Слайд 1Мeningeal syndrome
in clinic
of infectious diseases
Meningococcal infection
Слайд 2MENINGITIS - inflammation of meninges of brain and spinal cord.
Acute meningitis plays a leading role in infectious pathology of
the central nervous system. The majority of researchers propose to classify meningitis by the following criteria:
By appearance:
• Primary - occurs without any preceding infection
or local inflammation as an independent disease
• Secondary – occurs as a complication of general
or local infectious process;
According to etiology:
• Bacterial
• Viral
• Fungal
• Spirochetosis
• Rickettsial
• Protozoal
• Helminthic
• Combined
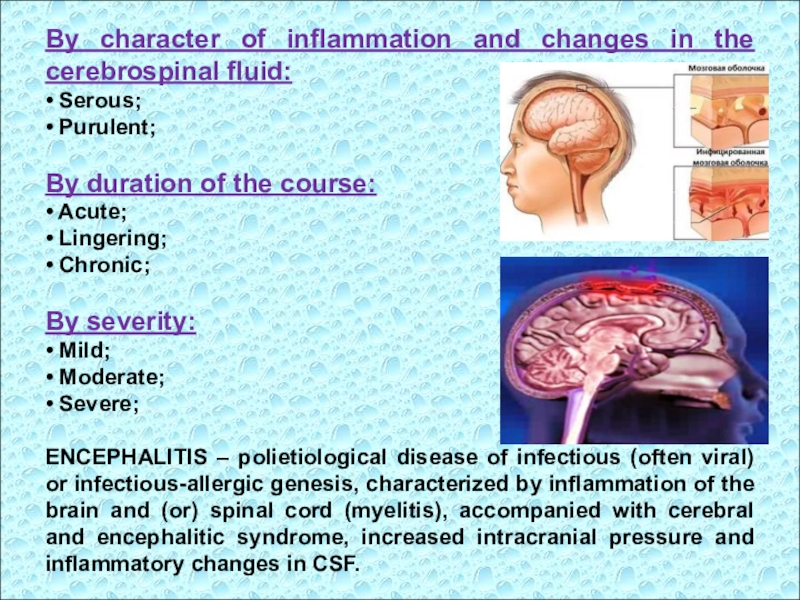
Слайд 3By character of inflammation and changes in the cerebrospinal fluid:
•
Serous;
• Purulent;
By duration of the course:
• Acute;
• Lingering;
• Chronic;
By severity:
•
Mild;
• Moderate;
• Severe;
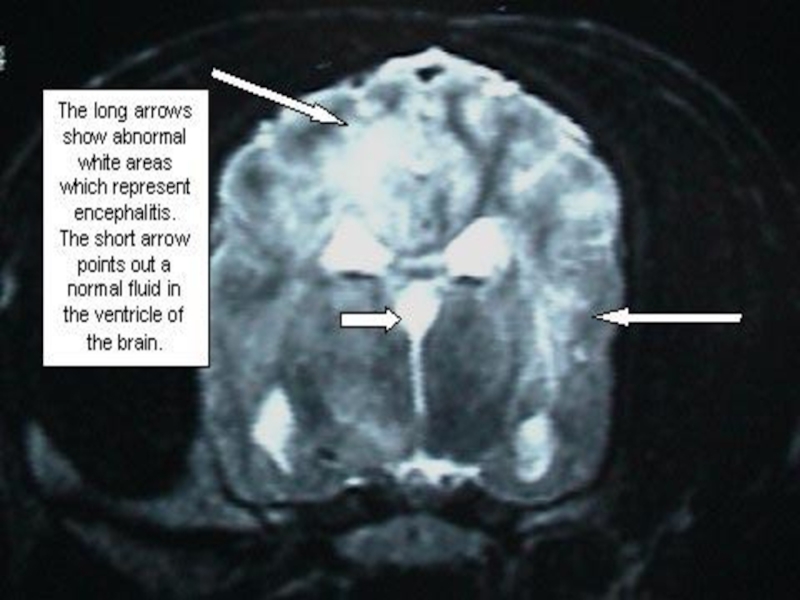
ENCEPHALITIS – polietiological disease of infectious (often viral) or infectious-allergic genesis, characterized by inflammation of the brain and (or) spinal cord (myelitis), accompanied with cerebral and encephalitic syndrome, increased intracranial pressure and inflammatory changes in CSF.
Слайд 4PATHOGENESIS
The entrance gates for causative agent can be:
nasopharynx,
respiratory
tract,
intestine,
primary focal inflammation;
Dissemination of the pathogen occurs
by:
hematogenous,
lymphogenous,
contact way.
3 pathogenetic factors play an important role
in the development of the disease:
bacteremia,
toxemia,
macroorganism (initial immunity)
Слайд 5- Destruction of bacteria,
- releasing of endotoxins,
- development of toxemia,
-
increased levels of biologically active substances,
products of disturbed metabolism
Leads to
- increased permeability of cellular and vascular membranes,
blood-brain barrier;
- active penetration of bacteria and toxins in the CNS
with development of the pathological process.
irritation of the vascular plexus of brain ventricles
(by bacteria, antigens, toxins and immune complexes);
increase of cerebrospinal fluid production and intracranial
pressure.
Слайд 6Irritation of structures of the diencephalic region
(centers of thermoregulation, vomiting
and vascular) causes the main clinical manifestations of the disease
(headache,
repeated vomiting, meningeal symptoms).
The complex of symptoms of acute meningitis consists of 4 major syndromes:
general intoxication,
cerebral sd,
meningeal syndrome,
sd of inflammatory changes in the cerebrospinal fluid.
General intoxication:
- acute onset with fever (febrile),
- pale skin,
- chills, lethargy, weakness,
- anorexia,
- tachypnea, dyspnea,
- tachycardia, muffled tones of the heart, changing heart rate,
unstable blood pressure.
Слайд 7Cerebral syndrome:
headache – strong, diffused, sometimes local, increases when
changing body position (due to high intracranial pressure and irritation
of pain receptors by pathogen toxins);
vomiting - has a central mechanism (due to a direct irritation of the vomiting center), repeated, occurs suddenly, without previous nausea, does not bring relief, increases when change body position;
possible disturbance of consciousness
(from agitation to somnolence, stupor and coma);
seizures (from twitching of some
muscles to generalized convulsions and convulsive status);
expansion of veins on the head, eyelids and eyes.
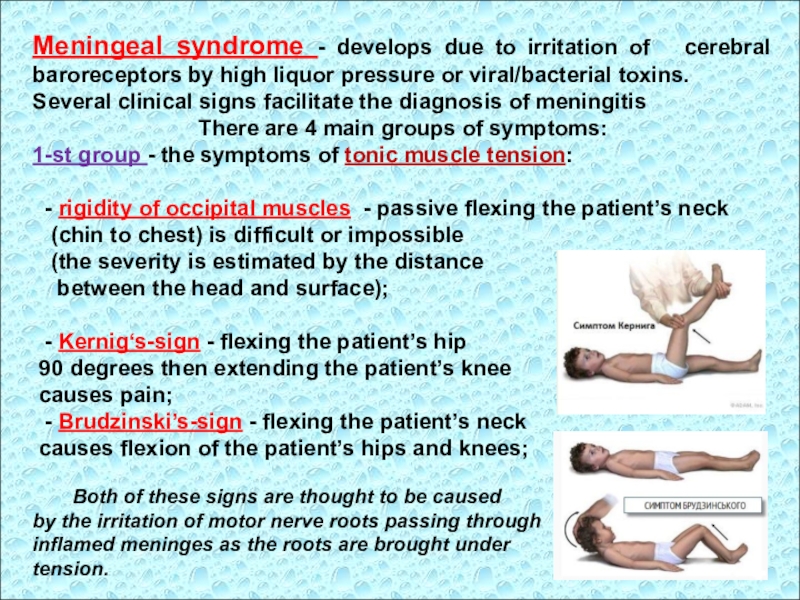
Слайд 8Meningeal syndrome - develops due to irritation of cerebral
baroreceptors by high liquor pressure or viral/bacterial toxins.
Several clinical
signs facilitate the diagnosis of meningitis
There are 4 main groups of symptoms:
1-st group - the symptoms of tonic muscle tension:
- rigidity of occipital muscles - passive flexing the patient’s neck
(chin to chest) is difficult or impossible
(the severity is estimated by the distance
between the head and surface);
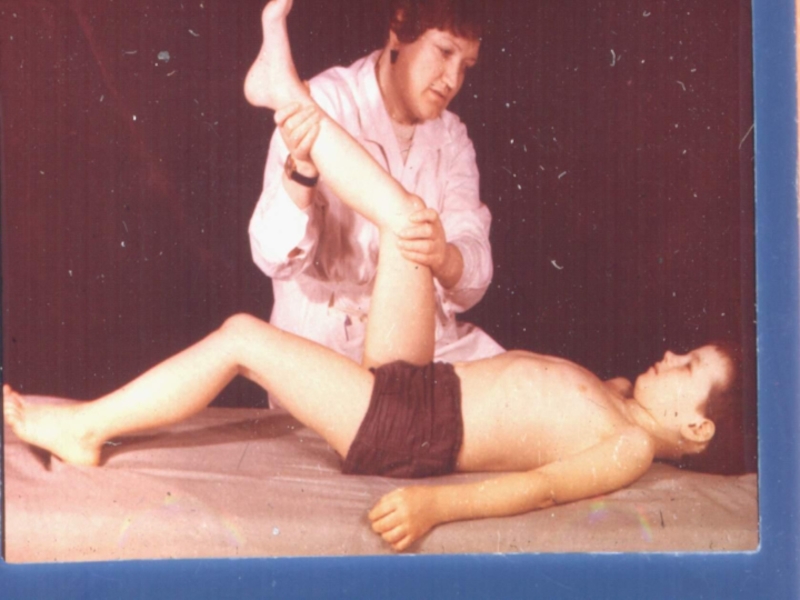
- Kernig‘s-sign - flexing the patient’s hip
90 degrees then extending the patient’s knee
causes pain;
- Brudzinski’s-sign - flexing the patient’s neck
causes flexion of the patient’s hips and knees;
Both of these signs are thought to be caused
by the irritation of motor nerve roots passing through
inflamed meninges as the roots are brought under
tension.
