Слайд 1The Skeletal System
Bone Structure and Function
Слайд 2The Skeletal System: A Dynamic System
The skeleton is more than
a supporting framework
The skeletal system is composed of dynamic living
tissues
It interacts with all other organ systems
It continually rebuilds and remodels itself
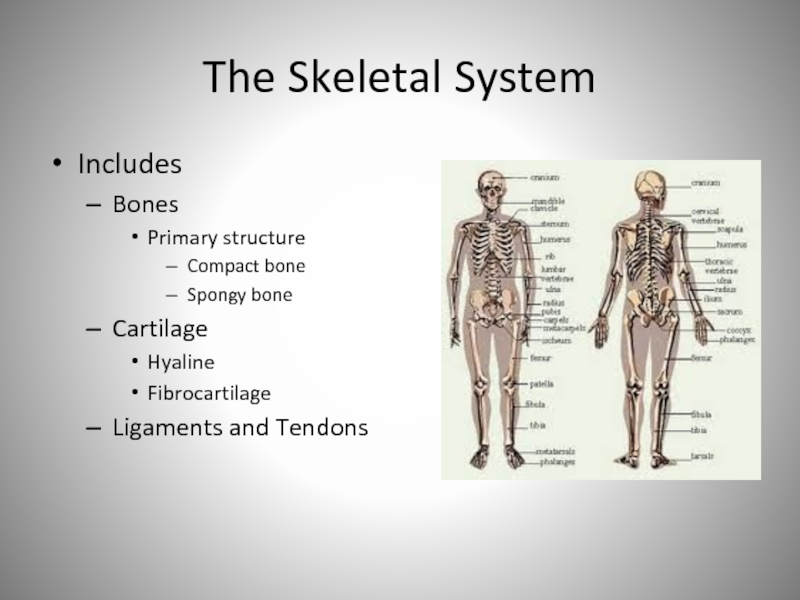
Слайд 3The Skeletal System
Includes
Bones
Primary structure
Compact bone
Spongy bone
Cartilage
Hyaline
Fibrocartilage
Ligaments and Tendons
Слайд 4Bones: Types
Compact Bone
also called dense or cortical bone
relatively dense connective
bone tissue
appears white, smooth, and solid
80% of bone mass
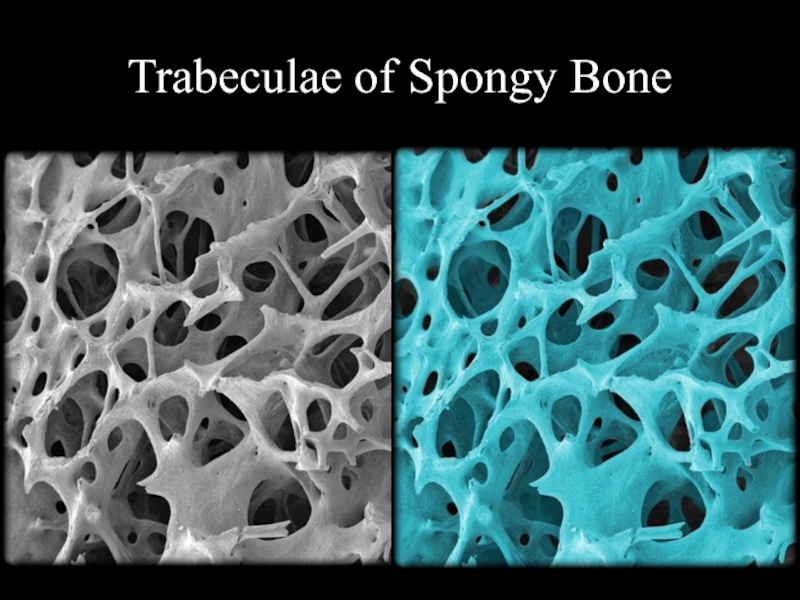
Spongy Bone
also
called cancellous or trabecular bone
located internal to compact bone
appears porous
20% of bone mass
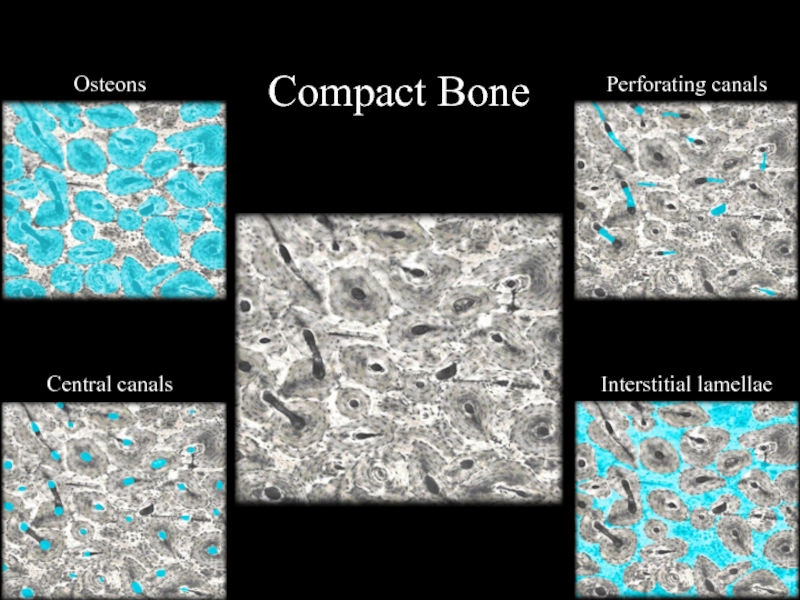
Слайд 5Compact Bone
Osteons
Central canals
Perforating canals
Interstitial lamellae
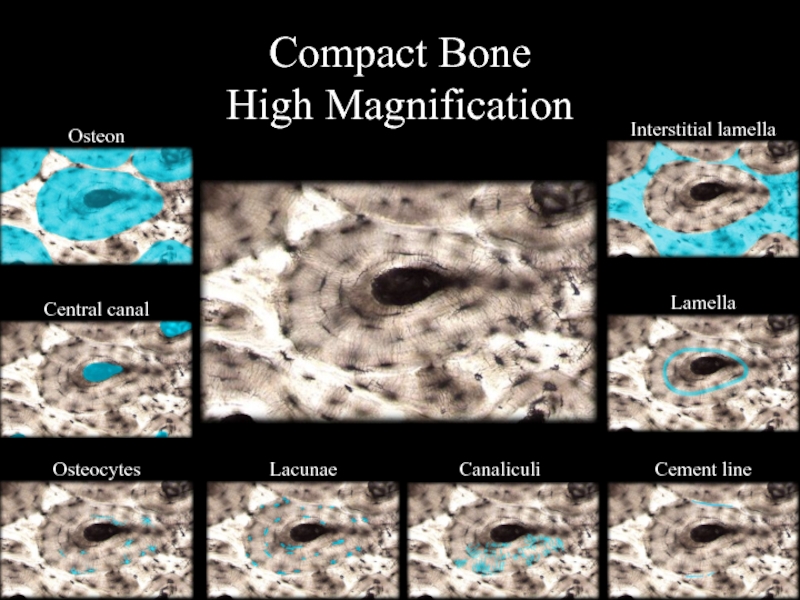
Слайд 6Compact Bone
High Magnification
Osteon
Central canal
Osteocytes
Lacunae
Interstitial lamella
Lamella
Cement line
Canaliculi
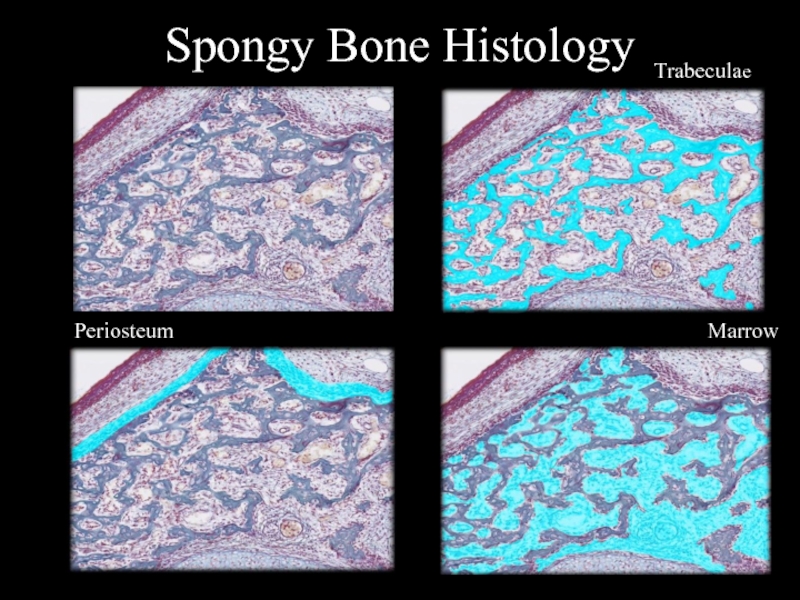
Слайд 7Spongy Bone Histology
Marrow
Trabeculae
Periosteum
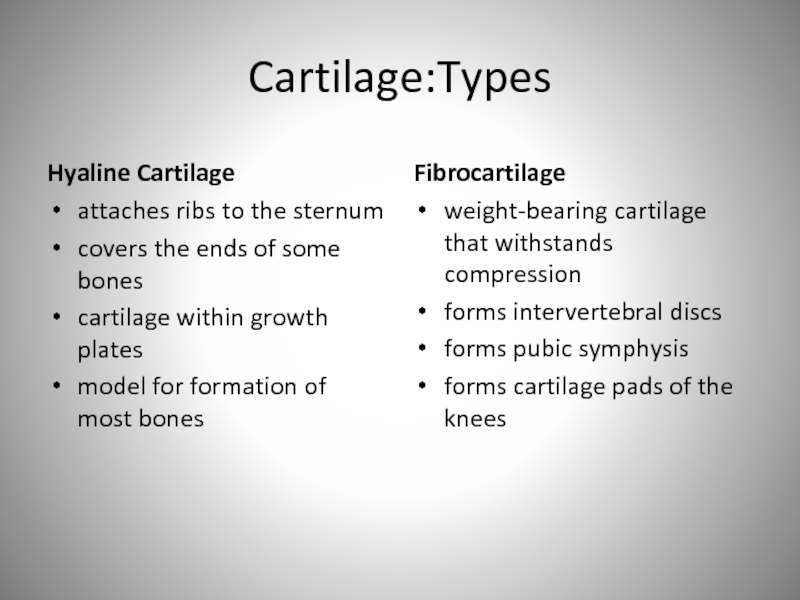
Слайд 9Cartilage:Types
Hyaline Cartilage
attaches ribs to the sternum
covers the ends of some
bones
cartilage within growth plates
model for formation of most bones
Fibrocartilage
weight-bearing cartilage
that withstands compression
forms intervertebral discs
forms pubic symphysis
forms cartilage pads of the knees
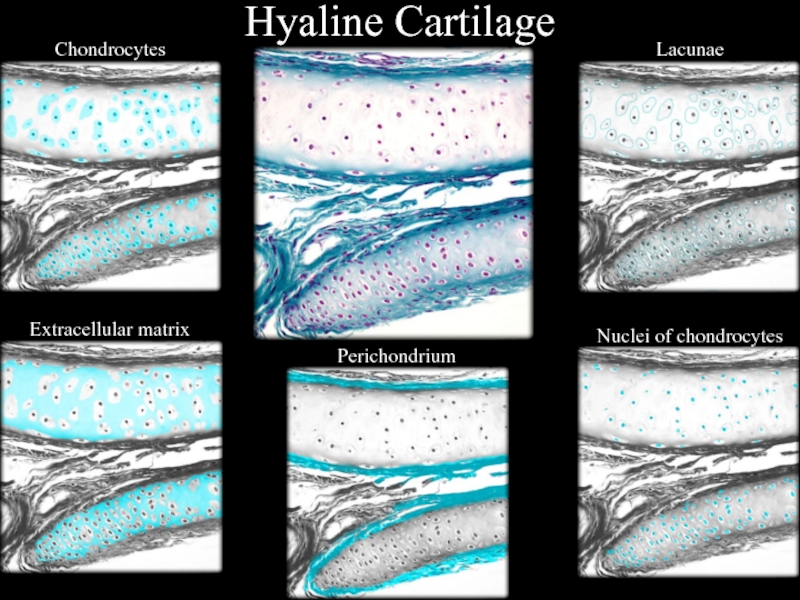
Слайд 10Hyaline Cartilage
Chondrocytes
Extracellular matrix
Perichondrium
Lacunae
Nuclei of chondrocytes
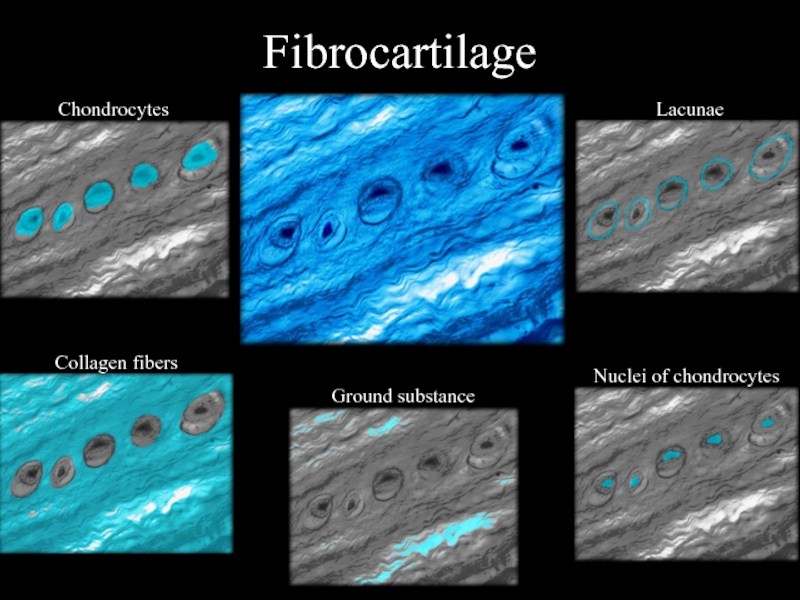
Слайд 11Fibrocartilage
Chondrocytes
Collagen fibers
Ground substance
Lacunae
Nuclei of chondrocytes
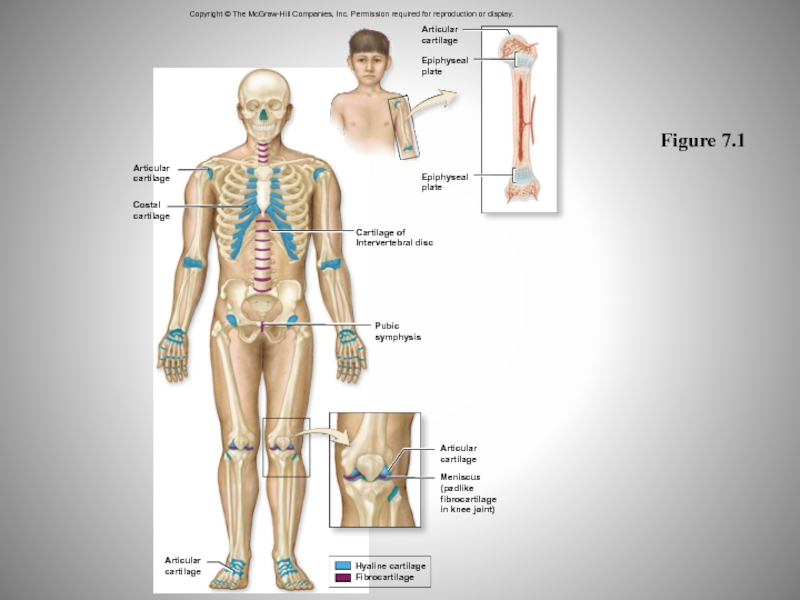
Слайд 12Figure 7.1
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
Articular
cartilage
Costal
cartilage
Articular
cartilage
Articular
cartilage
Epiphyseal
plate
Epiphyseal
plate
Cartilage of
Intervertebral disc
Pubic
symphysis
Articular
cartilage
Meniscus
(padlike
fibrocartilage
in knee joint)
Hyaline cartilage
Fibrocartilage
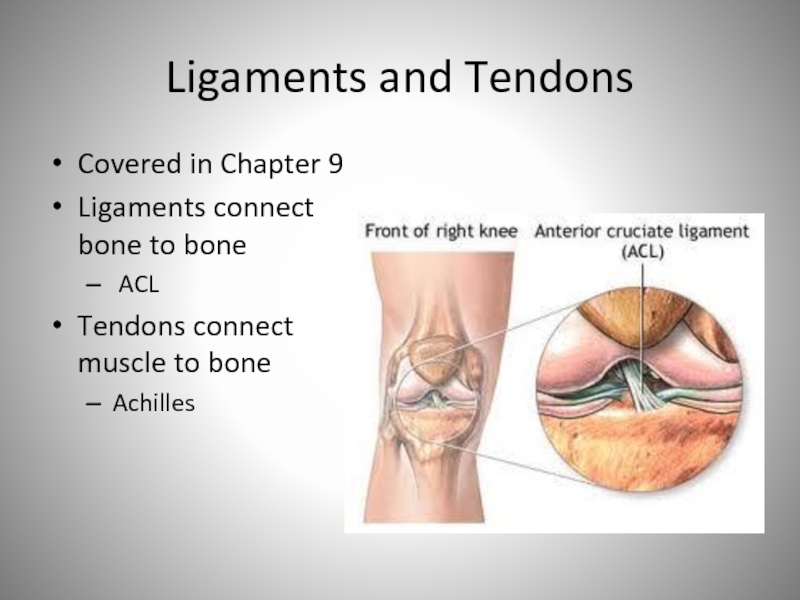
Слайд 13Ligaments and Tendons
