Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Cardiology/EKG Board Review
Содержание
- 1. Cardiology/EKG Board Review
- 2. ObjectivesReview general method for EKG interpretationReview specific
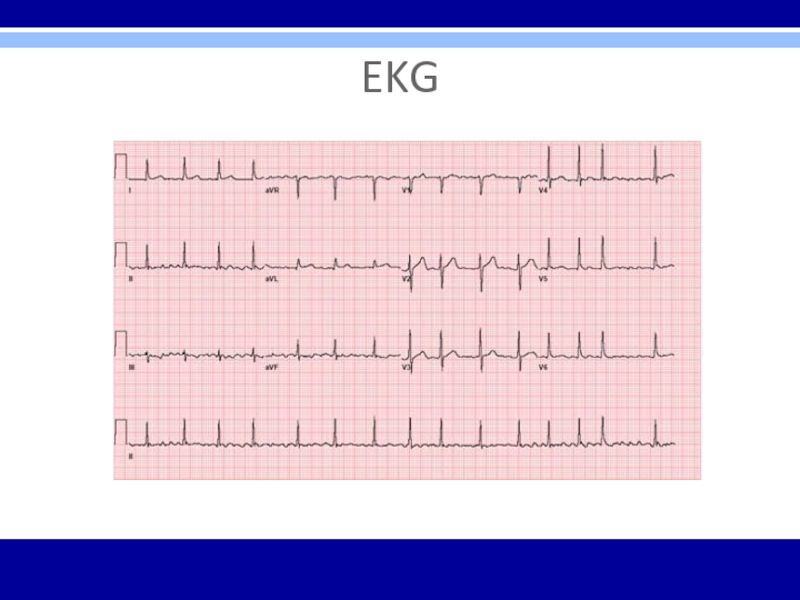
- 3. EKG
- 4. EKG – 12 LeadsAnterior Leads - V1,
- 5. 11 Step Method for Reading EKG’s“Data Gathering”
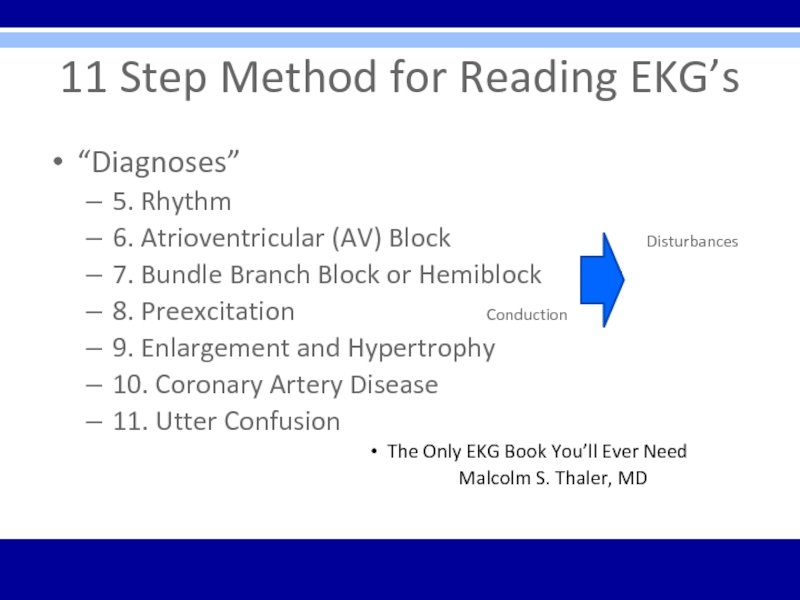
- 6. 11 Step Method for Reading EKG’s“Diagnoses”5. Rhythm6.
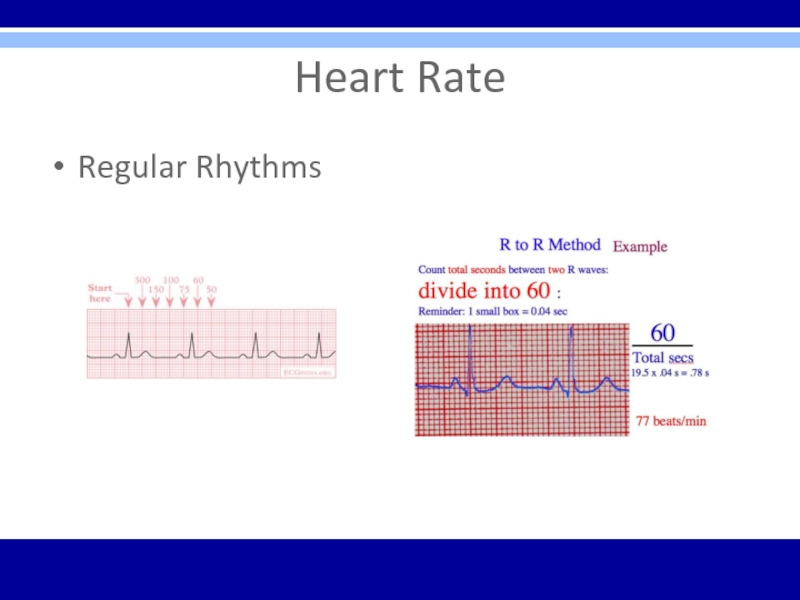
- 7. Heart RateRegular Rhythms
- 8. Heart RateIrregular Rhythms
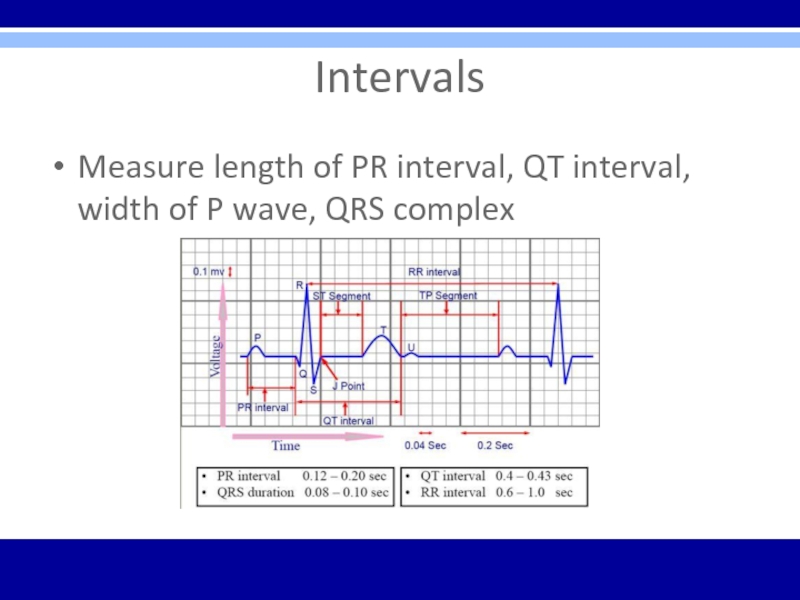
- 9. IntervalsMeasure length of PR interval, QT interval, width of P wave, QRS complex
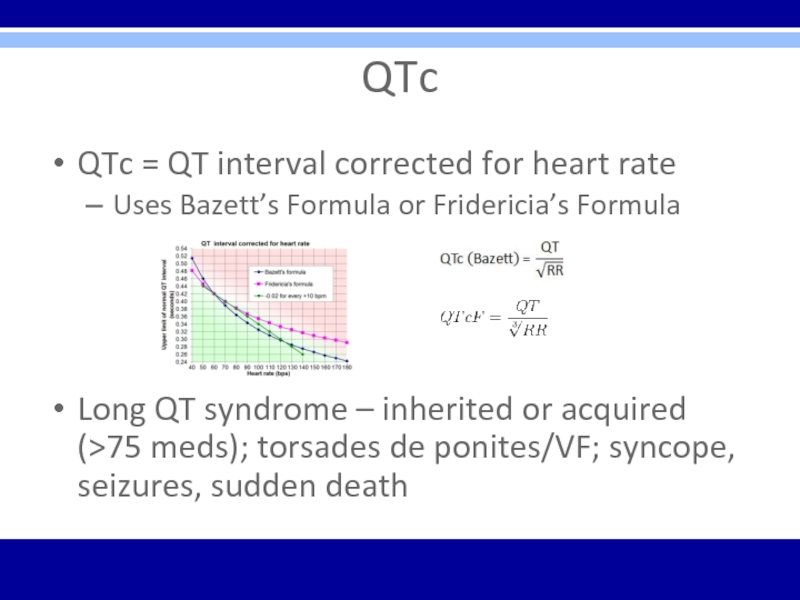
- 10. QTcQTc = QT interval corrected for heart
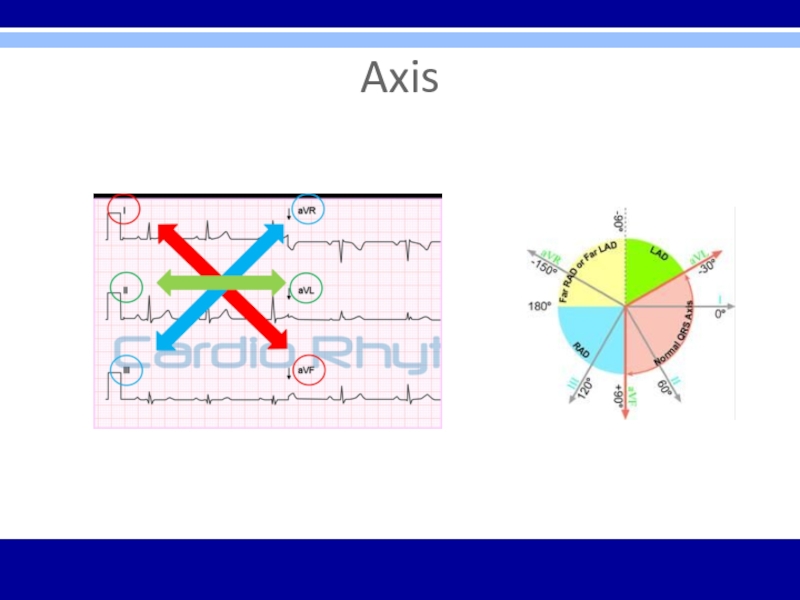
- 11. Axis
- 12. Rhythm4 Questions1. Are normal P waves present?2.
