Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
D I C
Содержание
- 1. D I C
- 2. WHAT IS DIC ?Disseminated intravascular coagulation (DIC) is an acquired
- 3. Normal Pregnancy – Hypercoagulable state.After the 1st
- 4. TYPES OF DIC ?ACUTE DIC – the physical findings are
- 5. Amniotic fluid has been shown to be
- 6. CHRONIC DIC- manifestation is thrombosis from excess
- 7. COMMON CAUSES OF DICACUTE DIC Abruptio PlacentaeEndotoxemia-
- 8. Vesicular moleDextran InfusionHemorrhagic shock due to –PPH
- 9. PATHOPHYSIOLOGYDIC is diagnosed in almost one-half of
- 10. PATHOPHYSIOLOGY
- 11. CLINICAL MANIFESTATIONClinical manifestations of DIC are related to
- 12. The hypercoagulability of DIC manifests as the
- 13. Bleeding from at 3 unrelated sites is
- 14. LAB INVESTIGATIONSThe laboratory investigation should include coagulation tests
- 15. LAB RESULTSprolongation of PT and/or aPTTplatelet counts less
- 16. DIC is an unlikely diagnosis in the
- 17. RISK ASSESSMENTDoes the patient have an underlying disorder
- 18. Prolonged PT 6 sec = 2 point.Fibrinogen
- 19. Слайд 19
- 20. TREATMENTThe morbidity and mortality associated with DIC
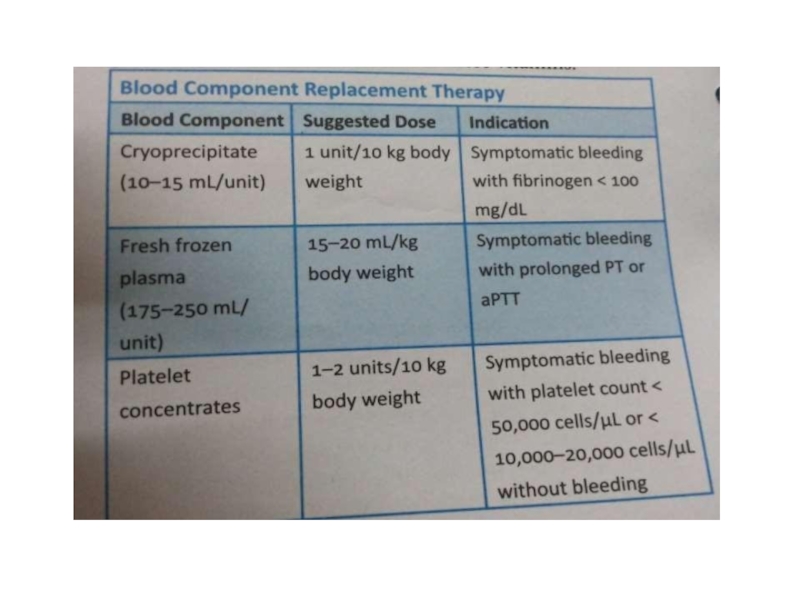
- 21. MANAGEMENT OFHEMORRHAGIC SYMPTOMSThe control of bleeding in DIC patients with marked thrombocytopenia (platelet counts
- 22. The PT (>1.5 times the normal) provides
- 23. The transfusion must be adjusted according to
- 24. REPLACEM ENT O F CO AG ULATI O N
- 25. The use of antifibrinolytic drugs, EACA, or
- 26. Слайд 26
- 27. THANK YOU!!
- 28. Скачать презентанцию
WHAT IS DIC ?Disseminated intravascular coagulation (DIC) is an acquired syndrome characterized by the intravascular activation of coagulation with loss of localization arising from different causes.It can originate from and cause damage to microvasculature,
Слайды и текст этой презентации
Слайд 2WHAT IS DIC ?
Disseminated intravascular coagulation (DIC) is an acquired syndrome characterized by
Слайд 3Normal Pregnancy – Hypercoagulable state.
After the 1st trimester there occurs
a marked increase in plasma fibrinogen( more than double the
non pregnant level ).Plasma fibrinolytic activity is decreased during pregnancy and returns to normal within one hour of delivery of placenta.
Слайд 4TYPES OF DIC ?
ACUTE DIC – the physical findings are those of underlying
or inciting etiology .
Patients with acute DIC have petechiae on
the soft palate and legs from thrombocytopenia and ecchymosis at venipuncture sites.Acute DIC occurs in obstetric calamities such as placental abruption
and amniotic fluid emboli.
Слайд 5Amniotic fluid has been shown to be able to activate
coagulation in vitro, and the degree of placental seperation correlates
with the extent of DIC , suggesting that leakage of thromboplastin like material from the placental system is responsible for the occurrence of DIC.Coagulation system may also be activated in patients with pre
eclampsia and HELLP syndrome.