Covered in Chapter 9
Ligaments connect bone to bone
ACL
Tendons connect muscle to bone
Achilles
Слайд 14Bones
206 bones is standard / typical (but nearly everyone has
more/fewer)
Слайд 16Bone Functions
Support and Protection
Body’s framework
Protects from trauma
Movement
Sites of muscle attachment
Hemopoiesis
Production
of red, white blood cells and platelets
Storage of Mineral and
Energy Reserves
Calcium, Phosphorous
Lipids
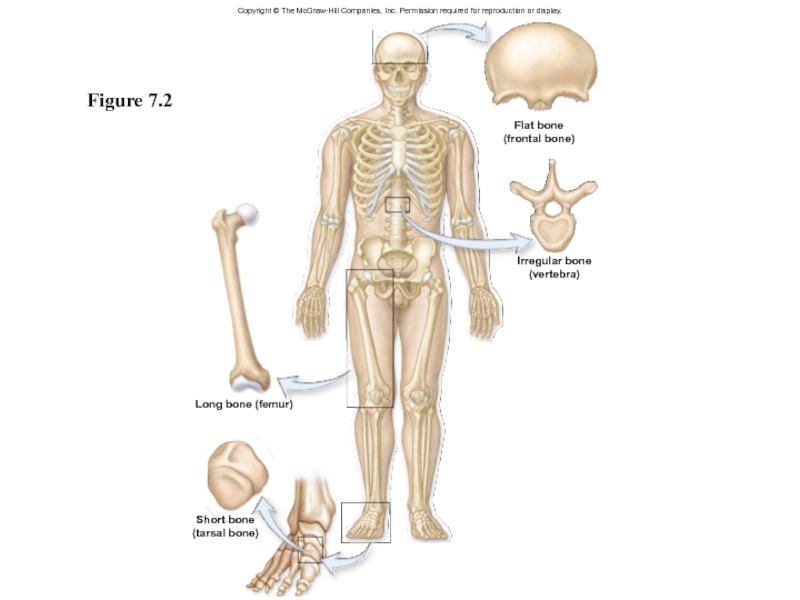
Слайд 17Bone Classification
Four classes determined by shape
Long bones
Short bones
Flat bones
Irregular bones
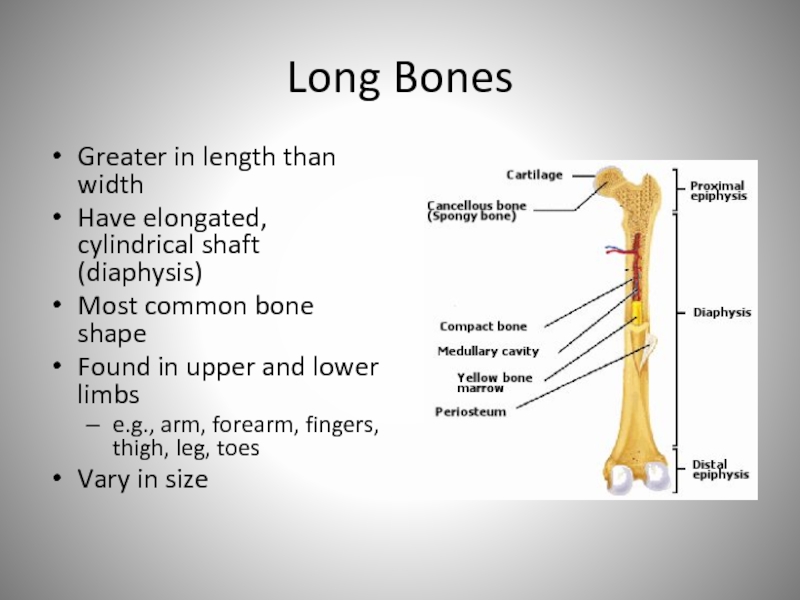
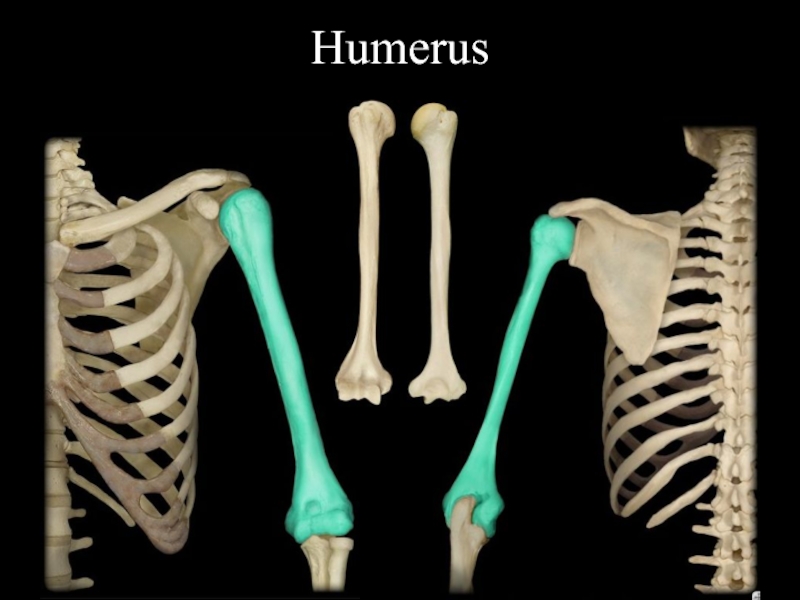
Слайд 18Long Bones
Greater in length than width
Have elongated, cylindrical shaft (diaphysis)
Most
common bone shape
Found in upper and lower limbs
e.g., arm, forearm,
fingers, thigh, leg, toes
Vary in size
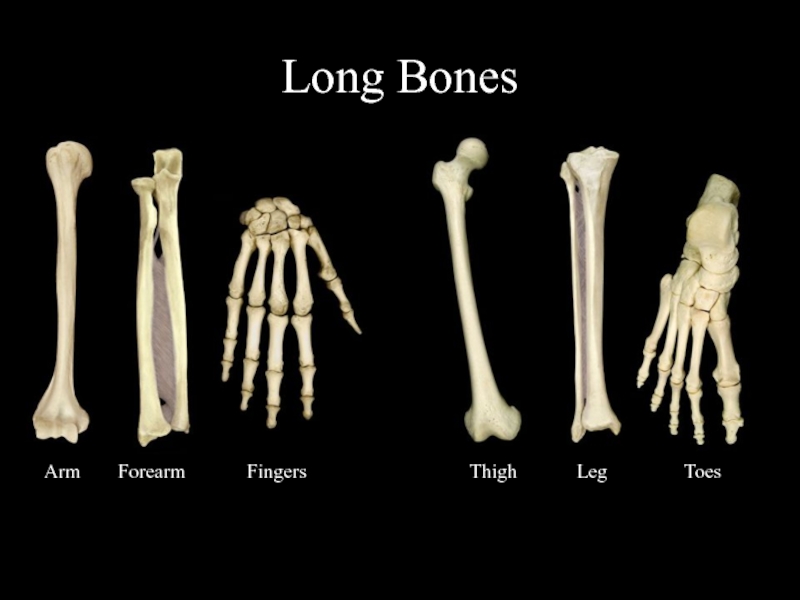
Слайд 19Long Bones
Arm
Forearm
Fingers
Thigh
Leg
Toes
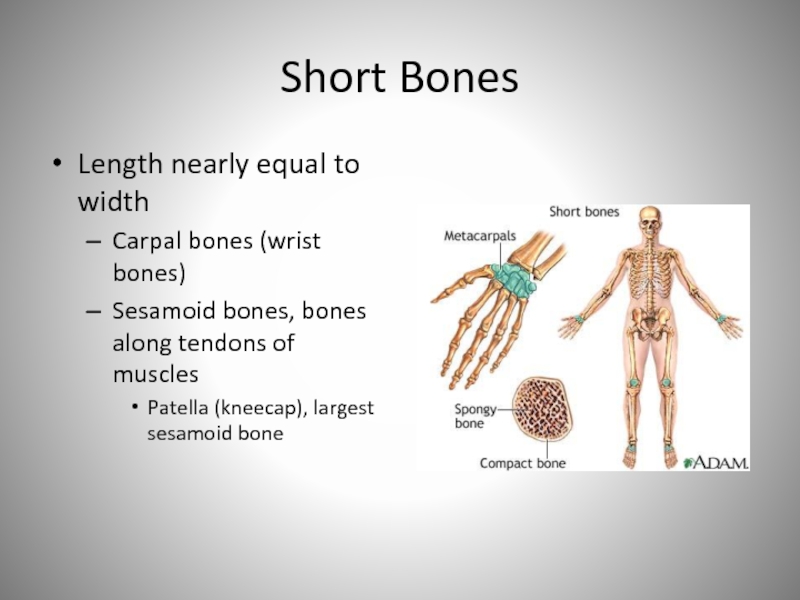
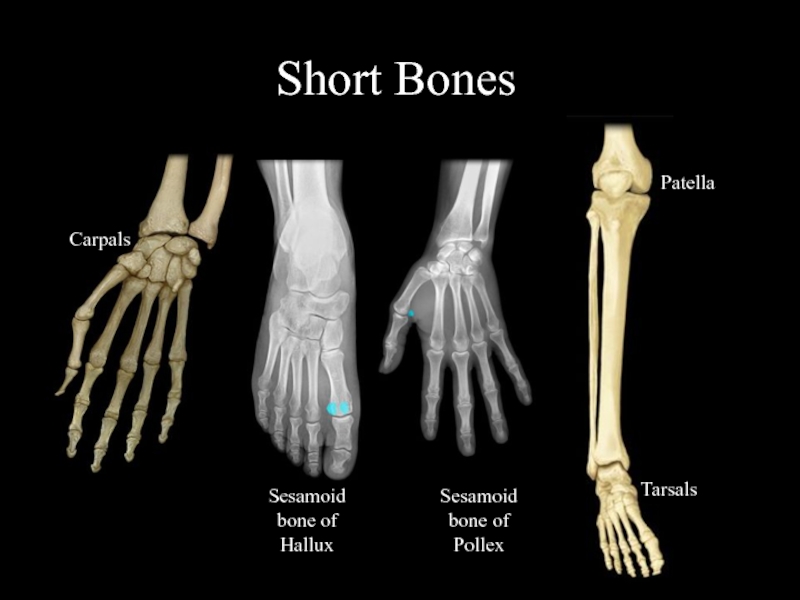
Слайд 20Short Bones
Length nearly equal to width
Carpal bones (wrist bones)
Sesamoid bones,
bones along tendons of muscles
Patella (kneecap), largest sesamoid bone
Слайд 21Short Bones
Carpals
Sesamoid bone of Hallux
Sesamoid bone of Pollex
Patella
Tarsals
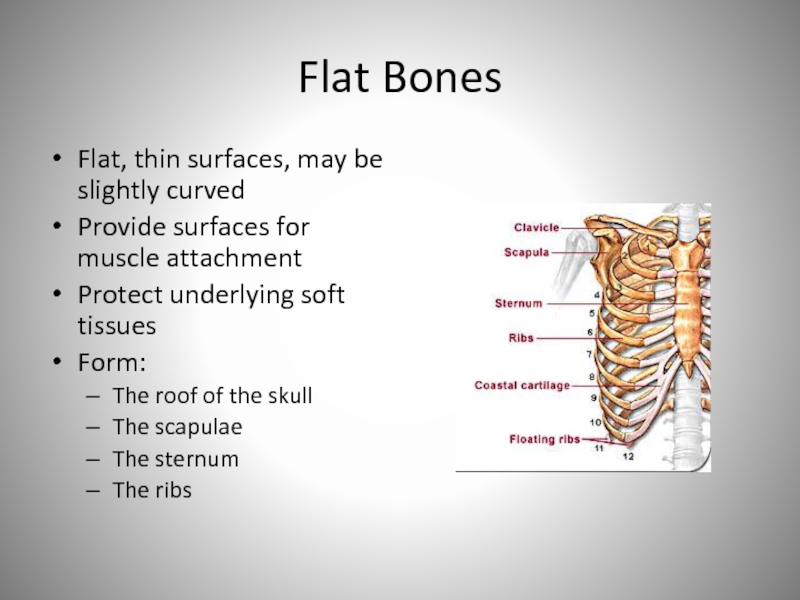
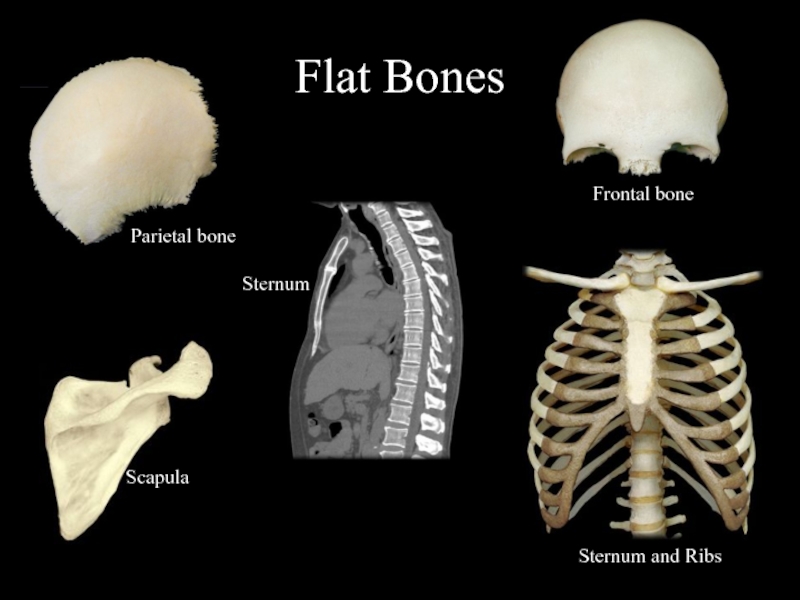
Слайд 22Flat Bones
Flat, thin surfaces, may be slightly curved
Provide surfaces for
muscle attachment
Protect underlying soft tissues
Form:
The roof of the skull
The scapulae
The sternum
The ribs
Слайд 23Flat Bones
Parietal bone
Scapula
Sternum
Sternum and Ribs
Frontal bone
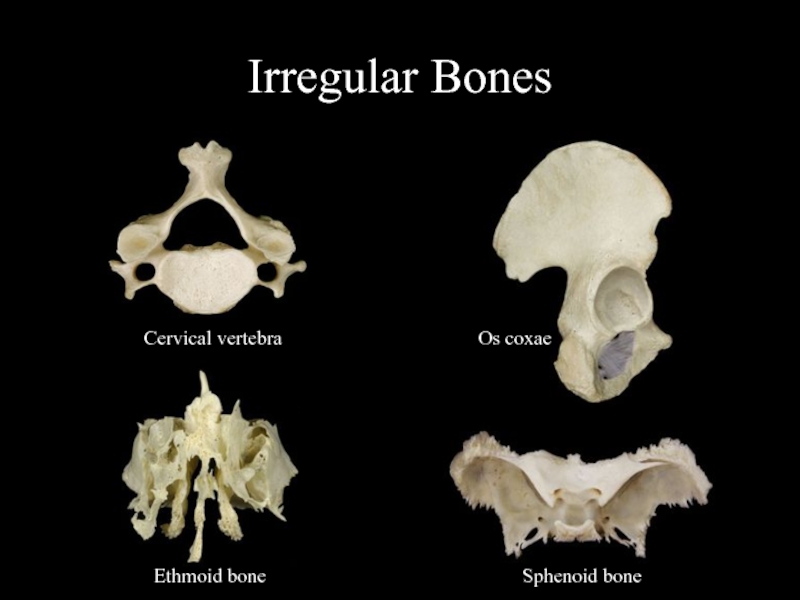
Слайд 24Irregular Bones
Have elaborate shapes
E.g., vertebrae, ossa coxae (hip bones)
E.g., several
bones in the skull (ethmoid, sphenoid
Слайд 25Irregular Bones
Cervical vertebra
Os coxae
Ethmoid bone
Sphenoid bone
Слайд 26Figure 7.2
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
Flat bone
(frontal bone)
Irregular bone
(vertebra)
Long bone (femur)
Short bone
(tarsal bone)
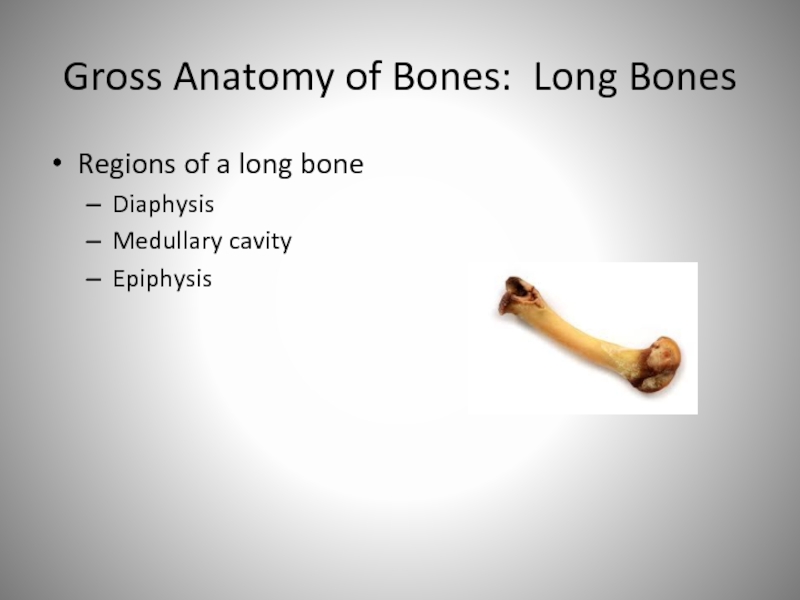
Слайд 27Gross Anatomy of Bones: Long Bones
Regions of a long bone
Diaphysis
Medullary
cavity
Epiphysis
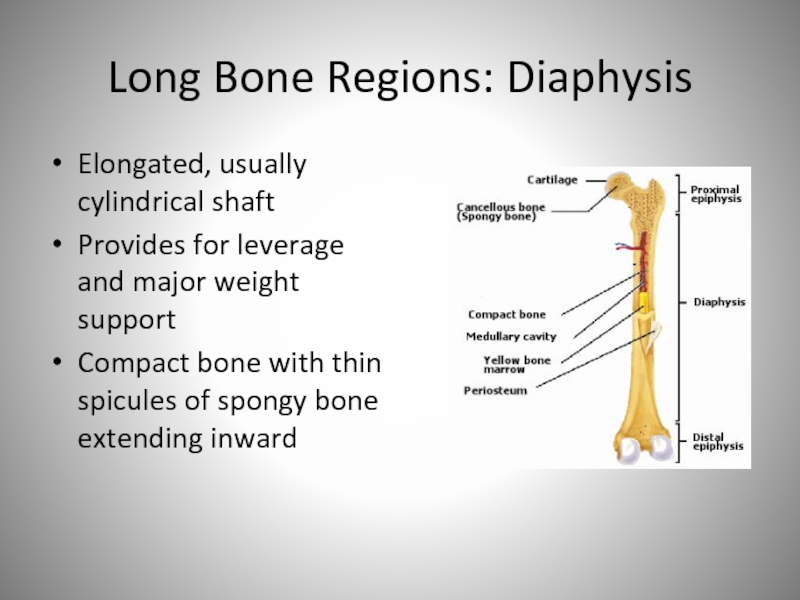
Слайд 28Long Bone Regions: Diaphysis
