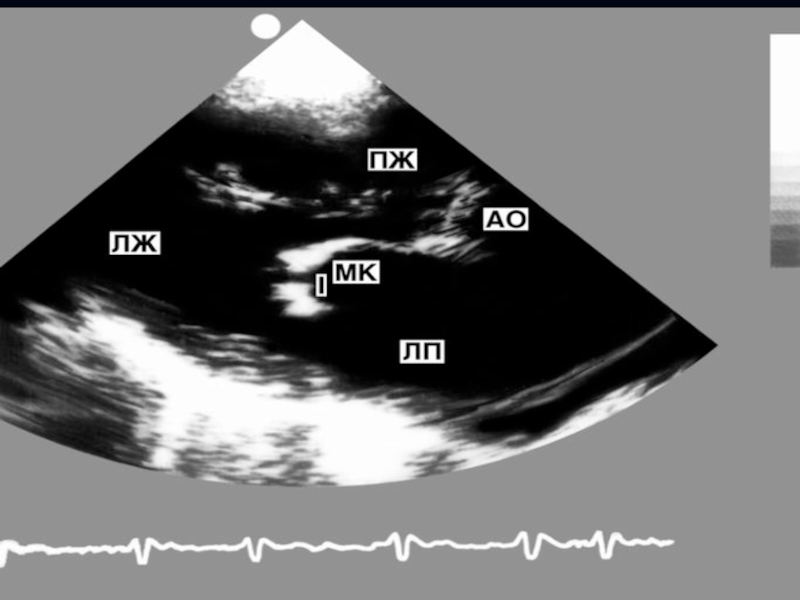
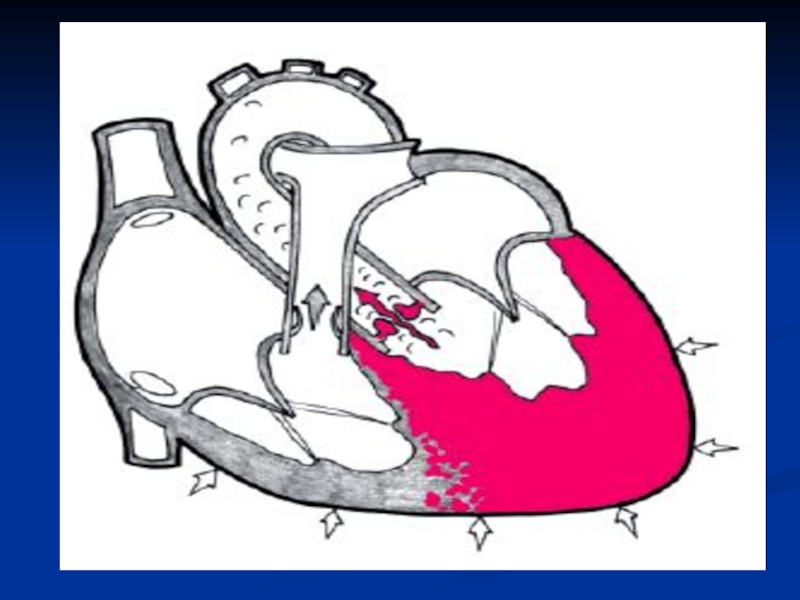
- 17. Echocardiographyis the most specific and sensitive method
- 18. Слайд 18
- 19. With echocardiography, the size of the mitral
- 20. Transesophageal echocardiography provides better quality images
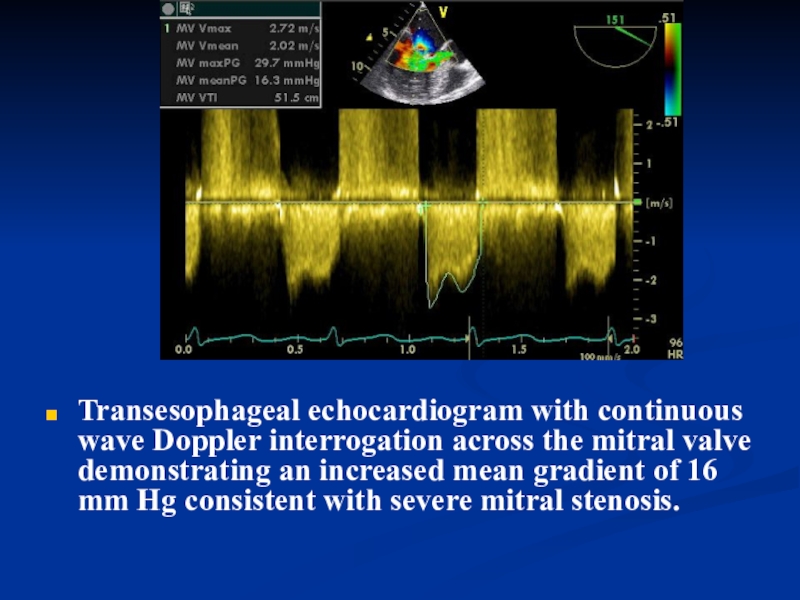
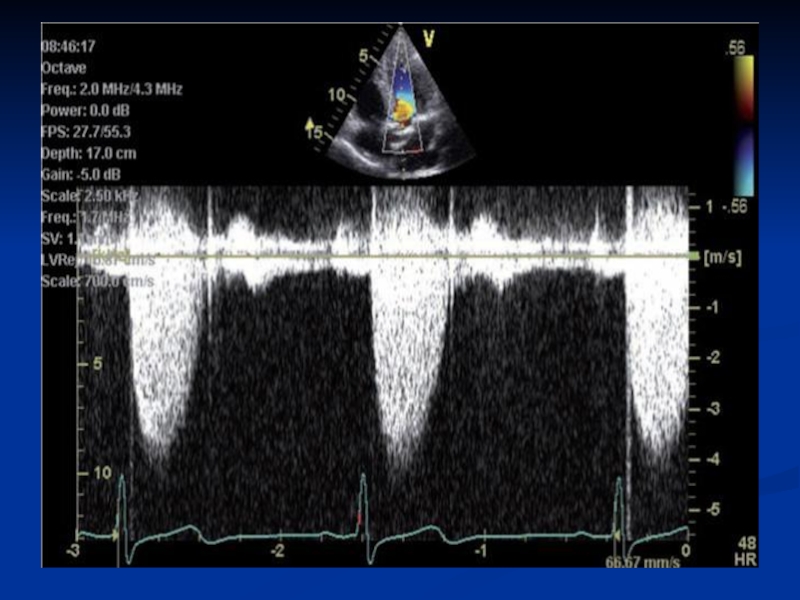
- 21. Transesophageal echocardiogram with continuous wave Doppler interrogation
- 22. Laboratory Studiesperform routine baseline tests such as
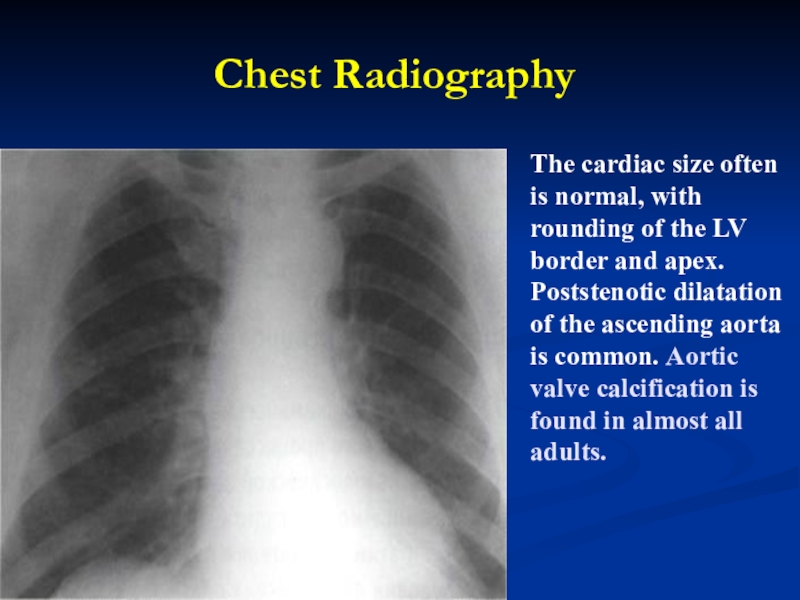
- 23. ComplicationsHemoptysis;Pulmonary edema;Atrial fibrillation;Systemic embolization (10-25%);Congestive heart failure;Pulmonary infections.
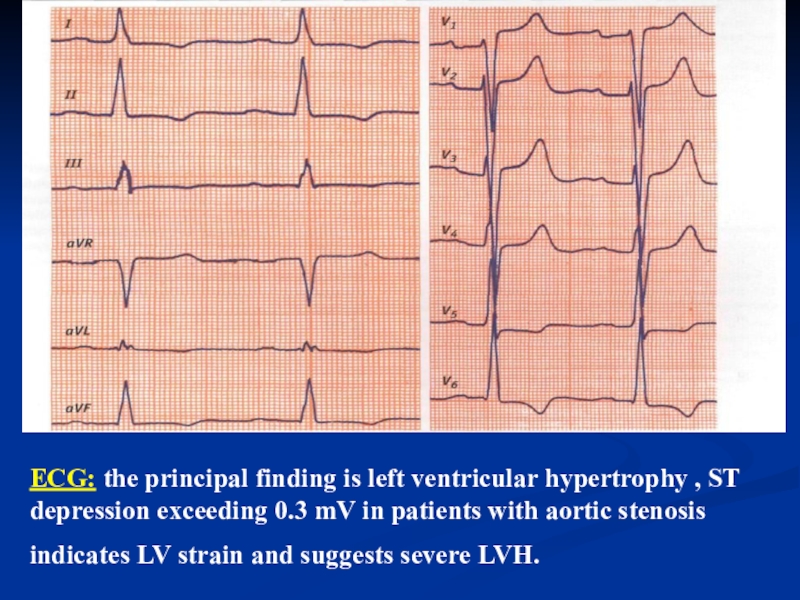
- 24. Differential Diagnosis Mitral insufficiency.Aortic insufficiency.Tuberculosis, bronchiectasis .Primary pulmonary hypertension.Atrial septal defect.