Слайд 6CHRONIC DIC- manifestation is thrombosis from excess thrombin formation ,
the symptoms and signs of venous thromboembolism may be present.
Слайд 7COMMON CAUSES OF DIC
ACUTE DIC
Abruptio Placentae
Endotoxemia- septic abortions, chorioamnionitis,
pyelonephritis of pregnancy.
Amniotic Fluid Embolism
Severe pregnancy induced hypertension
Intra-amniotic hypertonic saline
Слайд 8Vesicular mole
Dextran Infusion
Hemorrhagic shock due to –PPH , Cs
CHRONIC DIC
– IUD ( prolonged retension of dead fetus).
Слайд 9PATHOPHYSIOLOGY
DIC is diagnosed in almost one-half of pregnant women with
abruptio placentae, or with amniotic fluid embolism. Trauma, particularly to
the brain, can also result in DIC.Слайд 11CLINICAL MANIFESTATION
Clinical manifestations of DIC are related to the magnitude of
the imbalance of hemostasis, to the underlying disease, or to
both.The most common findings are bleeding ranging from oozing from venipuncture sites, petechiae, and ecchymoses to severe hemorrhage from the gastrointestinal tract, lung, or into the CNS.
In chronic DIC, the bleeding symptoms are discrete and restricted to
skin or mucosal surfaces.
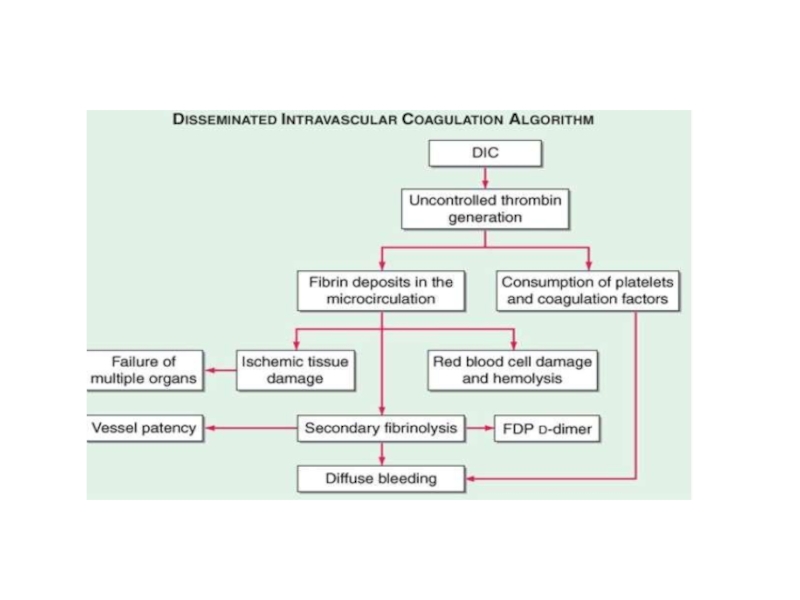
Слайд 12The hypercoagulability of DIC manifests as the occlusion of vessels
in the microcirculation and resulting organ failure.
Thrombosis of large vessels
and cerebral embolism can alsooccur.
Hemodynamic complications and shock are common among patients with acute DIC. The mortality ranges from 30 to >80% depending on the underlying disease, the severity of the DIC, and the age of the patient.
Слайд 13Bleeding from at 3 unrelated sites is particularly suggestive of
DIC.
Brain- altered state of consiousness , seizures
Lungs- respiratory distress
Heart- hypotension,
cardiac arrestKidney – Oliguria,Anuria, Acidosis
Слайд 14LAB INVESTIGATIONS
The laboratory investigation should include coagulation tests [aPTT, PT, thrombin
time (TT)] and markers of fibrin degradation products (FDPs), in
addition to platelet and red cell count and analysis of the blood smear.These tests should be repeated over a period of 6–8 hours because an initially mild abnormality can change dramatically in patients with severe DIC.
A reduction in platelet count at subsequent tests is a sensitive sign of DIC.
