Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
PATHOPHYSIOLOGY OF CARBOHYDRATE METABOLISM
Содержание
- 1. PATHOPHYSIOLOGY OF CARBOHYDRATE METABOLISM
- 2. A. Physiologic remarks:
- 3. Слайд 3
- 4. Слайд 4
- 5. B. Disturbancies in Carbohydrate Resorbtion
- 6. Pathomechanisms Activity of
- 7. Lactase deficiency syndrome
- 8. Causes of secondary lactase deficiency:
- 9. Monosaccharides malabsorbtion Small
- 10. Glycogenosis
- 11. Слайд 11
- 12. DIABETES MELLITUSDIABETES MELLITUSDM – complex chronic metabolic
- 13. Regulation of the blood glucose level depends
- 14. DM is a chronic complex syndrome induced
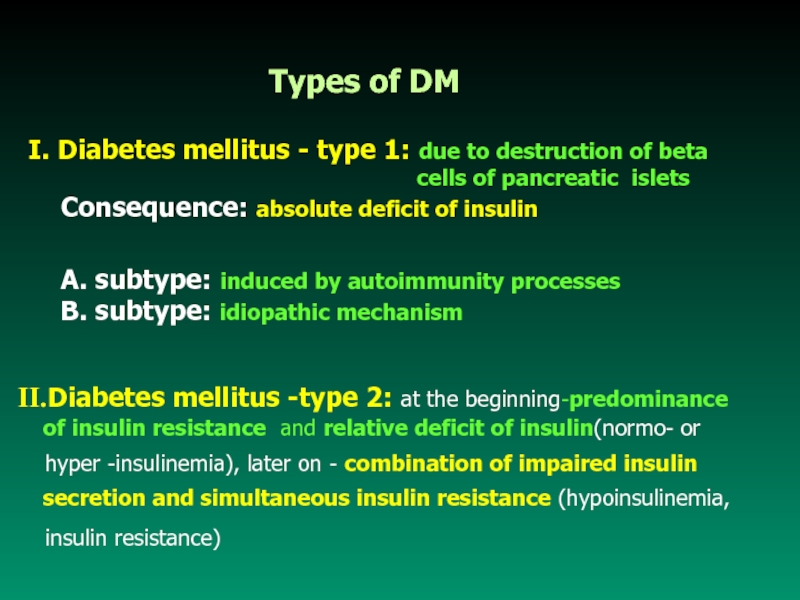
- 15. I. Diabetes mellitus - type 1:
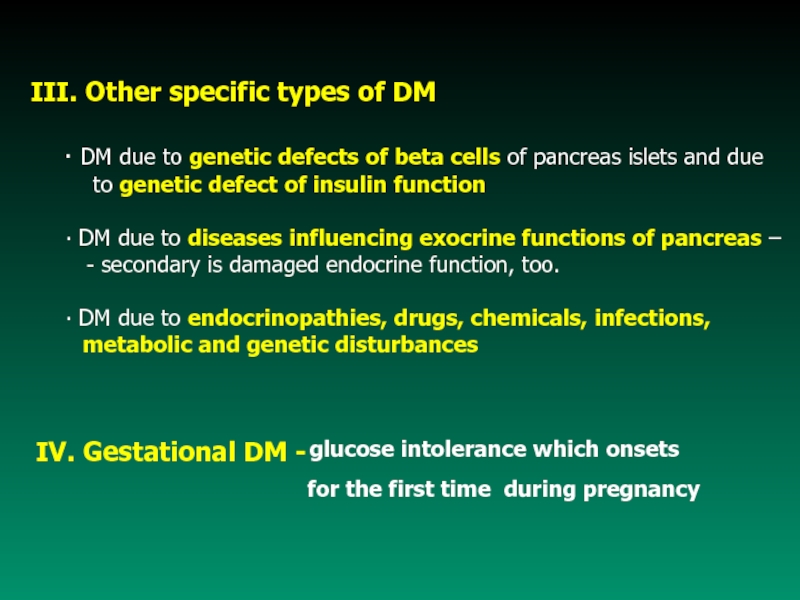
- 16. IV. Gestational DM - III. Other specific