- 13. Types of ArrhythmiasArrhythmias of sinus originEctopic rhythmsConduction BlocksPreexcitation syndromes
- 14. AV BlockDiagnosed by examining relationship of P
- 15. Слайд 15
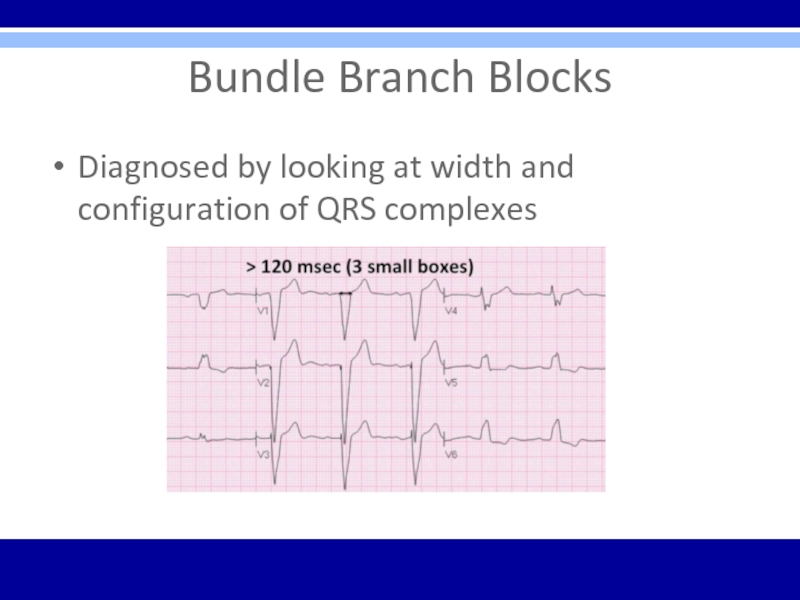
- 16. Bundle Branch BlocksDiagnosed by looking at width and configuration of QRS complexes
- 17. Bundle Branch BlocksRBBB criteria:1. QRS complex >
- 18. Bundle Branch Blocks
- 19. HemiblocksDiagnosed by looking at right or left
- 20. Bifascicular Block RBBB with LAHRBBB – QRS
- 21. PreexcitationWolff-Parkinson-White (WPW) Syndrome1. PR interval < 0.12
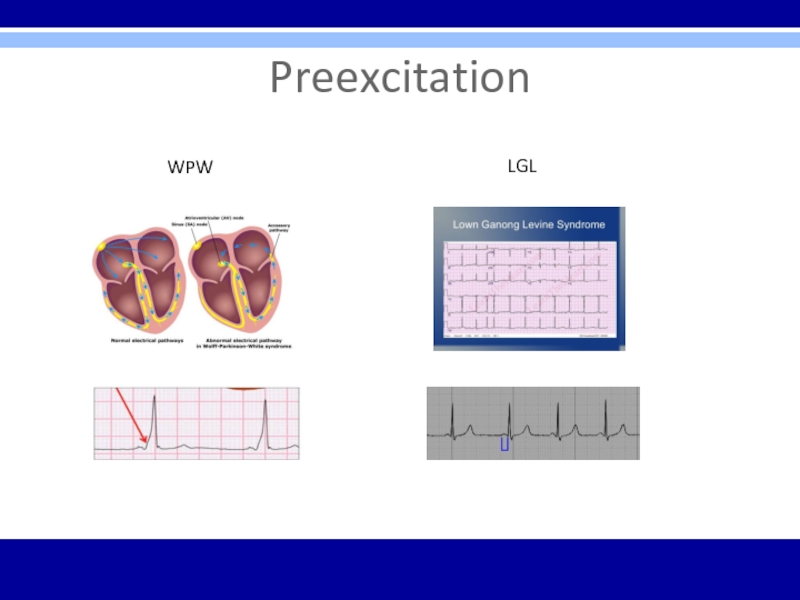
- 22. PreexcitationWPWLGL
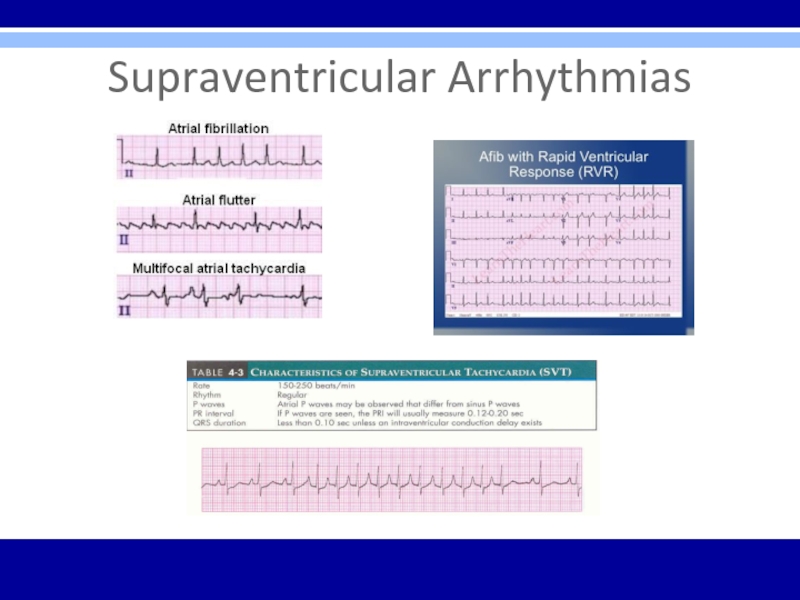
- 23. Supraventricular ArrhythmiasPSVT- regular; P waves retrograde if
- 24. Supraventricular Arrhythmias
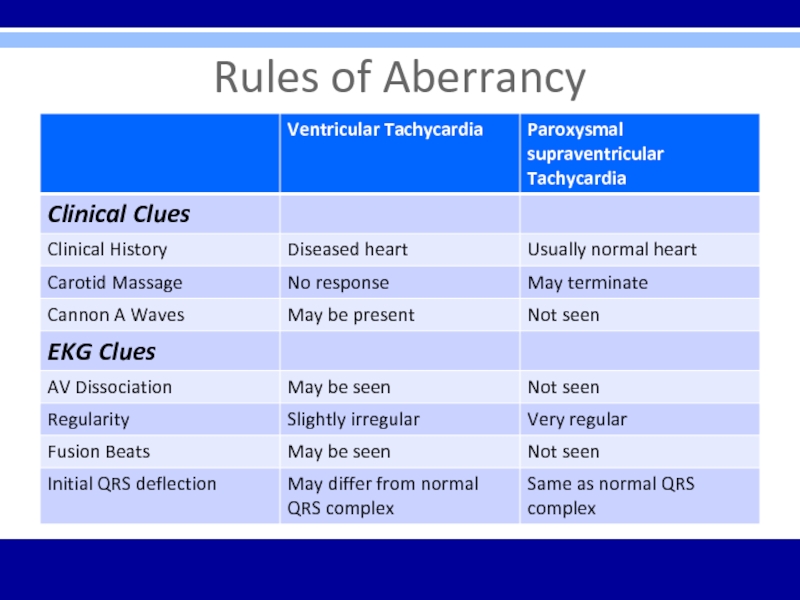