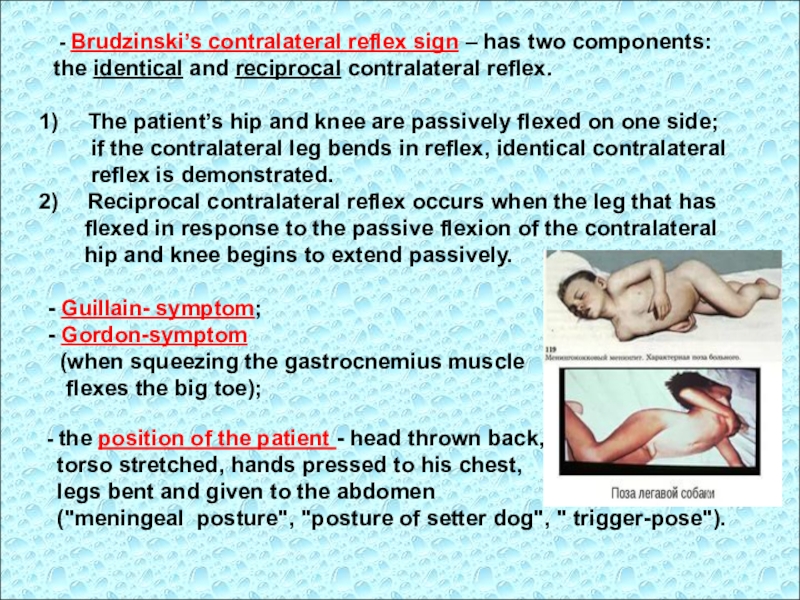
Слайд 9
- Brudzinski’s contralateral reflex sign – has two
components:
the identical and reciprocal contralateral reflex.
The patient’s hip
and knee are passively flexed on one side;
if the contralateral leg bends in reflex, identical contralateral
reflex is demonstrated.
Reciprocal contralateral reflex occurs when the leg that has
flexed in response to the passive flexion of the contralateral
hip and knee begins to extend passively.
- Guillain- symptom;
- Gordon-symptom
(when squeezing the gastrocnemius muscle
flexes the big toe);
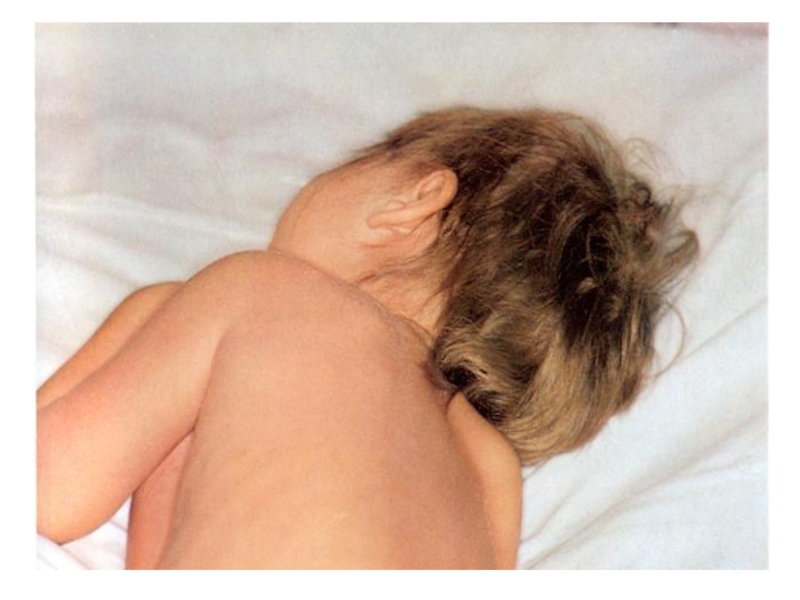
- the position of the patient - head thrown back,
torso stretched, hands pressed to his chest,
legs bent and given to the abdomen
("meningeal posture", "posture of setter dog", " trigger-pose").
Слайд 102-d group – symptoms of general hyperesthesia and hypersensitivity of
the sensory organs (photophobia, hyperacusia) due to irritation of the
posterior roots, cells of the spinal nodes, receptors of meninges, and dicreased level of sensitivity to various stimuli.
3-d group - reactive pain phenomena:
- Bekchterev-symptom;
Lobzin-symptom (painful grimace when pressing on the eyeballs
through closed eyelids);
- Kerer‘s symptom (pain in points of the trigeminal nerve);
- Pulatov-symptom (tenderness to percussion of the skull);
Mendel's symptom (pain when pressure on the frontal wall of the
external ear canal).
4-th group – changed dermal, pariosteal and tendon reflexes:
- Babinsky-reflex;
- Oppenheim-reflex;
- Gordon's reflex (pinching the gastrocnemius muscle);
- Sheffer’s reflex (compression of the Achilles tendon);
- Rossolimo-reflex.
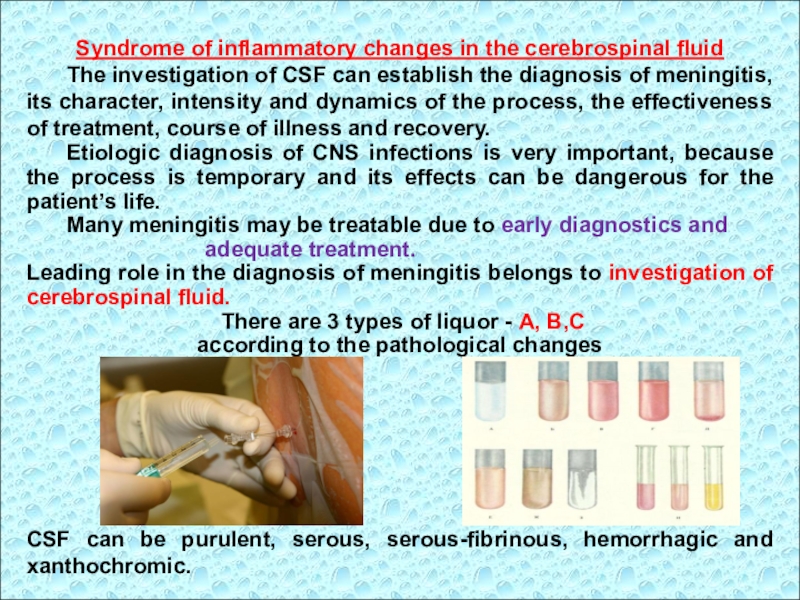
Слайд 11Syndrome of inflammatory changes in the cerebrospinal fluid
The investigation of
CSF can establish the diagnosis of meningitis, its character, intensity
and dynamics of the process, the effectiveness of treatment, course of illness and recovery.
Etiologic diagnosis of CNS infections is very important, because the process is temporary and its effects can be dangerous for the patient’s life.
Many meningitis may be treatable due to early diagnostics and
adequate treatment.
Leading role in the diagnosis of meningitis belongs to investigation of cerebrospinal fluid.
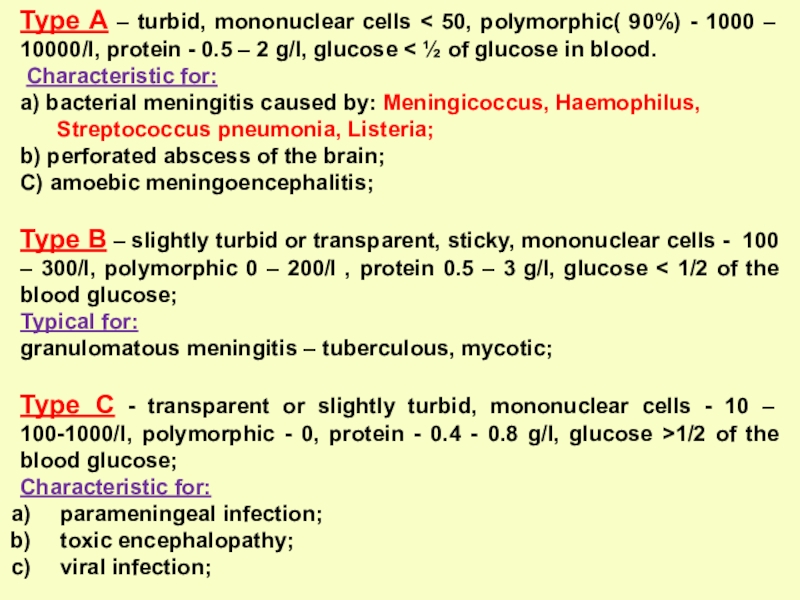
There are 3 types of liquor - A, B,C
according to the pathological changes
CSF can be purulent, serous, serous-fibrinous, hemorrhagic and xanthochromic.
Слайд 12Inflammation of meninges is accompanied by the following changes of
CSF:
• Increased pressure - cerebrospinal fluid is flowing streamly or
by frequent drops.
• Change in transparency (cloudy) or color (white, yellow-green etc.) depending on the etiology of the process.
• Pleocytosis with a predominance of neutrophils, lymphocytes, or mixed.
• Increase the protein content.
• Change in the level of glucose
and chlorides.
Type A – turbid, mononuclear cells < 50, polymorphic( 90%)
- 1000 – 10000/l, protein - 0.5 – 2 g/l, glucose < ½ of glucose in blood.