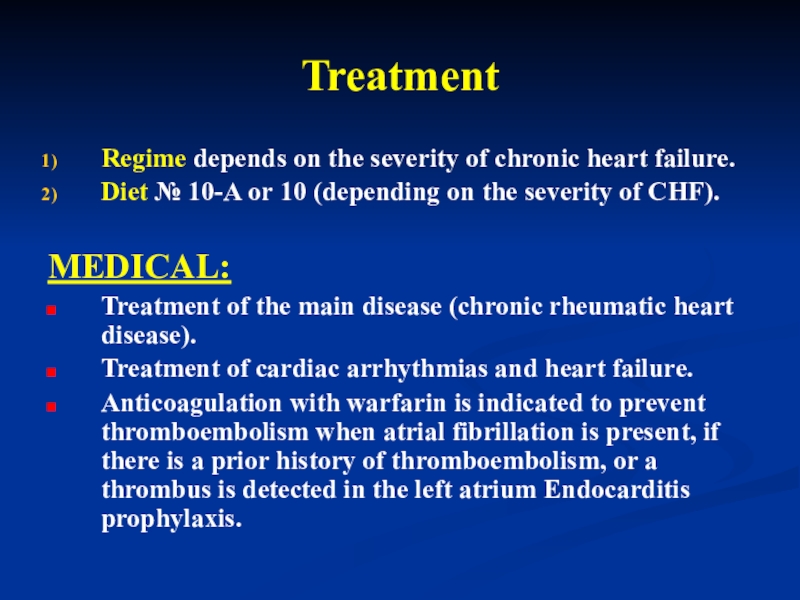
- 25. TreatmentRegime depends on the severity of chronic
- 26. Surgical TherapyMitral commissurotomyMitral Valve ReplacementMechanicalBioprosthetic Invasive therapy
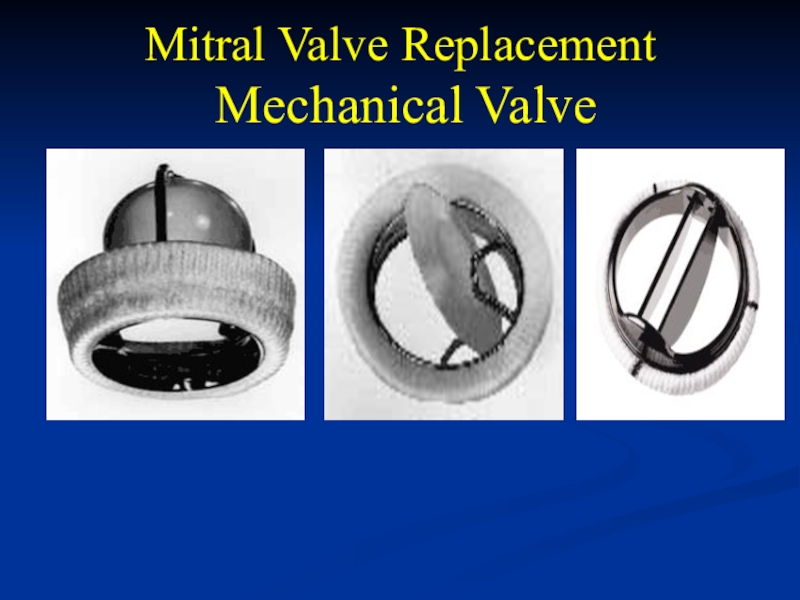
- 27. Mitral Valve Replacement Mechanical Valve
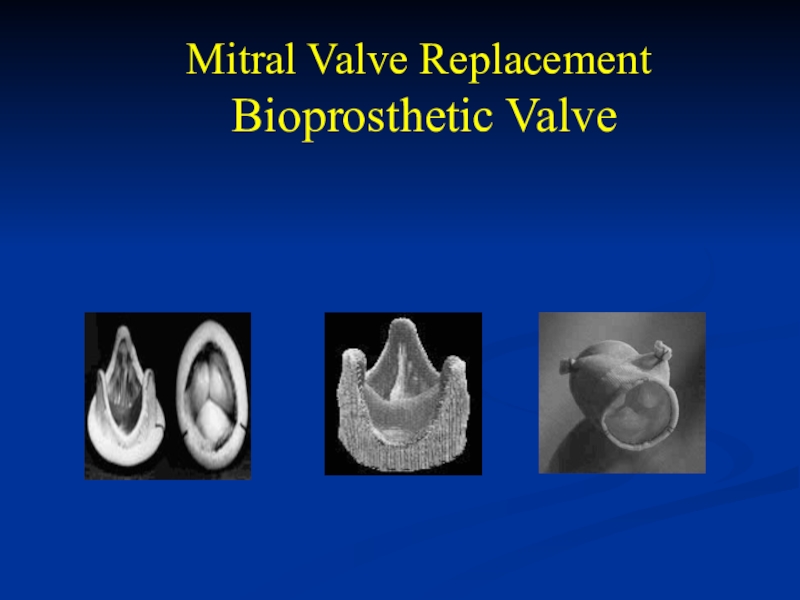
- 28. Mitral Valve Replacement Bioprosthetic Valve
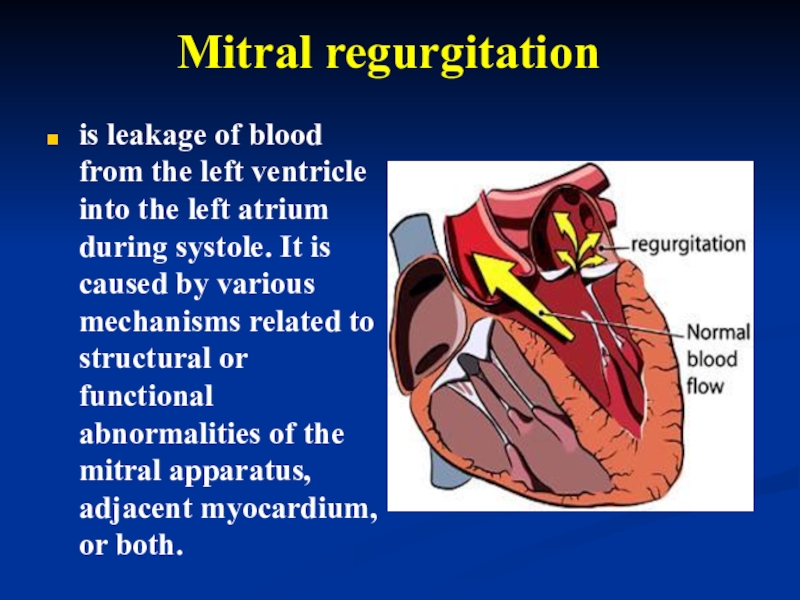
- 29. Mitral regurgitation is leakage of
- 30. EpidemiologySignificant mitral valve regurgitation occurs in about
- 31. EtiologyRheumatic fever.Infective endocarditis.Aterosclerosis.Myxomatous degeneration.Chordal rupture.Coronary artery disease.Cardiomyopathy.
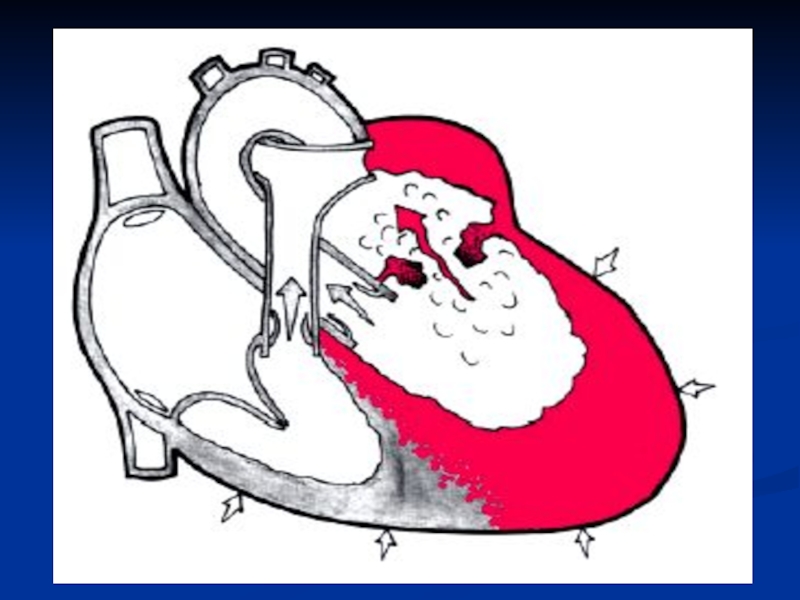
- 32. Pathophysiology Significant MR leads to volume
- 33. In chronic MR, a gradual
- 34. Слайд 34
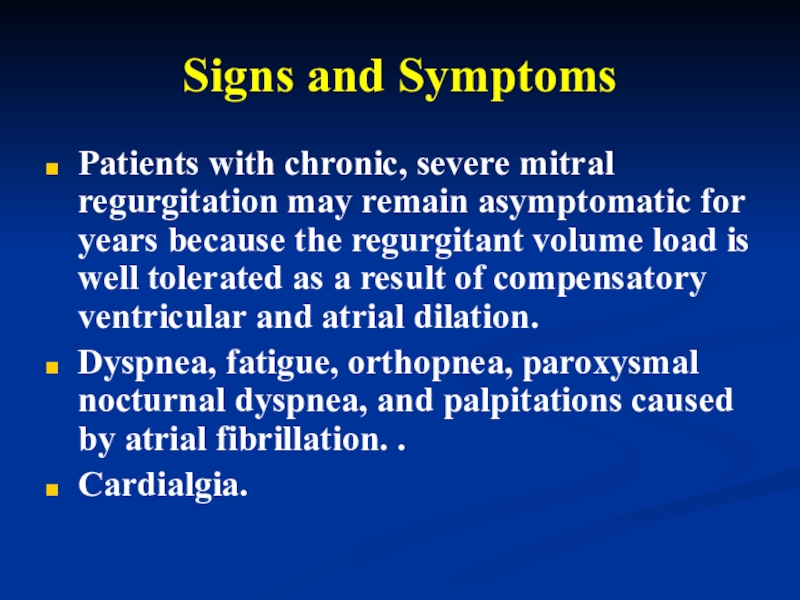
- 35. Signs and SymptomsPatients with chronic, severe mitral
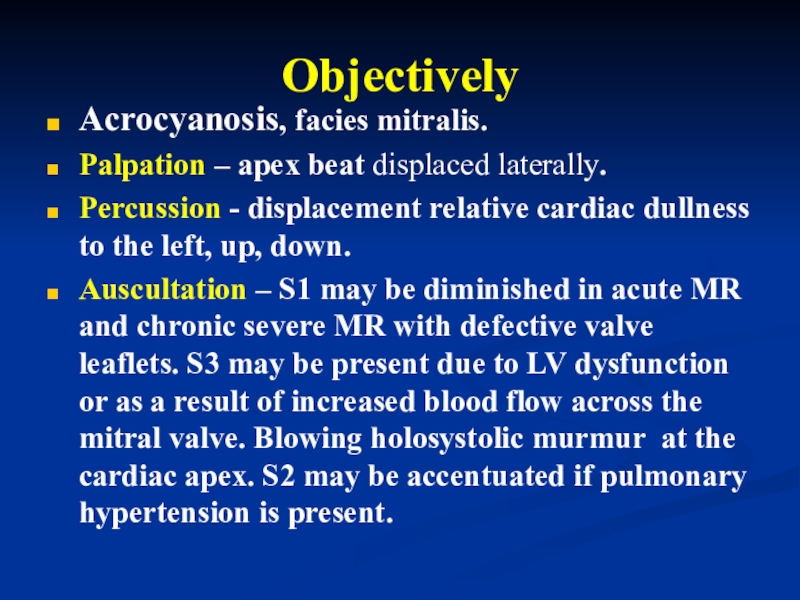