- 25. Rules of Aberrancy
- 26. Ventricular ArrhythmiasTorsades de PointesPVC’s
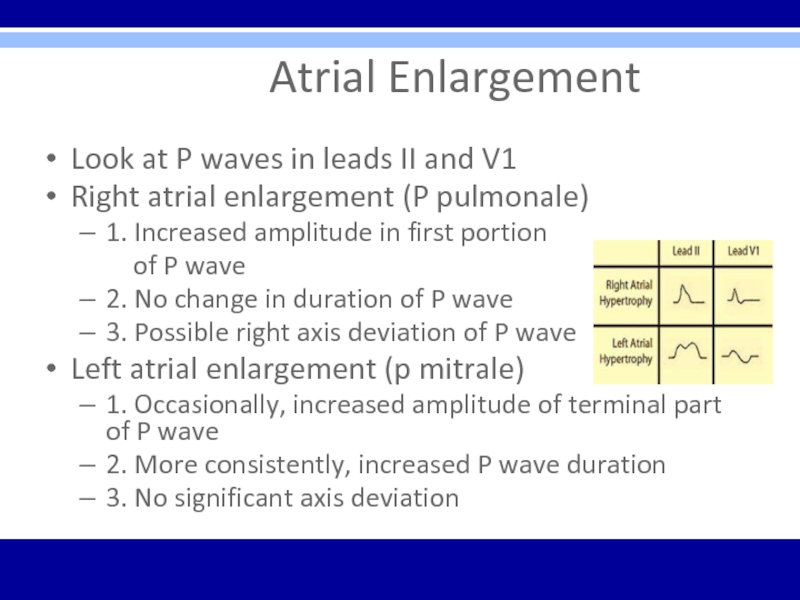
- 27. Atrial EnlargementLook
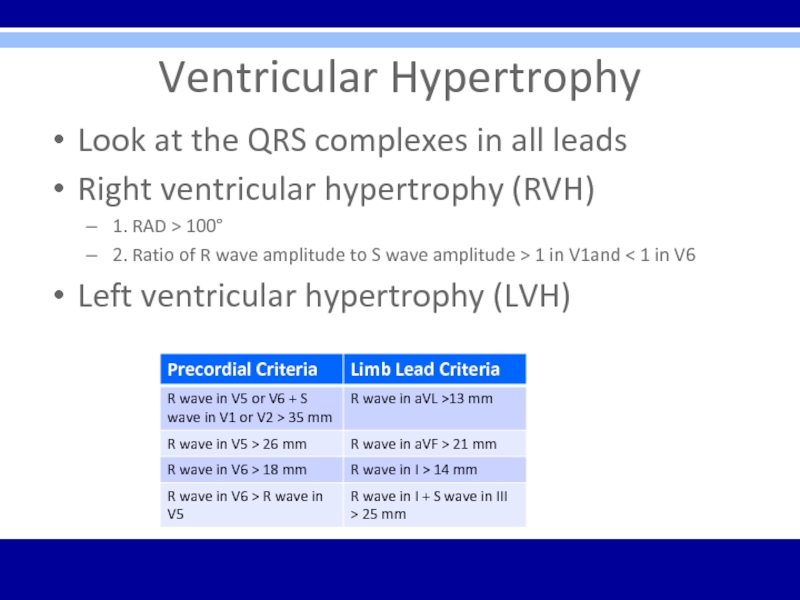
- 28. Ventricular HypertrophyLook at the QRS complexes in
- 29. Myocardial InfarctionDx – Hx, PE, serial cardiac
- 30. Q WavesCriteria for significant Q wavesQ wave
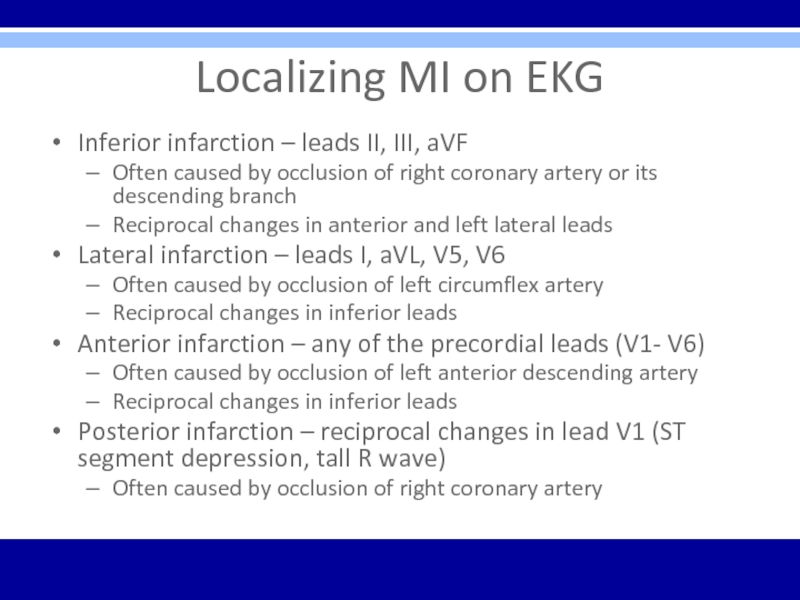
- 31. Localizing MI on EKGInferior infarction – leads
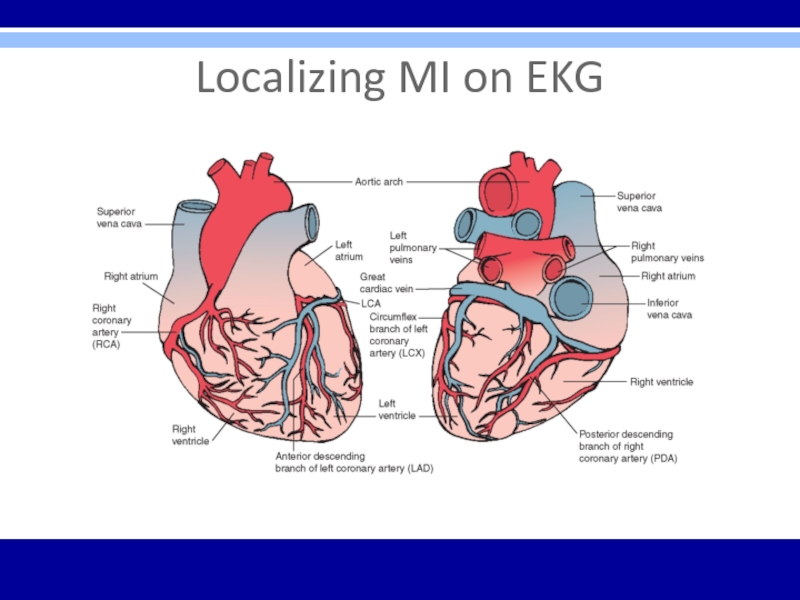
- 32. Localizing MI on EKG
- 33. ST segmentElevation Seen with evolving infarction, Prinzmetal’s
- 34. Electrolyte Abnormalities on EKGHyperkalemia – peaked T
- 35. DrugsDigitalis Therapeutic levels – ST segment and
- 36. EKG ∆’s in other Cardiac ConditionsPericarditis –
- 37. EKG ∆’s in Pulmonary Disorders COPD
- 38. EKG ∆’s in Other ConditionsHypothermia – Osborn