Characteristic for:
a) bacterial meningitis caused by: Мeningicoccus, Haemophilus,
Streptococcus pneumonia, Listeria;
b) perforated abscess of the brain;
C) amoebic meningoencephalitis;
Type B – slightly turbid or transparent, sticky, mononuclear cells - 100 – 300/l, polymorphic 0 – 200/l , protein 0.5 – 3 g/l, glucose < 1/2 of the blood glucose;
Typical for:
granulomatous meningitis – tuberculous, mycotic;
Type C - transparent or slightly turbid, mononuclear cells - 10 – 100-1000/l, polymorphic - 0, protein - 0.4 - 0.8 g/l, glucose >1/2 of the blood glucose;
Characteristic for:
parameningeal infection;
toxic encephalopathy;
viral infection;
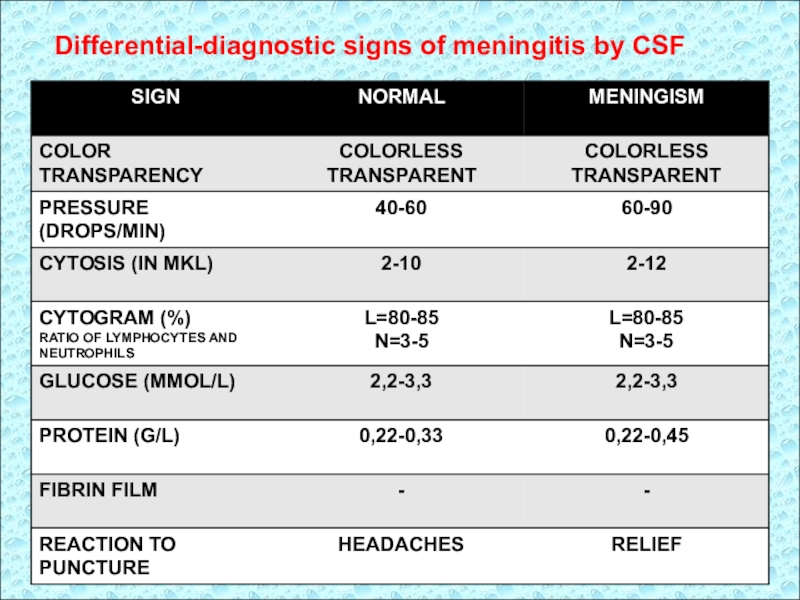
Слайд 14Differential-diagnostic signs of meningitis by CSF
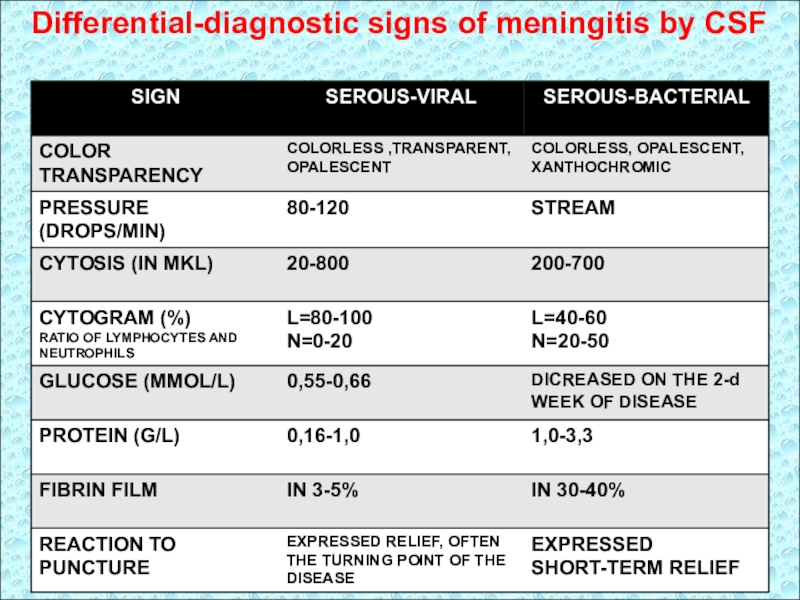
Слайд 15Differential-diagnostic signs of meningitis by CSF
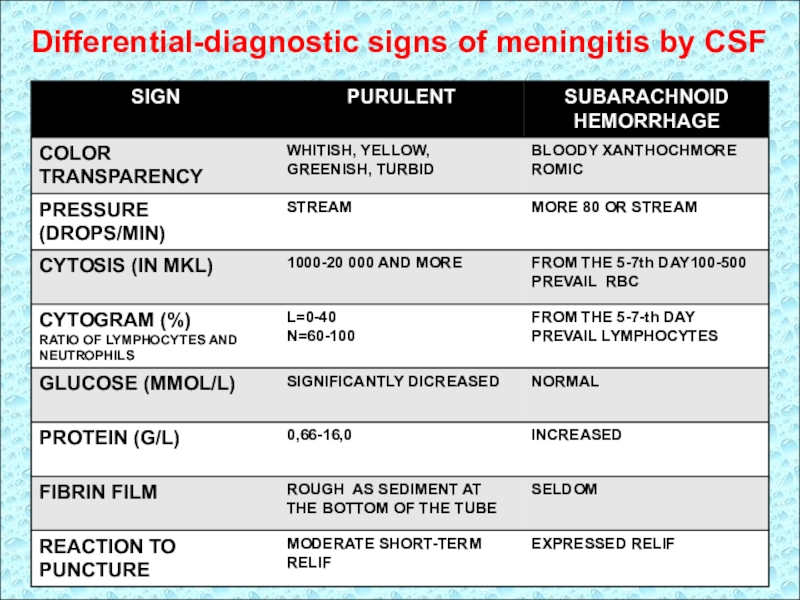
Слайд 16Differential-diagnostic signs of meningitis by CSF
Слайд 17Primary purulent meningitis is of meningococcal, pneumococcal, Haemophilus influenzae etiology.
Secondary
purulent meningitis developed as a complication of sepsis, diseases of
ENT-organs (otitis, mastoiditis, mastoiditis, sinusitis), lungs, kidneys and other organs and is most often caused by staphylococci, streptococci, Pseudomonas aeruginosa etc., Fungi, protozoa, helminths are rare pathogens.
Слайд 18Diagnostic criteria of primary purulent meningitis
Meningococcal infection – is acute
respiratory infection, antroponosis, with aerogenic mechanism of transmission, pathogenically is
characterized by the destruction of respiratory epithelium, clinically - intoxication, rhinopharyngitis, affection of CNS and sepsis-like state.
• Anamnesis
– winter-spring seasonality
(strong seasonality now is not seen);
route of transmission is airborne droplets, realized through close contact (within 2 hours at a distance of 30 – 50 cm);
source of infection - is sick of any form of meningococcal disease patient or carrier;
risk group - children under 1 year, the elderly , persons with chronic pathology of RT, ENT-organs, immunosuppression;
frequency of incidence is 8-10 years.
Слайд 19
EPIDEMIOLOGY - anthroponosis
Source: Epidemiological danger
- patients with
generalised forms of disease
- patients with a nasopharyngitis
- carriers of N.m.
Duration of infectious period 3 - 4 weeks.
Patients are INFECTIOUS - during a prodromal and acute
phases of disease!!!
Mortality in meningitis is 3-5%,
meningococcemia - to 20%.
Слайд 20Causative agent - Neisseria meningitidis
- Small gram-negative diplococci;
- typical location in a pair of coffee beans;
-
do not form spores, the capsule is nonconstant;
- nonmotile;
- aerobic, obligate intracellular microbe;
- grows on artificial nutrient media (blood agar);
- for capsular AG allocate nine serogroups (A, B, C, D, X, Y, Z, W135 and E);
- releases endotoxin;
- produces hyaluronidase and neuraminidase;
- secretes IgA-proteases that cleave the IgA molecule that protects
the bacteria from Ig;
- nonstable in environment;
- sensitive to drying and cooling, to penicillin, tetracycline,
erythromycin and disinfectants
Слайд 23
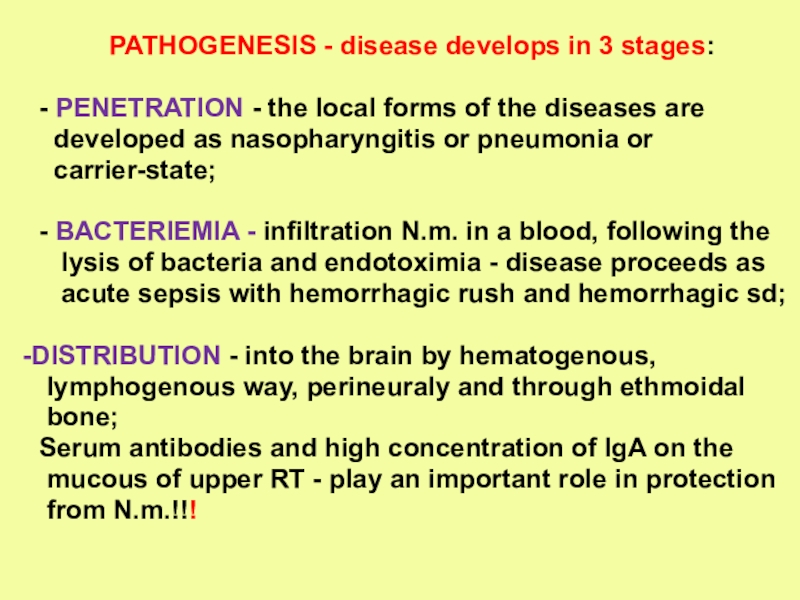
PATHOGENESIS - disease develops in 3 stages:
- PENETRATION -
the local forms of the diseases are
developed as
nasopharyngitis or pneumonia or
carrier-state;
- BACTERIEMIA - infiltration N.m. in a blood, following the
lysis of bacteria and endotoximia - disease proceeds as
acute sepsis with hemorrhagic rush and hemorrhagic sd;
DISTRIBUTION - into the brain by hematogenous,
lymphogenous way, perineuraly and through ethmoidal
bone;
Serum antibodies and high concentration of IgA on the
mucous of upper RT - play an important role in protection
from N.m.!!!