- 36. Objectively Acrocyanosis, facies mitralis.Palpation – apex beat
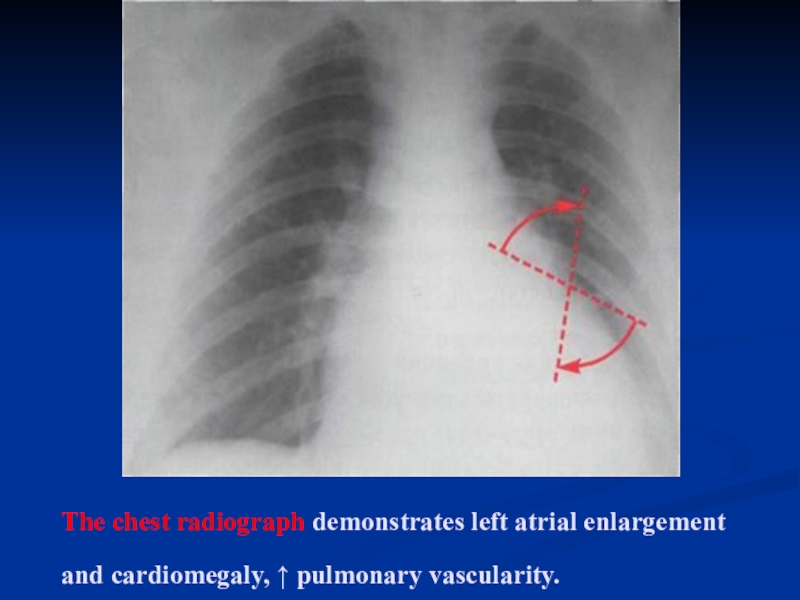
- 37. The chest radiograph demonstrates left atrial enlargement and cardiomegaly, pulmonary vascularity.
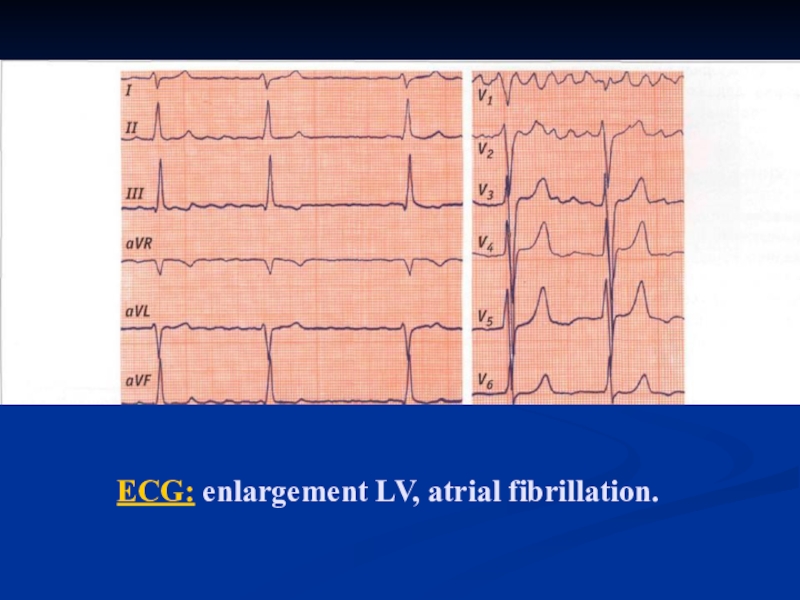
- 38. ECG: enlargement LV, atrial fibrillation.
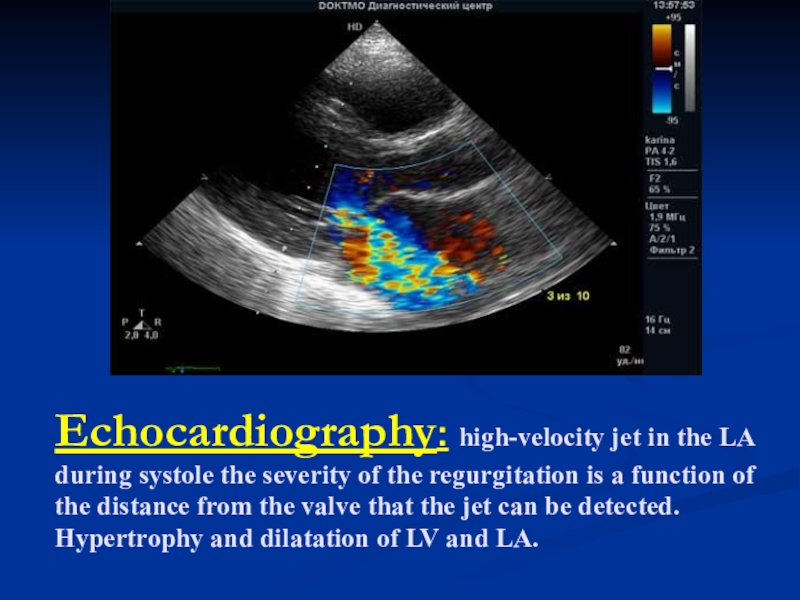
- 39. Echocardiography: high-velocity jet in the LA during
- 40. COMPLICATIONS Hemoptysis;Pulmonary edema;Atrial fibrillation;Thromboembolism.
- 41. Differential DiagnosesAortic StenosisMitral StenosisComplications of Myocardial InfarctionMitral Valve ProlapseVentricular Septal Defect
- 42. TreatmentRegime depends on the severity of chronic
- 43. Prognosis after surgical treatment prognosis is favorable
- 44. Aortic Stenosis Aortic stenosis refers
- 45. Слайд 45
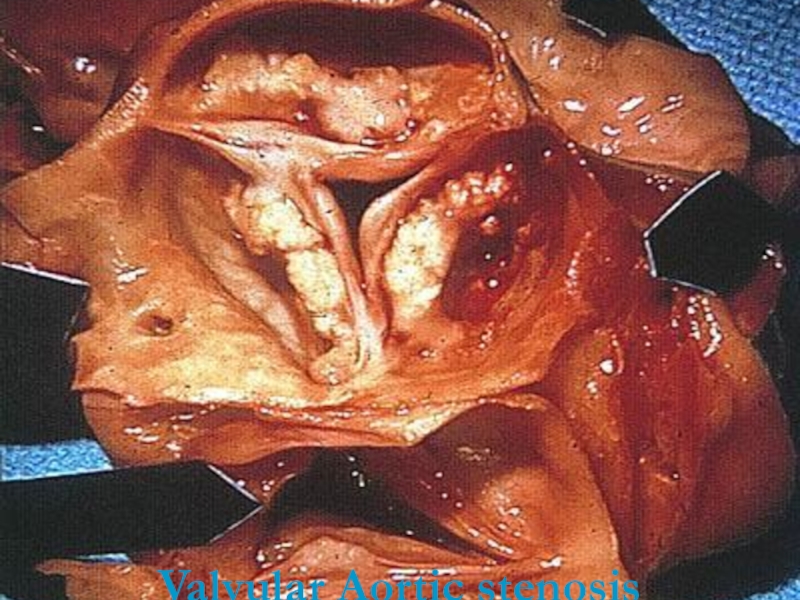
- 46. Valvular Aortic stenosisValvular Aortic stenosis.
- 47. EtiologyRheumatic fever.Degenerative calcific aortic stenosis.Infective endocarditis.Hypertrophic cardiomyopathy.