- 39. Utter ConfusionVerify lead placementRepeat EKGRepeat standardized process
- 40. Arrhythmia Indications to Consult CardiologyDiagnostic or management
- 41. Care Considerations Prior to Cardiology ConsultThorough
- 42. Pacemaker ConsiderationsThird-degree (complete) AV blockSymptomatic lesser degree
- 43. Osteopathic ConsiderationsTreatments –Lymphatics – thoracic inlet, abdominal
- 44. Clinical Cases/EKG’s
- 45. Case 153 year old caucasian female with
- 46. Case 1Diagnosis? EKG findings?
- 47. Case 1Acute anterior ST-elevation MI with “tombstone” or “fireman’s hat” in V1-V4Tx? Localization?
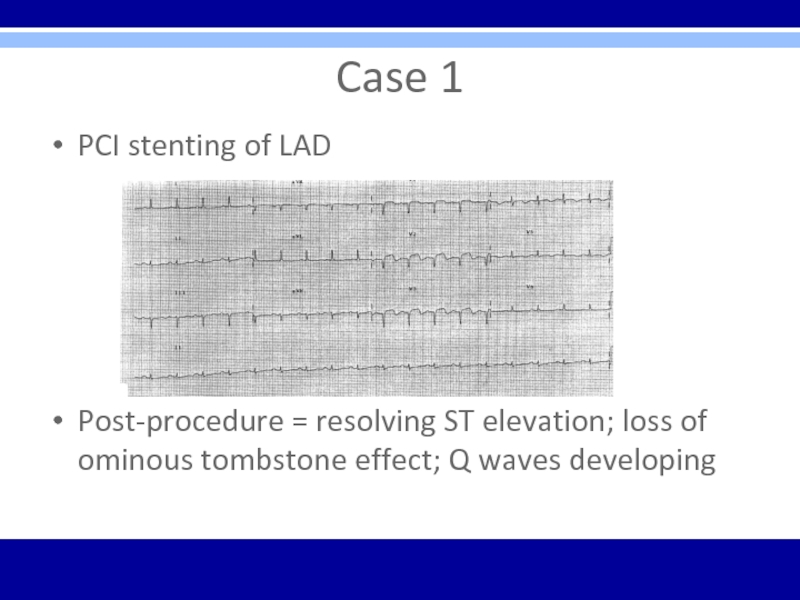
- 48. Case 1PCI stenting of LADPost-procedure = resolving
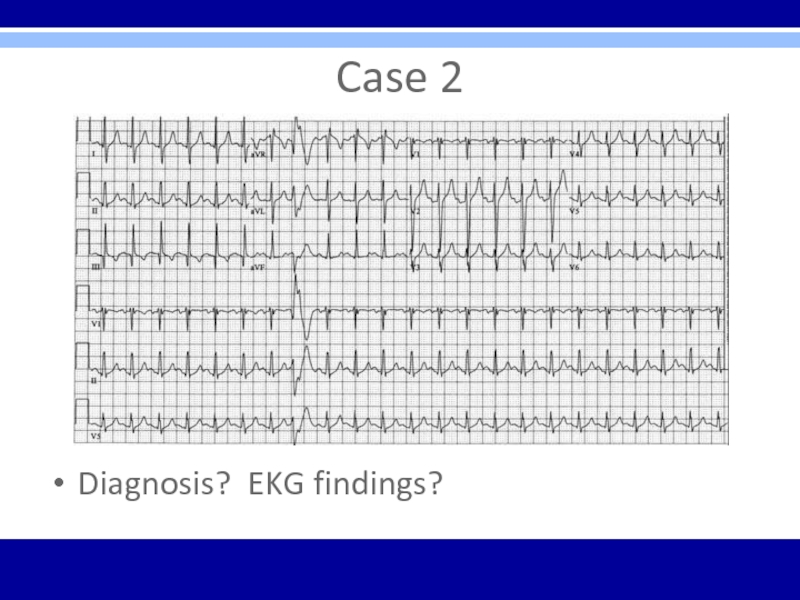
- 49. Case 245 yo male presents with acute
- 50. Case 2Diagnosis? EKG findings?
