Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Darji maulik s. Topic : 11
Содержание
- 1. Darji maulik s. Topic : 11
- 2. Cesarean section is obstetrical operation with the
- 3. Historical BackgroundIn the first, according to legend,
- 4. ContinuationThe second explanation is that the name
- 5. ContinuationThe third explanation is that the word
- 6. Слайд 6
- 7. The recommended percentage of caesarean sections (WHO, 2008) – 10-15%.
- 8. WHO: every year the world produces about
- 9. Maternal death associated with caesarean
- 10. Caesarean section increases the risk
- 11. Selected Complications Associated with Emergency Cesarean Delivery
- 12. Methods (types) of Cesarean section: Intraperitoneal Cesarean
- 13. Today, one of the most frequent indications
- 14. Indications for Cesarean Section during pregnancy (planned
- 15. CONTINUATIONCicatricial deformity of cervix and vagina after
- 16. Слайд 16
- 17. Severe extragenital pathology:III degree of arterial hypertension.Aortal
- 18. Indications for Cesarean Section during labor (urgent):Clinically
- 19. Слайд 19
- 20. Conditions for Cesarean section:Alive fetus (besides massive
- 21. Anesthetic management of Cesarean section: Endotracheal anesthesia.Epidural anesthesia.In exceptional cases – local infiltration anesthesia.
- 22. Indications for corporeal cesarean section: Inaccessibility
- 23. Contraindications for intraperitoneal Cesarean section: Extragenital infections.Water
- 24. Preparation of woman for Cesarean section:Cleansing
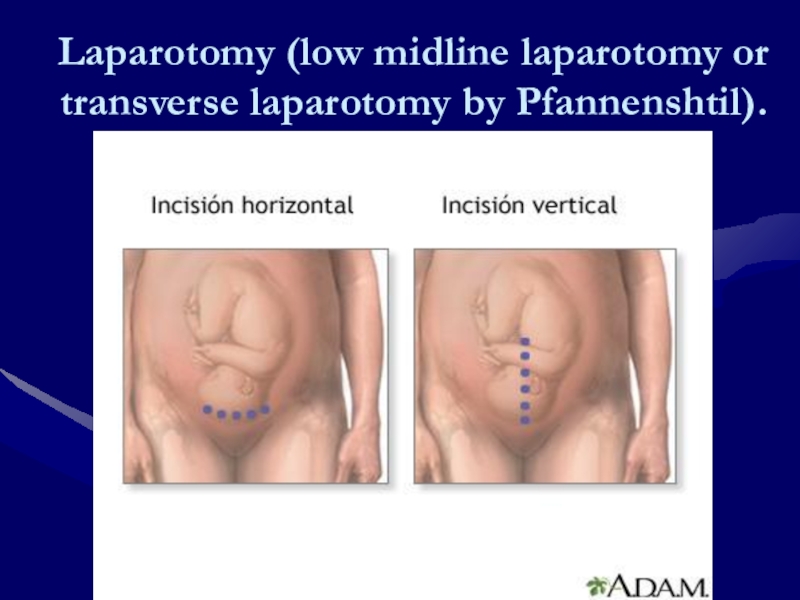
- 25. Laparotomy (low midline laparotomy or transverse laparotomy by Pfannenshtil).
- 26. Surgical technique: Laparotomy (low midline laparotomy or
- 27. CONTINUATIONStraight away the evacuation of child intravenous
- 28. Слайд 28
- 29. Слайд 29
- 30. Possible complications during operation: Bleeding. The first
- 31. Postoperative care for woman in early postoperative
- 32. ContinuationAfter transfer to her room, the woman
- 33. Postoperative care for woman in early postoperative
- 34. THANK YOU FOR YOUR ATTENTION!!!
- 35. Скачать презентанцию
Cesarean section is obstetrical operation with the help of which fetus and afterbirth are extracted from uterus throw incision of uterus and laparotomy incision.