Elongated, usually cylindrical shaft
Provides for leverage and
major weight support
Compact bone with thin spicules of spongy bone
extending inward
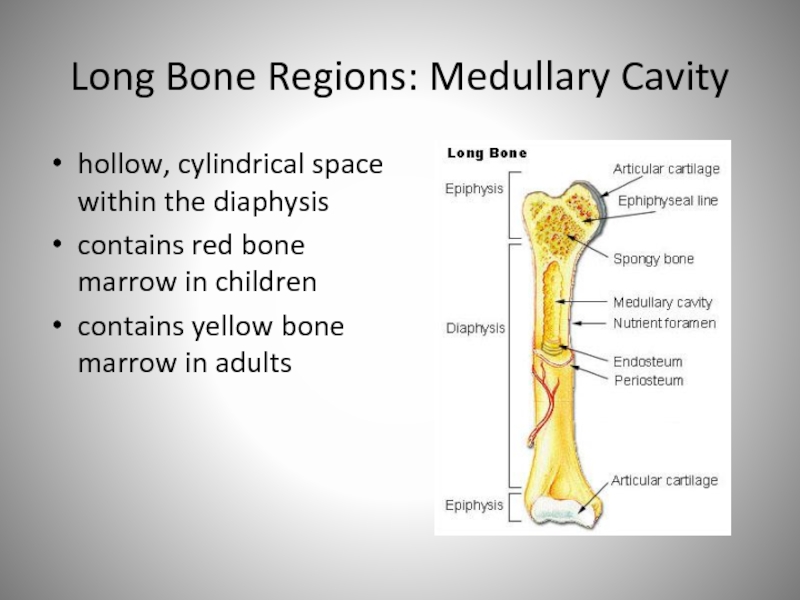
Слайд 29Long Bone Regions: Medullary Cavity
hollow, cylindrical space within the diaphysis
contains
red bone marrow in children
contains yellow bone marrow in adults
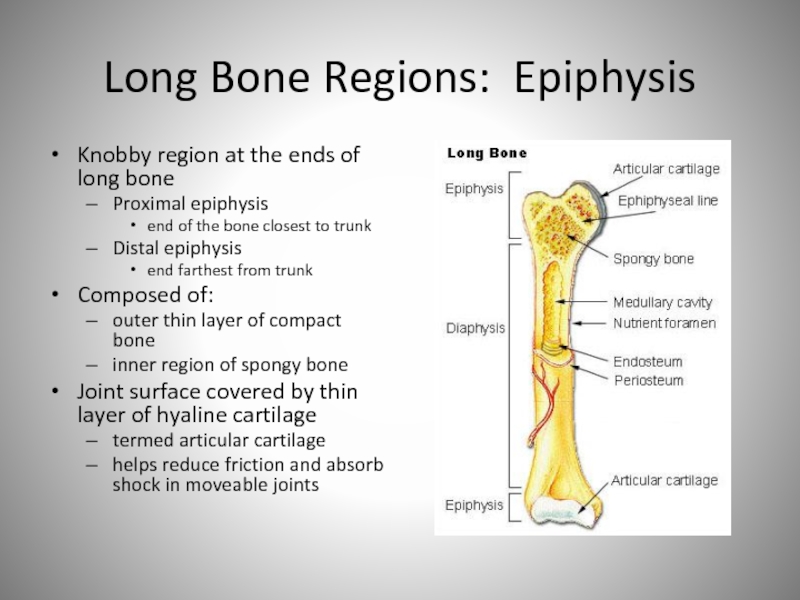
Слайд 30Long Bone Regions: Epiphysis
Knobby region at the ends of long
bone
Proximal epiphysis
end of the bone closest to trunk
Distal epiphysis
end farthest from trunk
Composed of:
outer thin layer of compact bone
inner region of spongy bone
Joint surface covered by thin layer of hyaline cartilage
termed articular cartilage
helps reduce friction and absorb shock in moveable joints
Слайд 31Long Bone Regions: Epiphysis
Metaphysis
Region of mature bone between diaphysis and
epiphysis
Epiphyseal plate
In metaphysis
Thin layer of hyaline cartilage
Provides for continued lengthwise
bone growth
Remnant in adults termed the epiphyseal line
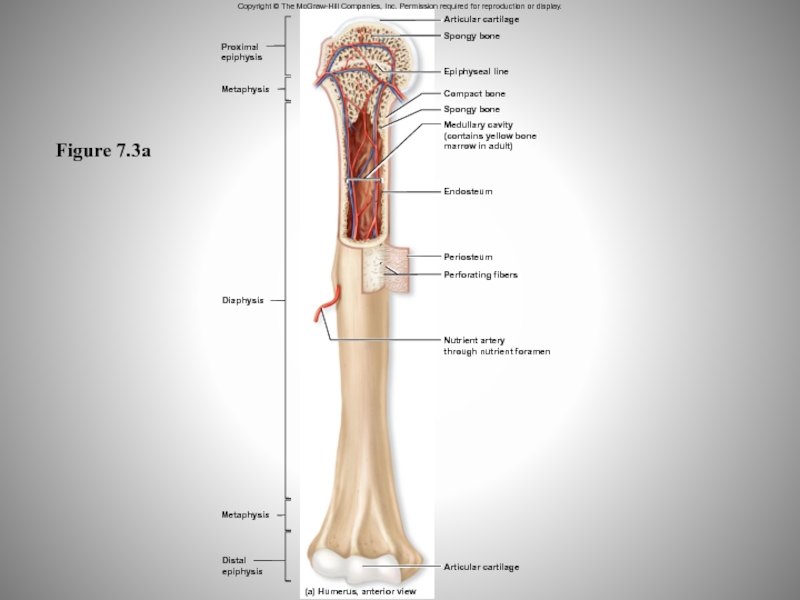
Слайд 32Figure 7.3a
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
Proximal
epiphysis
Metaphysis
Diaphysis
Metaphysis
Distal
epiphysis
(a) Humerus, anterior view
Articular cartilage
Spongy bone
Articular cartilage
Epiphyseal line
Compact
bone
Spongy bone
Medullary cavity
(contains yellow bone
marrow in adult)
Endosteum
Periosteum
Perforating fibers
Nutrient artery
through nutrient foramen
Слайд 34Bone Coverings
Periosteum
Tough sheath covering outer surface of bone
Outer fibrous layer
of dense irregular connective tissue
Protects bone from surrounding structures
Anchors blood
vessels and nerves to bone surface
Attachment site for ligaments and tendons
Inner cellular layer
Includes osteoprogenitor cells, osteoblasts, and osteoclasts
Attached to bone by numerous collagen fibers
Termed perforating fibers
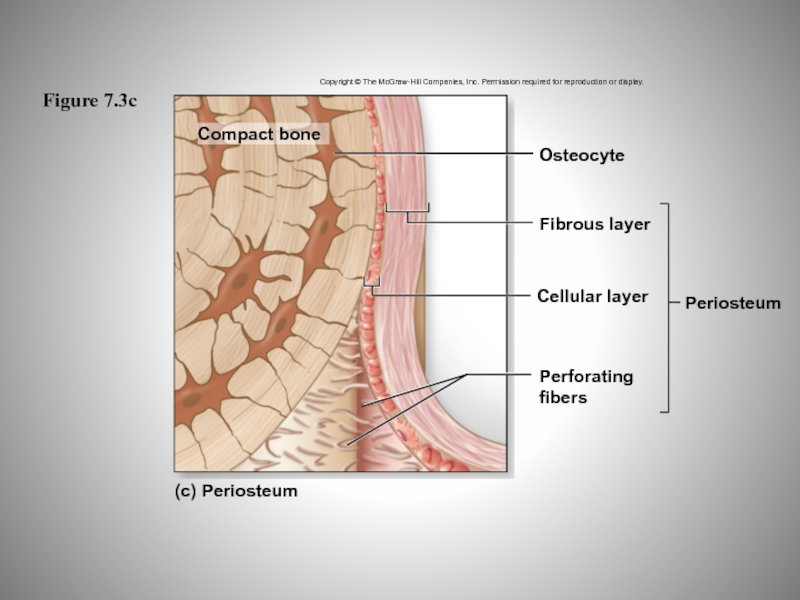
Слайд 35Figure 7.3c
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
(c) Periosteum
Perforating
fibers
Periosteum
Cellular layer
Fibrous layer
Osteocyte
Compact bone
Compact bone
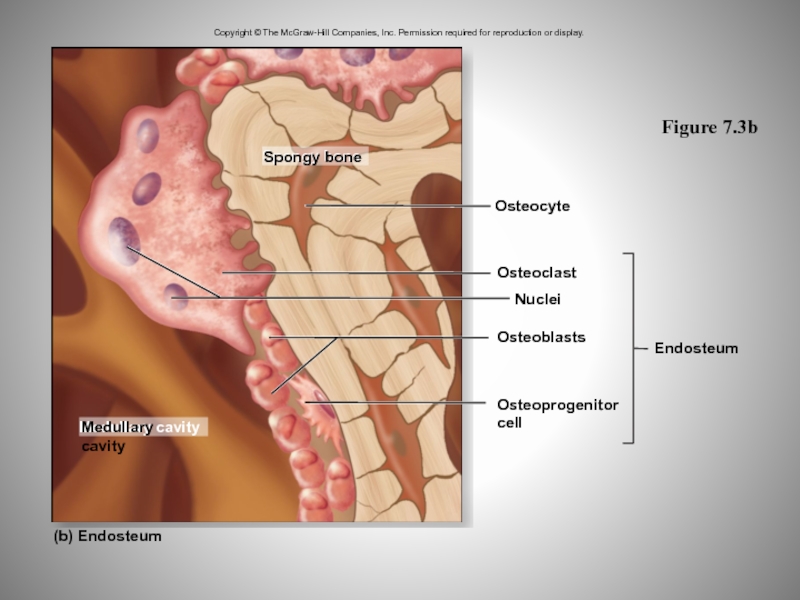
Слайд 36Bone Coverings
Endosteum
Covers all internal surfaces of bone within medullary cavity
Incomplete
layer of cells