- 51. Case 2Acute PE with sinus tachycardia, a PVC, and S1Q3T3 pattern
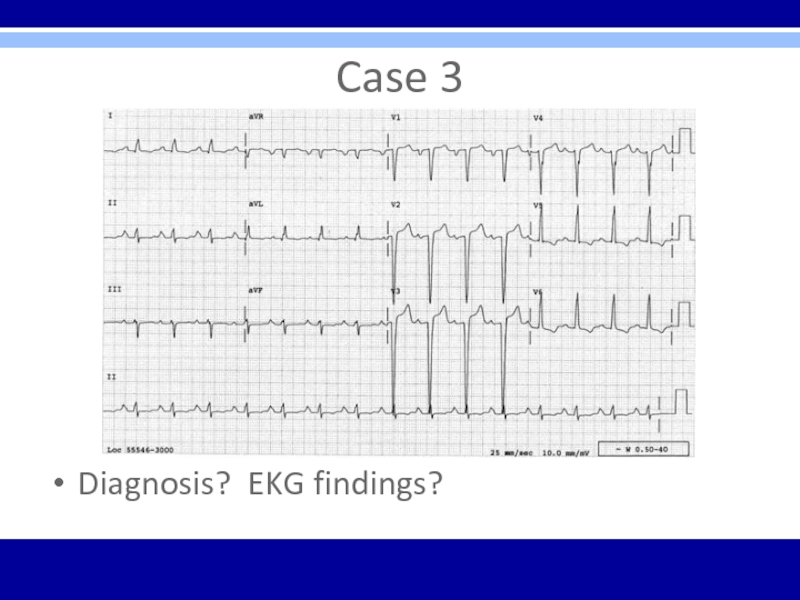
- 52. Case 372 yo male presents to the
- 53. Case 3Diagnosis? EKG findings?
- 54. Case 3LVH – QRS voltage criteria in precordial leads and repolarization changes in V5, V6
- 55. Case 427 yo female presents to the
- 56. Case 4Diagnosis? EKG findings?
- 57. Case 4SVT – regular, narrow-QRS tachycardia, rate of 160 bpm
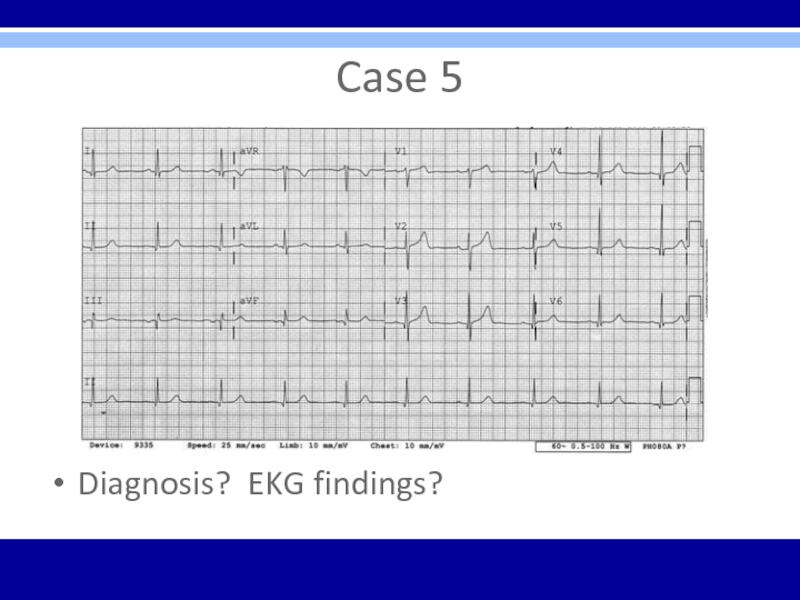
- 58. Case 546 yo male presents to ED
- 59. Case 5Diagnosis? EKG findings?
- 60. Case 5Normal EKG
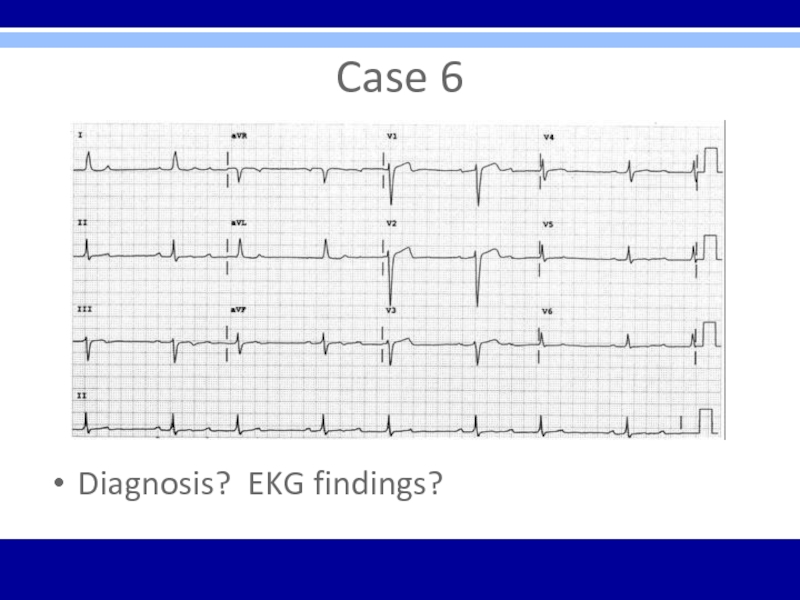
- 61. Case 656 yo female presents to family
- 62. Case 6Diagnosis? EKG findings?
- 63. Case 6Second degree AV block – Mobitz
- 64. Case 728 yo male presents for commercial
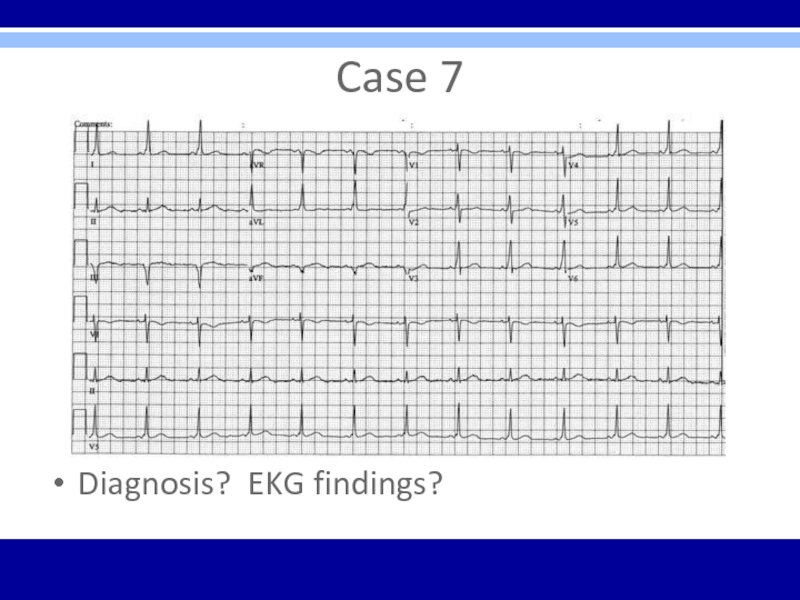
- 65. Case 7Diagnosis? EKG findings?
- 66. Case 7Typical preexcitation (WPW) patternShort PR interval
- 67. Case 832 yo male presents to ED
- 68. Case 8Diagnosis? EKG findings?
- 69. Case 8Acute pericarditis – diffuse ST elevation with PR segment depression is diagnostic
- 70. Case 967 yo male presents to his
- 71. Case 9Diagnosis? EKG findings?