Слайды и текст этой презентации
Слайд 2Cesarean section is obstetrical operation with the help of which
fetus and afterbirth are extracted from uterus throw incision of
uterus and laparotomy incision.Слайд 3Historical Background
In the first, according to legend, Julius Caesar was
born in this manner, with the result that the procedure
became known as the Caesarean operation. Several circumstances weaken this explanation.Слайд 4Continuation
The second explanation is that the name of the operation
is derived from a Roman law, supposedly created in the
8th century BC by Numa Pompilius, ordering that the procedure be performed upon women dying in the last few weeks of pregnancy in the hope of saving the child. This lex regia—king's rule or law—later became the lex caesarea under the emperors, and the operation itself became known as the caesarean operation. The German term Kaiserschnitt—Kaiser cut—reflects this derivation.Слайд 5Continuation
The third explanation is that the word caesarean was derived
from the Latin verb caedere, to cut. This explanation seems
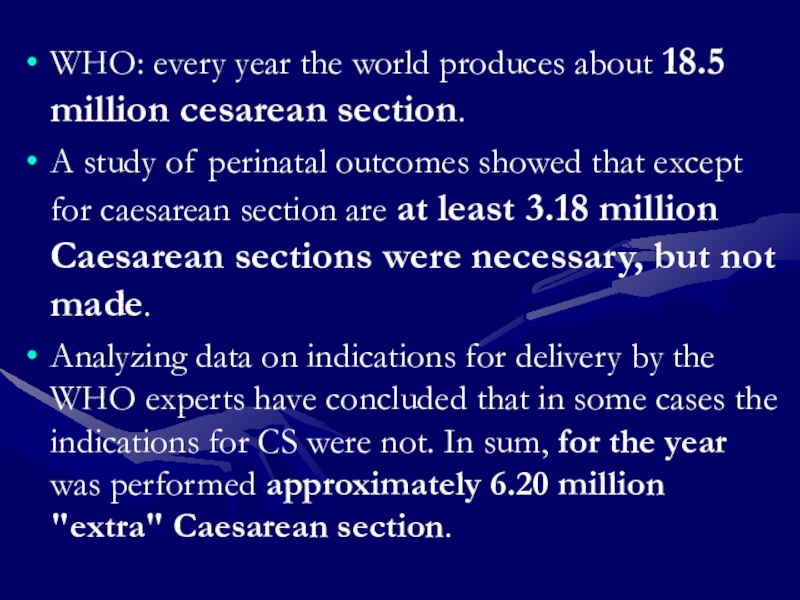
most logical, but exactly when it was first applied to the operation is uncertain. Because section is derived from the Latin verb seco, which also means cut, the term caesarean section seems tautological—thus cesarean delivery is used. In the United States, the ae in the first syllable of caesarean is replaced with the letter e. In the United Kingdom, Australia, and most commonwealth nations, the ae is retained.Слайд 8WHO: every year the world produces about 18.5 million cesarean
section.
A study of perinatal outcomes showed that except for caesarean
section are at least 3.18 million Caesarean sections were necessary, but not made.Analyzing data on indications for delivery by the WHO experts have concluded that in some cases the indications for CS were not. In sum, for the year was performed approximately 6.20 million "extra" Caesarean section.