- 48. EpidemiologyDegenerative calcific aortic stenosis usually manifests in
- 49. Слайд 49
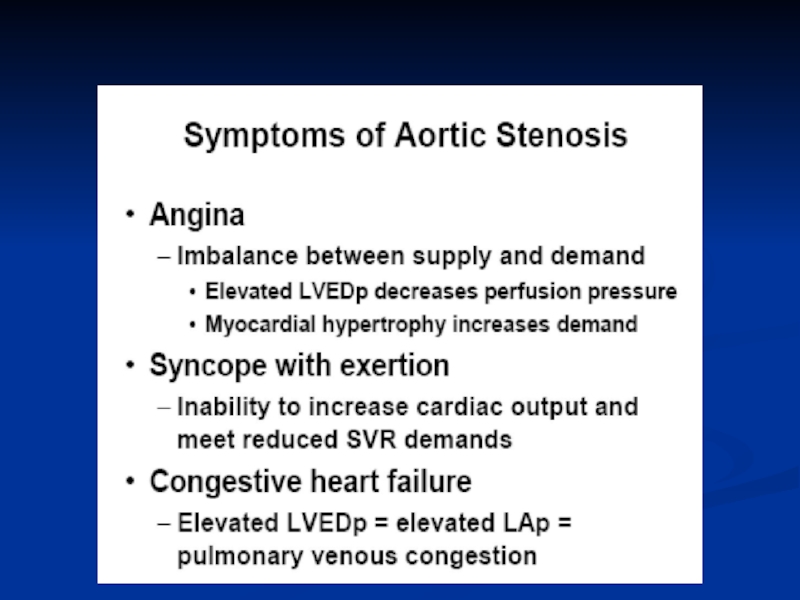
- 50. Symptoms and signsCommon in asymptomatic adults.Fatigue, dizziness, syncope. Angina pectoris.Dyspnea.Pulmonary edema.Hemoptysis.
- 51. Слайд 51
- 52. Physical Examination Pale skin or cyanosis.On palpation
- 53. On auscultation – S1 is usually normal
- 54. Physical ExaminationPulsus parvus and tardus (Carotid Impulse).Systolic
- 55. The cardiac size often is normal, with
- 56. ECG: the principal finding is left ventricular
- 57. Echocardiography: The following 3 echocardiographic findings are
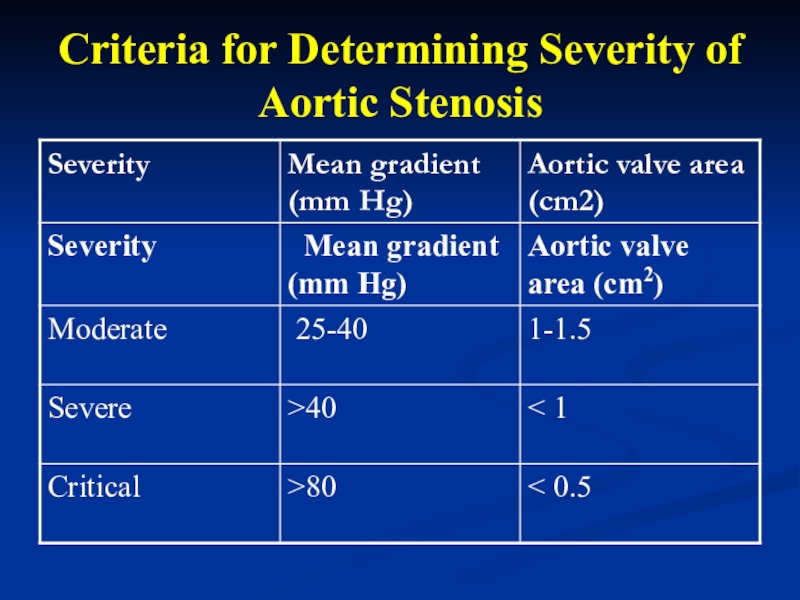
- 58. Criteria for Determining Severity of Aortic Stenosis
- 59. Слайд 59
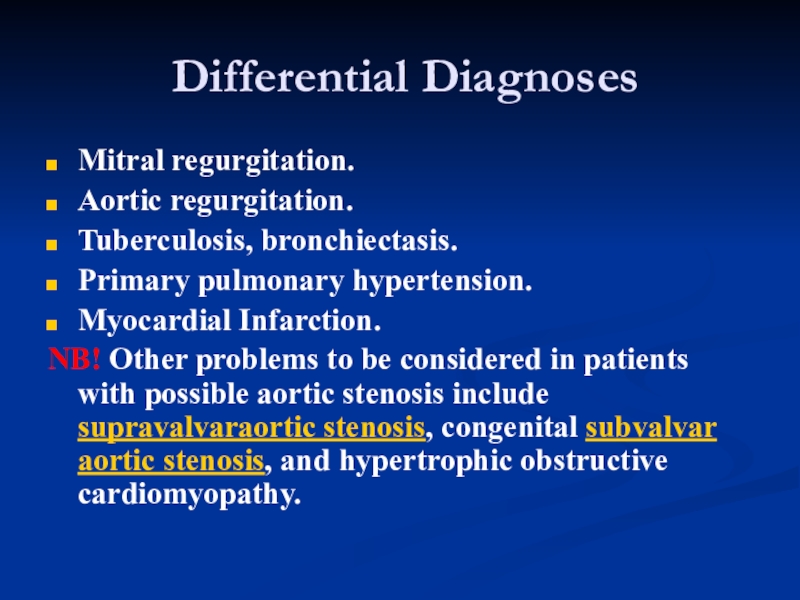
- 60. Differential DiagnosesMitral regurgitation.Aortic regurgitation.Tuberculosis, bronchiectasis.Primary pulmonary
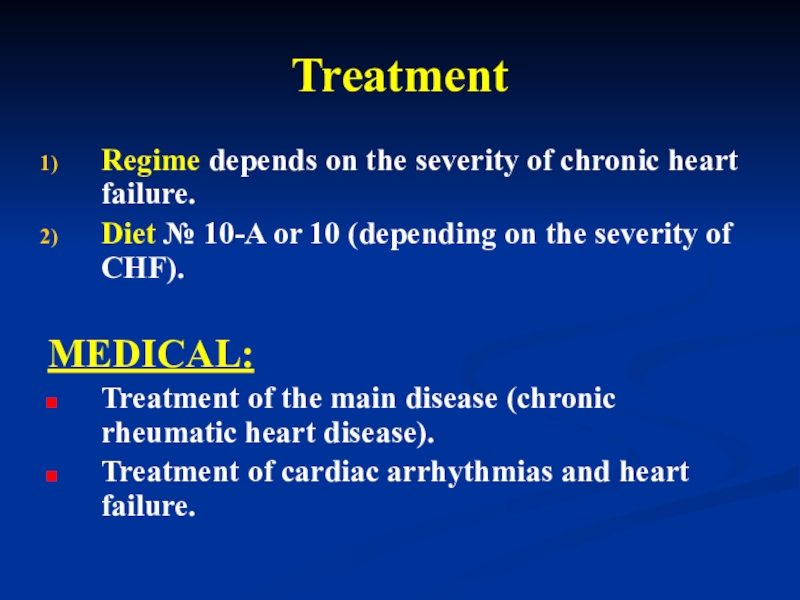
- 61. TreatmentRegime depends on the severity of chronic
- 62. Surgical TherapyAccording to both the ACC/AHA and
- 63. Surgical TherapyPatient with symptomatic AS and valve
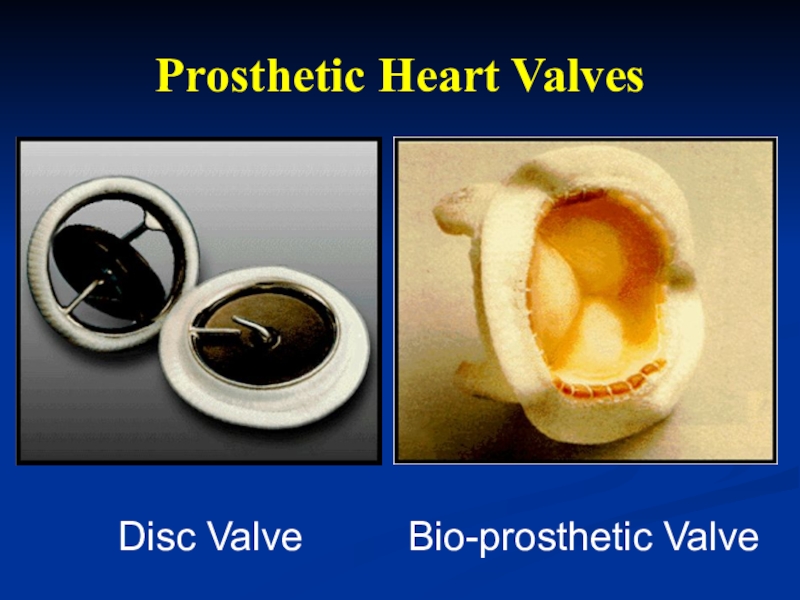
- 64. Prosthetic Heart ValvesDisc ValveBio-prosthetic Valve
- 65. PROGNOSIS The only definitive treatment for
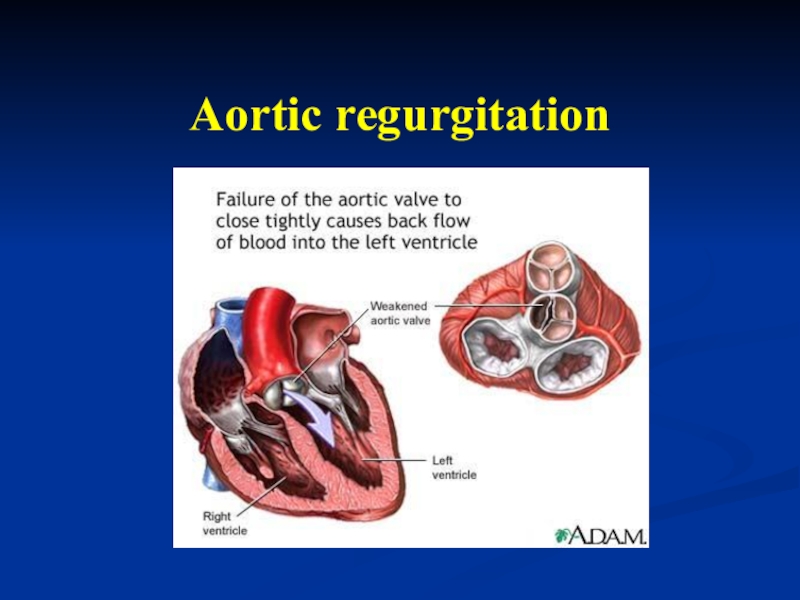
- 66. Aortic regurgitation
- 67. EtiologyAcquired:Rheumatic fever (60-80%).Infective endocarditis.Syphilitic aortitis.Collagen vascular diseases.