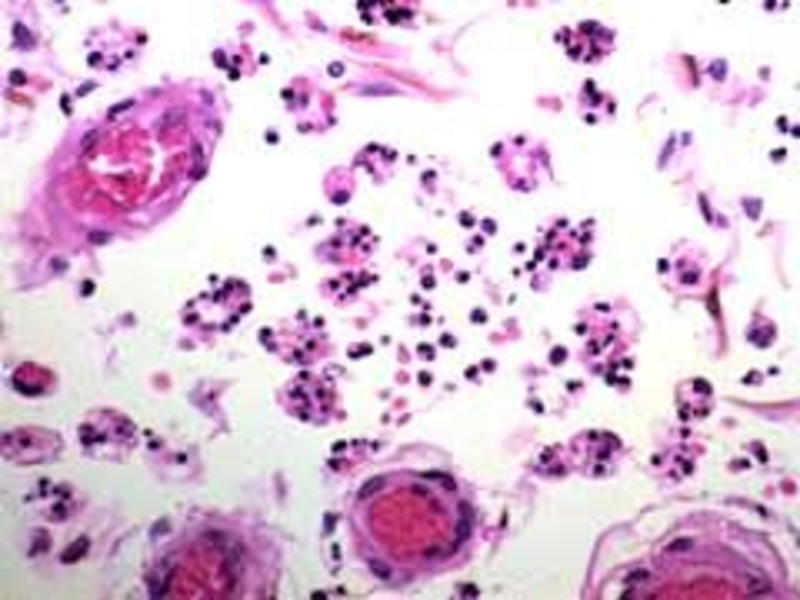
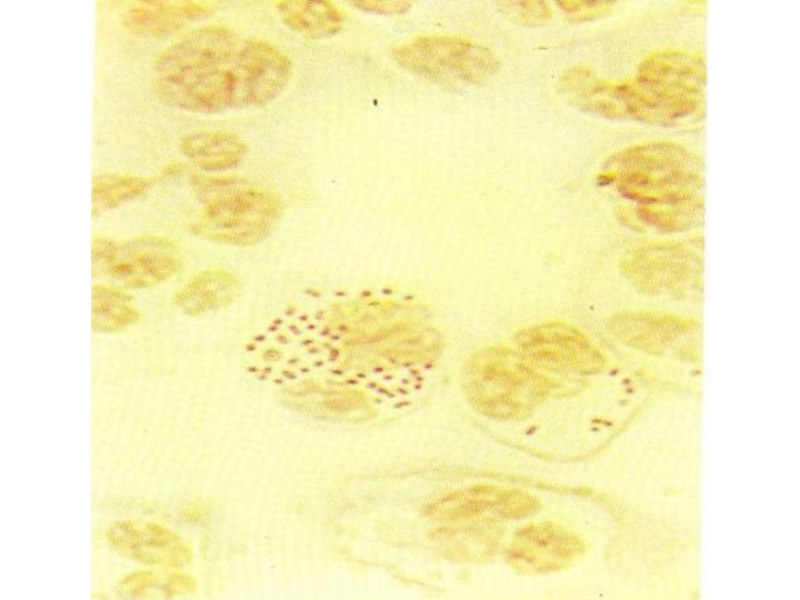
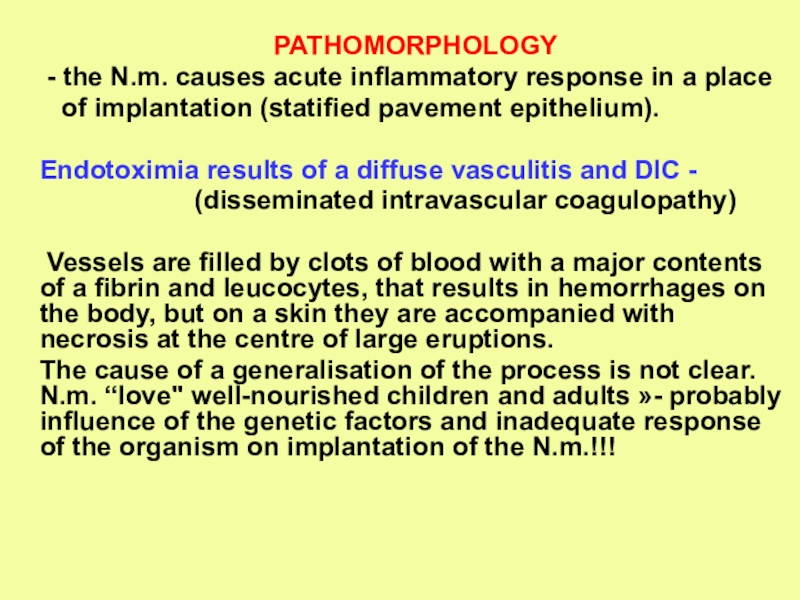
Слайд 24
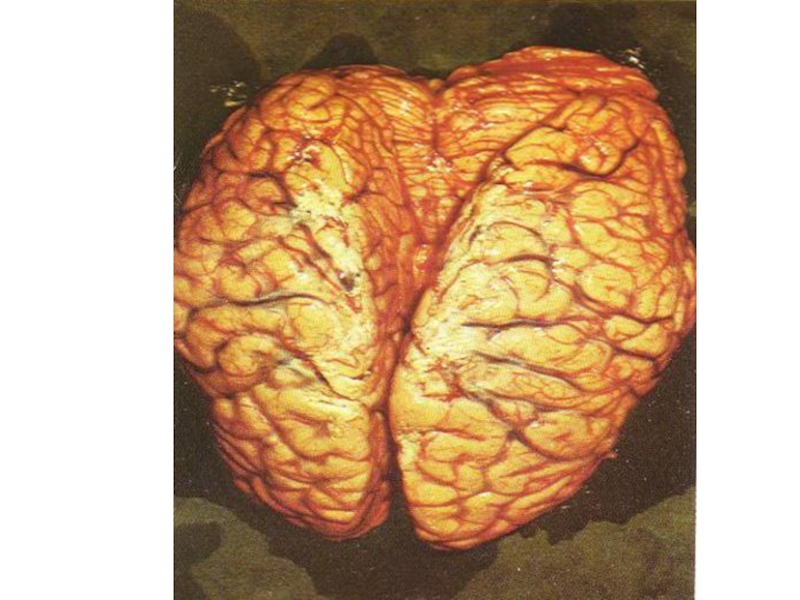
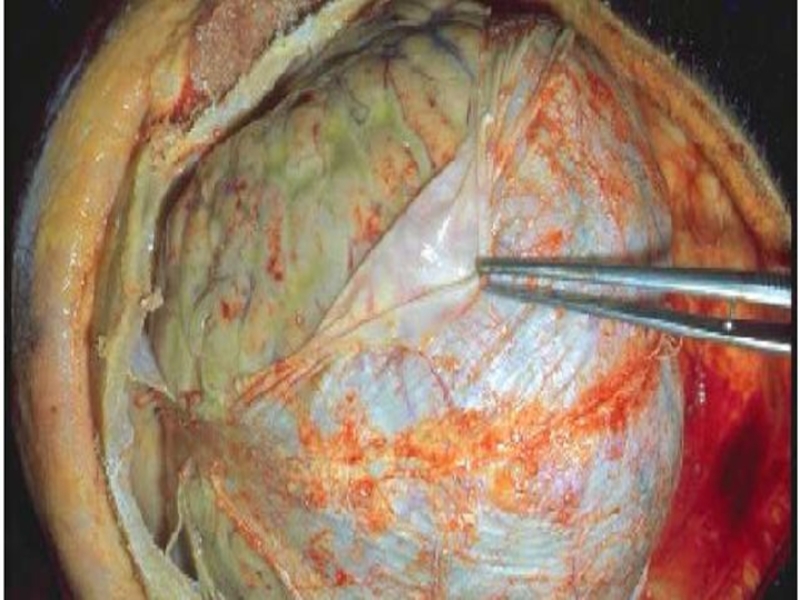
PATHOMORPHOLOGY
- the N.m. causes acute inflammatory response in a
place
of implantation (statified pavement epithelium).
Endotoximia results
of a diffuse vasculitis and DIC -
(disseminated intravascular coagulopathy)
Vessels are filled by clots of blood with a major contents of a fibrin and leucocytes, that results in hemorrhages on the body, but on a skin they are accompanied with necrosis at the centre of large eruptions.
The cause of a generalisation of the process is not clear. N.m. “love" well-nourished children and adults »- probably influence of the genetic factors and inadequate response of the organism on implantation of the N.m.!!!
Слайд 25
CLASSIFICATION
Localized forms:
- Carriage –without clinical manifestation,
can be revealed
by detection of N.m. in culture
and smears from a
nasopharynx;
- Nasopharyngitis;
- Meningococcal pneumonia;
Generalized forms:
- Meningococcal sepsis (acute and chronic)
- Meningitis
- Meningoencephalitis
- Mixed (sepsis + meningitis and etc. )
- Infrequent forms of disease: endocarditis, arthritis,
pneumonia, iridocyclitis, otitis etc.)
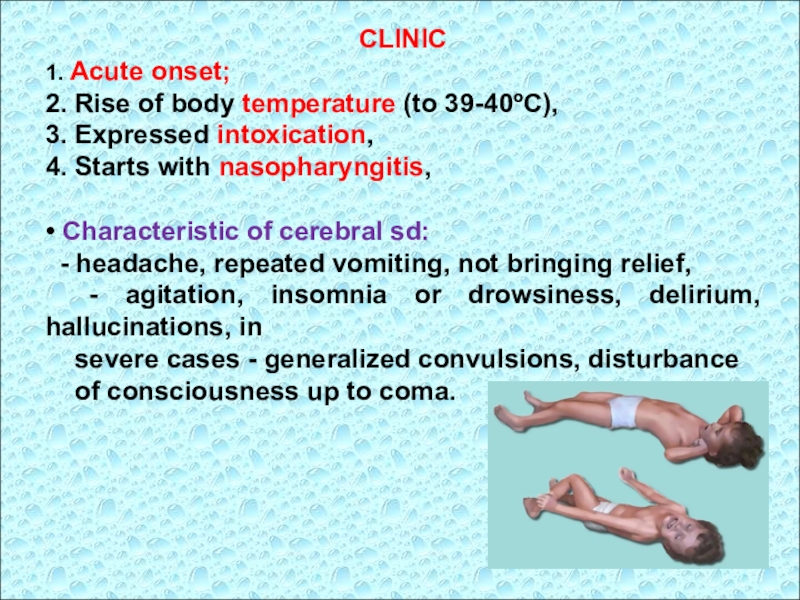
Слайд 26CLINIC
1. Acute onset;
2. Rise of body temperature (to 39-40ºC),
3. Expressed
intoxication,
4. Starts with nasopharyngitis,
• Characteristic of cerebral sd:
- headache,
repeated vomiting, not bringing relief,
- agitation, insomnia or drowsiness, delirium, hallucinations, in
severe cases - generalized convulsions, disturbance
of consciousness up to coma.