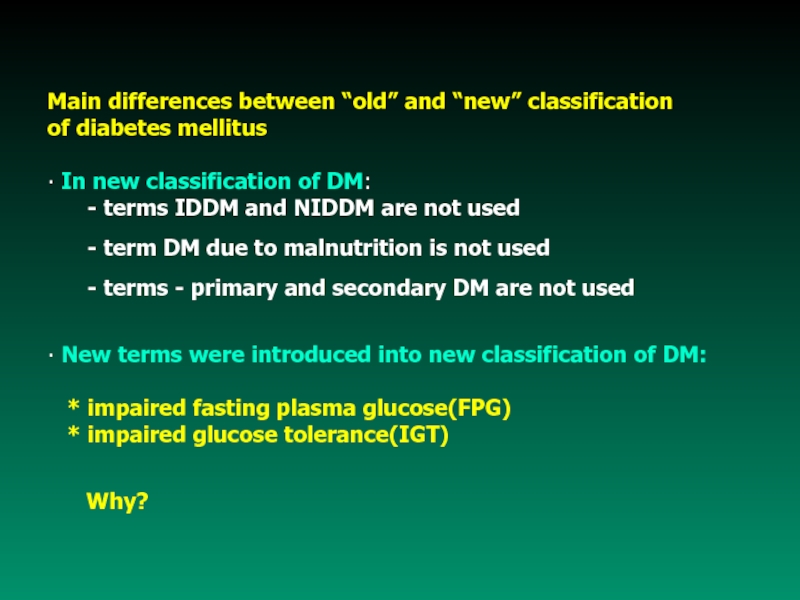
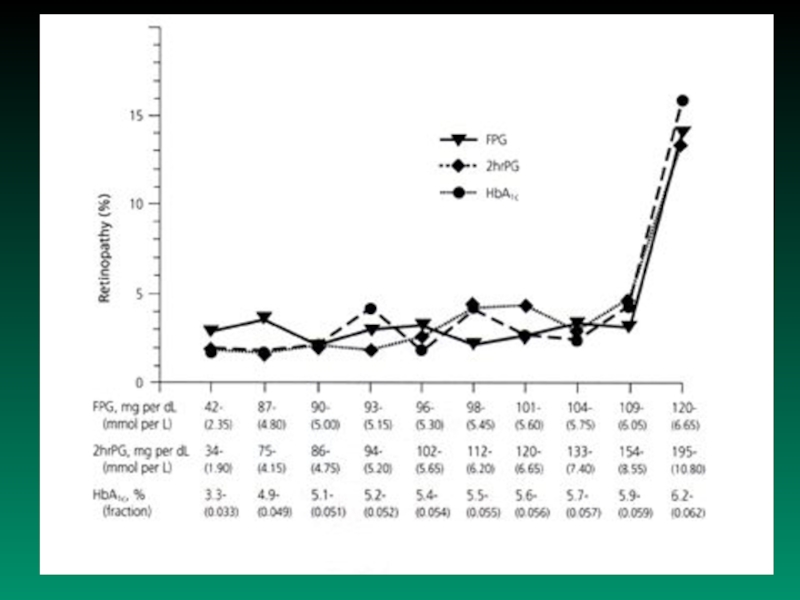
- 17. Main differences between “old” and “new” classificationof
- 18. Слайд 18
- 19. Normal fasting value of
- 20. Impaired fasting plasma glucose: 6.1 but
- 21. Syndrome X (metabolic X syndrome) - frequently
- 22. Слайд 22
- 23. 3. defective signal transduction
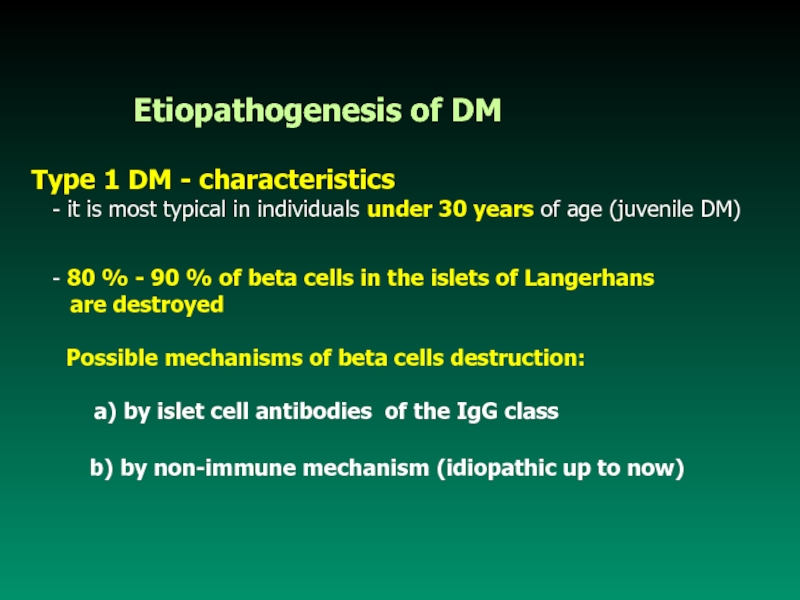
- 24. Etiopathogenesis of DMType 1
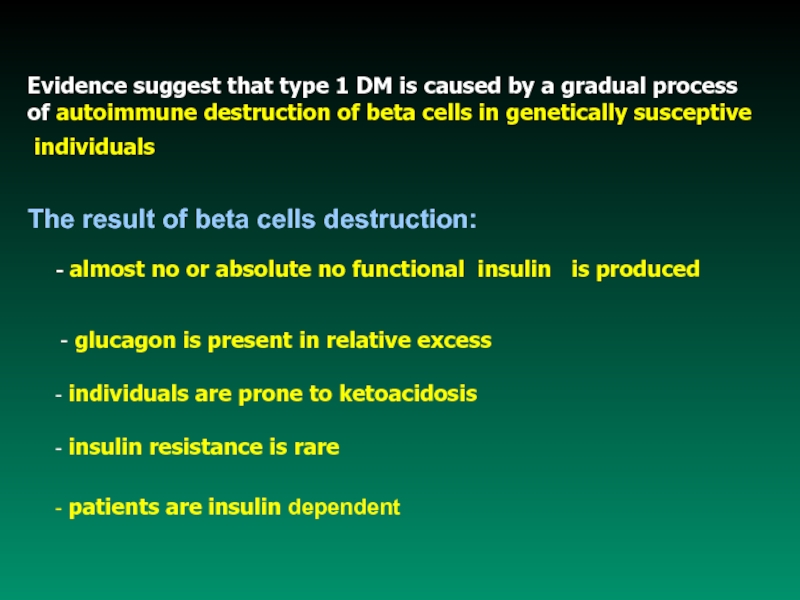
- 25. Evidence suggest that type 1 DM is
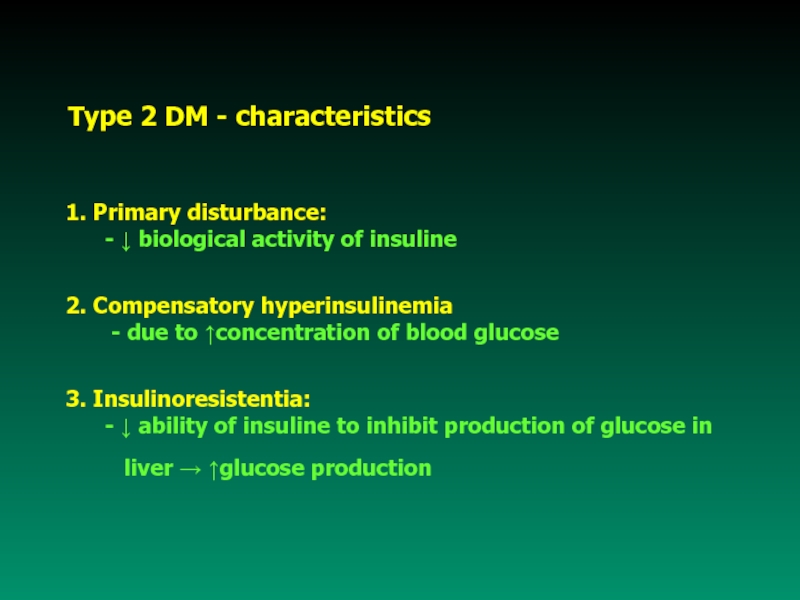
- 26. Type 2 DM - characteristics1. Primary disturbance:
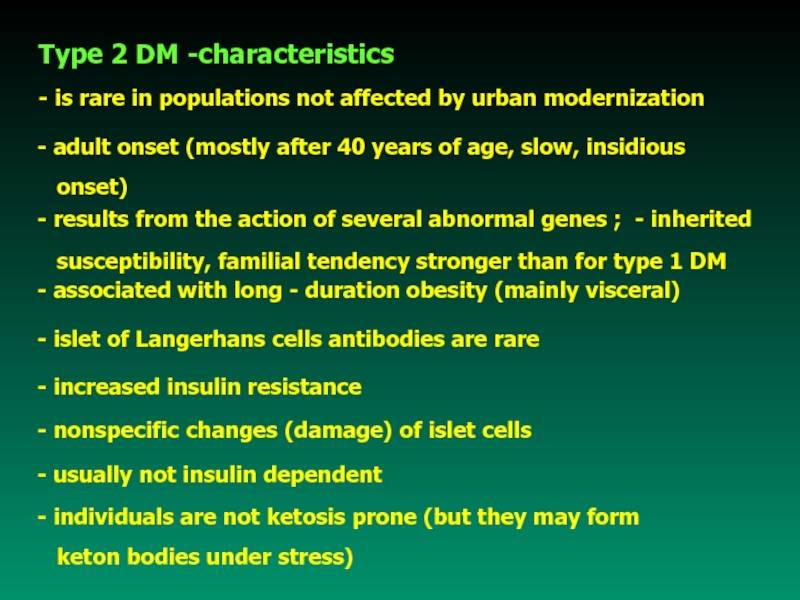
- 27. Type 2 DM -characteristics - is
- 28. Слайд 28
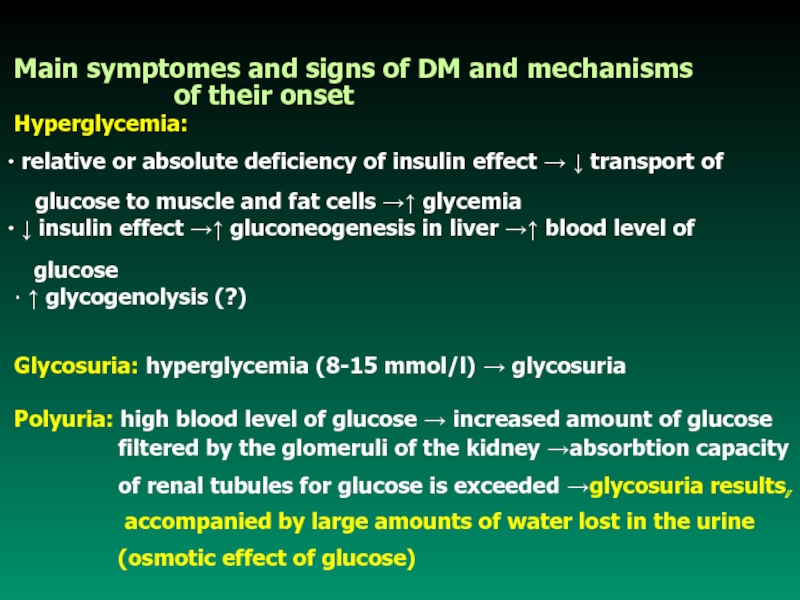
- 29. Main symptomes and signs of DM and
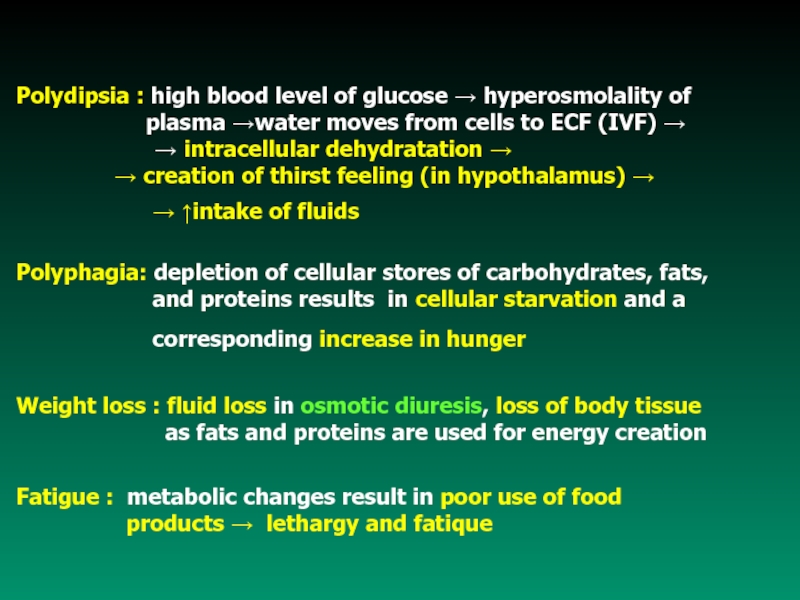