- 68. Epidemiology Although rheumatic heart
- 69. Слайд 69
- 70. Symptoms and singsPatients with chronic AR often
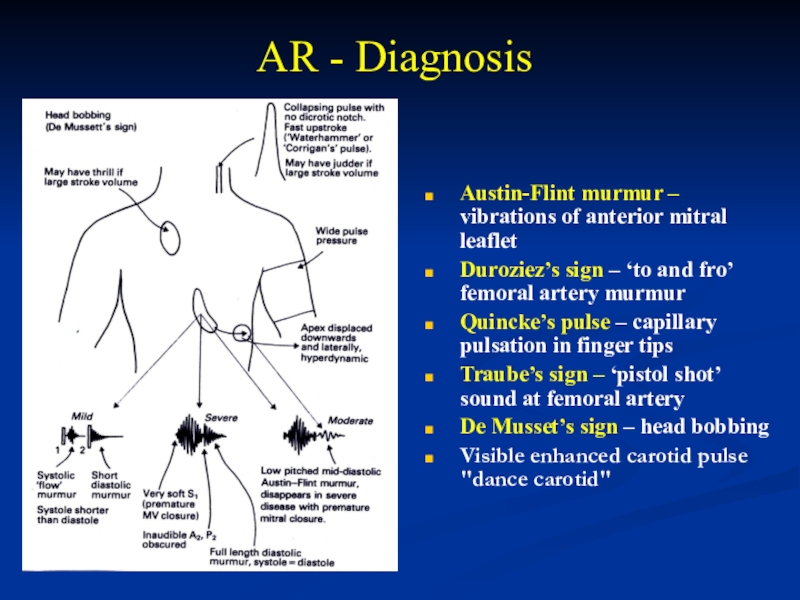
- 71. AR - DiagnosisAustin-Flint murmur – vibrations of
- 72. On palpation - the point of maximal
- 73. Pulsus- pulsus celer, tachycardia.BP – Diastolic pressures
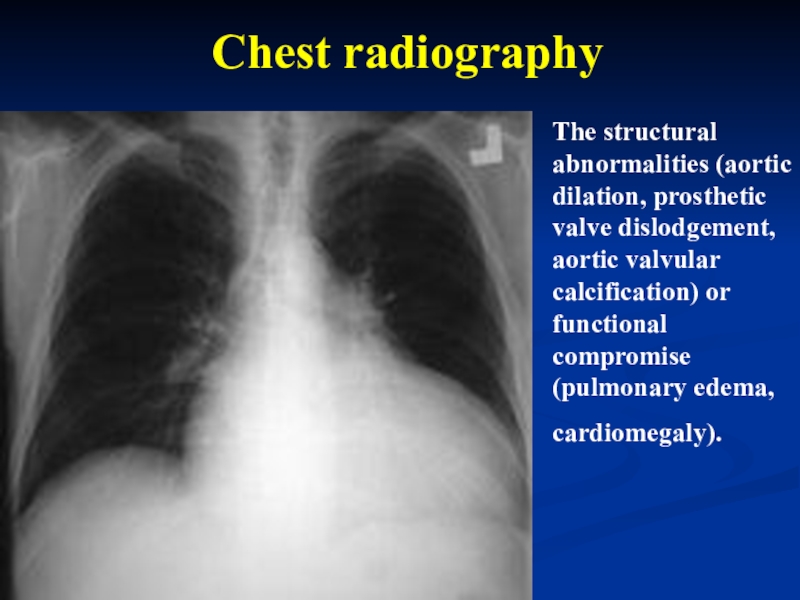
- 74. The structural abnormalities (aortic dilation, prosthetic valve
- 75. ECG: Left axis deviation , LV hypertrophy, LA enlargement.
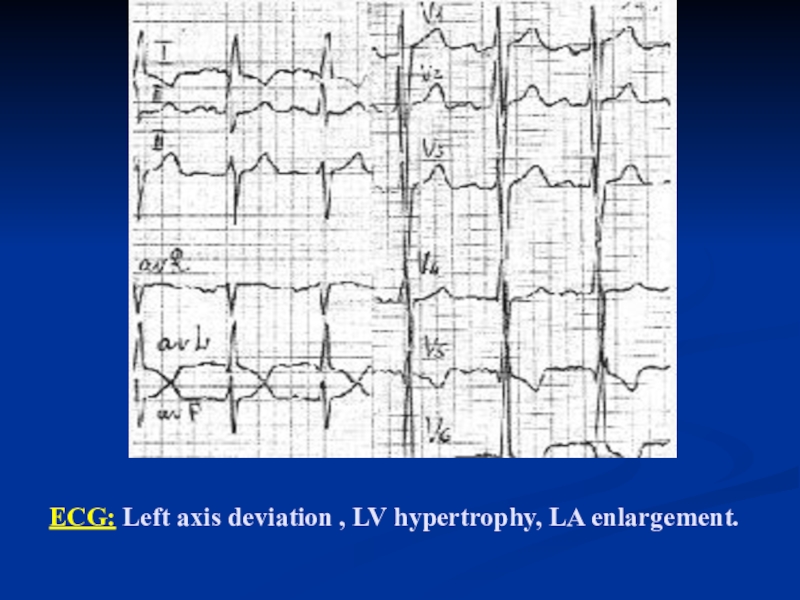
- 76. Echocardiography:Aortic valve structure and morphology - Bileaflet
- 77. Echocardiography:Premature closure of the mitral valve (seen
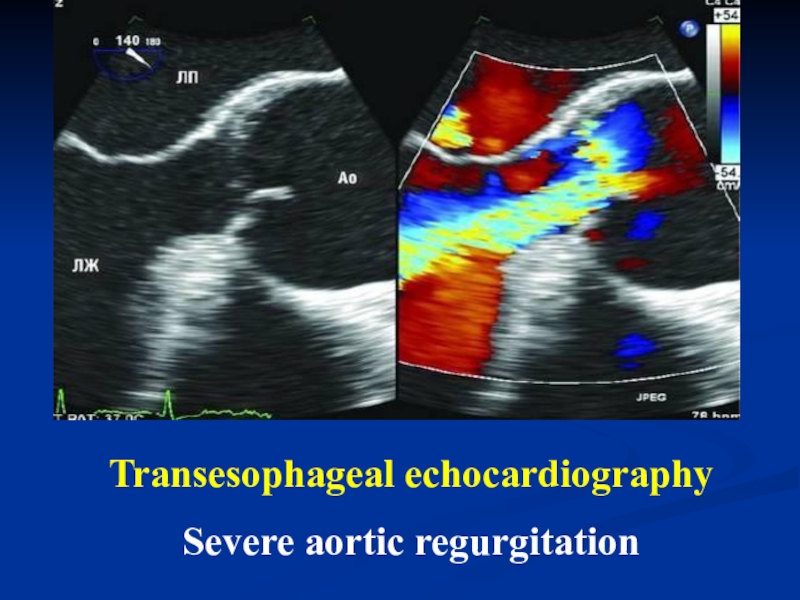
- 78. Transesophageal echocardiography Severe aortic regurgitation
- 79. Other methods of diagnostics:Radionuclide imaging (may provide
- 80. TreatmentRegime depends on the severity of chronic
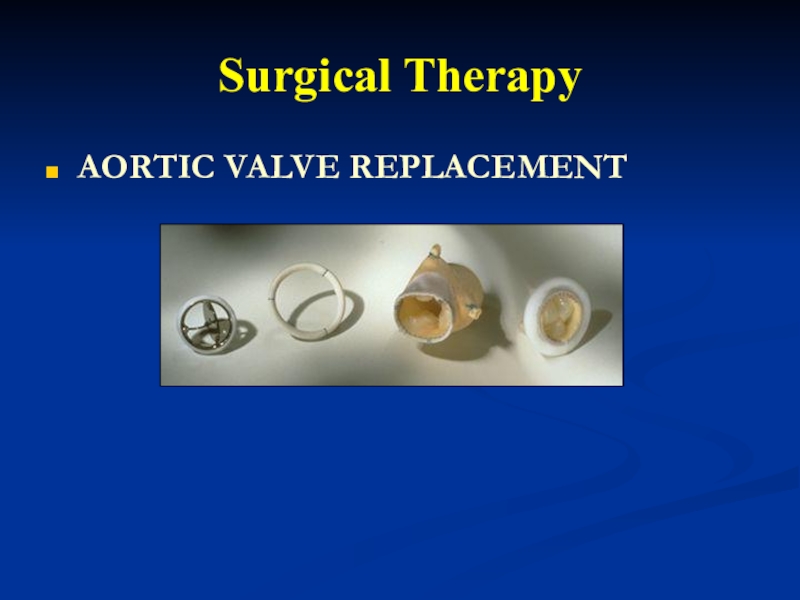
- 81. Surgical TherapyAORTIC VALVE REPLACEMENT
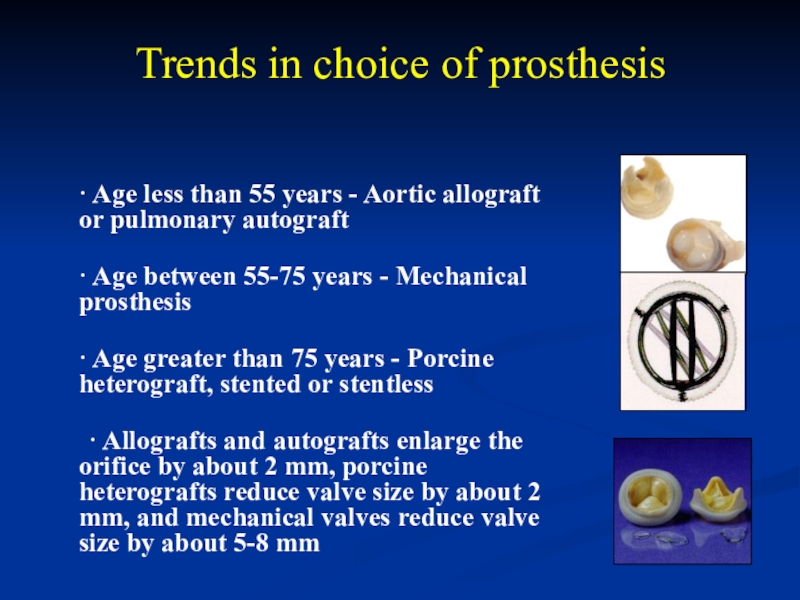
- 82. Trends in choice of prosthesis · Age
- 83. Prognosis Three fourths of patients with
- 84. http://www.escardio.org/guidelines-surveys/esc-guidelines/Pages/valvular-heart-disease.aspx ESC/EACTS Guidelines on the management
- 85. TAKE CARE YOUR HEART! THANK YOU!