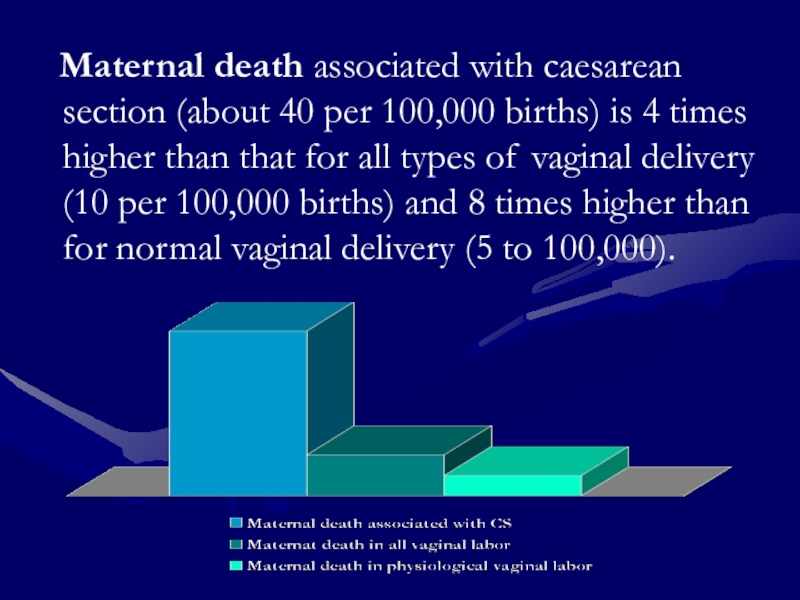
Слайд 9 Maternal death associated with caesarean section (about 40
per 100,000 births) is 4 times higher than that for
all types of vaginal delivery (10 per 100,000 births) and 8 times higher than for normal vaginal delivery (5 to 100,000).Слайд 10 Caesarean section increases the risk of serious complications
in the next pregnancy:
- ectopic pregnancy, - placenta previa,
- preeclampsia,
- birth of a child with a small for gestational period mass,
- anomalies of placenta,
- placental abruption,
- uterine rupture.
Слайд 11Selected Complications Associated with Emergency Cesarean Delivery (According to Decision-to-Incision
Interval from the Maternal-Fetal Medicine Units Network):
Maternal Outcome:
Endometritis,
Wound complication, Operative injury;Neonatal Outcome:
5-minute Apgar score less than 3, Umbilical artery pH <7.0, Hypoxic ischemic encephalopathy, Fetal death in labor, Neonatal death with or with no malformations.
Слайд 12Methods (types) of Cesarean section:
Intraperitoneal Cesarean section:
corporeal cesarean section
low cesarean
section (with the help of transverse incision in the inferior
uterine segment).Low cesarean section with temporary isolation of abdominal cavity.
Extraperitoneal cesarean section.
Cesarean section by Starc’s method.
Method of operation is determined by the obstetrical state, condition of woman, condition of fetus, doctor’s level of proficiency.
Слайд 13Today, one of the most frequent indications for elective caesarean
section is the presence of a uterine scar from a
previous caesarean section.According to the literature, repeated cesarean section involves a significant risk of maternal complications and increases the risk of placenta previa and increment the next pregnancy.
Слайд 14Indications for Cesarean Section during pregnancy (planned and urgent) are:
Central
type of placenta previa; Partial placental presentation with bleeding;
Premature detachment
of placenta with bleeding and/or intrauterine fetal distress;Failure of scar on uterus; Scar on uterus after corporal Cesarean section; Two or more scars on uterus;
Anatomically contracted pelvis III-IV degrees (conjugate Vera is lesser than 7.5 sm.) and infrequent forms of contracted pelvis;
Traumatic injury of pelvis and spinal column, condition after reparative operations;
Malformations of uterus and vagina, which put obstacles in for delivery;
Tumors of pelvic organs, which put obstacles in the way of delivery;
Absence of effects of treatment for severe gestosis if there are no condition for urgent delivery throw birth canal;
Слайд 15CONTINUATION
Cicatricial deformity of cervix and vagina after surgical treatment for
urogenital and cologenital abscess, fistulas;
Condition after 3 degree perineal tear
and plastic operations on perineum;Cancer of cervix;
HIV (Human Immunodeficiency Virus) infection in the mother with high viral load (more than 1000 copies);
Acute genital herpes during 3 weeks before the delivery;
Sterility, IVF, still birth in anamnesis in complex with other obstetrical pathology;
Varix of cervix, vagina;
Malpositions (transverse, oblique positions) of fetus;
Multiplied pregnancy and breech presentation or transverse (oblique) position of the first fetus; Conjoined twins; Triple or more pregnancy;
Breech presentation if the tentative mass of fetus is more than 3.700 gr.;
Severe fetal distress and absent conditions for urgent delivery throw the birth canal;
Слайд 17Severe extragenital pathology:
III degree of arterial hypertension.