Contains osteoprogenitor cells, osteoblasts, and osteoclasts
Слайд 37Figure 7.3b
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
Endosteum
Osteoprogenitor
cell
Osteoblasts
Nuclei
Osteoclast
Osteocyte
Spongy bone
Medullary cavity
(b) Endosteum
Spongy bone
Medullary cavity
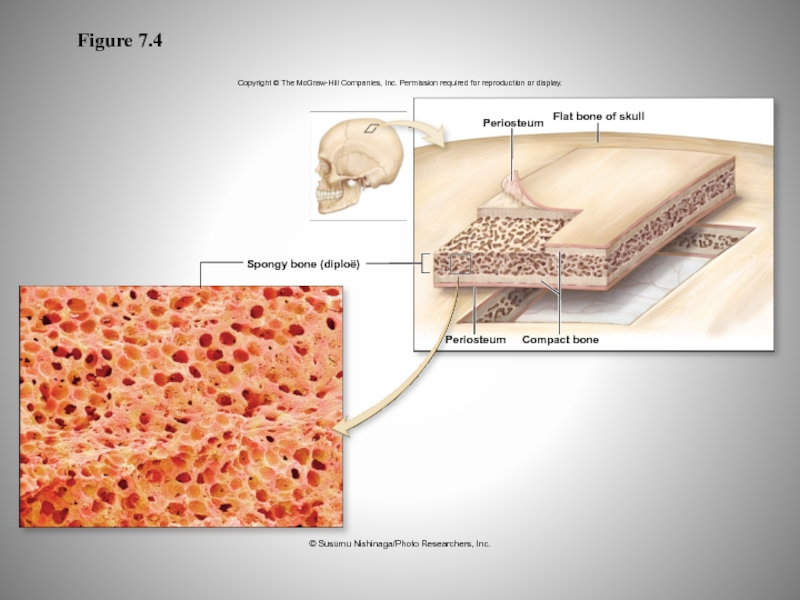
Слайд 38Gross Anatomy of Bones: Other Bones
Short, flat, and irregular bones
External
surface composed of compact bone
Interior composed of spongy bone
also called
diploë in flat skull bones
Lack a medullary cavity
Слайд 39Figure 7.4
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
SEM 5x
Flat bone of skull
Periosteum
Compact bone
Periosteum
Spongy bone (diploë)
©
Susumu Nishinaga/Photo Researchers, Inc.
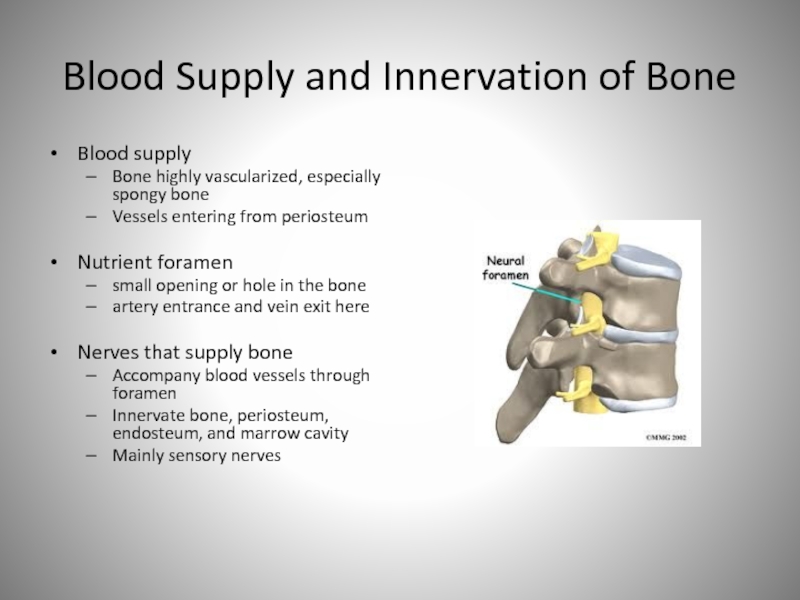
Слайд 40Blood Supply and Innervation of Bone
Blood supply
Bone highly vascularized, especially
spongy bone
Vessels entering from periosteum
Nutrient foramen
small opening or hole in
the bone
artery entrance and vein exit here
Nerves that supply bone
Accompany blood vessels through foramen
Innervate bone, periosteum, endosteum, and marrow cavity
Mainly sensory nerves
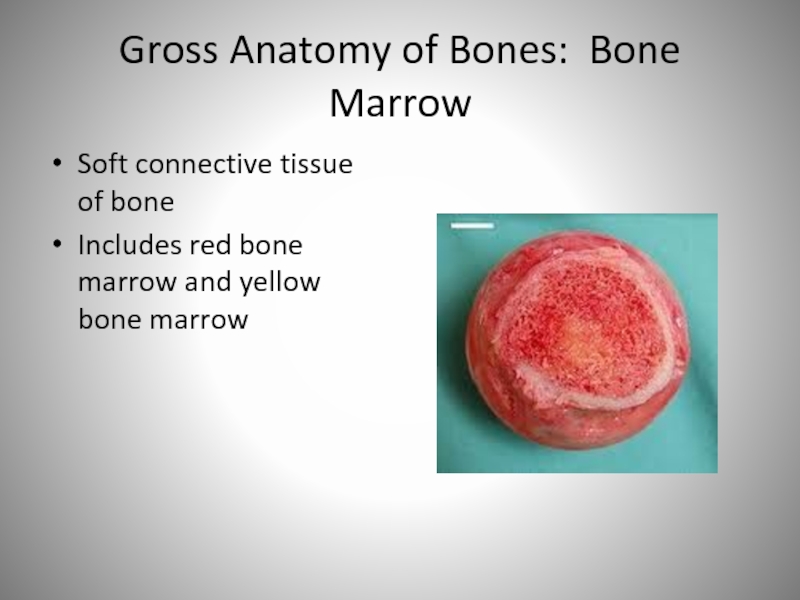
Слайд 41Gross Anatomy of Bones: Bone Marrow
Soft connective tissue of bone
Includes
red bone marrow and yellow bone marrow
Слайд 42Red Bone Marrow
Also known as myeloid tissue
Hemopoietic (blood cell forming)
Contains
reticular connective tissue, immature blood cells, and fat
In children,
located in
the spongy bone and medullary cavity of long bones
In adults,
located in portions of axial skeleton
located in proximal epiphyses of humerus and femur
skull, vertebrae, ribs, sternum, ossa coxae
Слайд 43Yellow Bone Marrow
Product of red bone marrow degeneration
Fatty substance
May
convert back to red bone marrow
may occur during severe anemia
condition with reduced erythrocytes (red blood cells)
facilitates the production of additional erythrocytes
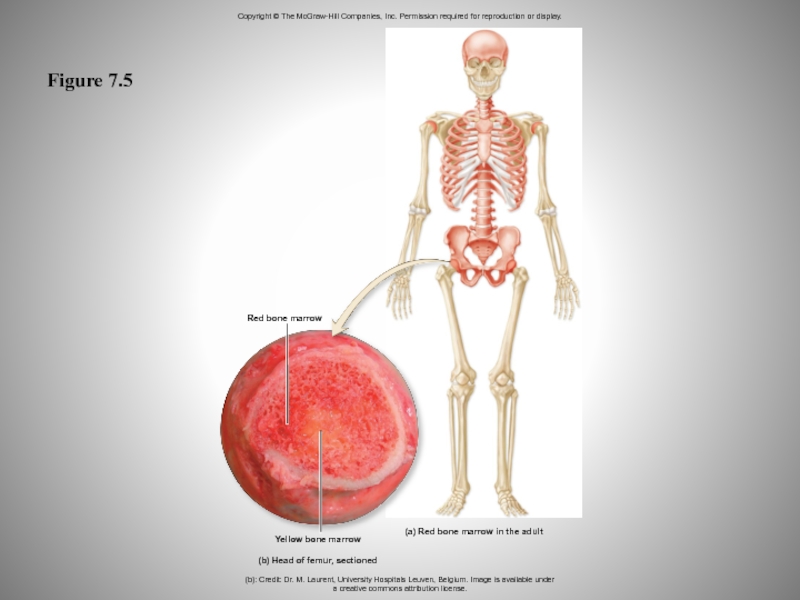
Слайд 44Figure 7.5
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
Red bone marrow
Yellow bone marrow
(b) Head of femur,
sectioned
(a) Red bone marrow in the adult
(b): Credit: Dr. M. Laurent, University Hospitals Leuven, Belgium. Image is available under
a creative commons attribution license.