- 86. Скачать презентанцию
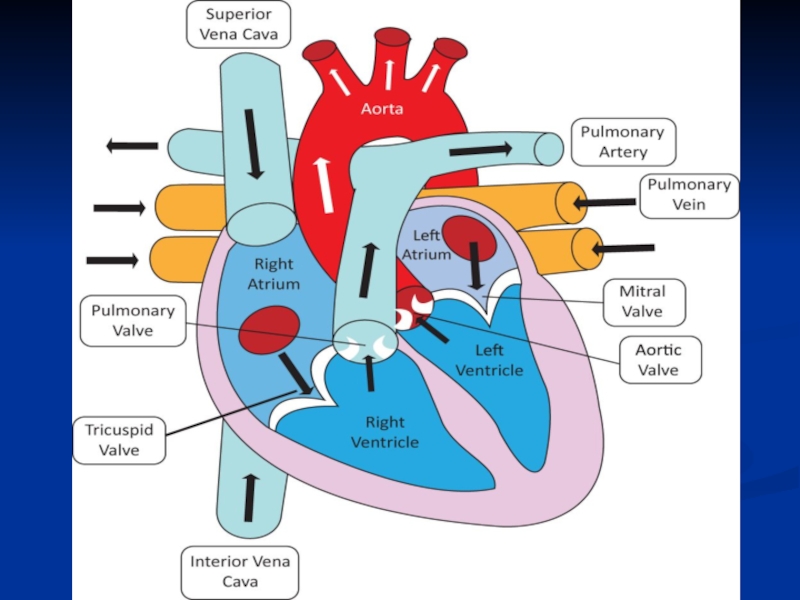
Valvular heart disease is any disease process involving one or more of the valves of the heart (the aortic and mitral valves on the left and the pulmonary and
Слайды и текст этой презентации
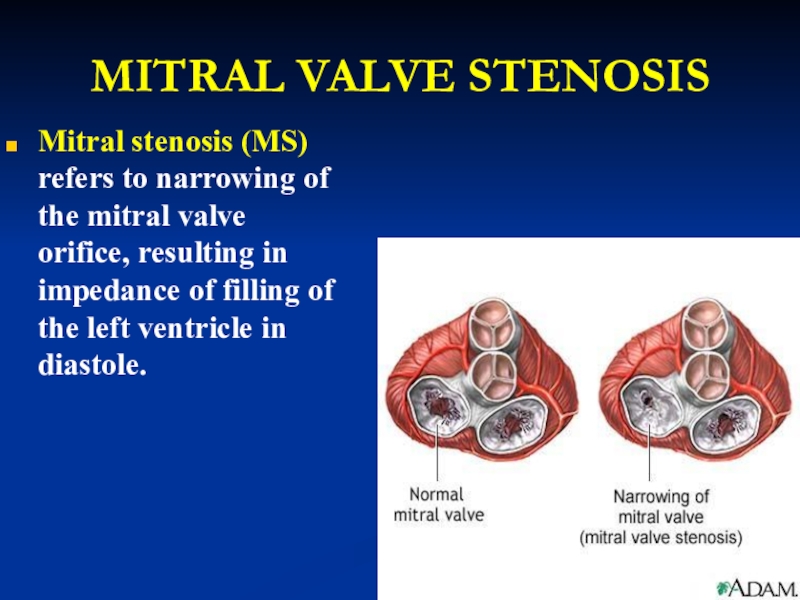
Слайд 4MITRAL VALVE STENOSIS
Mitral stenosis (MS) refers to narrowing of the
mitral valve orifice, resulting in impedance of filling of the
left ventricle in diastole.Слайд 5ETIOLOGY
Primarily a result of rheumatic fever.
Infective endocarditis.
Systemic lupus erythematosus, rheumatoid
arthritis.
Severe calcification of the mitral annulus.
The association of atrial
septal defect with rheumatic mitral stenosis is called Lutembacher syndrome. Epidemiology: The prevalence of rheumatic disease is higher in developing nations than in the United States. In India, for example, the prevalence is approximately 100-150 cases per 100,000, and in Africa the prevalence is 35 cases per 100,000.
Слайд 6Pathophysiology
Normal valve area: 4-6 cm2
Mild mitral stenosis:
MVA 1.5-2.5 cm2
Minimal
symptoms
Mod mitral stenosis
MVA 1.0-1.5 cm2 usually does not produce symptoms
at restSevere mitral stenosis
MVA < 1.0 cm2
Слайд 7Pathophysiology
Patients with MS typically present more than 20
years after an episode of rheumatic fever. Single or recurrent
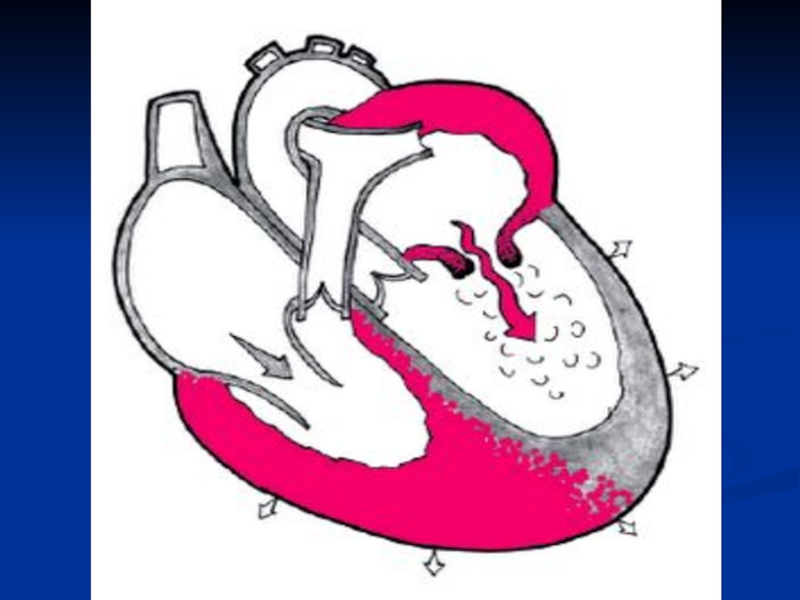
bouts of rheumatic carditis cause progressive thickening, scarring, and calcification of the mitral leaflets and chordae. Fusion of the commissures and chordae decreases the size of the mitral opening. This obstruction results in the development of a pressure gradient across the valve in diastole and causes an elevation in left atrial and pulmonary venous pressures.Слайд 8Pathophysiology
Elevated left atrial pressures lead to left atrial
enlargement, predisposing the patient to atrial fibrillation and arterial thromboembolism.
Elevated pulmonary venous pressure results in pulmonary congestion and pulmonary edema. In advanced mitral stenosis, patients develop pulmonary hypertension and right-sided heart failure.Слайд 10Symptoms and sings
Dyspnea , cough.
Left sided failure.
Hemoptysis.
Palpitation, Atrial arrhythmias.
Cardialgia.
Systemic embolism.
Right
sided failure (Hepatic Congestion, Edema).
Слайд 11Objectively
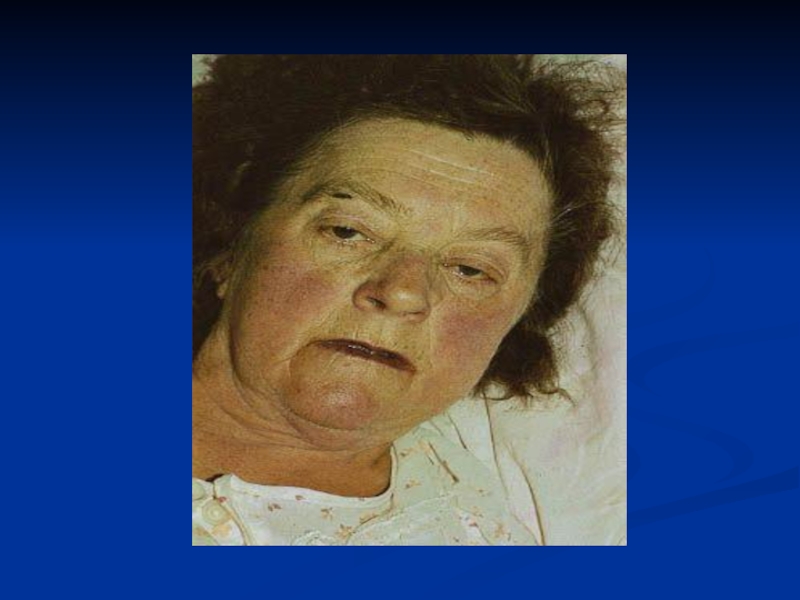
Acrocyanosis , facies mitralis.
Palpation - «purring thrill» - it refers
to a vibration, like a cat's purring, due to mitral
stenosis .Percussion – shifting boundaries of relative cardiac dullness up and right .
Слайд 13 Auscultation:
The auscultatory findings characteristic of mitral stenosis are
a loud first heart sound, an opening snap, and a
diastolic rumble.The first heart sound is accentuated because of a wide closing excursion of the mitral leaflets. The intensity of the first heart sound diminishes as the valve becomes more fibrotic, calcified, and thickened.
The diastolic murmur of mitral stenosis is of low pitch, rumbling in character, and best heard at the apex with the patient in the left lateral position. It commences after the opening snap of the mitral valve, and the duration of the murmur correlates with the severity of the stenosis.