Aortal coarctation. Aneurism of
aorta or of other big arteries.
Systolic dysfunction of left ventricle.
Latest
hemorrhage into retina on the background of diabetic or hypertensive angiopathy.Lung disorders with danger of pneumothorax. Lung bleeding lesser than 4 weeks before delivery.
Portal hypertension with varix of esophagus and stomach.
Splenomegaly, Diaphragmatic hernia.
Syndrome of liquor hypertension.
Condition after hemorrhage stroke.
Necessity to exclude labor pushing in case of absence of cephalic presentation.
Etc.
Слайд 18Indications for Cesarean Section during labor (urgent):
Clinically contracted pelvis;
Preterm amniotic
fluid discharge and ineffective labor induction;
Not treatable anomalies of birth
activity;Premature detachment of placenta with bleeding and/or intrauterine fetal distress;
Severe fetal distress and absent conditions for urgent delivery throw the birth canal;
Rupture of uterus (threatened rupture or beginning of rupture);
Prolapse of pulsing umbilical cord;
Malpresentations (vertex and brow presentations), high straight position of sagittate suture;
Agony or clinical death of mother and alive fetus.
Слайд 20Conditions for Cesarean section:
Alive fetus (besides massive bleeding in case
of complete placental presentation, premature detachment of placenta (abruption placentae),
IV degree of contraction of pelvis).Whole amniotic sac or waterless period lesser than 12 hours.
Absence of fever in the woman.
Organizational Conditions for Cesarean section:
Agreement of woman or her relatives for surgical delivery.
Choosing of the most optimal time for surgical delivery (fill-term pregnancy, beginning of operation in the beginning of labor).
Determination of type of antibiotic for prophylaxis.
Presence of conditions and experienced doctors.
Слайд 21Anesthetic management of
Cesarean section:
Endotracheal anesthesia.
Epidural anesthesia.
In exceptional cases –
local infiltration anesthesia.
Слайд 22Indications for corporeal
cesarean section:
Inaccessibility of inferior uterine segment due
to postoperative adhesions after the previous cesarean section.
Transverse position of
fetus and back presentation.Malformations of fetus (conjoined twins).
Big interstitial myoma in the inferior uterine segment.
Mostly evident vascularity of inferior uterine segment due to placenta previa or cancer of cervix.
Слайд 23Contraindications for intraperitoneal Cesarean section:
Extragenital infections.
Water loss period more than
12 hours.
Intrauterine death of the fetus (besides premature detachment of
placenta and central tipes of placenta previa). Слайд 24Preparation of woman for
Cesarean section:
Cleansing of vagina by local
vaginal anti-infective drugs.
Putting the woman onto surgical table with the
prophylaxis of inferior vena cava syndrome (surgical table must be slightly bended to the left).Mobilization of vein and intravenous infusion of blood substitutes.
Urinary bladder catheterization and urine evacuation.
Scrubbing of surgeon’s hands.
Abdominal cleansing preparation.