- 30. Polydipsia : high blood level of glucose
- 31. Complications of Diabetes MellitusAcute complications
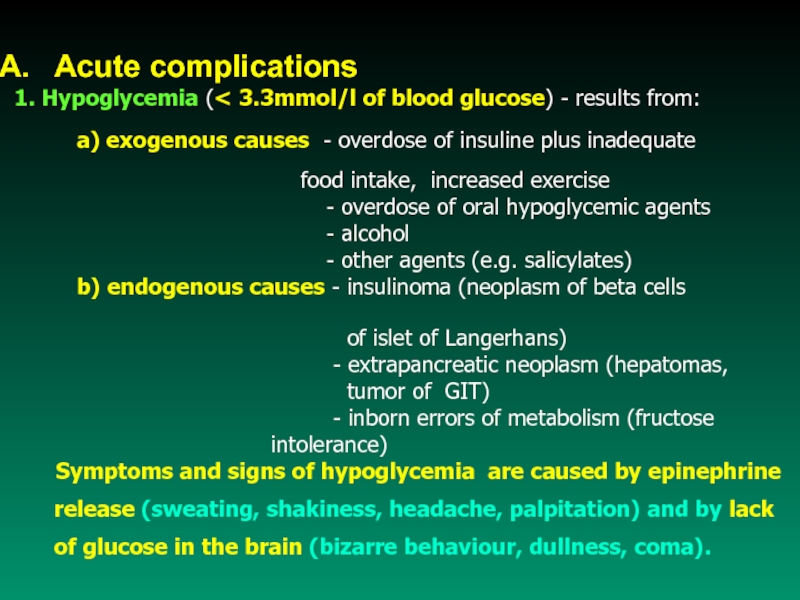
- 32. Acute complications1. Hypoglycemia ( 3.3mmol/l of blood
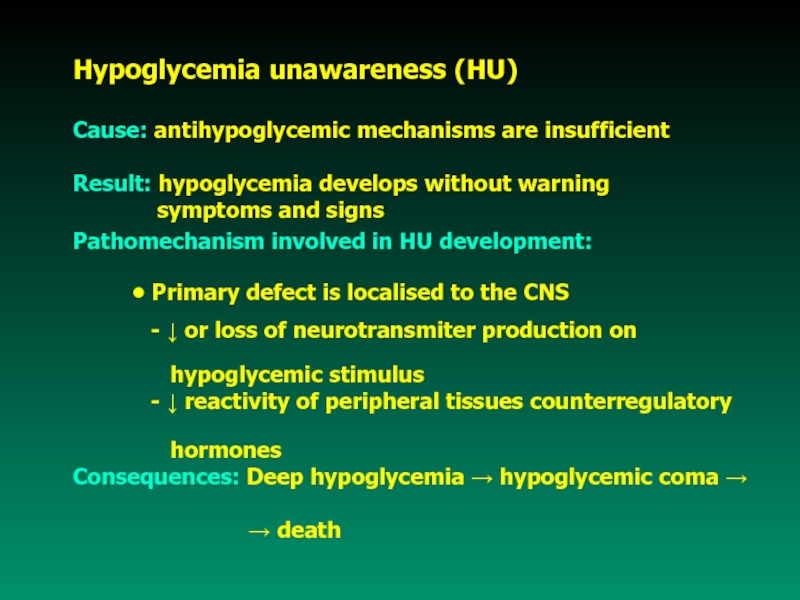
- 33. Hypoglycemia unawareness (HU)Cause: antihypoglycemic mechanisms are insufficientResult:
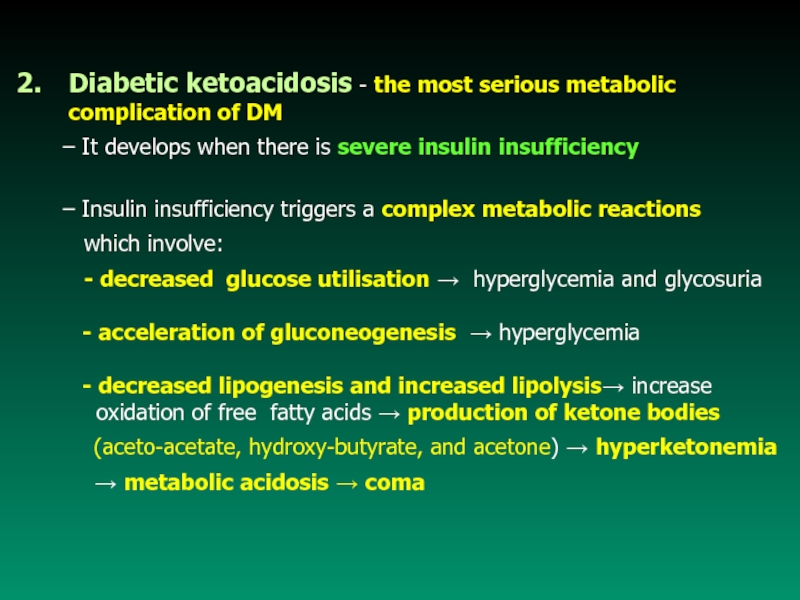
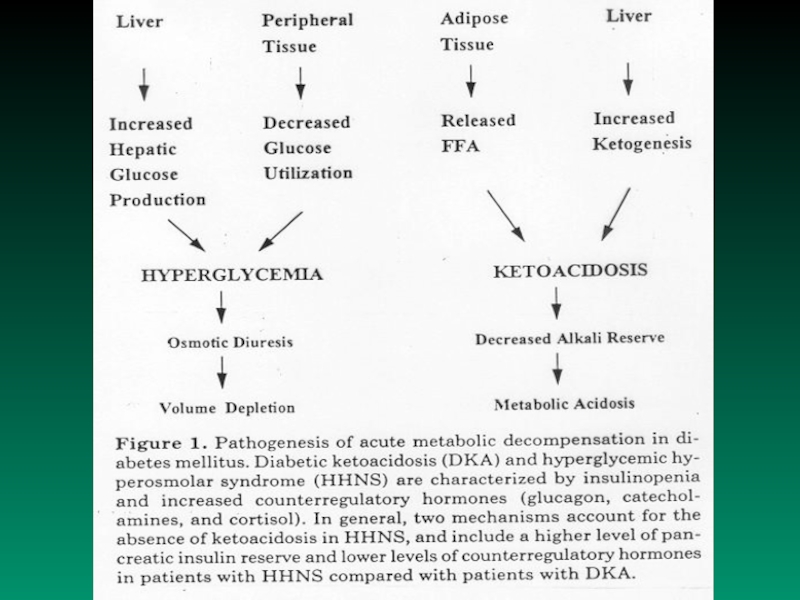
- 34. Diabetic ketoacidosis - the most serious metabolic
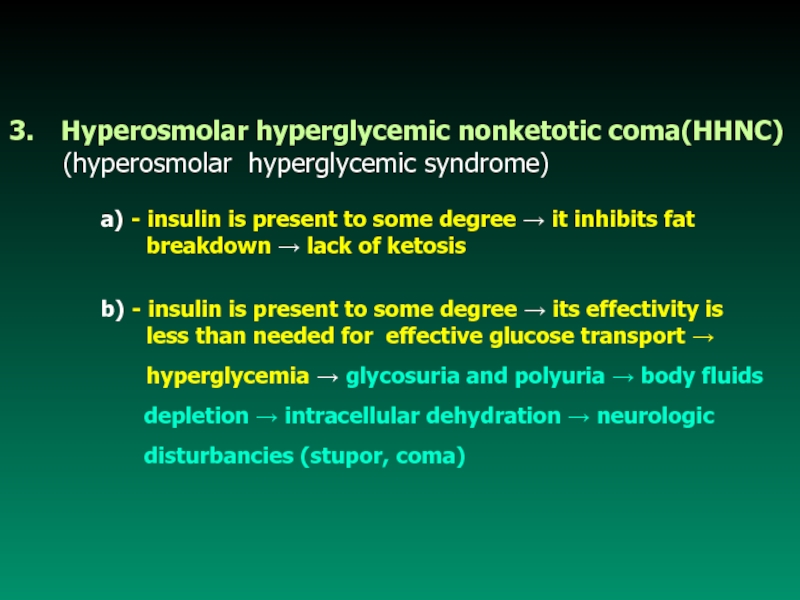
- 35. Hyperosmolar hyperglycemic nonketotic coma(HHNC) (hyperosmolar
- 36. Слайд 36
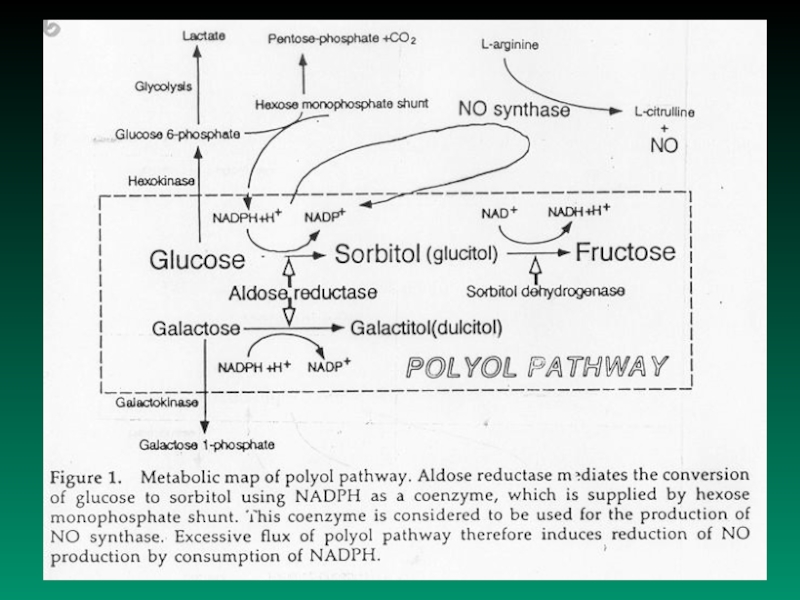
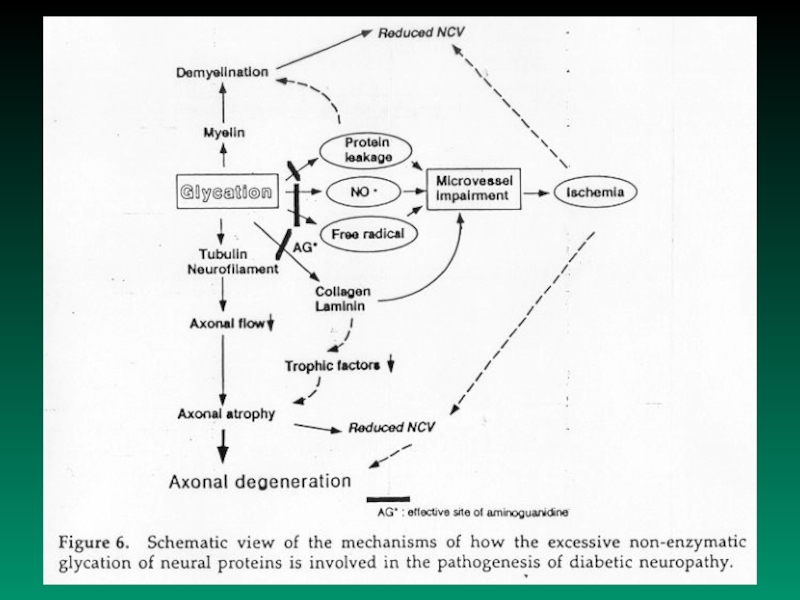
- 37. B. Chronic complications Today,
- 38. Слайд 38
- 39. Слайд 39
- 40. Слайд 40
- 41. Functional consequences:
- 42. Main functions of vascular endotelium• regulates vascular
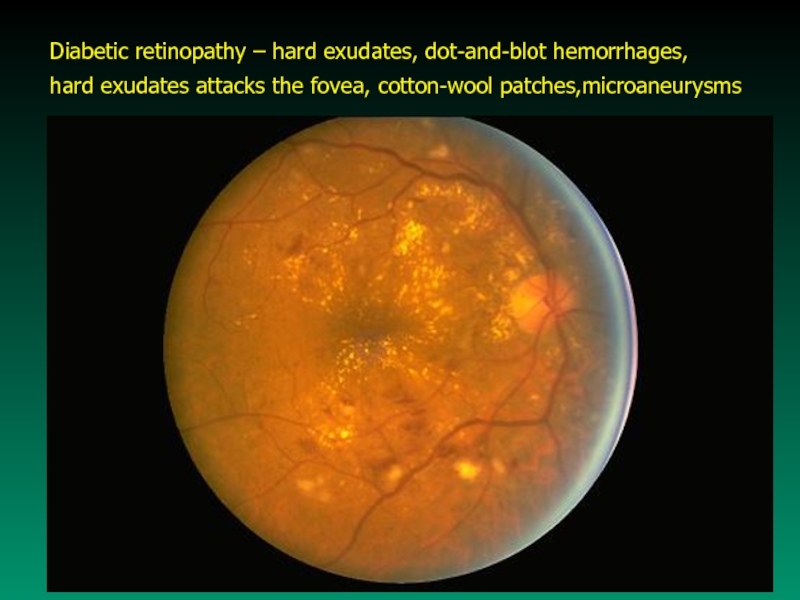
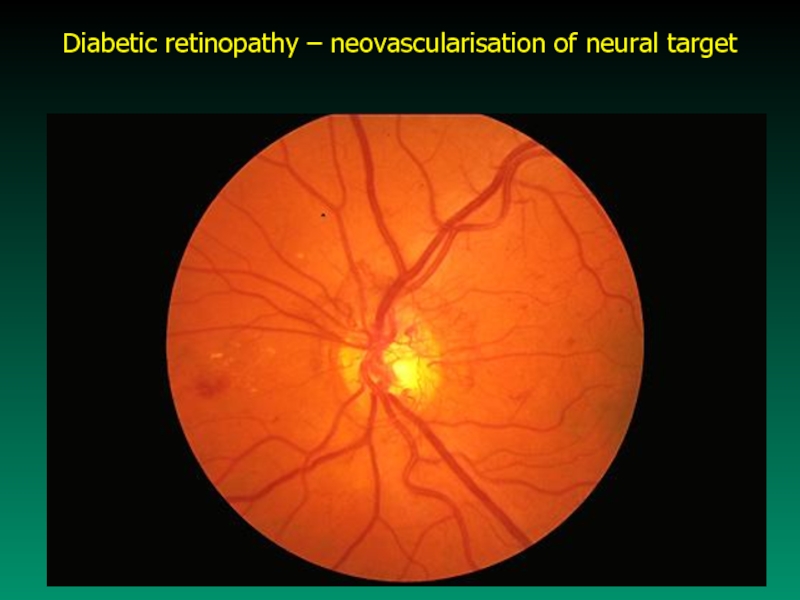
- 43. Microvascular disease - specific lesion of DM
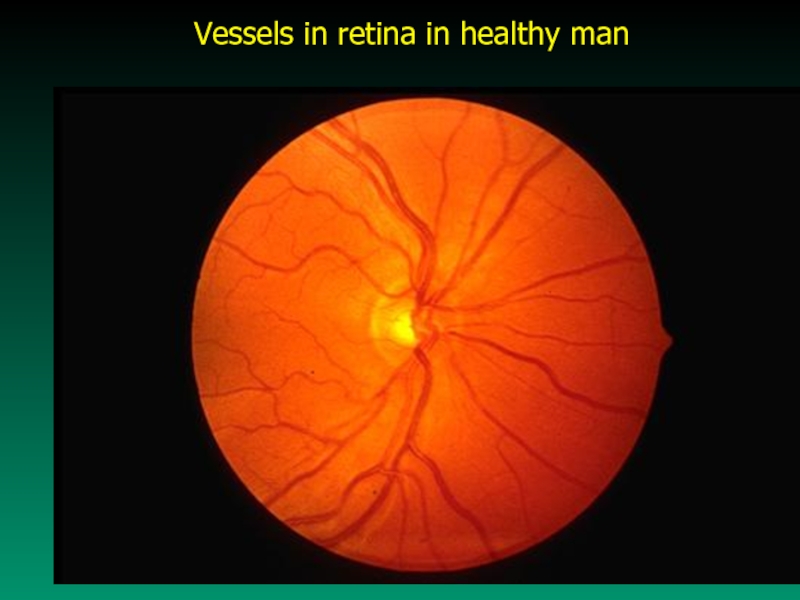
- 44. Vessels in retina in healthy man
- 45. Diabetic retinopathy – hard exudates, dot-and-blot hemorrhages,hard exudates attacks the fovea, cotton-wool patches,microaneurysms
- 46. Diabetic retinopathy – neovascularisation of neural target
- 47. b) Nephropathy - it is the result
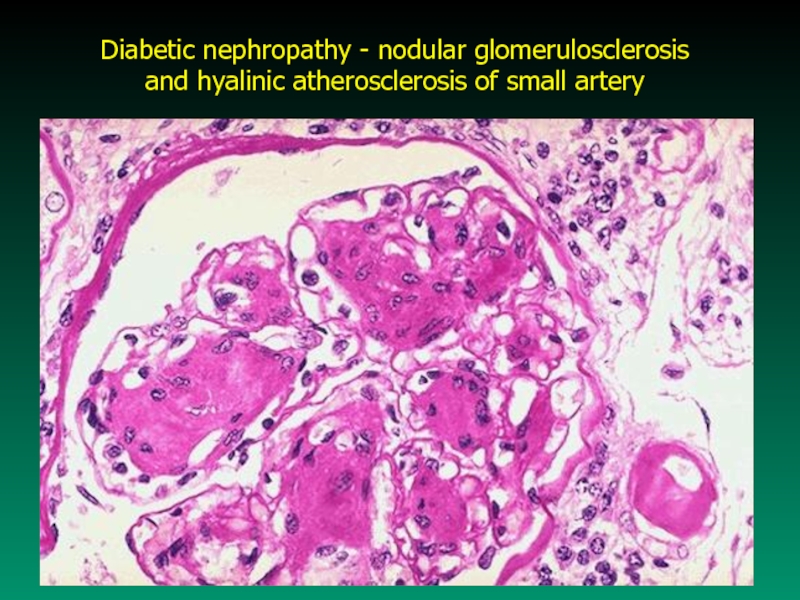
- 48. Diabetic nephropathy - nodular glomerulosclerosis and hyalinic atherosclerosis of small artery
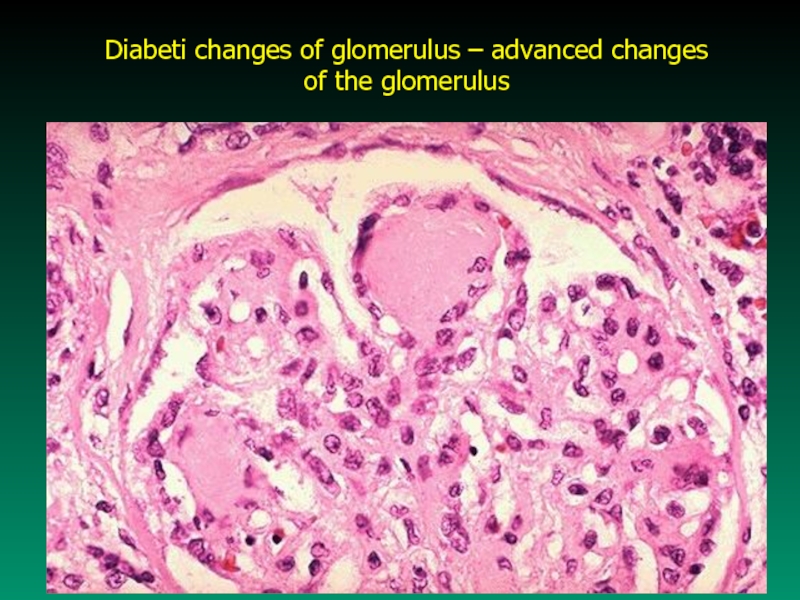
- 49. Diabeti changes of glomerulus – advanced changes of the glomerulus