Слайд 27• Meningeal syndrome appears in the first days of the
disease of different severity:
often occurs with development of edema-
swelling of brain
(the attacks of psychomotor agitation);
1-1,5% of the patients revealed signs
of encephalitis (paralysis of the facial muscles
paraparesis, paralysis, disorder of coordination);
affection of cranial nerves;
visual and auditory hallucinations, euphoria or
depression;
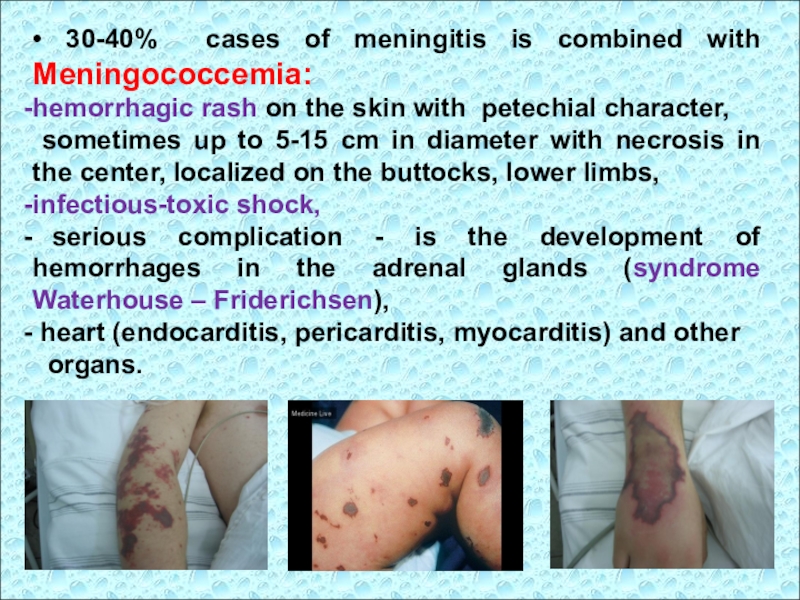
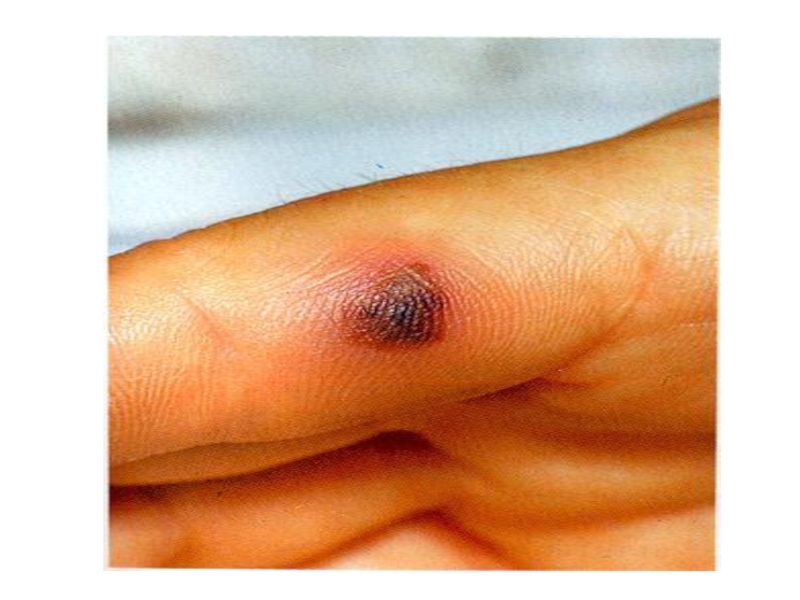
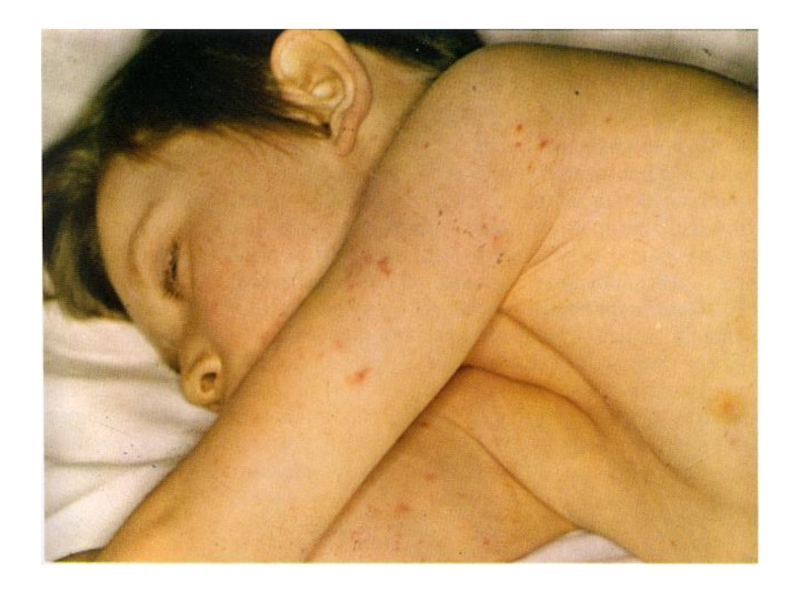
Слайд 28• 30-40% cases of meningitis is combined with Meningococcemia:
hemorrhagic rash
on the skin with petechial character,
sometimes up to 5-15
cm in diameter with necrosis in the center, localized on the buttocks, lower limbs,
infectious-toxic shock,
serious complication - is the development of hemorrhages in the adrenal glands (syndrome Waterhouse – Friderichsen),
heart (endocarditis, pericarditis, myocarditis) and other
organs.
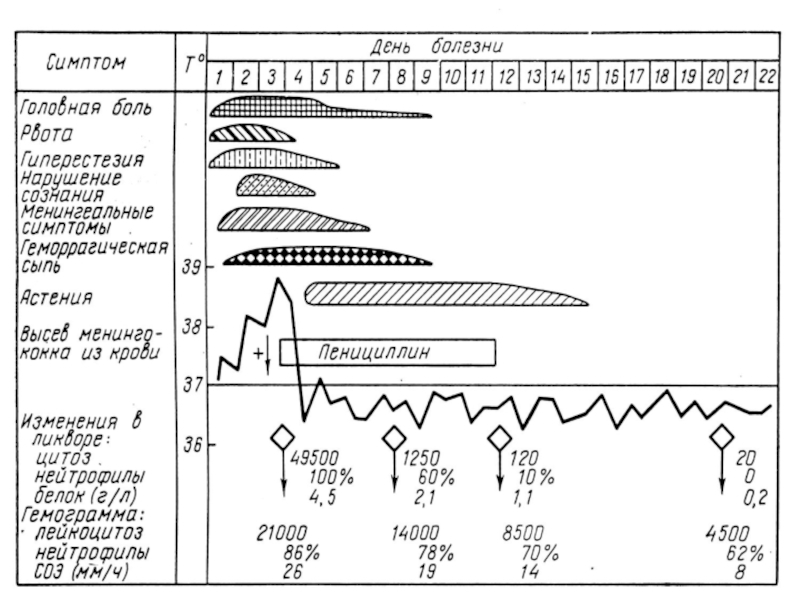
Слайд 29• CBC: leukocytosis, neutrophilia, shift of the formula to myelocytes,
lymphopenia, increased ESR.
• CSF:
is cloudy, yellow-colored,
flows streamly,
protein
is increased to 1g/l,
count of neutrophils - more than 1,000 cells in 1 ml,
in the first hours of the disease can be seen only
increased CSF pressure or signs of serous meningitis,
• Microscopy of CSF, thick drops of blood or discharging from the nasopharynx can be used to detect gram-negative diplococci, located intracellular.
Слайд 30• Bacteriological examination of mucus from the nasopharynx, blood, cerebrospinal
fluid is leading in the diagnosis of meningococcal disease.
Material
for bac. exam. should be taking before etiotropic therapy;
• Serology (RIHA) carried out with diagnostics of meningococci of group A and C (conditionally diagnostic titer of antibodies in adults 1:40-1:80).
In severe meningococcal infection and infectious-toxic shock antibodies are detected in low titers, and in some cases not detected at all.
Слайд 31
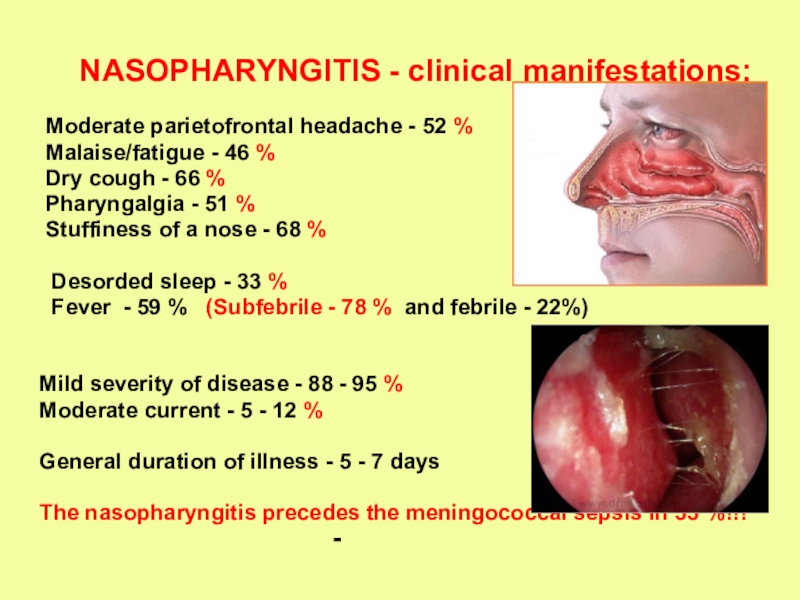
NASOPHARYNGITIS - clinical manifestations:
Moderate parietofrontal headache
- 52 %
Malaise/fatigue - 46 %
Dry cough -
66 %
Pharyngalgia - 51 %
Stuffiness of a nose - 68 %
Desorded sleep - 33 %
Fever - 59 % (Subfebrile - 78 % and febrile - 22%)
Mild severity of disease - 88 - 95 %
Moderate current - 5 - 12 %
General duration of illness - 5 - 7 days
The nasopharyngitis precedes the meningococcal sepsis in 33 %!!!
Слайд 32
MENINGOCOCCAL SEPSIS:
- acute beginning with chill and fast rise
of intermittent
temperature up to 38 - 40ºC
expressed intoxication (headache, thirst, weakness,
paleness and dryness of a skin)
appearance of hemorrhagic syndrome: hemorrhagic rush
with necrosis on the skin of buttocks, legs, trunk, arms,
eyelids (in 2-4-6 hours from the onset of disease!!!)
- enanthema in a transitive folds of conjuctiva, hemorrhages
on sclera
the hemorrhages in joints - on 5 - 13 % are more often
than in fingers and legs
- common manifestations of a hemorrhagic syndrome -
nasal, uterine, internal bleeding
Слайд 44
CVS - dull heart sounds, hypotonia, tachycardia
- RT
- dyspnea, cyanosis, superficial breathing, dry rales
GIT - coated tongue, constipations, increased liver and
spleen sizes
- UGT- decreased diuresis, proteinuria, leucocyturia,
erythrocyturia, casts
WBC – hyperleukocytosis, increased ESR (40-65 mm/h)
- Electrolites - hypokalemia, hyponatriumia, hypochloremia
Слайд 45
Differential diagnosis will be carried out with
haematosepsis,
severe influenza,
hemorrhagic vasculitis,
Werlhof's disease (idiopathic thrombocytopenia purpura).
CHRONIC MENINGOCOCCAL SEPSIS
is
more often characterized by:
- loss of appetite
- loss of body mass
- increased body temperature
- arthralgia or purulent arthritis
- spotted or papular rush on the skin
- meningococcal subacute ENDOCARDITIS!!!
Слайд 46
MENINGITIS
- the sudden beginning (in first hour of disease)
- high fever
- intensive headache in the occipital area
- vomiting, which does not bring relief
- hyperesthesia, hyperacusia, photophobia
- appearance and increase of an aggressiveness
- Meningeal sms - rigidity of neck muscles, “+” Kernig’s,
Brudzinski’s symptoms)
- damage of cranial nervous:
- 3-4 pair (diplopia, ptosis, anisocoria)
- 7-8 pair (12,7 %)
- In CSF – neutrophils are more then 1000 in 1 mcl (83 %),
increased protein and dicreased level of a glucose.