- 72. Case 9Atrial fibrillation – irregularly irregular without
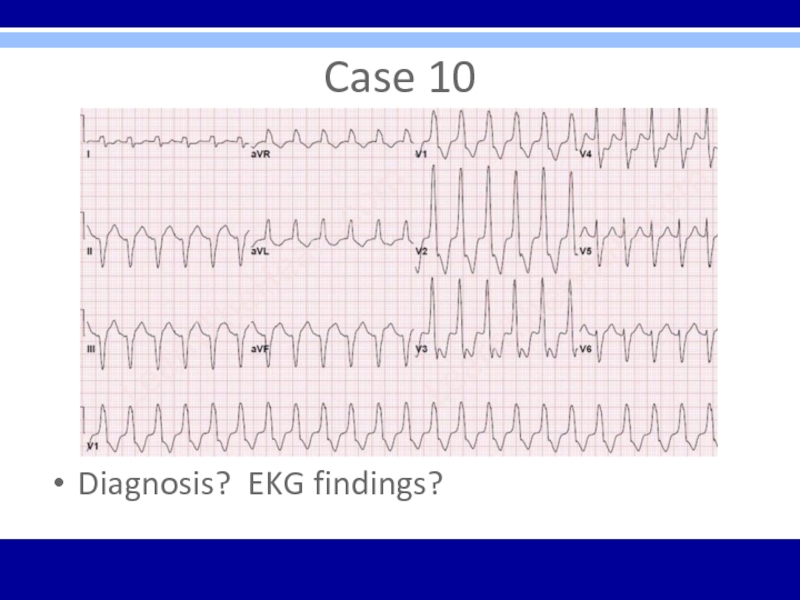
- 73. Case 1079 yo male brought to ED
- 74. Case 10Diagnosis? EKG findings?
- 75. Case 10Monomorphic sustained ventricular tachycardia (VT) –
- 76. Case 1182 yo female admitted to acute
- 77. Case 11Diagnosis? EKG findings?
- 78. Case 11LBBB – wide QRS; broad, notched
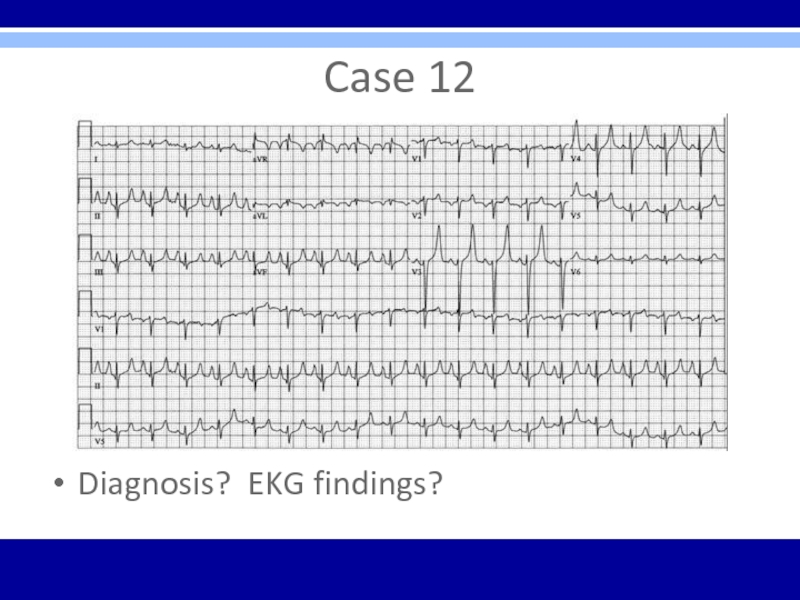
- 79. Case 1259 yo male presents to ED
- 80. Case 12Diagnosis? EKG findings?
- 81. Case 12Hyperkalemia – tall peaked T waves
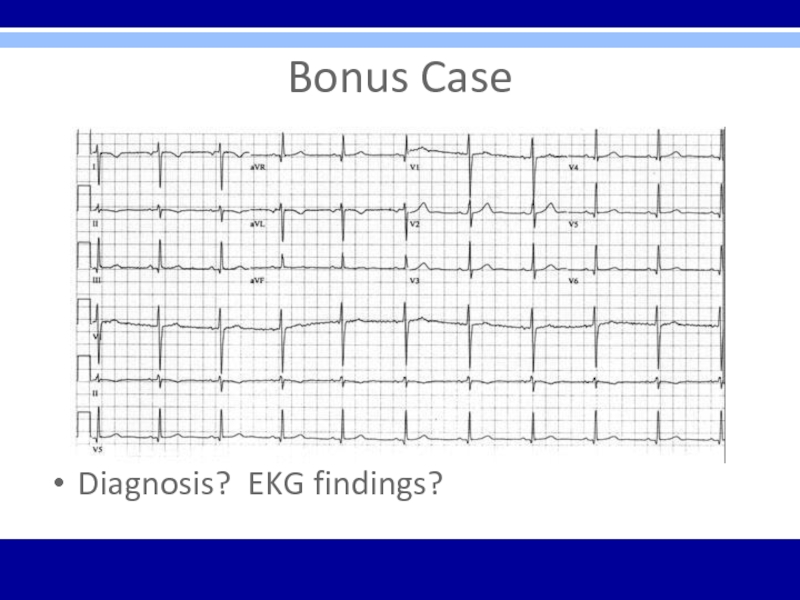
- 82. Bonus Case18 yo male undergoing military physical
- 83. Bonus CaseDiagnosis? EKG findings?
- 84. Bonus CaseReversed arm leads – inverted P
- 85. Board Exam PointsEKG’s likely to have 1
- 86. Questions?
- 87. ResourcesSources and Suggested ReferencesThe Only EKG Book
- 88. Скачать презентанцию
ObjectivesReview general method for EKG interpretationReview specific points of “data gathering” and “diagnoses” on EKGReview treatment considerationsReview clinical cases/EKG’sBoard exam considerations
Слайды и текст этой презентации
Слайд 1Cardiology/EKG
Board Review
Michael J. Bradley D.O.
DME/Program Director
Family Medicine Residency
Слайд 2Objectives
Review general method for EKG interpretation
Review specific points of “data
gathering” and “diagnoses” on EKG
considerationsСлайд 4EKG – 12 Leads
Anterior Leads - V1, V2, V3, V4
Inferior
Leads – II, III, aVF
Left Lateral Leads – I, aVL,
V5, V6Right Leads – aVR, V1
Слайд 511 Step Method for Reading EKG’s
“Data Gathering” – steps 1-4
1.
Standardization – make sure paper and paper speed is standardized
2.
Heart Rate3. Intervals – PR, QT, QRS width
4. Axis – normal vs. deviation
Слайд 611 Step Method for Reading EKG’s
“Diagnoses”
5. Rhythm
6. Atrioventricular (AV) Block
Disturbances
7. Bundle Branch Block or Hemiblock of
8. Preexcitation Conduction
9. Enlargement and Hypertrophy
10. Coronary Artery Disease
11. Utter Confusion
The Only EKG Book You’ll Ever Need
Malcolm S. Thaler, MD
Слайд 10QTc
QTc = QT interval corrected for heart rate
Uses Bazett’s Formula
or Fridericia’s Formula
Long QT syndrome – inherited or acquired (>75
meds); torsades de ponites/VF; syncope, seizures, sudden deathСлайд 12Rhythm
4 Questions
1. Are normal P waves present?
2. Are QRS complexes
narrow or wide (≤ or ≥ 0.12)?
3. What is relationship
between P waves and QRS complexes?4. Is rhythm regular or irregular?