Слайд 45Microscopic Anatomy of Bone: Cells of Bone
Bone connective tissue
Primary component
of bone
Also called osseous connective tissue
Composed of cells and extracellular
matrix
Four types found in bone connective tissue
Osteoprogenitor cells
Osteoblasts
Osteocytes
Osteoclasts
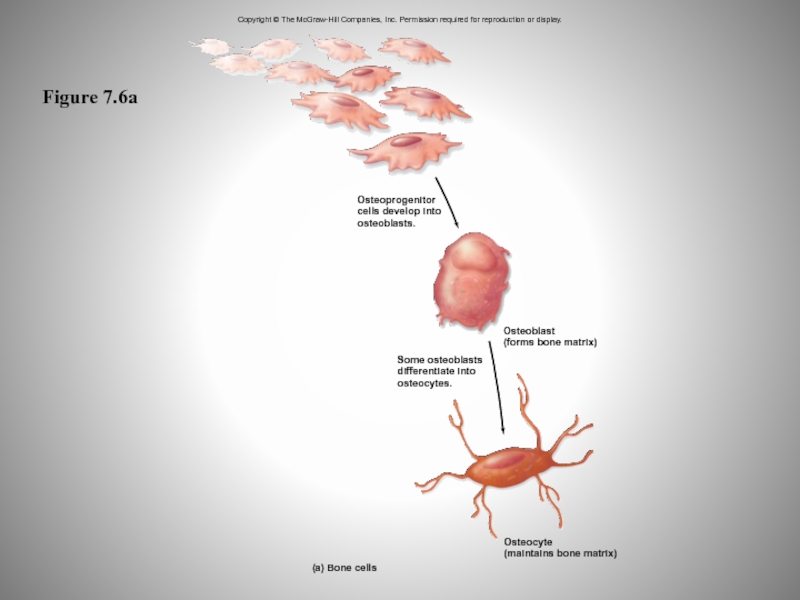
Слайд 46Osteoprogenitor Cells
Stem cells derived from mesenchyme
Produce cells that mature to
become osteoblasts
Located in periosteum and endosteum
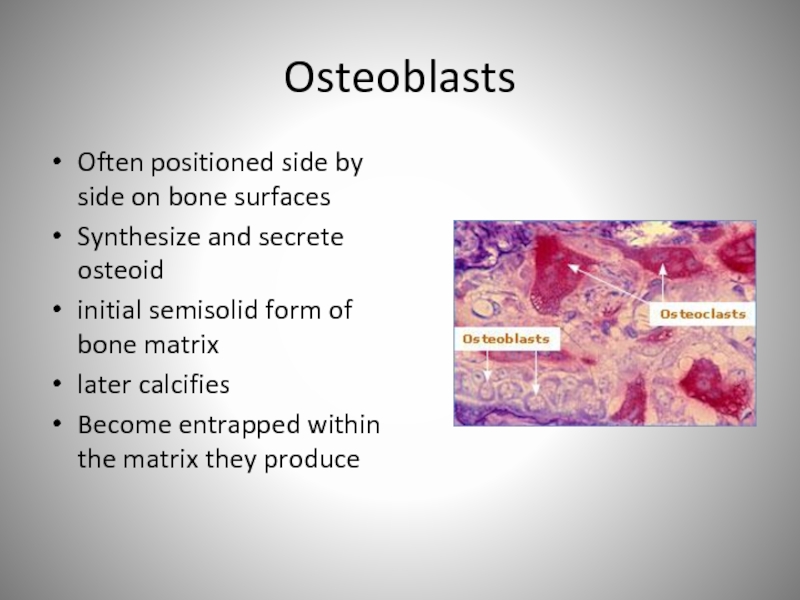
Слайд 47Osteoblasts
Often positioned side by side on bone surfaces
Synthesize and secrete
osteoid
initial semisolid form of bone matrix
later calcifies
Become entrapped within
the matrix they produce
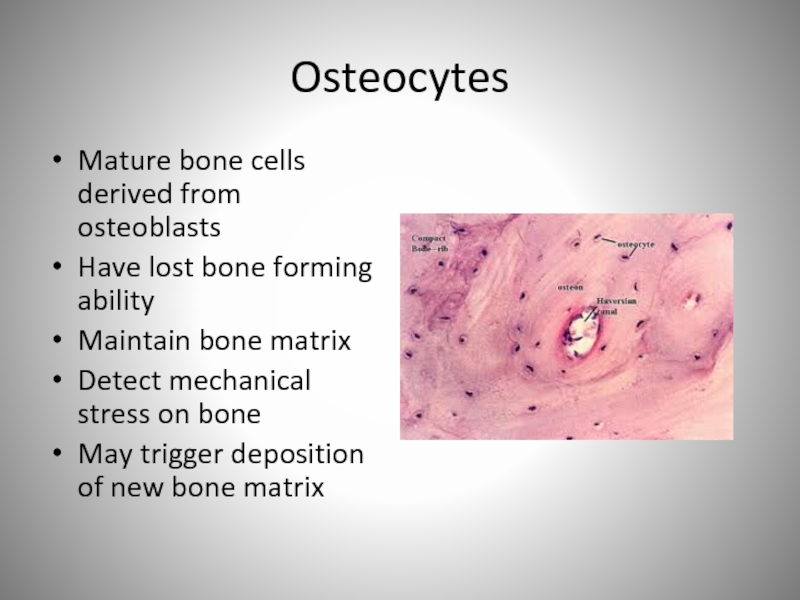
Слайд 48Osteocytes
Mature bone cells derived from osteoblasts
Have lost bone forming ability
Maintain
bone matrix
Detect mechanical stress on bone
May trigger deposition of
new bone matrix
Слайд 49Figure 7.6a
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
Osteoprogenitor
cells develop into
osteoblasts.
Some osteoblasts
differentiate into
osteocytes.
(a) Bone cells
Osteocyte
(maintains bone
matrix)
Osteoblast
(forms bone matrix)
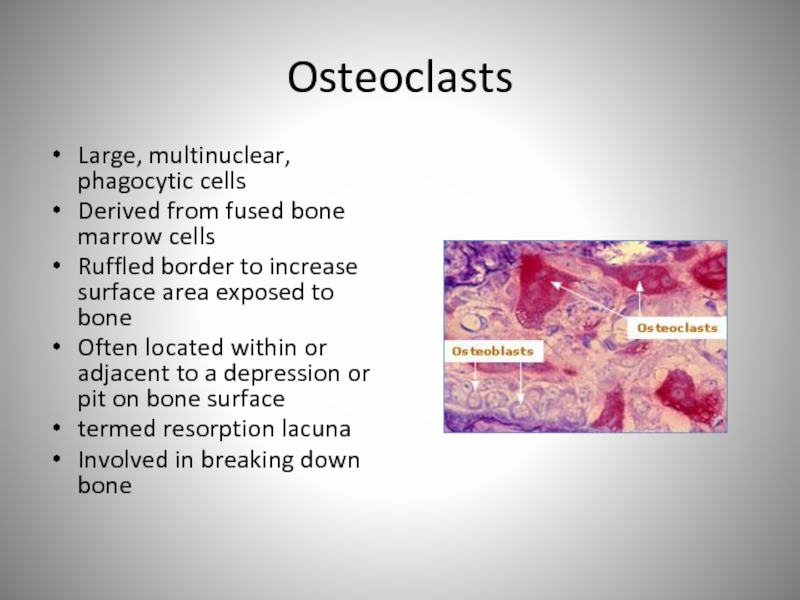
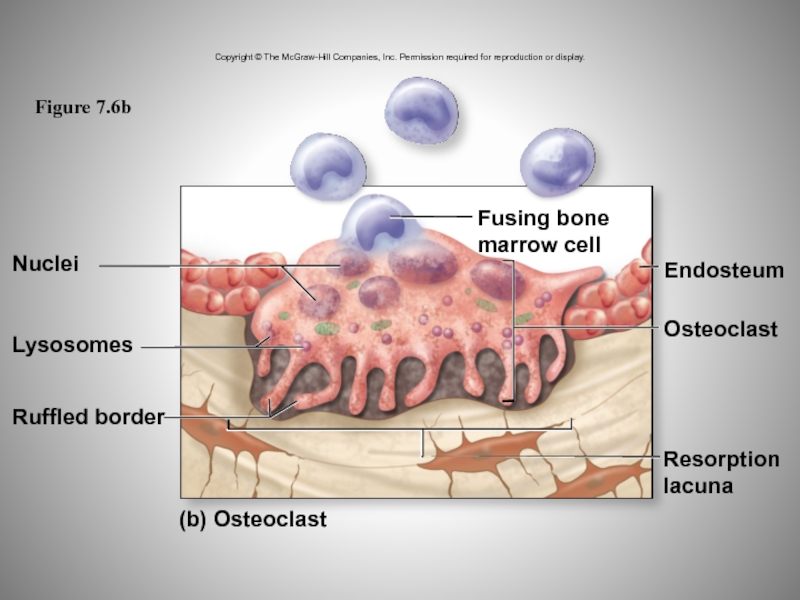
Слайд 50Osteoclasts
Large, multinuclear, phagocytic cells
Derived from fused bone marrow cells
Ruffled border
to increase surface area exposed to bone
Often located within or
adjacent to a depression or pit on bone surface
termed resorption lacuna
Involved in breaking down bone
Слайд 51Figure 7.6b
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
Resorption
lacuna
Endosteum
Osteoclast
Nuclei
Lysosomes
Ruffled border
(b) Osteoclast
Fusing bone
marrow cell
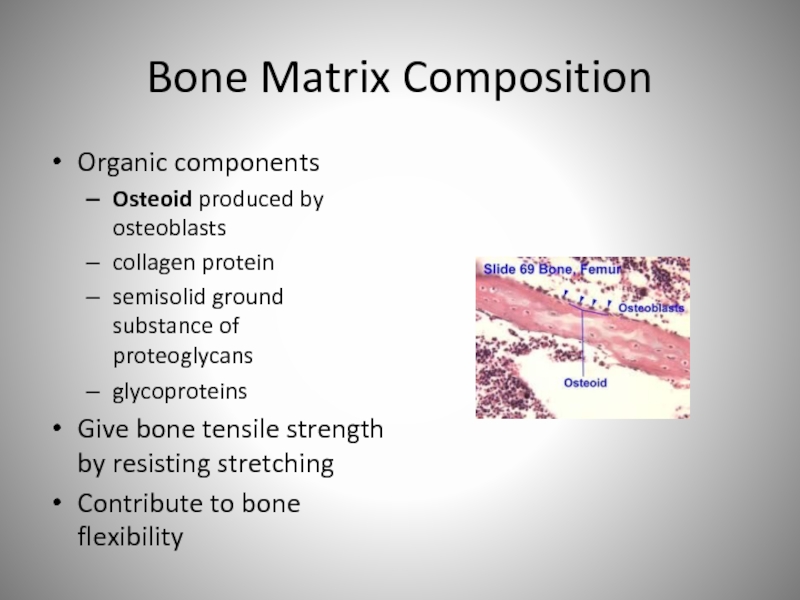
Слайд 52Bone Matrix Composition
Organic components
Osteoid produced by osteoblasts
collagen protein
semisolid ground
substance of proteoglycans
glycoproteins
Give bone tensile strength by resisting stretching
Contribute
to bone flexibility
Слайд 53Bone Matrix Composition
Inorganic components
Made of salt crystals, primarily calcium phosphate,
Ca3(PO4)2
Interacts with calcium hydroxide
forms crystals of hydroxyapatite, Ca10(PO4)6(OH)2
Other substances
incorporated into crystals
e.g., calcium carbonate, sodium, magnesium ions
Crystals deposited around collagen fibers
Harden the matrix and account for relative rigidity of bones
Слайд 54Changes to Molecular Composition of Bone
Correct proportion allows optimal functioning
Loss of protein resulting in brittle bones
Insufficient calcium resulting in
soft bones
Слайд 55Bone Matrix Formation
Begins with secretion of osteoid
Proceeds with calcification, when
hydroxyapatite crystals deposited
calcium and phosphate ions precipitating out, forming crystals
Process
requires vitamin D
enhances calcium absorption from gastrointestinal tract
Requires vitamin C
needed for collagen formation
Requires calcium and phosphate for calcification
Слайд 56Bone Matrix Resorption
Bone matrix destroyed by substances released from osteoclasts
Proteolytic
enzymes released from lysosomes within osteoclasts
chemically digest organic matrix components
Calcium
and phosphate dissolved by hydrochloric acid
May occur when blood calcium levels low