- 50. B) Macrovascular disease - atherosclerotic lesion
- 51. Слайд 51
- 52. Слайд 52
- 53. 3. Infection Persons with DM are
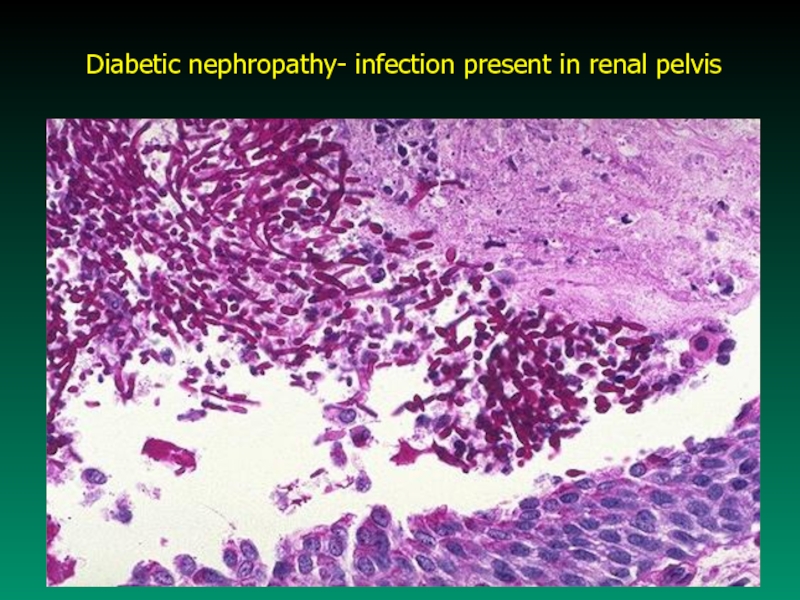
- 54. Diabetic nephropathy- infection present in renal pelvis
- 55. Скачать презентанцию
Слайды и текст этой презентации
Слайд 1PATHOPHYSIOLOGY
OF CARBOHYDRATE METABOLISM
Prof. J. Hanacek, MD, PhD
Technical
co-operative: L.Šurinová
Слайд 2
A. Physiologic remarks:
Carbohydrates are
present in food in various forms:
1. simple
sugars - monosaccharides2. complex chemical units - disaccharides
- polysaccharides
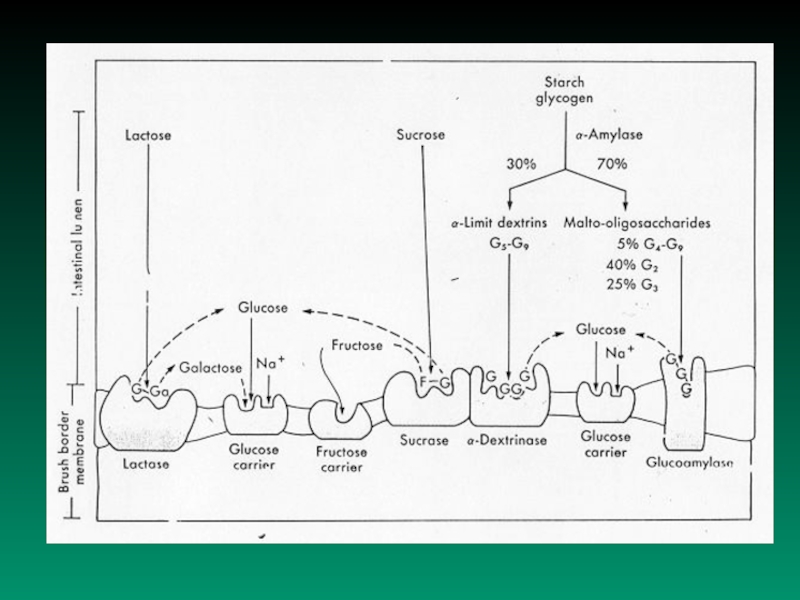
Processing of carbohydrates in GIT
Ingested carbohydrates cleaving proces
monosaccharides absorbtion in stomach,
duodenum and proximal jejunum
Слайд 5B. Disturbancies in Carbohydrate Resorbtion
1.