Sinus rhythm = normal P waves, narrow QRS complexes, 1 P wave to every 1 QRS complex, and regular rhythm
Слайд 13Types of Arrhythmias
Arrhythmias of sinus origin
Ectopic rhythms
Conduction Blocks
Preexcitation syndromes
Слайд 14AV Block
Diagnosed by examining relationship of P waves to QRS
complexes
First Degree – PR interval > 0.2 seconds; all beats
conducted through to the ventriclesSecond Degree – only some beats are conducted through to the ventricles
Mobitz Type I (Wenckebach) – progressive prolongation of PR interval until a QRS is dropped
Mobitz Type II – All-or-nothing conduction in which QRS complexes are dropped without PR interval prolongation
Third Degree – No beats are conducted through to the ventricles; complete heart block with AV dissociation; atria and ventricles are driven by individual pacemakers
Слайд 17Bundle Branch Blocks
RBBB criteria:
1. QRS complex > 0.12 seconds
2. RSR’
in leads V1 and V2 (rabbit ears) with ST segment
depression and T wave inversion3. Reciprocal changes in leads V5, V6, I, and aVL
LBBB criteria:
1. QRS complex > 0.12 seconds
2. Broad or notched R wave with prolonged upstroke in leads V5, V6, I, and aVL with ST segment depression and T wave inversion.
3. Reciprocal changes in leads V1 and V2.
4. Left axis deviation may be present.
Слайд 19Hemiblocks
Diagnosed by looking at right or left axis deviation
Left Anterior
Hemiblock
1.Normal QRS duration and no ST segment or T wave
changes2. Left axis deviation greater than -30°
3. No other cause of left axis deviation is present
Left Posterior Hemiblock
1. Normal QRS duration and no ST segment or T wave changes
2. Right axis deviation
3. No other cause of right axis deviation is present
Слайд 20Bifascicular Block
RBBB with LAH
RBBB – QRS > 0.12 sec
and RSR’ in V1 and V2 with LAH – left
axis deviationRBBB with LPH
RBBB – RS > 0.12 sec and RSR’ in V1 and V2 with LPH – right axis deviation
Слайд 21Preexcitation
Wolff-Parkinson-White (WPW) Syndrome
1. PR interval < 0.12 sec
2. Wide QRS
complexes
3. Delta waves seen in some leads
Lown-Ganong-Levine (LGL) Syndrome –
1.
PR interval < 0.12 sec2. Normal QRS width
3. No delta wave
Common Arrhythmias
Paroxysmal Supraventricular Tachycardia (PSVT) – narrow QRS’s are more common than wide QRS’s
Atrial Fibrillation – can be rapid and lead to ventricular fibrillation
Слайд 23Supraventricular Arrhythmias
PSVT- regular; P waves retrograde if visible; rate 150-250
bpm; carotid massage: slows or terminates
Flutter – regular; saw-toothed pattern;
2:1, 3:1, 4:1, etc. block; atrial rate 250-350 bpm; ventricular rate ½, ⅓, ¼, etc. of atrial rate; carotid massage: increases blockFibrillation – irregular; undulating baseline; atrial rate 350 to 500 bpm; variable ventricular rate; carotid massage: may slow ventricular rate
Multifocal atrial tachycardia (MAT) – irregular; at least 3 different P wave morphologies; rate –usually 100 to 200 bpm; sometimes < 100 bpm; carotid massage: no effect
PAT – regular; 100 to 200 bpm; characteristic warm-up period in the automatic form; carotid massage: no effect, or mild slowing
Слайд 27 Atrial Enlargement
Look at P waves
in leads II and V1
Right atrial enlargement (P pulmonale)
1. Increased
amplitude in first portion of P wave
2. No change in duration of P wave
3. Possible right axis deviation of P wave
Left atrial enlargement (p mitrale)
1. Occasionally, increased amplitude of terminal part of P wave
2. More consistently, increased P wave duration
3. No significant axis deviation
Слайд 28Ventricular Hypertrophy
Look at the QRS complexes in all leads
Right
ventricular hypertrophy (RVH)
1. RAD > 100°
2. Ratio of R wave
amplitude to S wave amplitude > 1 in V1and < 1 in V6Left ventricular hypertrophy (LVH)
Слайд 29Myocardial Infarction
Dx – Hx, PE, serial cardiac enzymes, serial EKG’s
3
EKG stages of acute MI
1. T wave peaks and
then inverts2. ST segment elevates
3. Q waves appear
Слайд 30Q Waves
Criteria for significant Q waves
Q wave > 0.04 seconds
in duration
Q wave depth > ⅓ height of R wave
in same QRS complexCriteria for Non-Q Wave MI
T wave inversion
ST segment depression persisting > 48 hours in appropriate clinical setting
Слайд 31Localizing MI on EKG
Inferior infarction – leads II, III, aVF
Often
caused by occlusion of right coronary artery or its descending
branchReciprocal changes in anterior and left lateral leads
Lateral infarction – leads I, aVL, V5, V6
Often caused by occlusion of left circumflex artery
Reciprocal changes in inferior leads
Anterior infarction – any of the precordial leads (V1- V6)
Often caused by occlusion of left anterior descending artery
Reciprocal changes in inferior leads
Posterior infarction – reciprocal changes in lead V1 (ST segment depression, tall R wave)
Often caused by occlusion of right coronary artery
Слайд 33ST segment
Elevation
Seen with evolving infarction, Prinzmetal’s angina
Other causes –
J point elevation, apical ballooning syndrome, acute pericarditis, acute myocarditis,
hyperkalemia, pulmonary embolism, Brugada syndrome, hypothermiaDepression
Seen with typical exertional angina, non-Q wave MI
Indicator of + stress test
Слайд 34Electrolyte Abnormalities on EKG
Hyperkalemia – peaked T waves, prolonged PR,
flattened P waves, widened QRS, merging QRS with T waves
into sine wave, VFHypokalemia – ST depression, flattened T waves, U waves
Hypocalcemia – prolonged QT interval
Hypercalcemia – shortened QT interval
Слайд 35Drugs
Digitalis
Therapeutic levels – ST segment and T wave changes
in leads with tall R waves
Toxic levels – tachyarrhythmias and
conduction blocks; PAT with block is most characteristic.Multiple drugs associated with prolonged QT interval, U waves
Sotalol, quinidine, procainamide, disopyramide, amiodarone, dofetilide, dronedarone, TCA’s, erythromycin, quinolones, phenothiazines, various antifungals, some antihistamines, citalopram (only prolonged QT interval – dose-dependent)
Слайд 36EKG ∆’s in other Cardiac Conditions
Pericarditis – Diffuse ST segment
elevations and T wave inversions; large effusion may cause low
voltage and electrical alternans (altering QRS amplitude or axis and wandering baseline)Myocarditis – conduction blocks
Hypertrophic Cardiomyopathy – ventricular hypertrophy, left axis deviation, septal Q waves
Слайд 37EKG ∆’s in Pulmonary Disorders
COPD – low voltage,
right axis deviation, and poor R wave progression.
Chronic cor
pulmonale – P pulmonale with right ventricular hypertrophy and repolarization abnormalitiesAcute pulmonary embolism – right ventricular hypertrophy with strain, RBBB, and S1Q3T3 (with T wave inversion). Sinus tachycardia and atrial fibrillation are common.