Слайд 14 Auscultation:
3. The second heart sound is normally split, and
the pulmonic component is accentuated if pulmonary hypertension is present.
4. A high-pitched decrescendo diastolic murmur secondary to pulmonary regurgitation (Graham Steell murmur) may be audible at the upper sternal border.
Pulse – tachycardia, pulsus differens.
Слайд 15Chest radiographic findings suggestive of mitral stenosis include left atrial
enlargement prominent pulmonary vessels, redistribution of pulmonary vasculature to the
upper lobes, mitral valve calcification, and interstitial edema.Diagnosis
Слайд 17Echocardiography
is the most specific and sensitive method of diagnosing and
quantifying the severity of mitral stenosis. Using a transthoracic 2-dimensional
echocardiogram, Doppler study, and color-flow Doppler imaging, the anatomic abnormalities of the stenotic valve (ie, thickening, mobility, motion, calcification), involvement of the subvalvular apparatus and the characteristic fusion of the commissures can be well defined.Слайд 19With echocardiography, the size of the mitral valve orifice can
be precisely quantified. Important information about the ventricular and atrial
chamber sizes, the presence of a left atrial thrombus, measurement of transvalvular gradient, and pulmonary arterial pressure can also be obtained.With the use of Doppler echocardiography, sufficient information can be obtained to develop a therapeutic plan, and, consequently, most patients do not require invasive procedures such as cardiac catheterization.
Слайд 20Transesophageal echocardiography
provides better quality images than transthoracic
echocardiography and is more accurate in assessing the anatomic features
of the valve and the presence of left atrial appendage thrombus.Transesophageal echocardiography is indicated in patients before percutaneous mitral balloon valvotomy or cardioversion.
Слайд 21
Transesophageal echocardiogram with continuous wave Doppler interrogation across the mitral
valve demonstrating an increased mean gradient of 16 mm Hg
consistent with severe mitral stenosis.Слайд 22Laboratory Studies
perform routine baseline tests such as CBC count, electrolyte
status, and renal and liver function tests.
Слайд 23Complications
Hemoptysis;
Pulmonary edema;
Atrial fibrillation;
Systemic embolization (10-25%);
Congestive heart failure;
Pulmonary infections.
Слайд 24Differential Diagnosis
Mitral insufficiency.
Aortic insufficiency.
Tuberculosis, bronchiectasis .
Primary pulmonary hypertension.
Atrial septal
defect.
Слайд 25Treatment
Regime depends on the severity of chronic heart failure.
Diet №
10-A or 10 (depending on the severity of CHF).
MEDICAL:
Treatment
of the main disease (chronic rheumatic heart disease). Treatment of cardiac arrhythmias and heart failure.
Anticoagulation with warfarin is indicated to prevent thromboembolism when atrial fibrillation is present, if there is a prior history of thromboembolism, or a thrombus is detected in the left atrium Endocarditis prophylaxis.
Слайд 26Surgical Therapy
Mitral commissurotomy
Mitral Valve Replacement
Mechanical
Bioprosthetic
Invasive therapy should be considered
for all patients with symptomatic mitral stenosis. Percutaneous mitral balloon
valvotomy and surgical commissurotomy provide equivalent immediate and long-term outcome results and delay the need for mitral valve replacement.Слайд 29Mitral regurgitation
is leakage of blood from the left ventricle
into the left atrium during systole. It is caused by
various mechanisms related to structural or functional abnormalities of the mitral apparatus, adjacent myocardium, or both.Слайд 30Epidemiology
Significant mitral valve regurgitation occurs in about 2% of the
population with a similar prevalence in males and females.
Слайд 31Etiology
Rheumatic fever.
Infective endocarditis.
Aterosclerosis.
Myxomatous degeneration.
Chordal rupture.
Coronary artery disease.
Cardiomyopathy.
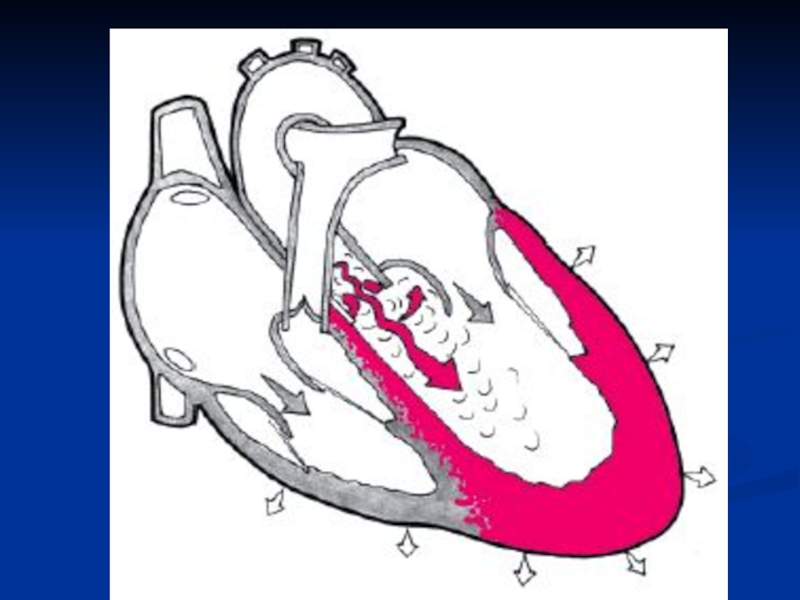
Слайд 32Pathophysiology
Significant MR leads to volume overload of the
left ventricle, because it has to accommodate both the stroke
volume and regurgitant volume with each heartbeat. To compensate, the left ventricle dilates and becomes hyperdynamic. In acute severe MR, the left atrial and pulmonary venous pressures increase quickly, leading to pulmonary congestion and pulmonary edema.Слайд 33 In chronic MR, a gradual increase in left
atrial size and compliance compensate so that left atrial and
pulmonary venous pressures do not increase until late in the course of the disease. Progressive left ventricular dilation eventually leads to an increase in afterload, contractile dysfunction, and heart failure. Left atrial enlargement predisposes the patient to atrial fibrillation and arterial thromboembolism. In long-standing MR, patients may develop pulmonary hypertension and right-sided heart failure.Слайд 35Signs and Symptoms
Patients with chronic, severe mitral regurgitation may remain
asymptomatic for years because the regurgitant volume load is well
tolerated as a result of compensatory ventricular and atrial dilation.Dyspnea, fatigue, orthopnea, paroxysmal nocturnal dyspnea, and palpitations caused by atrial fibrillation. .
Cardialgia.
Слайд 36Objectively
Acrocyanosis, facies mitralis.
Palpation – apex beat displaced laterally.
Percussion -
displacement relative cardiac dullness to the left, up, down.
Auscultation –
S1 may be diminished in acute MR and chronic severe MR with defective valve leaflets. S3 may be present due to LV dysfunction or as a result of increased blood flow across the mitral valve. Blowing holosystolic murmur at the cardiac apex. S2 may be accentuated if pulmonary hypertension is present. Слайд 37The chest radiograph demonstrates left atrial enlargement and cardiomegaly,
pulmonary vascularity.
Слайд 39Echocardiography: high-velocity jet in the LA during systole the severity
of the regurgitation is a function of the distance from
the valve that the jet can be detected. Hypertrophy and dilatation of LV and LA.Слайд 41Differential Diagnoses
Aortic Stenosis
Mitral Stenosis
Complications of Myocardial Infarction
Mitral Valve Prolapse
Ventricular Septal
Defect
Слайд 42Treatment
Regime depends on the severity of chronic heart failure.
Diet №
10-A or 10 (depending on the severity of CHF).
MEDICAL:
Treatment
of the main disease (chronic rheumatic heart disease). Treatment of cardiac arrhythmias and heart failure.
Anticoagulation with warfarin is indicated to prevent thromboembolism when atrial fibrillation is present, if there is a prior history of thromboembolism, or a thrombus is detected in the left atrium Endocarditis prophylaxis.
Слайд 44Aortic Stenosis
Aortic stenosis refers
to obstruction
of flow at the level of the aortic valve and
does not include the subvalvular and supravalvular formsof this disease.
Слайд 47Etiology
Rheumatic fever.
Degenerative calcific aortic stenosis.
Infective endocarditis.
Hypertrophic cardiomyopathy.
Aortic stenosis has several etiologies, including congenital (unicuspid
or bicuspid valve), calcific (due to degenerative changes), and rheumatic.Слайд 48Epidemiology
Degenerative calcific aortic stenosis usually manifests in individuals older than
75 years and occurs most frequently in males. Aortic sclerosis
(aortic valve calcification without obstruction to blood flow, considered a precursor of calcific degenerative calcific aortic stenosis) increases in incidence with age and is present in 29% of individuals older than 65 years and in 37% of individuals older than 75 years. Degenerative calcific aortic stenosis usually manifests in individuals older than 75 years and occurs most frequently in males.Слайд 50 Symptoms and signs
Common in asymptomatic adults.
Fatigue, dizziness, syncope.
Angina
pectoris.
Dyspnea.
Pulmonary edema.
Hemoptysis.
Слайд 52Physical Examination
Pale skin or cyanosis.
On palpation – apex beat amplified
and shifted to the left.
On percussion – displacement of relative
cardiac dullness to the left, down.Слайд 53On auscultation – S1 is usually normal or soft. The
aortic component of the second heart sound, A2, is usually
diminished or absent, because the aortic valve is calcified and immobile and/or the aortic ejection is prolonged and it is obscured by the prolonged systolic ejection murmur. The presence of a normal or accentuated A2 speaks against the presence of severe aortic stenosis.The classic crescendo-decrescendo harsh systolic murmur of aortic stenosis begins shortly after the first heart sound.
The intensity of the systolic murmur does not correspond to the severity of aortic stenosis; rather, the timing of the peak and the duration of the murmur corresponds to the severity of aortic stenosis.
Слайд 54Physical Examination
Pulsus parvus and tardus (Carotid Impulse).