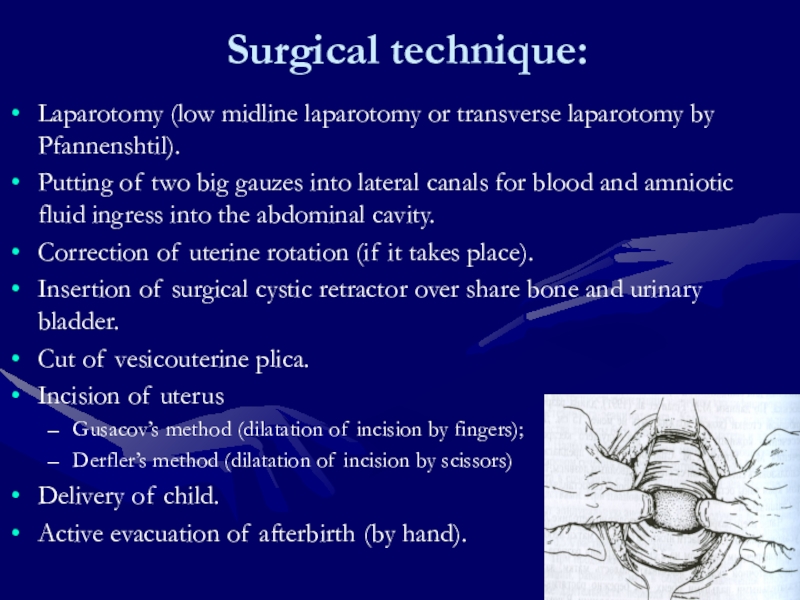
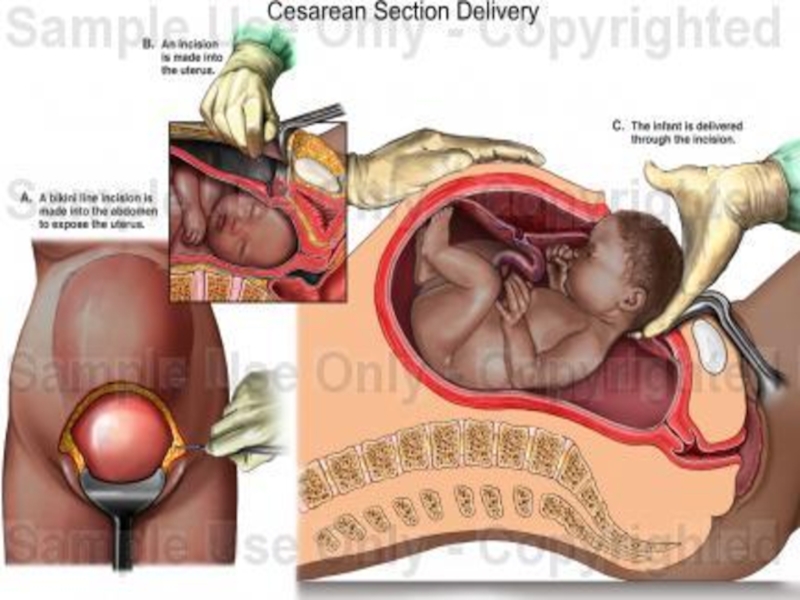
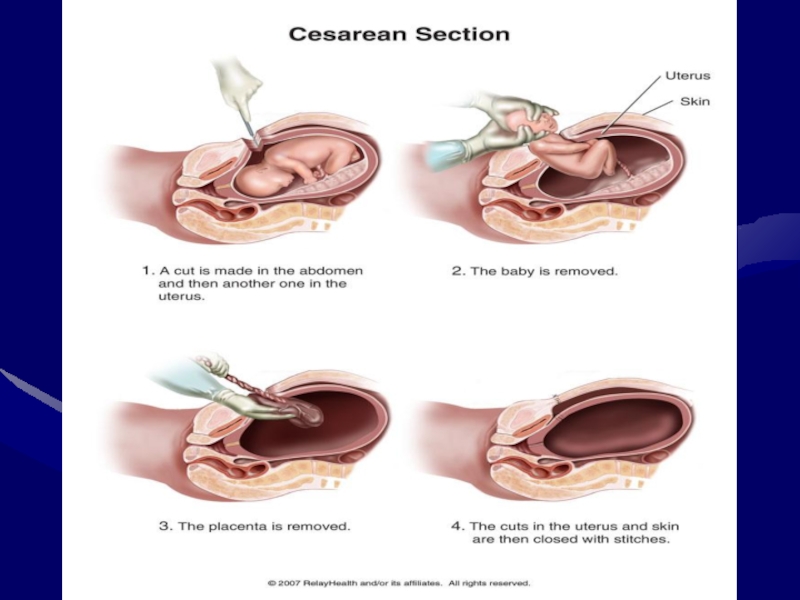
Слайд 26Surgical technique:
Laparotomy (low midline laparotomy or transverse laparotomy by Pfannenshtil).