Disaccharidase deficiency syndrome
saccharase = enzyme
which hydrolyses disaccharide saccharose (to fructose and glucose)
laktase = enzyme which splits disaccharide lactose
(to glucose and galactose)
maltase = enzyme which splits disaccharide maltose
(to two molecule of glucose)
Слайд 6Pathomechanisms
Activity of disaccharidase is decreased
decreased
hydrolysis of disaccharide decreased resorbtion
of substrate increased concentration of disaccharide in small intestine lumen increased osmotic activity of the lumen fluid
diarrhea
b) Activity of disaccharidase is decreased increased
concentration of disaccharide in small intestine lumen
increased concentration of disaccharide in large intestine
disaccharide fermentation by bacteria increased
concentration of lactic acid and fatty acids
stimulation of intestine wall abdominal cramps,
bloating, diarrhea, acidic stools, explosive diarrhea
Слайд 7
Lactase deficiency syndrome
Causes of lactase deficiency:
- genetic defect (primary)
- secondary to a wide variety of gastrointestinal diseases that damage the mucosa of the small intestine (secondary)
Disaccharide lactose is the principal carbohydrate in milk.
- Many persons showing milk intolerance prove to be lactase –
deficient
- Primary lactase deficiency incidence is as high as 80 % to 90 %
among African - Americans, Asians, and Bantus population
- Milk intolerance may not become clinically apparent until
adolescence
Слайд 8Causes of secondary lactase deficiency:
-
nontropical (celiac disease)and tropical sprue,
- regional
enteritis, - viral and bacterial infections of the intestinal tract,
- giardiasis, cystic fibrosis, ulcerative colitis,
- kwashiorkor, coeliac disease
Symptoms and signs - are mentioned at previous page
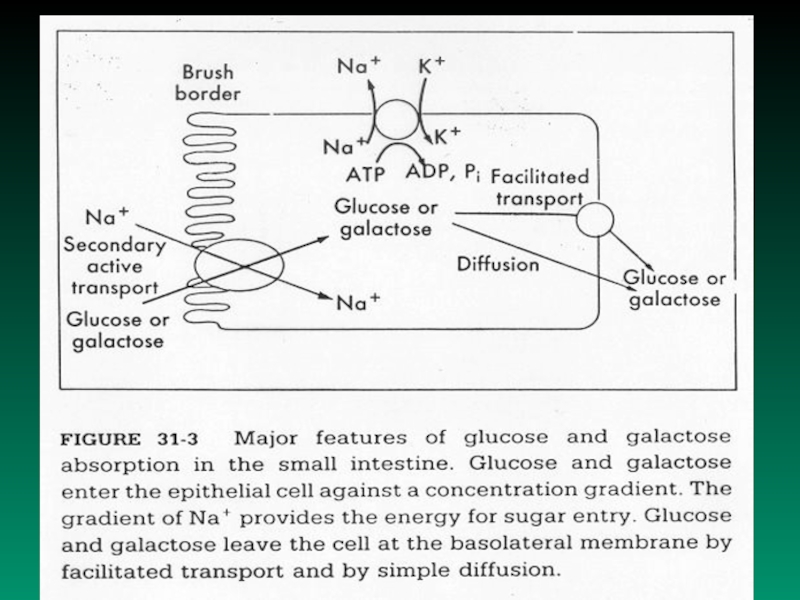
Слайд 9 Monosaccharides malabsorbtion
Small intestine ability to
resorb glucose and galactose is
decreased
Cause: Specific transport system for galactose and glucose
absorbtion in cells of small intestine is insufficient
Results: Symptoms and signs similar to disaccharidase
deficiency syndrome
Слайд 10
Glycogenosis (glycogen storage
disease)
Autosomal recessive disease (inborn errors of
metabolism,emzymopathy)
There are defects in degradation of glycogen.
The disturbances result in storage of abnormal glycogen,
or storage of abnormal amount of glycogen in various
organs of the body
Example: Hepatorenal glycogenosis (Morbus von Gierke)
Cause: Deficit of glucose-6-fosfatase in liver and kidney
Results: Hypoglycemia in fasting individuals,
hyperlipemia, ketonemia
There are 9 other types of glycogenosis
Слайд 12DIABETES MELLITUS
DIABETES MELLITUS
DM – complex chronic metabolic disorder leading
to multiorgan complications
Main pathophysiological questions related
to DMWhy and how the DM develops?
Why and how develop the complications of DM?
What are the mechanisms involved in manifestation
of diabetic symptoms and signs
Слайд 13Regulation of the blood glucose level depends on liver:
1. extracting
glucose from blood
2. synthesizing glycogen
3. performing glycogenolysis
4. performing gluconeogenesisTo a lesser extent peripheral tissues (muscle and adipocytes) use glucose for their energy needs, thus contributing to maintinance of normal blood glucose level
The livers uptake and output of glucose and the use of glucose by peripheral tissues depend on the physiologic balance of several hormones that:
1. lower blood glucose level - insulin
2. rise blood glucose level - glucagon, epinephrine, GH,
glucocorticoids...
Слайд 14DM is a chronic complex syndrome induced by absolute or
relative deficit of insuline which is characterized by metabolic disorders
of carbohydrates, lipids and proteins.The metabolic disturbances are accompanied by loss of carbohydrate tolerance, fasting hyperglycemia, ketoacidosis, decreased lipogenesis, increased lipolysis, increased proteolysis and some other metabolic disorders
Definition of DM
Classification of DM
(according to International Expert Committee, 1997)
Base for the classification are etiopathogenetic mechanisms
involved in onset and development of DM
Слайд 15 I. Diabetes mellitus - type 1: due to destruction
of beta
cells of pancreatic isletsConsequence: absolute deficit of insulin
A. subtype: induced by autoimmunity processes
B. subtype: idiopathic mechanism
Types of DM
II.Diabetes mellitus -type 2: at the beginning-predominance
of insulin resistance and relative deficit of insulin(normo- or
hyper -insulinemia), later on - combination of impaired insulin
secretion and simultaneous insulin resistance (hypoinsulinemia,
insulin resistance)
Слайд 16IV. Gestational DM -
III. Other specific types of DM
DM due to genetic defects of beta
cells of pancreas islets and due to genetic defect of insulin function
DM due to diseases influencing exocrine functions of pancreas –
- secondary is damaged endocrine function, too.
DM due to endocrinopathies, drugs, chemicals, infections,
metabolic and genetic disturbances
glucose intolerance which onsets
for the first time during pregnancy
Слайд 17Main differences between “old” and “new” classification
of diabetes mellitus
In
new classification of DM:
- terms IDDM and NIDDM are not
used- term DM due to malnutrition is not used
- terms - primary and secondary DM are not used
New terms were introduced into new classification of DM:
* impaired fasting plasma glucose(FPG)
* impaired glucose tolerance(IGT)
Why?