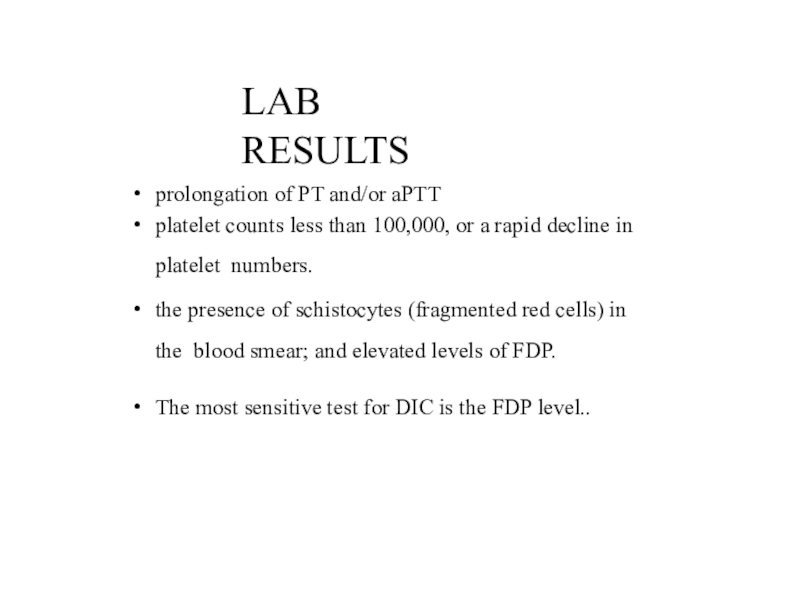
Слайд 15LAB RESULTS
prolongation of PT and/or aPTT
platelet counts less than 100,000, or
a rapid decline in platelet numbers.
the presence of schistocytes (fragmented
red cells) in the blood smear; and elevated levels of FDP.The most sensitive test for DIC is the FDP level..
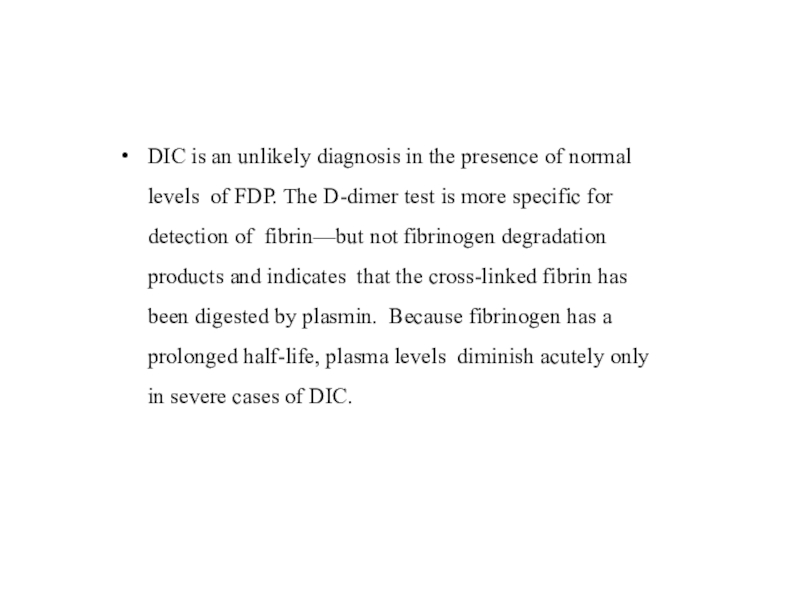
Слайд 16DIC is an unlikely diagnosis in the presence of normal
levels of FDP. The D-dimer test is more specific for
detection of fibrin—but not fibrinogen degradation products and indicates that the cross-linked fibrin has been digested by plasmin. Because fibrinogen has a prolonged half-life, plasma levels diminish acutely only in severe cases of DIC.Слайд 17RISK ASSESSMENT
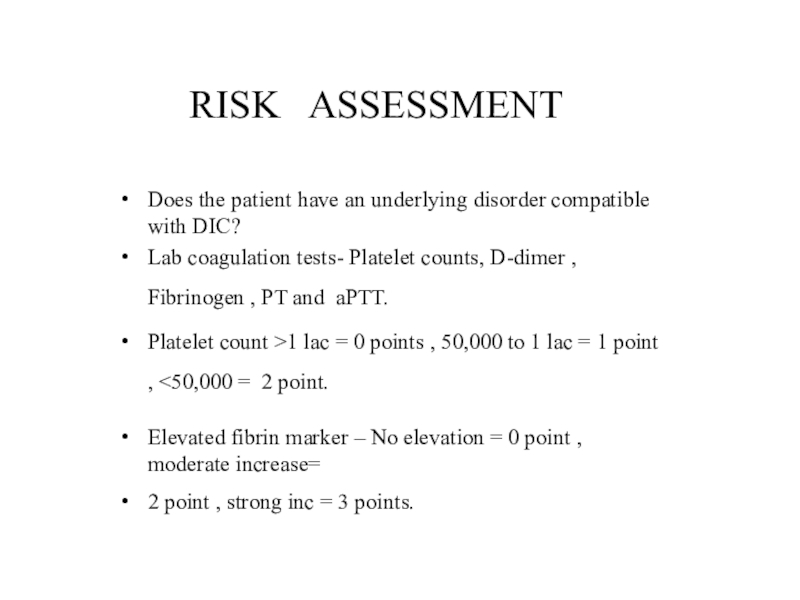
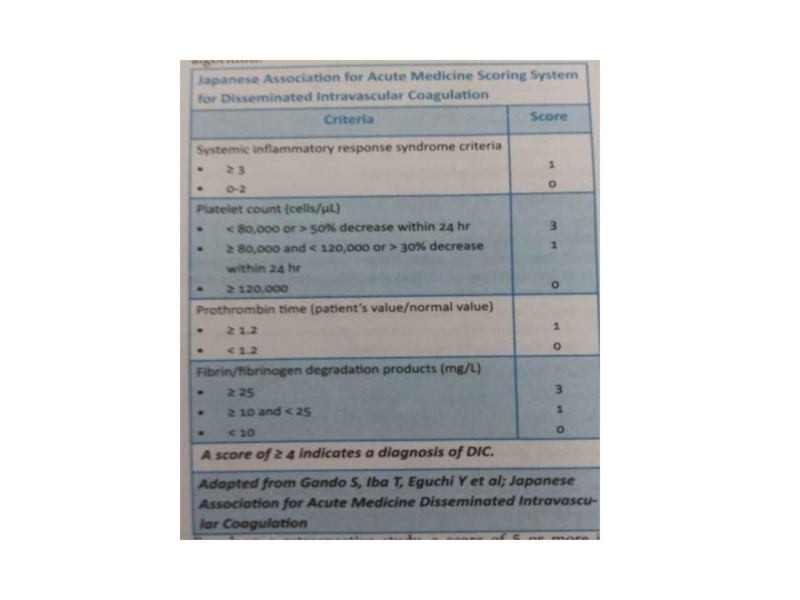
Does the patient have an underlying disorder compatible with DIC?
Lab
coagulation tests- Platelet counts, D-dimer , Fibrinogen , PT and
aPTT.Platelet count >1 lac = 0 points , 50,000 to 1 lac = 1 point , <50,000 = 2 point.
Elevated fibrin marker – No elevation = 0 point , moderate increase=
2 point , strong inc = 3 points.
Слайд 18Prolonged PT
sec = 1 point , >6 sec = 2 point.
Fibrinogen
level > 1 gm/l = 0 points , < 1 = 1 pointCalculate Score- > or = 5 compatible with overt DIC , repeat scoring daily.
Слайд 20TREATMENT
The morbidity and mortality associated with DIC are primarily related
to the underlying disease rather than the complications of the
DIC. The control or elimination of the underlying cause should therefore be the primary concern.Patients with severe DIC require control of hemodynamic parameters, respiratory support, and sometimes invasive surgical procedures.
Attempts to treat DIC without accompanying treatment of the
causative disease are likely to fail.
Слайд 21MANAGEMENT OF