Слайд 58
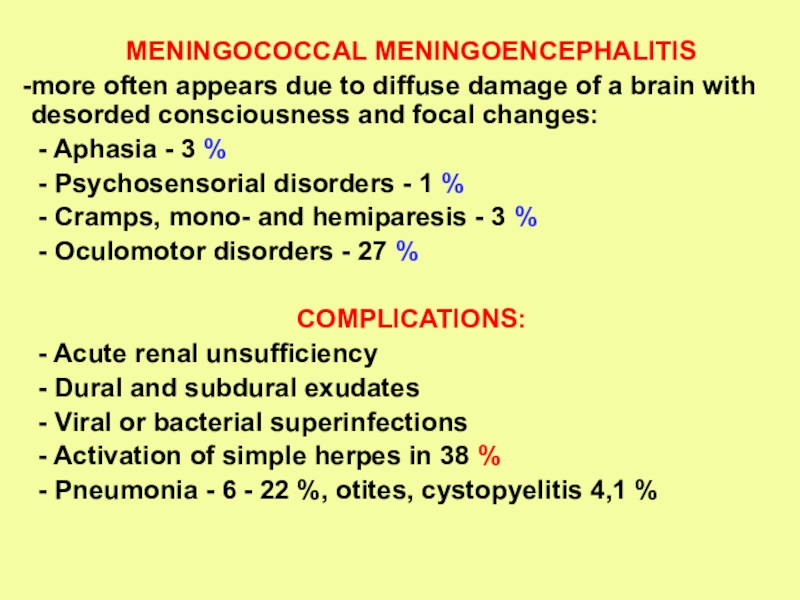
MENINGOCOCCAL MENINGOENCEPHALITIS
more often appears due to diffuse damage of
a brain with desorded consciousness and focal changes:
- Aphasia
- 3 %
- Psychosensorial disorders - 1 %
- Cramps, mono- and hemiparesis - 3 %
- Oculomotor disorders - 27 %
COMPLICATIONS:
- Acute renal unsufficiency
- Dural and subdural exudates
- Viral or bacterial superinfections
- Activation of simple herpes in 38 %
- Pneumonia - 6 - 22 %, otites, cystopyelitis 4,1 %
Слайд 61
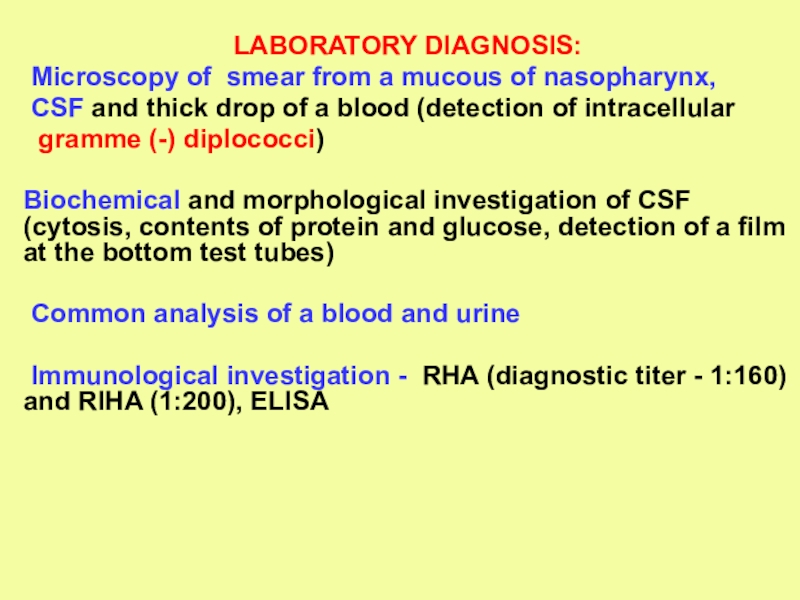
LABORATORY DIAGNOSIS:
Microscopy of smear from a mucous of nasopharynx,
CSF and thick drop of a blood (detection of intracellular
gramme (-) diplococci)
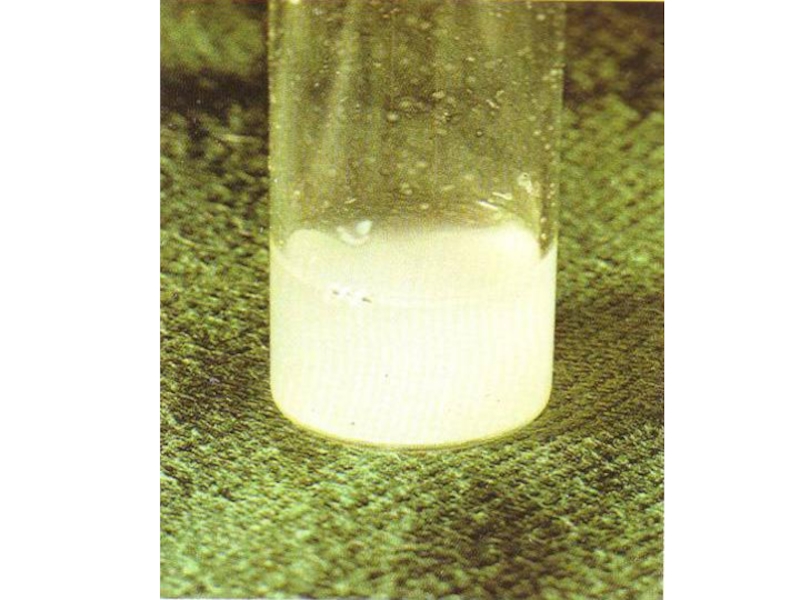
Biochemical and morphological investigation of CSF (cytosis, contents of protein and glucose, detection of a film at the bottom test tubes)
Common analysis of a blood and urine
Immunological investigation - RHA (diagnostic titer - 1:160) and RIHA (1:200), ELISA
Слайд 64
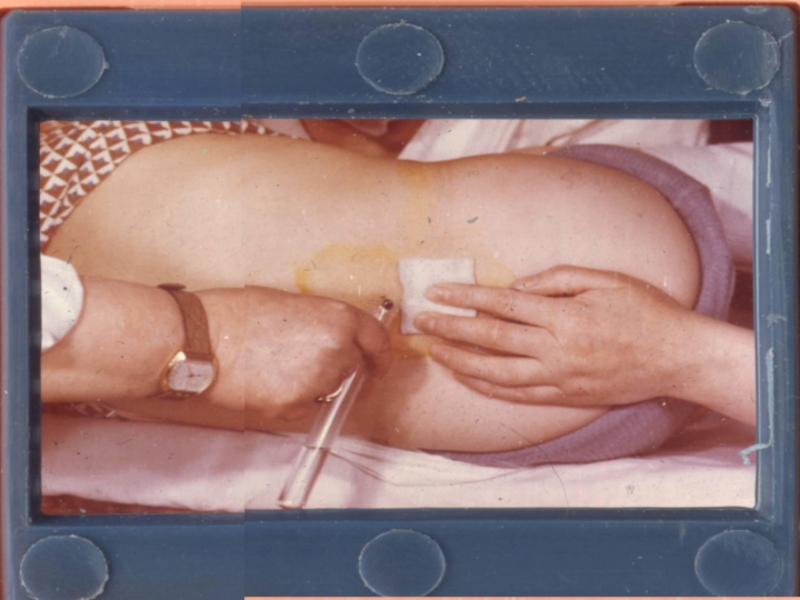
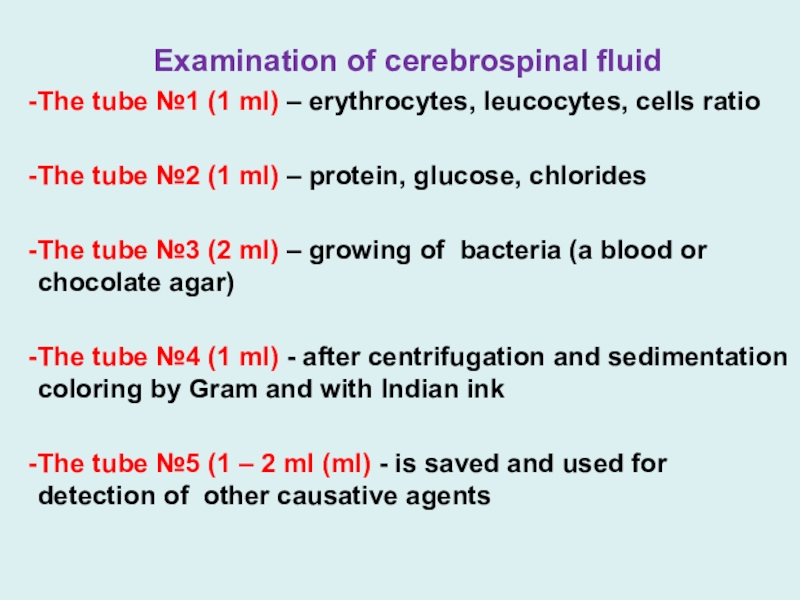
Examination of cerebrospinal fluid
The tube №1 (1 ml) – erythrocytes,
leucocytes, cells ratio
The tube №2 (1 ml) – protein, glucose,
chlorides
The tube №3 (2 ml) – growing of bacteria (a blood or chocolate agar)
The tube №4 (1 ml) - after centrifugation and sedimentation coloring by Gram and with Indian ink
The tube №5 (1 – 2 ml (ml) - is saved and used for detection of other causative agents
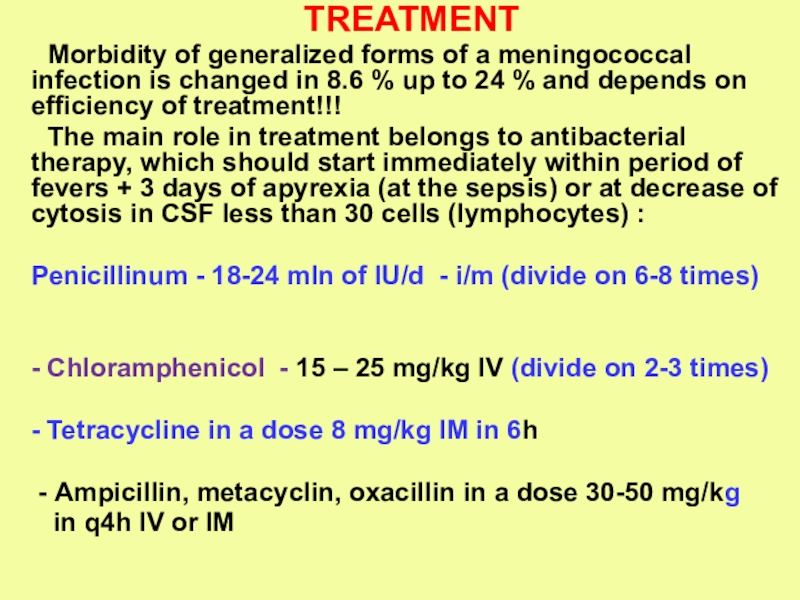
Слайд 65TREATMENT
Morbidity of generalized forms of a meningococcal infection is changed
in 8.6 % up to 24 % and depends on
efficiency of treatment!!!