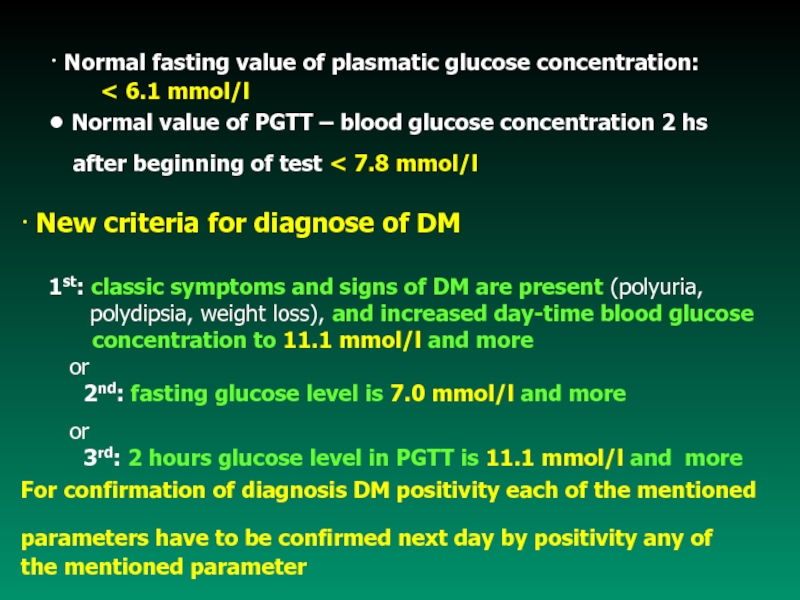
Слайд 19 Normal fasting value of plasmatic glucose concentration:
6.1 mmol/l
● Normal value
of PGTT – blood glucose concentration 2 hs after beginning of test 7.8 mmol/l
New criteria for diagnose of DM
1st: classic symptoms and signs of DM are present (polyuria,
polydipsia, weight loss), and increased day-time blood glucose
concentration to 11.1 mmol/l and more
or
2nd: fasting glucose level is 7.0 mmol/l and more
or
3rd: 2 hours glucose level in PGTT is 11.1 mmol/l and more
For confirmation of diagnosis DM positivity each of the mentioned
parameters have to be confirmed next day by positivity any of
the mentioned parameter
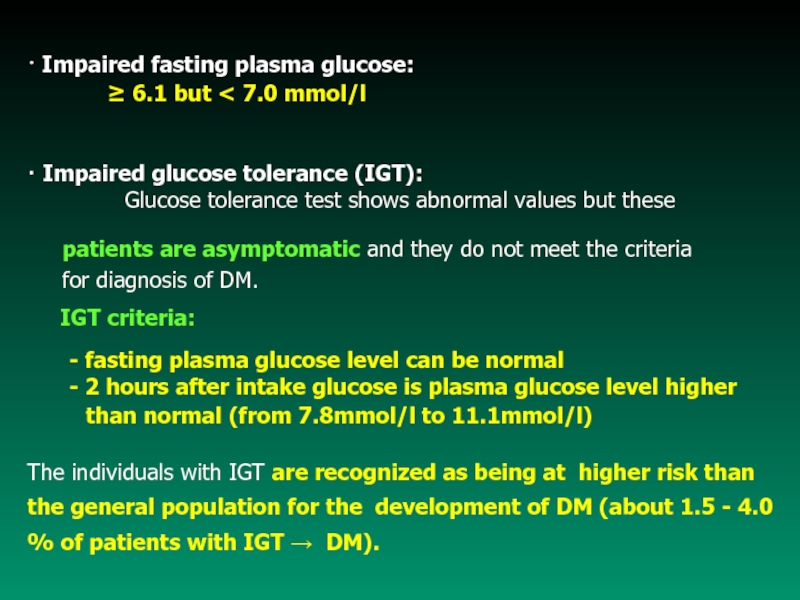
Слайд 20 Impaired fasting plasma glucose:
6.1 but 7.0 mmol/l
Impaired glucose tolerance (IGT):
Glucose tolerance test shows abnormal values but these patients are asymptomatic and they do not meet the criteria
for diagnosis of DM.
IGT criteria:
- fasting plasma glucose level can be normal
- 2 hours after intake glucose is plasma glucose level higher
than normal (from 7.8mmol/l to 11.1mmol/l)
The individuals with IGT are recognized as being at higher risk than the general population for the development of DM (about 1.5 - 4.0 % of patients with IGT DM).
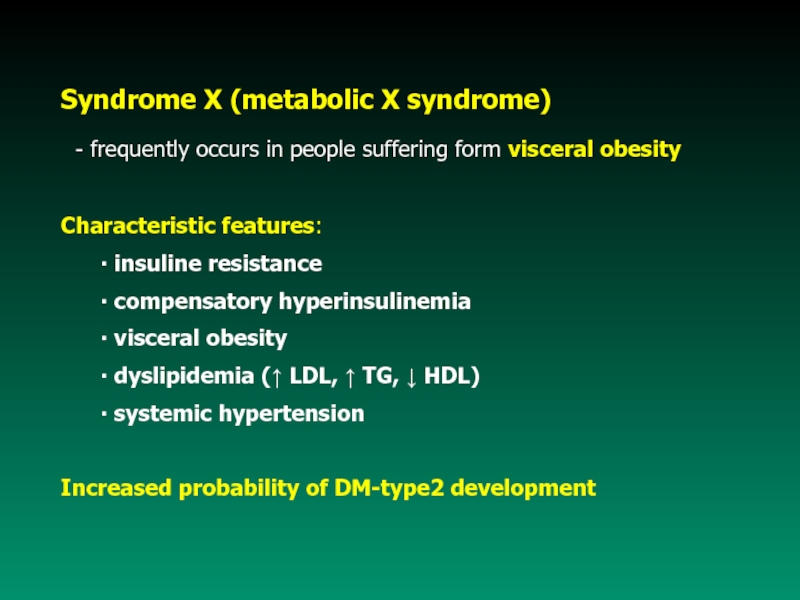
Слайд 21Syndrome X (metabolic X syndrome)
- frequently occurs in people
suffering form visceral obesity
Characteristic features:
insuline resistance
compensatory
hyperinsulinemia visceral obesity
dyslipidemia ( LDL, TG, HDL)
systemic hypertension
Increased probability of DM-type2 development
Слайд 22
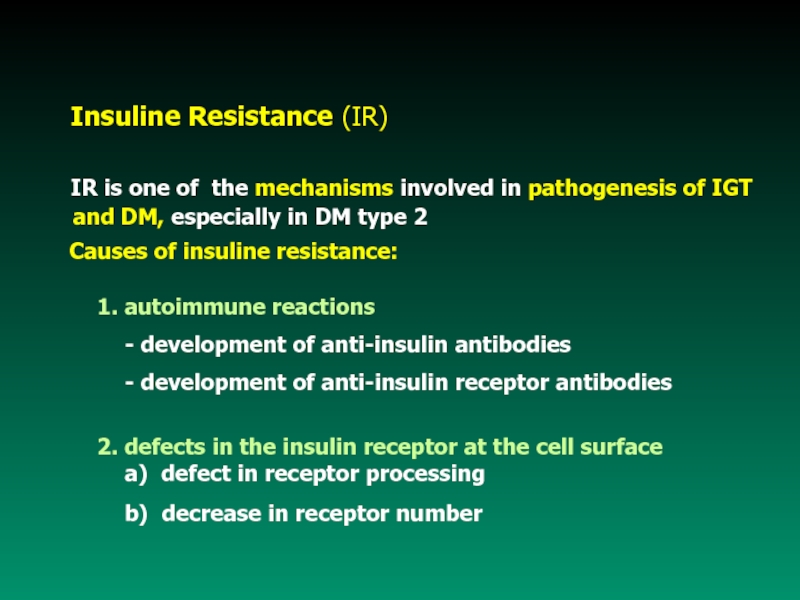
Insuline
Resistance (IR)
IR is one
of the mechanisms involved in pathogenesis of IGT and DM, especially in DM type 2
Causes of insuline resistance:
1. autoimmune reactions
- development of anti-insulin antibodies
- development of anti-insulin receptor antibodies
2. defects in the insulin receptor at the cell surface
a) defect in receptor processing
b) decrease in receptor number
Слайд 233. defective signal transduction
(from the receptor
to the plasma of cell)
4. postreceptor defect
5. increased concentration of
anti-insulinic hormonesСлайд 24 Etiopathogenesis of DM
Type 1 DM - characteristics
- it is most typical in individuals under 30
years of age (juvenile DM)- 80 % - 90 % of beta cells in the islets of Langerhans
are destroyed
Possible mechanisms of beta cells destruction:
a) by islet cell antibodies of the IgG class
b) by non-immune mechanism (idiopathic up to now)
Слайд 25Evidence suggest that type 1 DM is caused by a
gradual process
of autoimmune destruction of beta cells in genetically
susceptiveindividuals
The result of beta cells destruction:
- almost no or absolute no functional insulin is produced
- glucagon is present in relative excess
- individuals are prone to ketoacidosis
- insulin resistance is rare
- patients are insulin dependent
Слайд 26Type 2 DM - characteristics
1. Primary disturbance:
- biological activity of insuline
2. Compensatory hyperinsulinemia
- due to concentration of blood glucose3. Insulinoresistentia:
- ability of insuline to inhibit production of glucose in
liver glucose production
Слайд 27 Type 2 DM -characteristics
- is rare in populations
not affected by urban modernization
- adult onset (mostly after
40 years of age, slow, insidious onset)
- results from the action of several abnormal genes ; - inherited
susceptibility, familial tendency stronger than for type 1 DM
- associated with long - duration obesity (mainly visceral)
- islet of Langerhans cells antibodies are rare
- increased insulin resistance
- nonspecific changes (damage) of islet cells
- usually not insulin dependent
- individuals are not ketosis prone (but they may form
keton bodies under stress)
Слайд 29Main symptomes and signs of DM and mechanisms
of their
onset
Hyperglycemia:
relative or absolute deficiency of insulin effect
transport ofglucose to muscle and fat cells glycemia
insulin effect gluconeogenesis in liver blood level of
glucose
glycogenolysis (?)