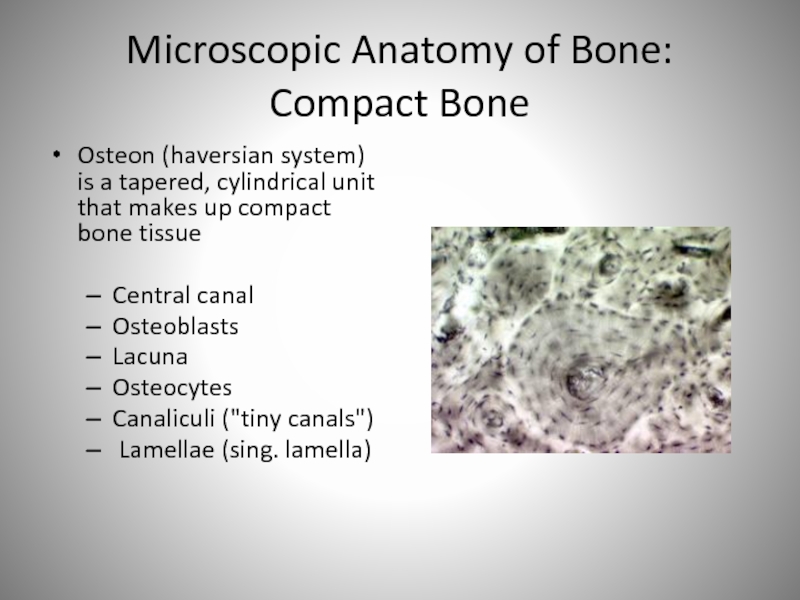
Слайд 57Microscopic Anatomy of Bone: Compact Bone
Osteon (haversian system) is a
tapered, cylindrical unit that makes up compact bone tissue
Central
canal
Osteoblasts
Lacuna
Osteocytes
Canaliculi ("tiny canals")
Lamellae (sing. lamella)
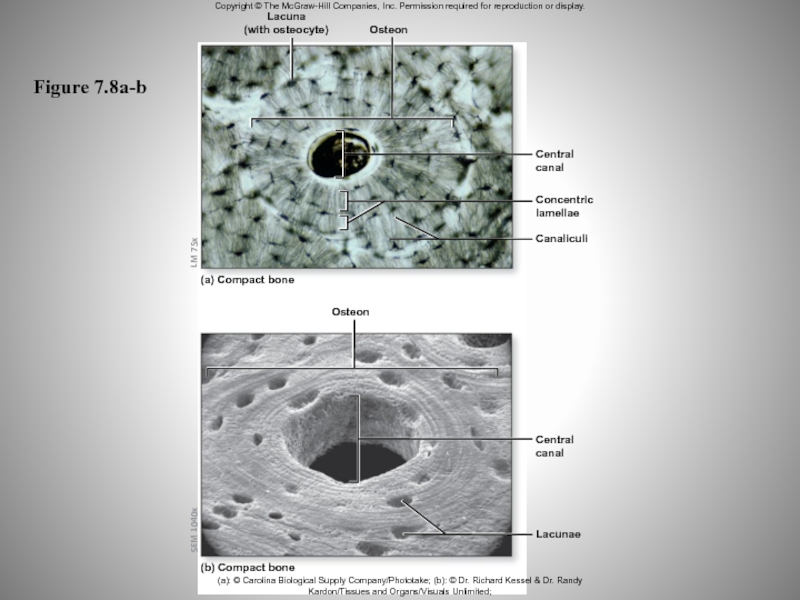
Слайд 58Figure 7.8a-b
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
SEM 1040x
LM 75x
Lacuna
(with osteocyte)
Osteon
Central
canal
Concentric
lamellae
Canaliculi
(a) Compact bone
Osteon
Central
canal
Lacunae
(b) Compact bone
(a):
© Carolina Biological Supply Company/Phototake; (b): © Dr. Richard Kessel & Dr. Randy Kardon/Tissues and Organs/Visuals Unlimited;
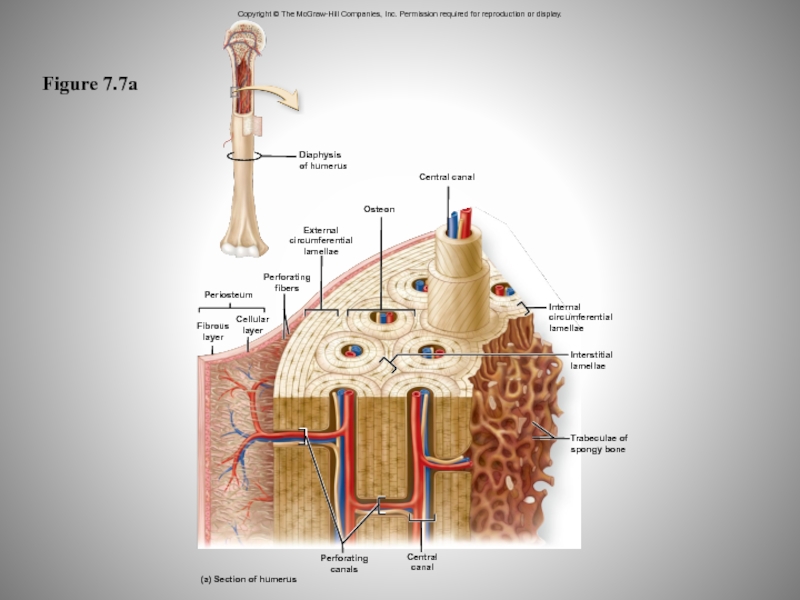
Слайд 59Figure 7.7a
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
(a) Section of humerus
Perforating
canals
Central
canal
Trabeculae of
spongy bone
Interstitial
lamellae
Internal
circumferential
lamellae
Diaphysis
of humerus
External
circumferential
lamellae
Osteon
Central canal
Perforating
fibers
Fibrous
layer
Cellular
layer
Periosteum
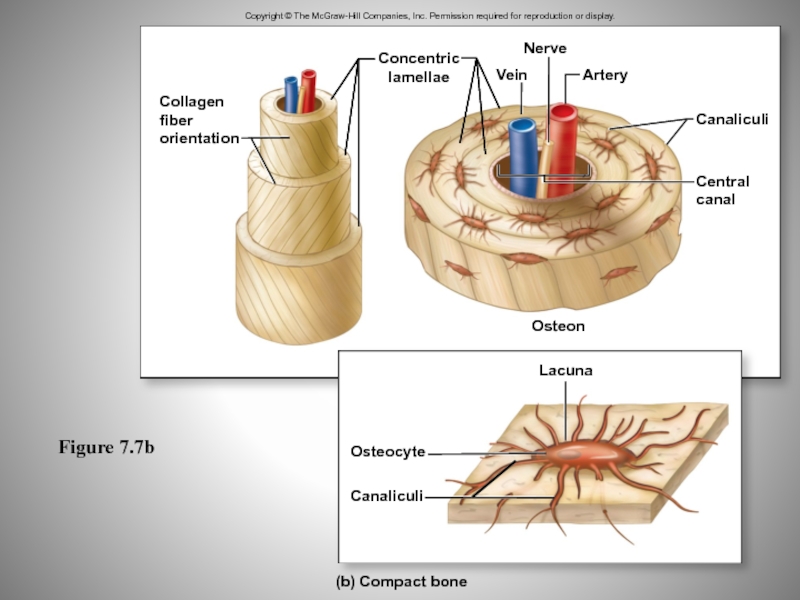
Слайд 60Figure 7.7b
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
Canaliculi
Central
canal
Osteon
Collagen
fiber
orientation
Concentric
lamellae
Nerve
Vein
Artery
Lacuna
(b) Compact bone
Osteocyte
Canaliculi
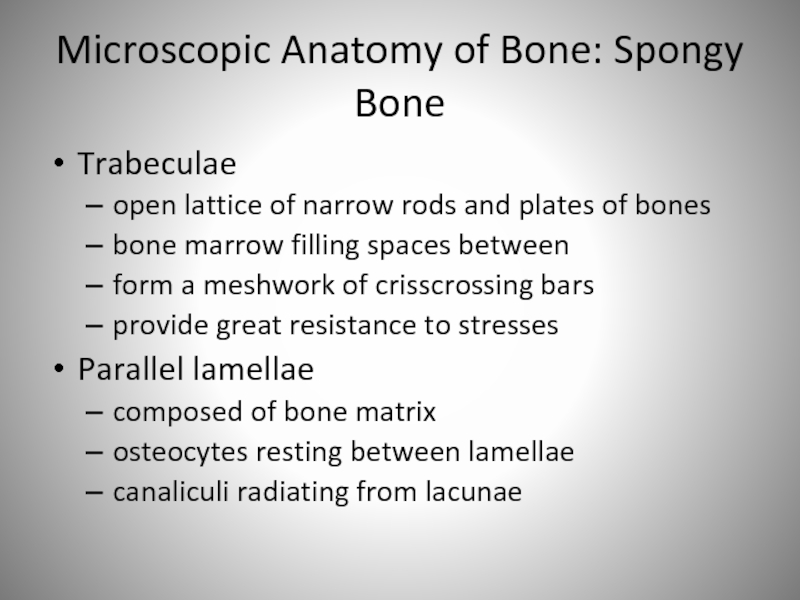
Слайд 61Microscopic Anatomy of Bone: Spongy Bone
Trabeculae
open lattice of narrow rods
and plates of bones
bone marrow filling spaces between
form a meshwork
of crisscrossing bars
provide great resistance to stresses
Parallel lamellae
composed of bone matrix
osteocytes resting between lamellae
canaliculi radiating from lacunae
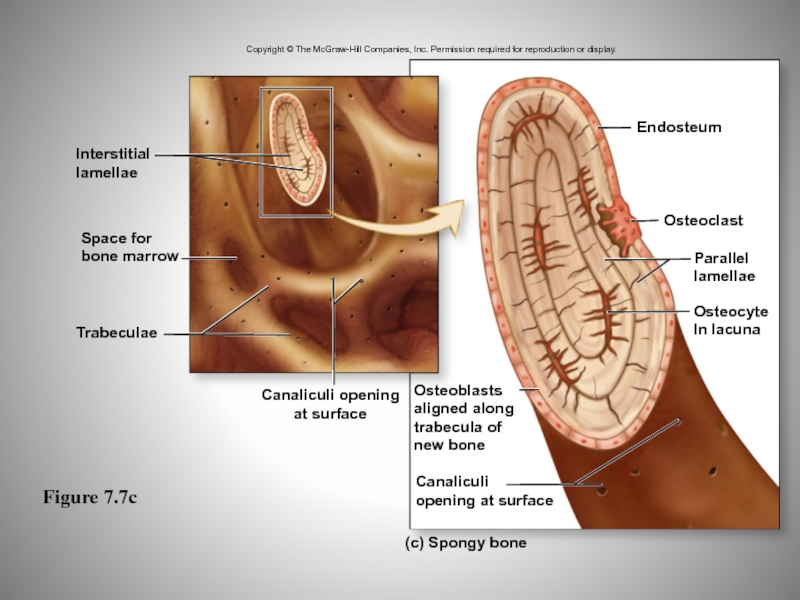
Слайд 62Figure 7.7c
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
Endosteum
Osteoclast
Parallel
lamellae
Osteocyte
In lacuna
(c) Spongy bone
Canaliculi
opening at surface
Canaliculi opening
at surface
Osteoblasts
aligned
along
trabecula of
new bone
Trabeculae
Space for
bone marrow
Interstitial
lamellae
Слайд 63Microscopic Anatomy: Hyaline Cartilage
Population of cells scattered through matrix of
protein fibers
Embedded in a gel-like ground substance
includes proteoglycans but not
calcium
Resilient and flexible
High percentage of water
Highly compressible and a good shock absorber
Avascular and contains no nerves
Слайд 64Microscopic Anatomy: Hyaline Cartilage
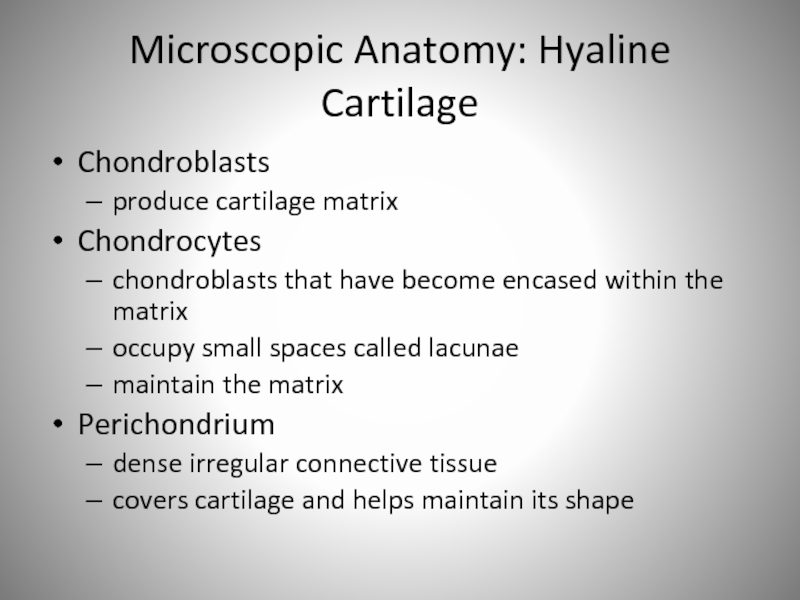
Chondroblasts
produce cartilage matrix
Chondrocytes
chondroblasts that have become encased
within the matrix
occupy small spaces called lacunae
maintain the matrix
Perichondrium
dense irregular
connective tissue
covers cartilage and helps maintain its shape
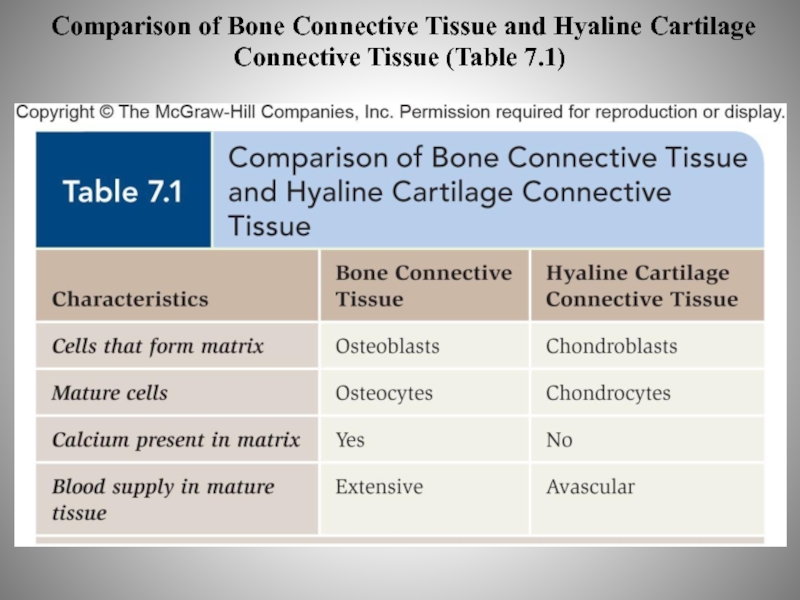
Слайд 65Comparison of Bone Connective Tissue and Hyaline Cartilage Connective Tissue
(Table 7.1)
Слайд 66Cartilage Growth
Process begins during embryologic development
Growth in length through interstitial
growth
occurs within the internal regions of cartilage
Growth in width by
appositional growth
occurs on cartilage’s outside edge
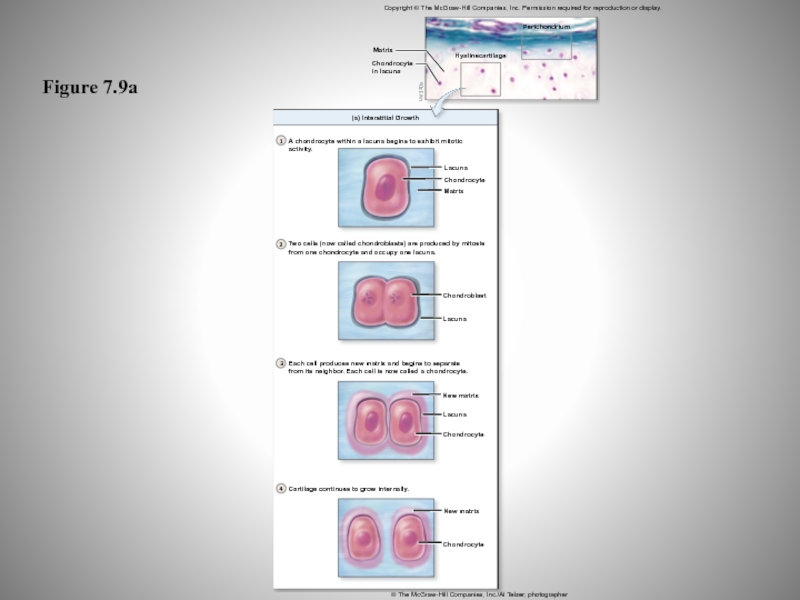
Слайд 67Figure 7.9a
1
2
3
4
Perichondrium
Hyalinecartilage
(a) Interstitial Growth
A chondrocyte within a lacuna begins to
exhibit mitotic activity.