The main role in treatment belongs to antibacterial therapy, which should start immediately within period of fevers + 3 days of apyrexia (at the sepsis) or at decrease of cytosis in СSF less than 30 cells (lymphocytes) :
Penicillinum - 18-24 mln of IU/d - i/m (divide on 6-8 times)
- Chloramphenicol - 15 – 25 mg/kg IV (divide on 2-3 times)
- Tetracycline in a dose 8 mg/kg IМ in 6h
- Аmpicillin, metacyclin, oxacillin in a dose 30-50 mg/kg
in q4h IV or IM
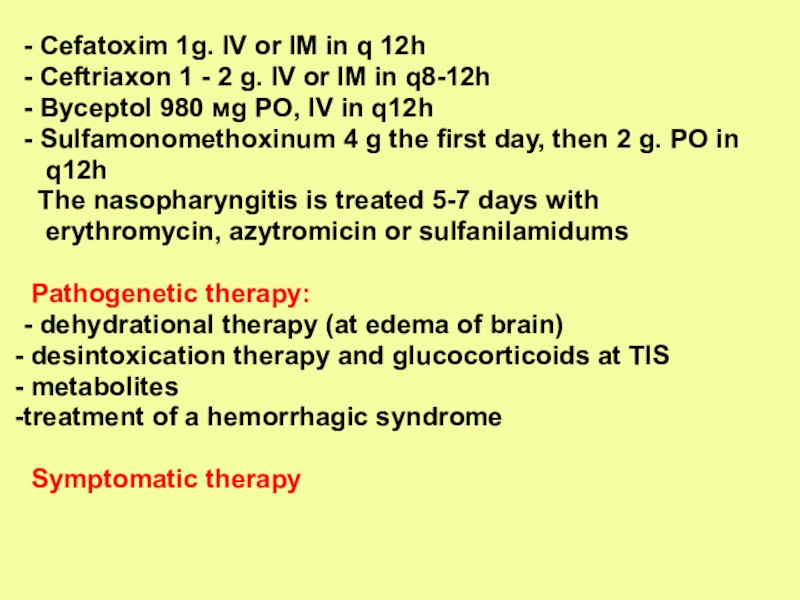
Слайд 66
- Cefatoxim 1g. IV or IM in q 12h
- Ceftriaxon 1 - 2 g. IV or IМ in
q8-12h
- Byceptol 980 мg PO, IV in q12h
- Sulfamonomethoxinum 4 g the first day, then 2 g. PO in
q12h
The nasopharyngitis is treated 5-7 days with
erythromycin, аzytromicin or sulfanilamidums
Pathogenetic therapy:
- dehydrational therapy (at edema of brain)
desintoxication therapy and glucocorticoids at ТIS
metabolites
treatment of a hemorrhagic syndrome
Symptomatic therapy
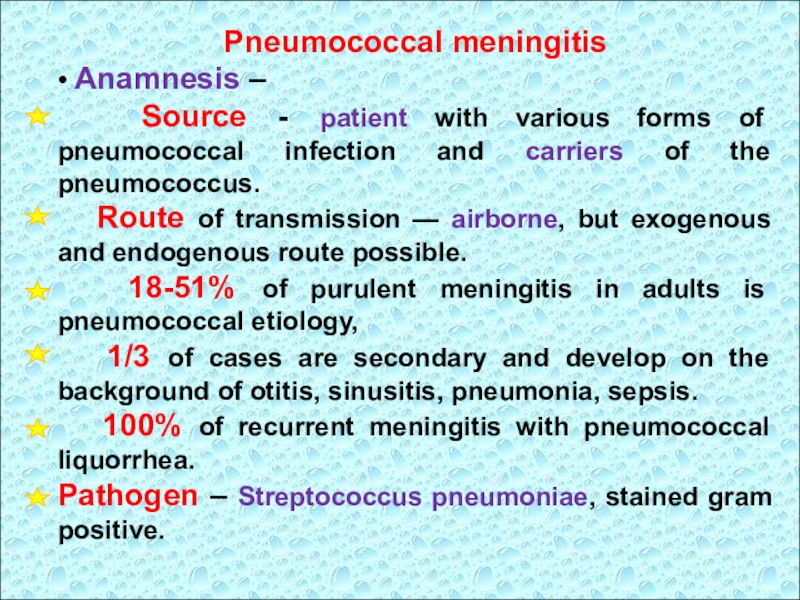
Слайд 67Pneumococcal meningitis
• Anamnesis –
Source - patient with
various forms of pneumococcal infection and carriers of the pneumococcus.
Route of transmission — airborne, but exogenous and endogenous route possible.
18-51% of purulent meningitis in adults is pneumococcal etiology,
1/3 of cases are secondary and develop on the background of otitis, sinusitis, pneumonia, sepsis.
100% of recurrent meningitis with pneumococcal liquorrhea.
Pathogen – Streptococcus pneumoniae, stained gram positive.
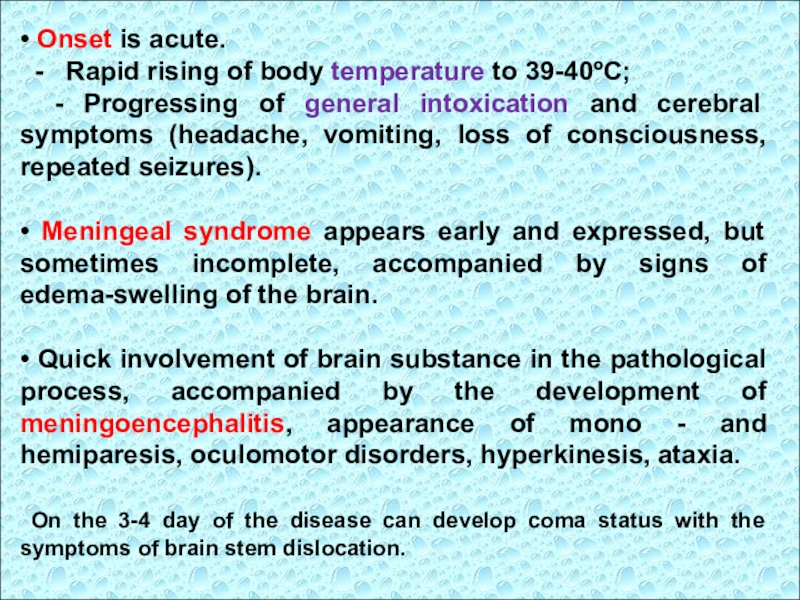
Слайд 68• Onset is acute.
- Rapid rising of
body temperature to 39-40ºC;
- Progressing of general intoxication and
cerebral symptoms (headache, vomiting, loss of consciousness, repeated seizures).
• Meningeal syndrome appears early and expressed, but sometimes incomplete, accompanied by signs of edema-swelling of the brain.
• Quick involvement of brain substance in the pathological process, accompanied by the development of meningoencephalitis, appearance of mono - and hemiparesis, oculomotor disorders, hyperkinesis, ataxia.
On the 3-4 day of the disease can develop coma status with the symptoms of brain stem dislocation.
Слайд 69• Course of the disease varies from malignant forms with
lethal outcome to a proloned and recurrent.
• With the development
of pneumococcal sepsis may be affection of other organs: hemorrhagic rash on the skin (like meningococcemia), pneumonia, endo - and pericarditis, arthritis.
• In 50% of patients residual effects remain, may be seen epilepsy, paresis, paralysis.
Слайд 70• Cerebrospinal fluid is turbid, of yellow-grey color with metallic
shade.
Cell count up to 30000 in 1
mkl, protein - 2-5 g/l.
Pressure of CSF is increased moderately due to accumulation of pus in the subarachnoid space and block of CSF pathways.
• CBC - expressed inflammatory changes.
• Bacteriological examination of blood, CSF
detects the Streptococcus pneumoniae.
Слайд 71SEROUS MENINGITIS
- is a group of CNS diseases
with the similar clinical manifestations and morphology, characterized by the
serous inflammation of the meninges, mostly of viral, rarely bacterial, fungal or parasitic etiology,
accompanied by acute development of hydrocephalic syndrome and nonexpressed meningeal syndrome.
Depending on the mechanism of CNS demerge serous meningitis are divided into primary and secondary.
Слайд 72 The etiology of primary serous meningitis is most often of
viral origin, the clinic is characterized only by meningeal syndrome
(Acute
lymphocytic choriomeningitis, mosquito and tick-borne encephalitis, the meningeal form of poliomyelitis).
Secondary serous meningitis develop on the background of main disease, usually of viral etiology (enterovirus infection, respiratory viral infections, chickenpox, measles, rubella, epidemic. mumps, HIV infection, herpesvirus infection, cytomegalovirus, rabies, arbovirus infection).
Less serous meningitis occurs by bacterial infections (typhoid, tuberculosis, brucellosis, leptospirosis, syphilis, Lyme disease, yersiniosis), parasitic (malaria, toxoplasmosis, amebiasis) or fungal infections (cryptococcosis, coccidioidomycosis, aspergillosis).
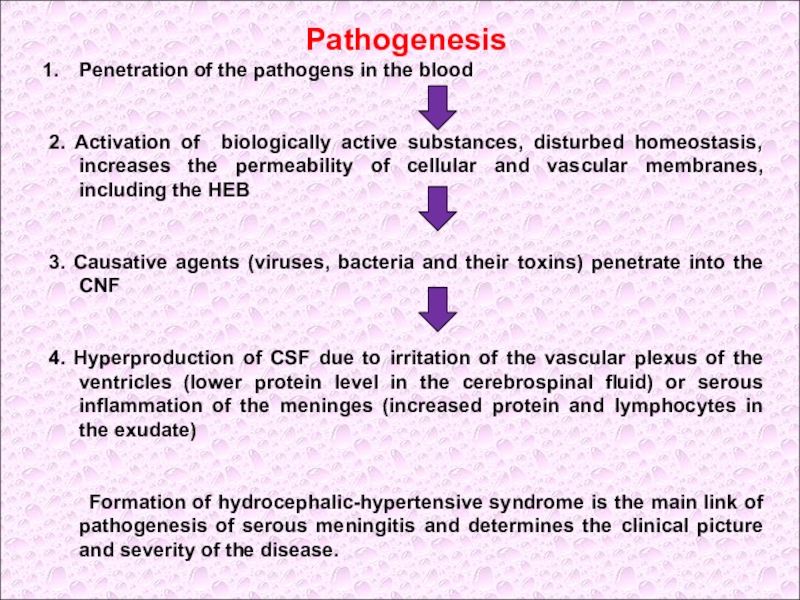
Слайд 73Pathogenesis
Penetration of the pathogens in the blood
2. Activation of
biologically active substances, disturbed homeostasis, increases the permeability of cellular
and vascular membranes, including the HEB
3. Causative agents (viruses, bacteria and their toxins) penetrate into the CNF
4. Hyperproduction of CSF due to irritation of the vascular plexus of the ventricles (lower protein level in the cerebrospinal fluid) or serous inflammation of the meninges (increased protein and lymphocytes in the exudate)
Formation of hydrocephalic-hypertensive syndrome is the main link of pathogenesis of serous meningitis and determines the clinical picture and severity of the disease.