Putting
of two big gauzes into lateral canals for blood and
amniotic fluid ingress into the abdominal cavity.Correction of uterine rotation (if it takes place).
Insertion of surgical cystic retractor over share bone and urinary bladder.
Cut of vesicouterine plica.
Incision of uterus
Gusacov’s method (dilatation of incision by fingers);
Derfler’s method (dilatation of incision by scissors)
Delivery of child.
Active evacuation of afterbirth (by hand).
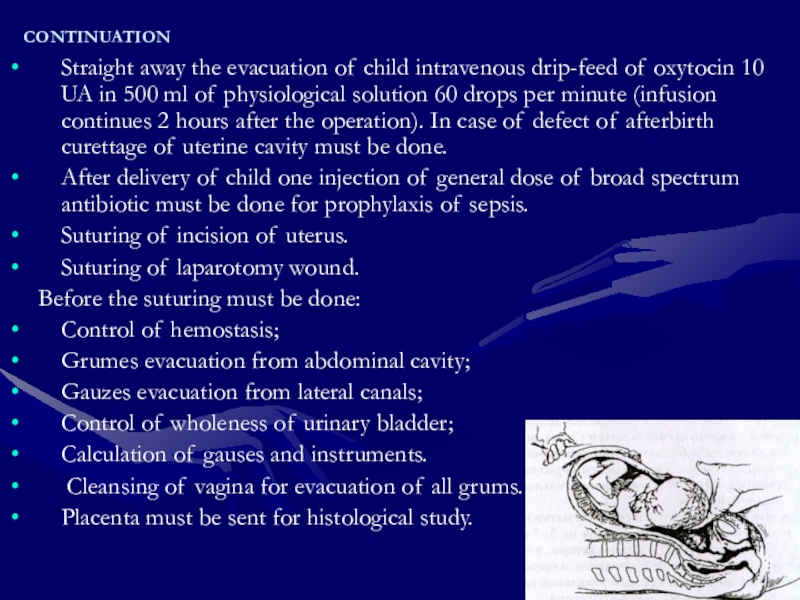
Слайд 27CONTINUATION
Straight away the evacuation of child intravenous drip-feed of oxytocin
10 UA in 500 ml of physiological solution 60 drops
per minute (infusion continues 2 hours after the operation). In case of defect of afterbirth curettage of uterine cavity must be done.After delivery of child one injection of general dose of broad spectrum antibiotic must be done for prophylaxis of sepsis.
Suturing of incision of uterus.
Suturing of laparotomy wound.
Before the suturing must be done:
Control of hemostasis;
Grumes evacuation from abdominal cavity;
Gauzes evacuation from lateral canals;
Control of wholeness of urinary bladder;
Calculation of gauses and instruments.
Cleansing of vagina for evacuation of all grums.
Placenta must be sent for histological study.
Слайд 30Possible complications during operation: Bleeding. The first aid:
Uterine massage.
Intravenous drip-feed
of oxytocin and intramuscular injection of Ergomethrine 0.2 mg. and
prostoglandins.Infusion of blood substitutes or blood transfusion of necessity.
In case of absence of effect of treatment and uterine atony - hysterectomy or great uterine vessels ligation.
Слайд 31Postoperative care for woman in early postoperative period:
Recovery Suite
Postoperatively, the
amount of bleeding from the vagina must be monitored closely,
and the uterine fundus must be identified frequently by palpation to ensure that the uterus is remaining firmly contracted.Once the mother is fully awake, bleeding is minimal, blood pressure is satisfactory, and urine flow is at least 50 mL/hour, she may be transferred to her room.
Слайд 32Continuation
After transfer to her room, the woman is assessed at
least hourly for 4 hours and thereafter, at intervals of
4 hours.Blood pressure, pulse, temperature, uterine tone, urine output, and amount of bleeding are evaluated.
The incision is inspected each day. By the third postpartum day, showering is not harmful to the incision.