Lacuna
Chondrocyte
Matrix
Two cells (now called chondroblasts) are produced by
mitosis
from one chondrocyte and occupy one lacuna.
Chondroblast
Lacuna
Each cell produces new matrix and begins to separate
from its neighbor. Each cell is now called a chondrocyte.
Cartilage continues to grow internally.
Chondrocyte
New matrix
Chondrocyte
Lacuna
New matrix
LM 320x
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
© The McGraw-Hill Companies, Inc./Al Telser, photographer
Matrix
Chondrocyte
in lacuna
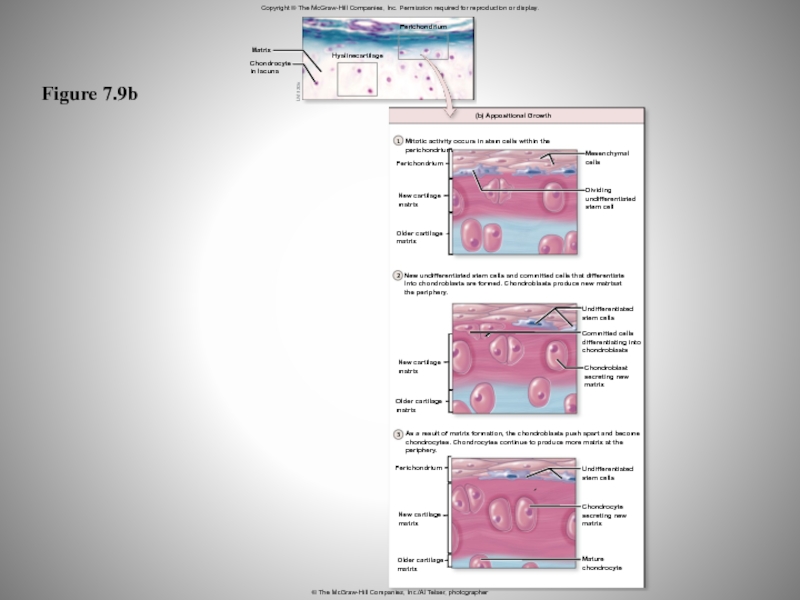
Слайд 68Figure 7.9b
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
1
2
3
LM 320x
Perichondrium
Matrix
Chondrocyte
in lacuna
Hyalinecartilage
(b) Appositional Growth
Mitotic activity occurs in
stem cells within the perichondrium.
Mesenchymal
cells
Dividing
undifferentiated
stem cell
New undifferentiated stem cells and committed cells that differentiate
Into chondroblasts are formed. Chondroblasts produce new matrixat
the periphery.
Undifferentiated
stem cells
Committed cells
differentiating into
chondroblasts
Chondroblast
secreting new
matrix
As a result of matrix formation, the chondroblasts push apart and become
chondrocytes. Chondrocytes continue to produce more matrix at the
periphery.
Undifferentiated
stem cells
Chondrocyte
secreting new
matrix
Mature
chondrocyte
Older cartilage
matrix
New cartilage
matrix
Perichondrium
Perichondrium
New cartilage
matrix
Older cartilage
matrix
New cartilage
matrix
Older cartilage
matrix
© The McGraw-Hill Companies, Inc./Al Telser, photographer
Слайд 69Cartilage Growth Stages
During early embryonic development
interstitial and appositional growth occur
simultaneously
As cartilage matures
interstitial growth declines rapidly
cartilage is semi-rigid
further growth primarily
apositional
After cartilage is fully mature
new cartilage growth stops
growth occurs only after injury
limited due to lack of blood vessels
Слайд 70Bone Formation
Process is called ossification
Begins in embryo 8-12 weeks
Always starts
with membrane or cartilage that turns to bone
Intermembranous ossification
Endochondral ossification
Слайд 71Intermembranous Ossification
Also known as dermal ossification
Produces:
flat bones of the skull
some
of the facial bones
mandible
central part of the clavicle
Begins when mesenchyme
becomes thickened with capillaires
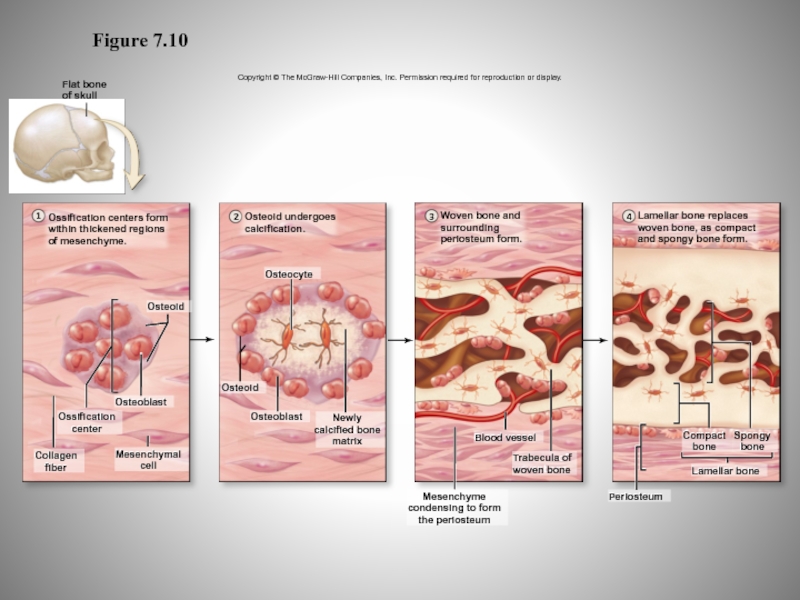
Слайд 72Figure 7.10
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
1
2
3
4
Flat bone
of skull
Ossification centers form
within thickened regions
of mesenchyme.
Osteoid
undergoes
calcification.
Woven bone and
surrounding
periosteum form.
Lamellar bone replaces
woven bone, as compact
and spongy bone form.
Spongy
bone
Lamellar bone
Compact
bone
Periosteum
Mesenchyme
condensing to form
the periosteum
Trabeculaof
wovenbone
Blood vessel
Newly
alcified bone
matrix
Osteoblast
Osteocyte
Osteoid
Collagen
fiber
Mesenchymal
cell
Ossification
center
Osteoblast
Spongy
bone
Lamellar bone
Compact
bone
Periosteum
Mesenchyme
condensing to form
the periosteum
Trabecula of
woven bone
Blood vessel
Newly
calcified bone
matrix
Osteoblast
Osteocyte
Osteoid
Collagen
fiber
Mesenchymal
cell
Ossification
center
Osteoblast
Osteoid
Osteoid
Слайд 73Endochondral Ossification
Begins with a hyaline cartilage model
Produces most bones of
the skeleton, including:
bones of the upper and lower limbs
pelvis
vertebrae
ends of
the clavicle
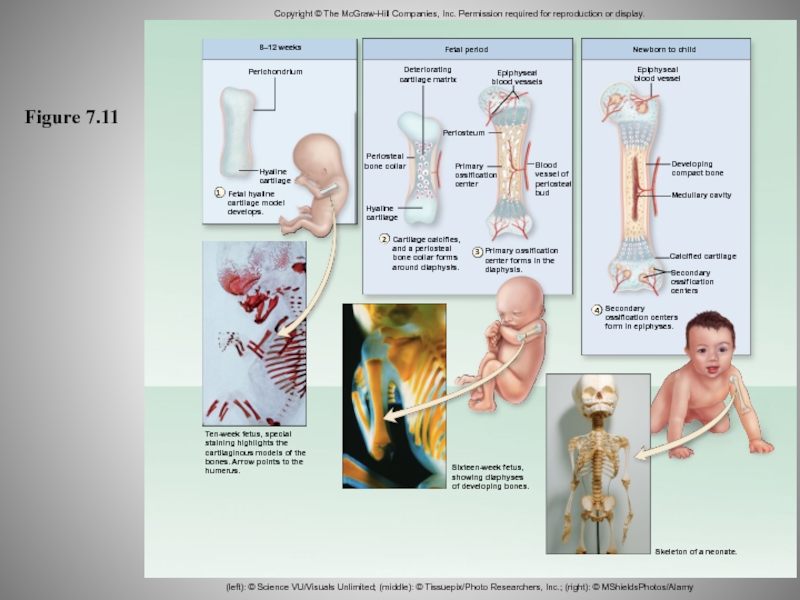
Слайд 74Figure 7.11
Ten-week fetus, special
staining highlights the
cartilaginous models of the
bones. Arrow
points to the
humerus.
8–12 weeks
Perichondrium
Hyaline
cartilage
Fetal hyaline
cartilage model
develops.
Sixteen-week fetus,
showing diaphyses
of developing bones.
Skeleton
of a neonate.
Fetal period
Newborn to child
Deteriorating
cartilage matrix
Epiphyseal
blood vessels
Epiphyseal
blood vessel
Periosteal
bone collar
Hyaline
cartilage
Cartilage calcifies,
and a periosteal
bone collar forms
around diaphysis.
Primary ossification
center forms in the
diaphysis.
Secondary
ossification centers
form in epiphyses.