HEMORRHAGIC SYMPTOMS
The control of bleeding in DIC patients with marked
thrombocytopenia (platelet counts
factors will require replacement therapy.Слайд 22The PT (>1.5 times the normal) provides a good indicator
of the
severity of the clotting factor consumption.
Replacement
with FFP is indicated (1 unit of FFP increases most coagulation factors by 3% in an adult without DIC).Low levels of fibrinogen (<100 mg/dL) or brisk hyperfibrinolysis will require infusion of cryoprecipitate (plasma fraction enriched for fibrinogen, FVIII, and vWF).
The replacement of 10 U of cryoprecipitate for every 2–3 U of FFP is sufficient to correct the hemostasis.
Слайд 23The transfusion must be adjusted according to the patient's clinical
and laboratory evolution.
Platelet concentrates at a dose of 1–2 U/10
kg body weight aresufficient for most DIC patients with severe thrombocytopenia.
Clotting factor concentrates are not recommended for control of bleeding in DIC because of the limited efficacy afforded by replacement of single factors (FVIII or FIX concentrates), and the high risk of
products containing traces of aPCCs that further aggravate the disease.
Слайд 24REPLACEM ENT O F CO AG ULATI O N O R FI BRI
NO LYSI S I NHI BI TO RS
Drugs to control coagulation
such as heparin, ATIII concentrates, or antifibrinolytic drugs have all been tried in the treatment of DIC.In acute DIC, the use of heparin is likely to aggravate bleeding. To date, the use of heparin in patients with severe DIC has no proven survival benefit.

![D I C LAB INVESTIGATIONSThe laboratory investigation should include coagulation tests [aPTT, PT, thrombin time LAB INVESTIGATIONSThe laboratory investigation should include coagulation tests [aPTT, PT, thrombin time (TT)] and markers of fibrin degradation](/img/tmb/6/568457/69ea9e5ae72e2658ac5ad5bd5fe30f3f-800x.jpg)