Слайд 38EKG ∆’s in Other Conditions
Hypothermia – Osborn waves, prolonged intervals,
sinus bradycardia, slow atrial fibrillation, beware of muscle tremor artifact
CNS
Disease – diffuse T wave inversion with T waves wide and deep, U wavesAthlete’s Heart – sinus bradycardia, nonspecific ST segment and T wave changes, RVH, LVH, incomplete RBBB, first degree or Wenckebach AV block, possible supraventricular arrhythmia
Слайд 39Utter Confusion
Verify lead placement
Repeat EKG
Repeat standardized process of EKG analysis-
starting over from the beginning with basics – rate, intervals,
axis, rhythm, etc. and proceed through entire stepwise analysisConsider Cardiology consultation
Слайд 40Arrhythmia Indications to Consult Cardiology
Diagnostic or management uncertainty
Medications not controlling
symptoms
Patient is in high-risk occupation or participates in high-risk activities
(pilot, scuba driving)Patients prefers intervention over long-term meds
Preexcitation
Underlying structural heart disease
Associated syncope or other significant symptoms
Wide QRS
Слайд 41Care Considerations Prior to
Cardiology Consult
Thorough Hx and PE
Basic labs
EKG
and repeat EKG
Holter monitor
Echocardiogram
Acuity of care required – consider risks,
hemodynamic stabilityСлайд 42Pacemaker Considerations
Third-degree (complete) AV block
Symptomatic lesser degree AV block or
bradycardia
Sudden onset of various combinations of AV block and BBB
during acute MIRecurrent tachycardias that can be overdriven and terminated by pacemakers
Слайд 43Osteopathic Considerations
Treatments –
Lymphatics – thoracic inlet, abdominal diaphragm, rib raising,
lymphatic pumps
Sympathetics (T1-T6) – cervical ganglion, rib raising, T1-T6, Chapman’s
reflexes, T10-L2 for adrenal/kidneyParasympathetics – OA/AA/cranial – vagus nerve
Слайд 45Case 1
53 year old caucasian female with 4 day hx
of severe central chest pain on exertion, previously alleviated with
rest; now worsened over last 24 hours and sustained at restPMHx – DM2, HTN, hyperlipidemia
Appears unwell, in pain, sweaty, and grey
Слайд 47Case 1
Acute anterior ST-elevation MI with “tombstone” or “fireman’s hat”
in V1-V4
Tx? Localization?
Слайд 48Case 1
PCI stenting of LAD
Post-procedure = resolving ST elevation; loss
of ominous tombstone effect; Q waves developing
Слайд 49Case 2
45 yo male presents with acute SOB s/p long
vacation in Paris
PMHx - asthma, Crohn’s disease, anxiety, GERD, tobacco
abuseVS 37, 148/92, 130, 26
Patient appears uncomfortable but otherwise unremarkable exam
Слайд 52Case 3
72 yo male presents to the office for evaluation
prior to cataract surgery
No complaints
PMHx – B/L cataracts, OA, HTN,
hyperlipidemia, and chronic low back painVS 37.2, 152/86, 74, 14
Слайд 55Case 4
27 yo female presents to the ED with c/o
chest discomfort and palpitations after studying all night for graduate
school examsAppears nervous and “uneasy” with rapid pulse
PMHx – unremarkable; no meds, admits to occasional alcohol, non-smoker, denies illicit drug use, used coffee to stay awake to study
Слайд 58Case 5
46 yo male presents to ED with c/o severe
HA persisting over 5 hours despite acetaminophen and NSAID attempts
as abortive therapyPMHx – occasional left shoulder pain, non-smoker
Construction worker
VSS; unremarkable exam
Слайд 61Case 6
56 yo female presents to family physician with c/o
light-headedness and occasional flutter in her chest
PMHx – anxiety, depression,
obesity, smokerWorks as retail store manager
VSS; course breath sounds, otherwise unremarkable exam
Слайд 63Case 6
Second degree AV block – Mobitz Type I –
Wenckebach (specifically 3:2 AV Wenckebach phenomenon where every 3rd P
wave is blocked)Слайд 64Case 7
28 yo male presents for commercial driver’s license (CDL)
evaluation
No complaints
VSS; asymptomatic; exam without significant findings
Слайд 66Case 7
Typical preexcitation (WPW) pattern
Short PR interval and delta waves
in many leads
Tx is close observation unless patient has had
SVT or atrial fibrillation which indicates tx with ablation of accessory pathway Слайд 67Case 8
32 yo male presents to ED with c/o feeling
sick for the last 6 days
Symptoms include fevers, cough, and
difficulty catching his breathPMHx – hyperlipidemia, obesity, metabolic syndrome
VS 38.1, 105, 128/84, 22
Слайд 70Case 9
67 yo male presents to his cardiologist for out-patient
6 week post-hospital visit
Previous hospitalization for non-cardiac chest pain
Post-hospital
cardiac meds – ACE inhibitor, beta blocker, aspirin, nitrateNo current complaints
Слайд 72Case 9
Atrial fibrillation – irregularly irregular without P waves
RBBB
– wide QRS with rsR’ pattern in V1, broad S
waves in leads I and aVLInferior infarct – non-acute (> 1 week) pathologic Q waves in inferior leads (II, III, and aVF)
Слайд 73Case 10
79 yo male brought to ED via EMS with
chest pain, SOB, and near-syncope
PMHx – unobtainable secondary to patient
distressVS – 36.9, 140’s, 82/40, 28
Слайд 75Case 10
Monomorphic sustained ventricular tachycardia (VT) – could rapidly deteriorate
into VF, torsades de pointes, asystole, or sudden death
Слайд 76Case 11
82 yo female admitted to acute care hospital secondary
to chest pain
PMHx – HTN, DM2, CHF, obesity, depression
Cardiology planning
cardiac catheterization secondary to new finding during initial consultationСлайд 78Case 11
LBBB – wide QRS; broad, notched R wave in
V5, V6 and I with ST depression and T wave
inversionСлайд 79Case 12
59 yo male presents to ED diaphoretic and in
distress
PMHx – HTN, ESRD, DM2, Left BKA
VS – 37.5, 108,
96/58, 24Слайд 81Case 12
Hyperkalemia – tall peaked T waves present throughout; other
progressive EKG changes may follow with increasing potassium levels –
prolonged PR interval, flattened P waves, widening QRS, sine wavesSinus tachycardia also present
Слайд 82Bonus Case
18 yo male undergoing military physical exam and evaluation
prior to boot camp
No complaints
PMHx – denies
VSS; exam unremarkable
Слайд 84Bonus Case
Reversed arm leads – inverted P waves in
lead I with normal R wave progression in precordial leads
Слайд 85Board Exam Points
EKG’s likely to have 1 main finding
Clinical case
likely included with each EKG
Question likely to focus on clinical
case as well as EKGStraight forward without tricks or obscure findings (not likely to see “zebras”)
Focus on common arrhythmias, common cardiac diagnoses, common non-cardiac EKG abnormalities, or emergent “can’t miss” diagnoses
Слайд 87Resources
Sources and Suggested References
The Only EKG Book You’ll Ever Need
- Malcolm S. Thaler
Rapid Interpretation of EKG’s – Dale Dubin,
M.D.“…Except for OMT!” – Dale Pratt-Harrington
American Family Physician – November 1, 2015
Up to Date
blog at wordpress.com
cme.umn.edu
ekgcasestudies.com
healio.com
lifeinthefastlane.com
learntheheart.com