Systolic hypertension can coexist
with aortic stenosis. However, a systolic blood pressure higher than
200 mm Hg is rare in patients with critical aortic stenosis.Слайд 55The cardiac size often is normal, with rounding of the
LV border and apex. Poststenotic dilatation of the ascending aorta
is common. Aortic valve calcification is found in almost all adults.Chest Radiography
Слайд 56ECG: the principal finding is left ventricular hypertrophy , ST
depression exceeding 0.3 mV in patients with aortic stenosis indicates
LV strain and suggests severe LVH.Слайд 57
Echocardiography: The following 3 echocardiographic findings are indicative of severe
aortic stenosis:
1. An echo-dense aortic valve with no cusp motion
(may be unreliable in congenital or rheumatic valvular stenosis).2. A decrease in the maximal aortic cusp separation (< 8 mm in the adult).
3. The presence of otherwise unexplained LV hypertrophy.
Cardiac Catheterization and Coronary Arteriography- if clinical findings are not consistent with Doppler echocardiogram results, cardiac catheterization is recommended for further hemodynamic assessment.
Слайд 60 Differential Diagnoses
Mitral regurgitation.
Aortic regurgitation.
Tuberculosis, bronchiectasis.
Primary pulmonary hypertension.
Myocardial Infarction.
NB! Other
problems to be considered in patients with possible aortic stenosis
include supravalvaraortic stenosis, congenital subvalvar aortic stenosis, and hypertrophic obstructive cardiomyopathy.Слайд 61Treatment
Regime depends on the severity of chronic heart failure.
Diet №
10-A or 10 (depending on the severity of CHF).
MEDICAL:
Treatment
of the main disease (chronic rheumatic heart disease). Treatment of cardiac arrhythmias and heart failure.
Слайд 62Surgical Therapy
According to both the ACC/AHA and ESC/EACTS guidelines, aortic
valve replacement should be performed in all symptomatic patients with
severe aortic stenosis, regardless of LV function, as survival is better with surgical treatment than with medical treatment.Слайд 63Surgical Therapy
Patient with symptomatic AS and valve gradient indicative of
moderate or severe stenosis(>50 mm Hg) should have valve replacement
Aortic
Balloon Valvuloplasty is useful in congenital aortic stenosisAnticoagulants are required only if patient have atrial fibrillation or have valve replacement with mechanical prosthesis
Слайд 65PROGNOSIS
The only definitive treatment for aortic stenosis
is aortic valve replacement. The development of symptoms due to
aortic stenosis provides a clear indication for replacement. For patients who are not candidates for aortic replacement, percutaneous aortic balloon valvuloplasty may provide some symptom relief.Medical treatment (such as diuretic therapy) in aortic stenosis may provide temporary symptom relief but is generally not effective long term.
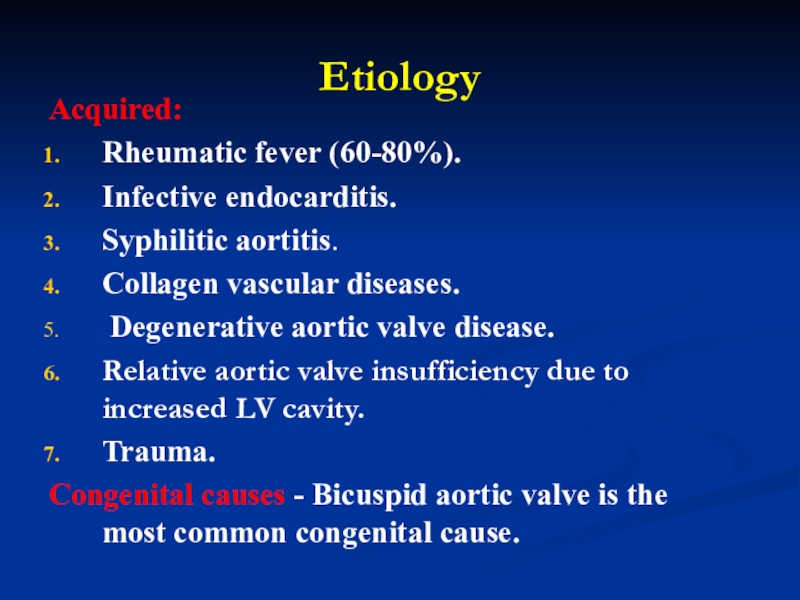
Слайд 67Etiology
Acquired:
Rheumatic fever (60-80%).
Infective endocarditis.
Syphilitic aortitis.
Collagen vascular diseases.
Degenerative aortic valve
disease.
Relative aortic valve insufficiency due to increased LV cavity.
Trauma.
Congenital
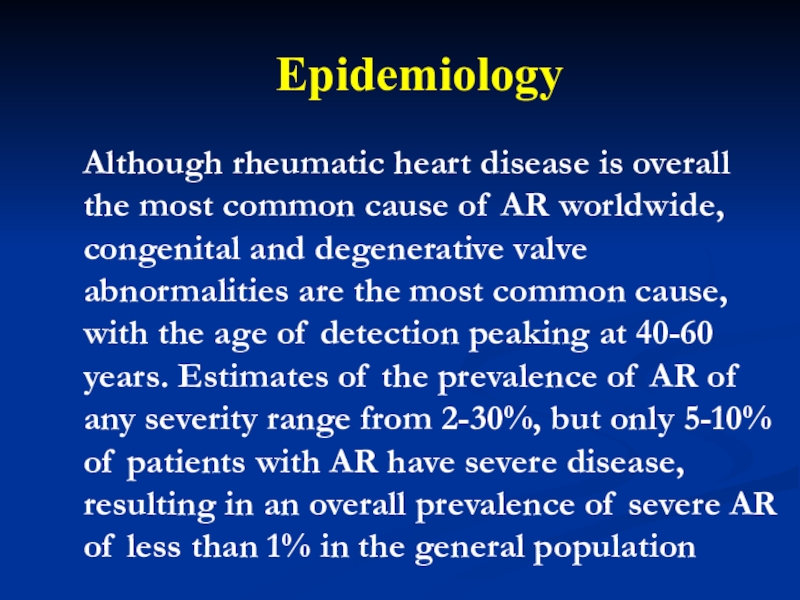
causes - Bicuspid aortic valve is the most common congenital cause. Слайд 68 Epidemiology
Although rheumatic heart disease is overall
the most common cause of AR worldwide, congenital and degenerative
valve abnormalities are the most common cause, with the age of detection peaking at 40-60 years. Estimates of the prevalence of AR of any severity range from 2-30%, but only 5-10% of patients with AR have severe disease, resulting in an overall prevalence of severe AR of less than 1% in the general populationСлайд 70Symptoms and sings
Patients with chronic AR often have a long-standing
asymptomatic period that may last for several years.
Palpitations - Often
described as the sensation of having forceful heart beats, due to widened pulse pressure with hyperdynamic circulation Uncomfortable awareness of the heartbeat
Shortness of breath - May not worsen with exertion in the early stages due to compensatory tachycardia with shortened diastole
Chest pain - Occurs if increased LV end-diastolic pressure compromises coronary perfusion pressure gradients
Headache pulsing character, dizziness, syncope.
Слайд 71AR - Diagnosis
Austin-Flint murmur – vibrations of anterior mitral leaflet
Duroziez’s
sign – ‘to and fro’ femoral artery murmur
Quincke’s pulse –
capillary pulsation in finger tipsTraube’s sign – ‘pistol shot’ sound at femoral artery
De Musset’s sign – head bobbing
Visible enhanced carotid pulse "dance carotid"
Слайд 72On palpation - the point of maximal heart beat may
be diffuse or hyperdynamic but is often displaced inferiorly and
toward the axilla.On percussion - displacement of relative cardiac dullness to the left, down.
On auscultation - weakening or disappearance of II sound of the aorta.
A systolic murmur of the aorta occurs in diastole, usually as a high-pitched sound that is loudest at the left sternal border.
An Austin-Flint murmur may be present at the cardiac apex in severe AR; it is a low-pitched, mid-diastolic rumbling murmur due to blood jets from the AR striking the anterior leaflet of the mitral valve, which results in premature closure of the mitral leaflets.
Слайд 73Pulsus- pulsus celer, tachycardia.
BP – Diastolic pressures are often lower
than 60 mm Hg, with pulse pressures often exceeding 100
mm Hg, although younger patients with more compliant vessels may have a less widened pulse pressure.Слайд 74The structural abnormalities (aortic dilation, prosthetic valve dislodgement, aortic valvular
calcification) or functional compromise (pulmonary edema, cardiomegaly).
Chest radiography
Слайд 76Echocardiography:
Aortic valve structure and morphology - Bileaflet versus trileaflet, flail,
thickening
Presence of vegetations or nodules - May require transesophageal echocardiography
in selected casesSeverity of AR
Color Doppler jet width
Regurgitant volume, fraction, and orifice area
Слайд 77Echocardiography:
Premature closure of the mitral valve (seen in severe AR)
and opening of the aortic valve (with severely elevated LV
end-diastolic pressure)Pressure half-time - Usually less than 300-350 ms with significant AR
Associated lesions of the aorta - Including dilation, aneurysm, dissection, or ectasia
LV structure and function
LV hypertrophy and dilation
Ejection fraction (EF) and end-systolic dimension
Слайд 79Other methods of diagnostics:
Radionuclide imaging (may provide complementary clinical information,
including the AR regurgitant fraction and the LV/right ventricular (RV)
stroke volume ratio.Aortic angiography (may provide useful information regarding the severity of the patient's AR).
Cardiac Catheterization.
Cardiac CT scanning and magnetic resonance imaging (MRI).
Слайд 80Treatment
Regime depends on the severity of chronic heart failure.
Diet №
10-A or 10 (depending on the severity of CHF).
MEDICAL:
Treatment
of the main disease (chronic rheumatic heart disease). Treatment chronic heart failure.
Слайд 82Trends in choice of prosthesis
· Age less than 55 years
- Aortic allograft or pulmonary autograft
· Age between 55-75 years
- Mechanical prosthesis· Age greater than 75 years - Porcine heterograft, stented or stentless
· Allografts and autografts enlarge the orifice by about 2 mm, porcine heterografts reduce valve size by about 2 mm, and mechanical valves reduce valve size by about 5-8 mm