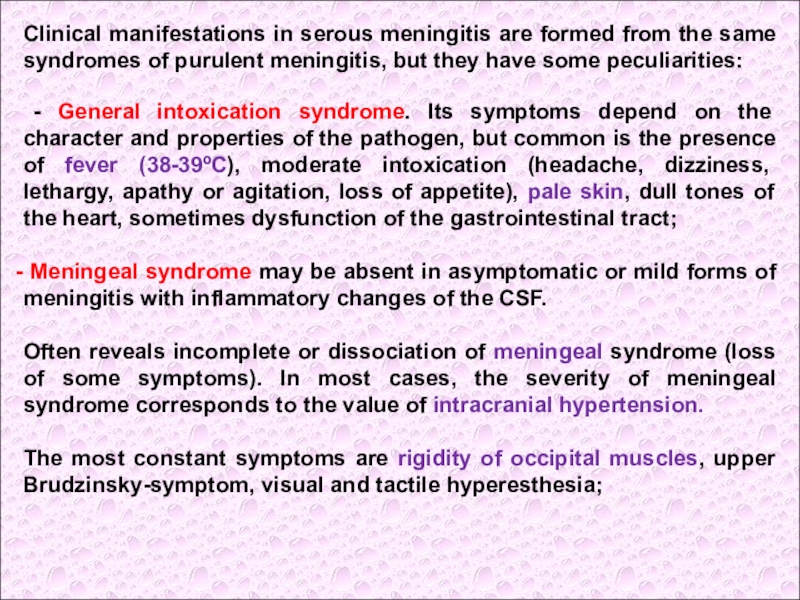
Слайд 74Clinical manifestations in serous meningitis are formed from the same
syndromes of purulent meningitis, but they have some peculiarities:
-
General intoxication syndrome. Its symptoms depend on the character and properties of the pathogen, but common is the presence of fever (38-39ºC), moderate intoxication (headache, dizziness, lethargy, apathy or agitation, loss of appetite), pale skin, dull tones of the heart, sometimes dysfunction of the gastrointestinal tract;
Meningeal syndrome may be absent in asymptomatic or mild forms of meningitis with inflammatory changes of the CSF.
Often reveals incomplete or dissociation of meningeal syndrome (loss of some symptoms). In most cases, the severity of meningeal syndrome corresponds to the value of intracranial hypertension.
The most constant symptoms are rigidity of occipital muscles, upper Brudzinsky-symptom, visual and tactile hyperesthesia;
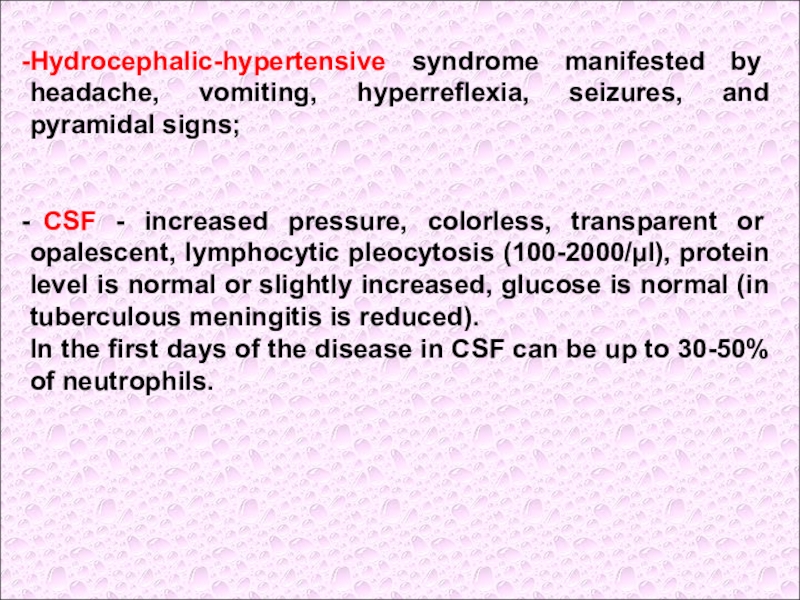
Слайд 75
Hydrocephalic-hypertensive syndrome manifested by headache, vomiting, hyperreflexia, seizures, and pyramidal
signs;
CSF - increased pressure, colorless, transparent or opalescent, lymphocytic
pleocytosis (100-2000/µl), protein level is normal or slightly increased, glucose is normal (in tuberculous meningitis is reduced).
In the first days of the disease in CSF can be up to 30-50% of neutrophils.
Слайд 76Enteroviral meningitis
Is caused by ECHO and Coxacky virus
of different
serotypes;
Infection is highly contagious;
Spring-summer seasonality, often outbreaks;
70-80% of population - children of 5-9 years;
Source of infection is a sick man and a virus carrier;
Mechanism of transmission is aerogenic (airborne),
but posible fecal-oral transmission of the pathogen.
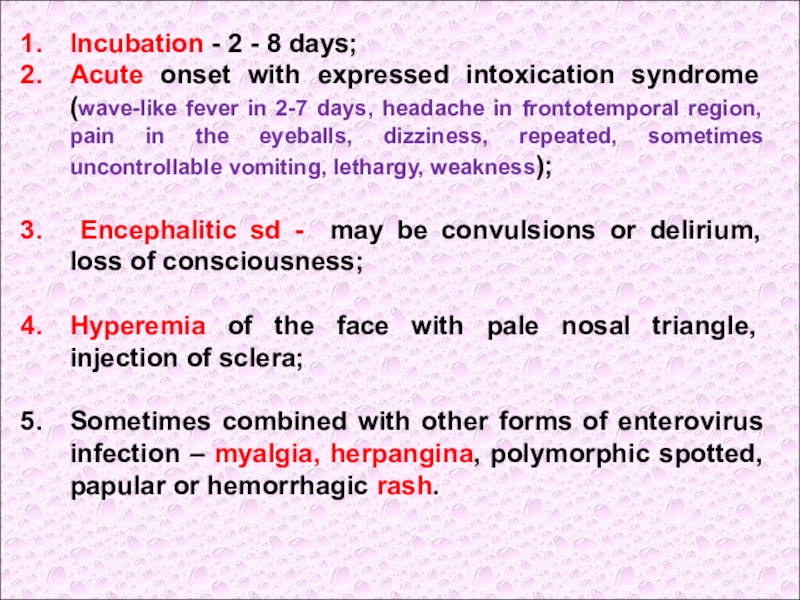
Слайд 77Incubation - 2 - 8 days;
Acute onset with expressed intoxication
syndrome (wave-like fever in 2-7 days, headache in frontotemporal region,
pain in the eyeballs, dizziness, repeated, sometimes uncontrollable vomiting, lethargy, weakness);
Encephalitic sd - may be convulsions or delirium, loss of consciousness;
Hyperemia of the face with pale nosal triangle, injection of sclera;
Sometimes combined with other forms of enterovirus infection – myalgia, herpangina, polymorphic spotted, papular or hemorrhagic rash.
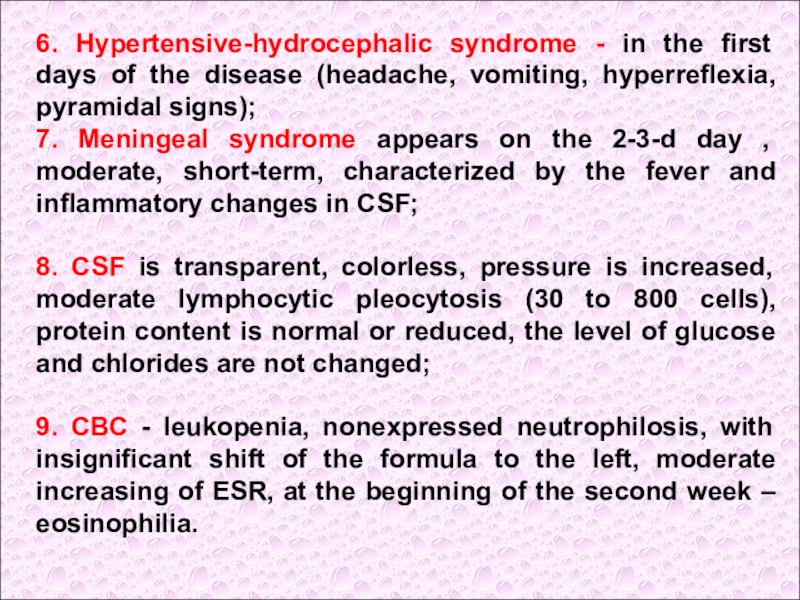
Слайд 786. Hypertensive-hydrocephalic syndrome - in the first days of the
disease (headache, vomiting, hyperreflexia, pyramidal signs);
7. Meningeal syndrome appears on
the 2-3-d day , moderate, short-term, characterized by the fever and inflammatory changes in CSF;
8. CSF is transparent, colorless, pressure is increased, moderate lymphocytic pleocytosis (30 to 800 cells), protein content is normal or reduced, the level of glucose and chlorides are not changed;
9. CBC - leukopenia, nonexpressed neutrophilosis, with insignificant shift of the formula to the left, moderate increasing of ESR, at the beginning of the second week – eosinophilia.
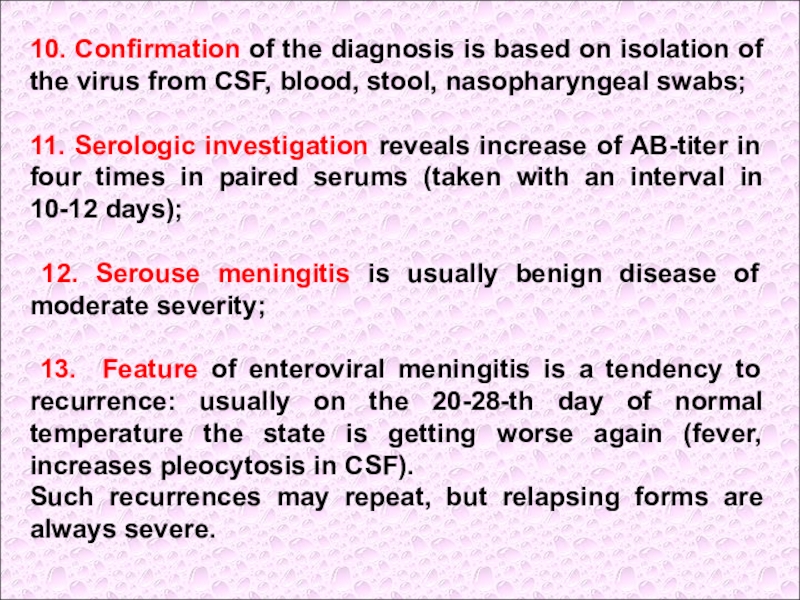
Слайд 7910. Confirmation of the diagnosis is based on isolation of
the virus from CSF, blood, stool, nasopharyngeal swabs;
11. Serologic investigation
reveals increase of AB-titer in four times in paired serums (taken with an interval in 10-12 days);
12. Serouse meningitis is usually benign disease of moderate severity;
13. Feature of enteroviral meningitis is a tendency to recurrence: usually on the 20-28-th day of normal temperature the state is getting worse again (fever, increases pleocytosis in CSF).
Such recurrences may repeat, but relapsing forms are always severe.