Glycosuria: hyperglycemia (8-15 mmol/l) glycosuria
Polyuria: high blood level of glucose increased amount of glucose
filtered by the glomeruli of the kidney absorbtion capacity
of renal tubules for glucose is exceeded glycosuria results,
accompanied by large amounts of water lost in the urine
(osmotic effect of glucose)
Слайд 30Polydipsia : high blood level of glucose hyperosmolality of
intracellular dehydratation
creation of thirst feeling (in hypothalamus)
intake of fluids
Polyphagia: depletion of cellular stores of carbohydrates, fats,
and proteins results in cellular starvation and a
corresponding increase in hunger
Weight loss : fluid loss in osmotic diuresis, loss of body tissue
as fats and proteins are used for energy creation
Fatigue : metabolic changes result in poor use of food
products lethargy and fatique
Слайд 31Complications of Diabetes Mellitus
Acute complications
• Hypoglycemia
• Ketoacidosis
• Hyperosmolar hyperglycemic nonketotic coma
B. Chronic complications
• Diabetic micro- and macrovascular changes
• Diabetic neuropathy
• Diabetic retinopathy
• Diabetic nephropathy
• Other complications
Слайд 32Acute complications
1. Hypoglycemia ( 3.3mmol/l of blood glucose) - results
from:
a) exogenous causes - overdose
of insuline plus inadequate food intake, increased exercise
- overdose of oral hypoglycemic agents
- alcohol
- other agents (e.g. salicylates)
b) endogenous causes - insulinoma (neoplasm of beta cells
of islet of Langerhans)
- extrapancreatic neoplasm (hepatomas,
tumor of GIT)
- inborn errors of metabolism (fructose
intolerance)
Symptoms and signs of hypoglycemia are caused by epinephrine release (sweating, shakiness, headache, palpitation) and by lack of glucose in the brain (bizarre behaviour, dullness, coma).
Слайд 33Hypoglycemia unawareness (HU)
Cause: antihypoglycemic mechanisms are insufficient
Result: hypoglycemia develops without
warning
symptoms and
signsPathomechanism involved in HU development:
• Primary defect is localised to the CNS
- or loss of neurotransmiter production on
hypoglycemic stimulus
- reactivity of peripheral tissues counterregulatory
hormones
Consequences: Deep hypoglycemia hypoglycemic coma
death
Слайд 34Diabetic ketoacidosis - the most serious metabolic
complication of
DM
– It develops when there is severe
insulin insufficiency– Insulin insufficiency triggers a complex metabolic reactions
which involve:
- decreased glucose utilisation hyperglycemia and glycosuria
- acceleration of gluconeogenesis hyperglycemia
- decreased lipogenesis and increased lipolysis increase
oxidation of free fatty acids production of ketone bodies
(aceto-acetate, hydroxy-butyrate, and acetone) hyperketonemia
metabolic acidosis coma
Слайд 35Hyperosmolar hyperglycemic nonketotic coma(HHNC)
(hyperosmolar hyperglycemic syndrome)
a) - insulin is present
to some degree it inhibits fat breakdown lack of ketosis
b) - insulin is present to some degree its effectivity is
less than needed for effective glucose transport
hyperglycemia glycosuria and polyuria body fluids
depletion intracellular dehydration neurologic
disturbancies (stupor, coma)
Слайд 37B. Chronic complications
Today, long-term survival
of patient suffering from DM is the
rule.
As a result, the problems of neuropathy, microvasculardisease, and macrovascular disease have become important
1. Diabetic neuropathies(DN) - probably the most common
complication in DM
Pathogenesis:
a) vascular damage of vasa nervorum
b) metabolic damage of nerve cels
c) non-enzymatic glycation of proteins
The very first morphologic and functional changes:
- axonal degeneration preferentially involved unmyelinated fibers
(in spinal cord, the posterior root ganglia, peripheral nerves)
Слайд 41 Functional consequences:
- abnormalities in
motor nerve function
(in advanced stages
of DM)- sensory nerve conduction is impaired
- autonomic neuropathy (diabetic diarrhea, orthostatic
hypotension....)
Possible mechanisms involved in development of DN
- blood supply to nerves is decreased because of microvascular damage
(vasa nervorum may be damaged)
- energy source for normal rest membrane potential maintain is
insufficient
- increased accumulation of sorbitol and fructose, decreased
concentration of myoinositol
- non-enzymatic glycation of proteins
Слайд 42Main functions of vascular endotelium
• regulates vascular tone and permeability
•
regulates the balance between coagulation and fibrinolysis
• regulation of subendothelial
matrix composition• influences extravasation of leucocytes
• influences the proliferation of vascular smooth muscle
and renal mesangial cells
To curry out these functions, the endothelium produces
components of extracellular matrix and variety of
regulatory mediators
2. Diabetic micro- and macroangiopathies
Слайд 43Microvascular disease - specific lesion of DM that affect capillaries
and arterioles of the retina, renal
glomeruli, peripheral nerves, musclesand skin
Characteristic lesion :
- thickening of the capillary basement membrane
- increased accumulation of glycoprotein in wall of small
arteries and capillaries
a)Retinopathy - it is the result of retinal ischemia caused by
microangiopathy
Pathomechanisms involved in retinopathy occurence:
- increased retinal capillary permeability, vein dilation
- microaneurism formation and hemorrhages
- narrowing of small arteries lumen
- neovascularisation and fibrous tissue formation within
the retina
- retinal scars formation blindness
Слайд 45Diabetic retinopathy – hard exudates, dot-and-blot hemorrhages,
hard exudates attacks the
fovea, cotton-wool patches,microaneurysms
Слайд 47
b) Nephropathy - it is the result of glomerular changes
caused by DM
Pathologic processes involved in diabetic nephropathy:
- glomerular enlargement - diffuse intercapillary
- glomerular basement membrane glomerulosclerosis
thickening
proteinuria
- systemic hypertension often occurs (more than 0.3g/day)
- neuropathy - see at B1.
Слайд 48Diabetic nephropathy - nodular glomerulosclerosis
and hyalinic atherosclerosis of small
artery
Слайд 50B) Macrovascular disease - atherosclerotic lesion
of
larger arteries (coronary arteries, brain arteries, peripheral arteries)
Main biochemical disturbancies leading to macrovasculardisease:
- accumulation of sorbitol in the vascular intima
- hyperlipoproteinemia vascular abnormality in blood
coagulation, occlusion by thrombus,
accelerated atherosclerosis
a) Coronary artery disease acute or chronic myocardial
ischemia and/or infarction
b) Stroke acute or chronic cerebral ischemia
c) Peripheral vascular disease gangrene and amputation
(diabetic foot)
Слайд 533. Infection
Persons with DM are at increased risk
for infection
throughout the body.
Causes:
- disturbancies of senses (neuropathy, retinopathy)
decreasing the function of early warning system
breaks in skin integrity
- tissue hypoxia (macro- and microangiopathy)
- increased level glucose in body fluids pathogens
are able to multiply rapidly
- white blood cells supply to the tissue is decreased
- function of white blood cells is impaired