Secondary
ossification
centers
Calcified cartilage
Developing
compact bone
Medullary cavity
Periosteum
Primary
ossification
center
Blood
vessel of
periosteal
bud
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
(left): © Science VU/Visuals Unlimited; (middle): © Tissuepix/Photo Researchers, Inc.; (right): © MShieldsPhotos/Alamy
1
2
3
4
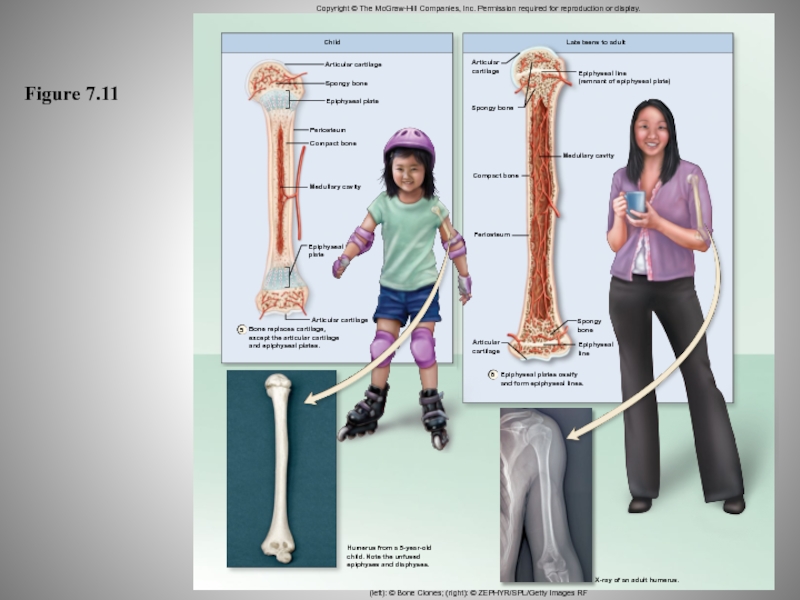
Слайд 75Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction
or display.
6
5
Humerus from a 5-year-old
child. Note the unfused
epiphyses and diaphyses.
X-ray
of an adult humerus.
Epiphyseal plates ossify
and form epiphyseal lines.
Epiphyseal
line
Medullary cavity
Epiphyseal line
(remnant of epiphyseal plate)
Compact bone
Periosteum
Spongy
bone
Articular
cartilage
Articular
cartilage
Spongy bone
Child
Articular cartilage
Spongy bone
Epiphyseal plate
Periosteum
Compact bone
Medullary cavity
Epiphyseal
plate
Articular cartilage
Bone replaces cartilage,
except the articular cartilage
and epiphyseal plates.
Late teens to adult
(left): © Bone Clones; (right): © ZEPHYR/SPL/Getty Images RF
Figure 7.11
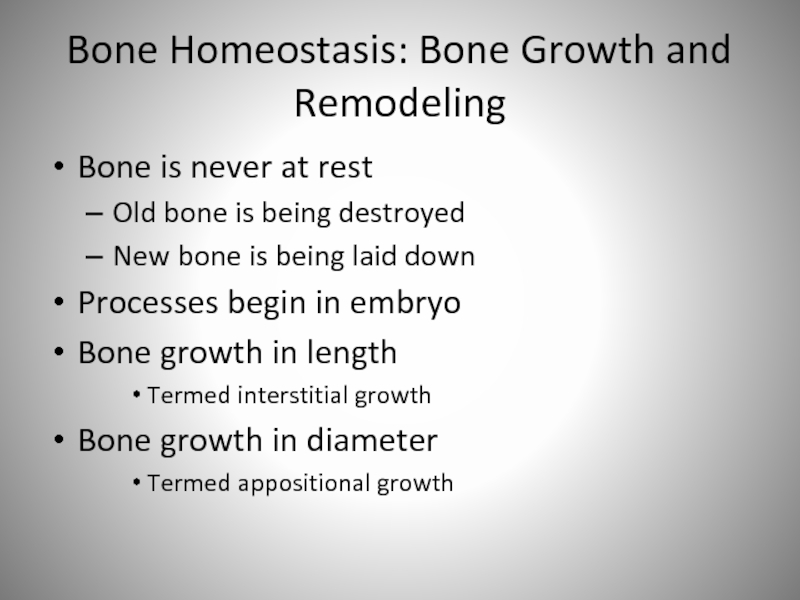
Слайд 76Bone Homeostasis: Bone Growth and Remodeling
Bone is never at rest
Old
bone is being destroyed
New bone is being laid down
Processes
begin in embryo
Bone growth in length
Termed interstitial growth
Bone growth in diameter
Termed appositional growth
Слайд 77Bone Growth and Remodeling: Role of Bone Cells
Osteoblasts make new
bone matrix (using Ca++ from blood)
Osteoclasts ("bone breakers") dissolve bone
matrix (releasing Ca++ to blood)
Слайд 78Bone Growth
Interstitial growth
Occurs in epiphyseal plate
Increases bone length
Appositional growth
Occurs within
the periosteum
Increases bone diameter
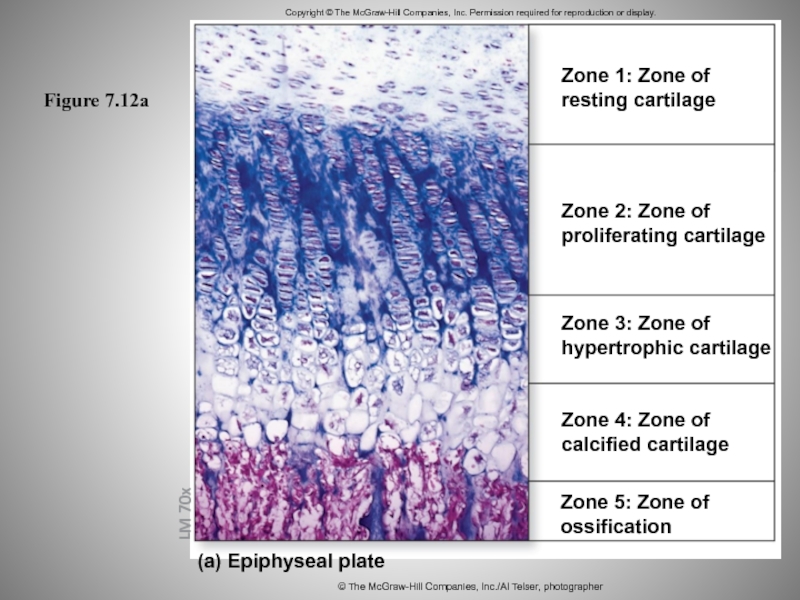
Слайд 79Figure 7.12a
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
LM 70x
Zone 1: Zone of
resting cartilage
Zone 2: Zone
of
proliferating cartilage
Zone 3: Zone of
hypertrophic cartilage
Zone 4: Zone of
calcified cartilage
Zone 5: Zone of
ossification
© The McGraw-Hill Companies, Inc./Al Telser, photographer
(a) Epiphyseal plate
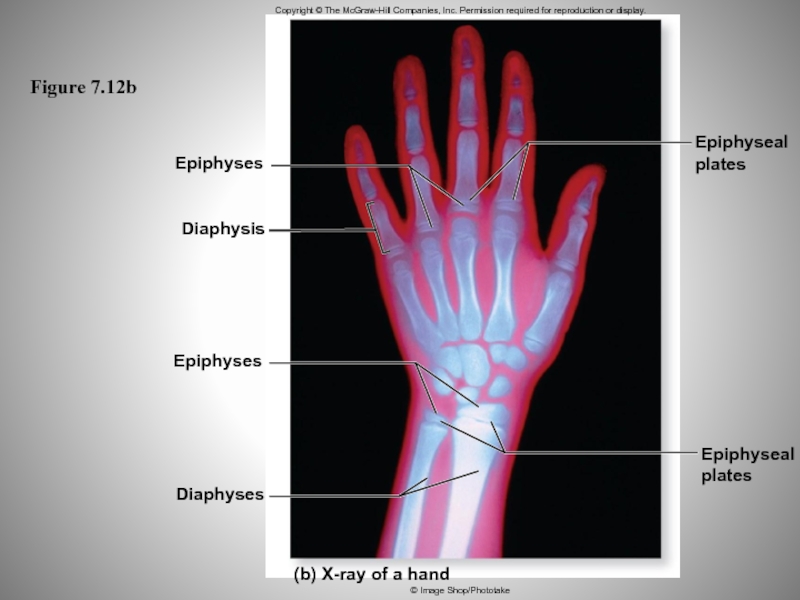
Слайд 80Figure 7.12b
Epiphyses
(b) X-ray of a hand
Epiphyseal
plates
Epiphyseal
plates
Diaphysis
Epiphyses
Diaphyses
Copyright © The McGraw-Hill Companies,
Inc. Permission required for reproduction or display.
© Image Shop/Phototake
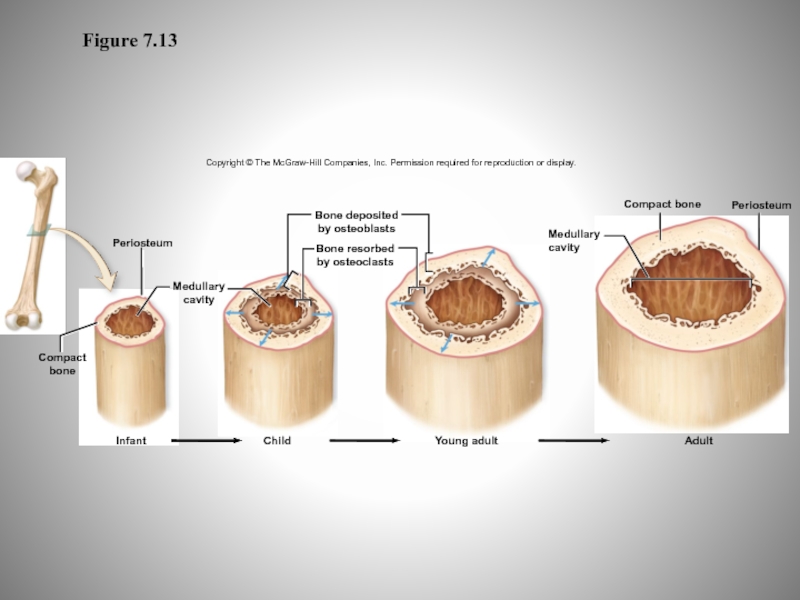
Слайд 82Figure 7.13
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
Bone deposited
by osteoblasts
Bone resorbed
by osteoclasts
Periosteum
Medullary
cavity
Compact
bone
Infant
Child
Young adult
Adult
Medullary
cavity
Compact bone
Periosteum
Слайд 83Bone Growth and Remodeling: Role of Hormones
Calcitonin (CT; from thyroid)
increases Ca++ storage (out of blood)
Parathyroid hormone (PTH) gets Ca++
out of storage (into blood)
Growth Hormone
Thyroid Hormone
Glucocorticoids
Serotonin
Estrogen/Testosterone
Слайд 84Bone Growth and Remodeling: Mechanical Stress
Weight bearing activity and exercise
causes bone growth
increased deposition of minerals salts and production of
collagen fibers
Benefits of weight-lifting, running
Lack of weight bearing activity weakens bones
astronauts
Слайд 85Blood Calcium Levels
Regulating calcium concentration in blood is essential
Calcium is
required for:
initiation of muscle contraction
exocytosis of molecules from cells, including
neurons
stimulation of the heart by pacemaker cells
blood clotting
Two primary hormones regulate blood calcium:
calcitriol
parathyroid hormone
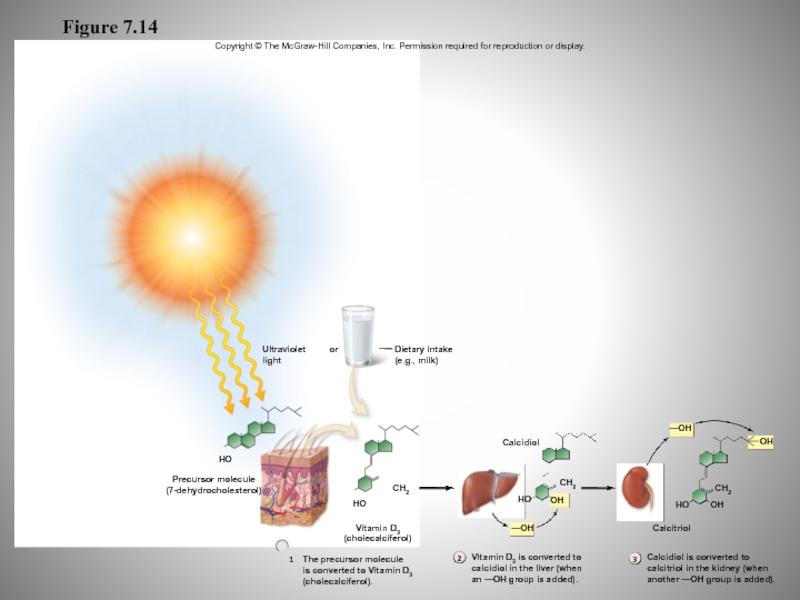
Слайд 86Figure 7.14
1
2
3
Dietary intake
(e.g., milk)
OH
Calcidiol
Ultraviolet
light
or
HO
Precursor molecule
(7-dehydrocholesterol)
The precursor molecule
is converted to Vitamin
D3
(cholecalciferol).
Vitamin D3 is converted to
calcidiol in the liver (when
an —OH
group is added).
Calcidiol is converted to
calcitriol in the kidney (when
another —OH group is added).
HO
CH2
—OH
—OH
CH2
OH
HO
CH2
OH
HO
Calcitriol
Vitamin D3
(cholecalciferol)
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Слайд 87Regulating Blood Calcium Levels:
Parathyroid Hormone and Calcitriol
Clinical View: Rickets
Disease
caused by vitamin D deficiency in childhood
Characterized by deficient calcification
of osteoid tissue
Acquire bowlegged appearance
Disturbances in growth, hypocalcemia, and tetany (cramps and twitches)
caused by low blood calcium
Continues to occur in some developing nations
Incidence increasing in urban U.S. children
Слайд 88Blood Calcium Levels
Calcitonin
Aids in regulating blood calcium levels
Less significant role
than PTH or calcitriol
Released from the thyroid gland in response
to high blood calcium levels
Inhibits osteoclast activity in bone connective tissue
less calcium released from bone into blood
Stimulates kidneys to increase loss of calcium in the urine
reducing blood calcium levels
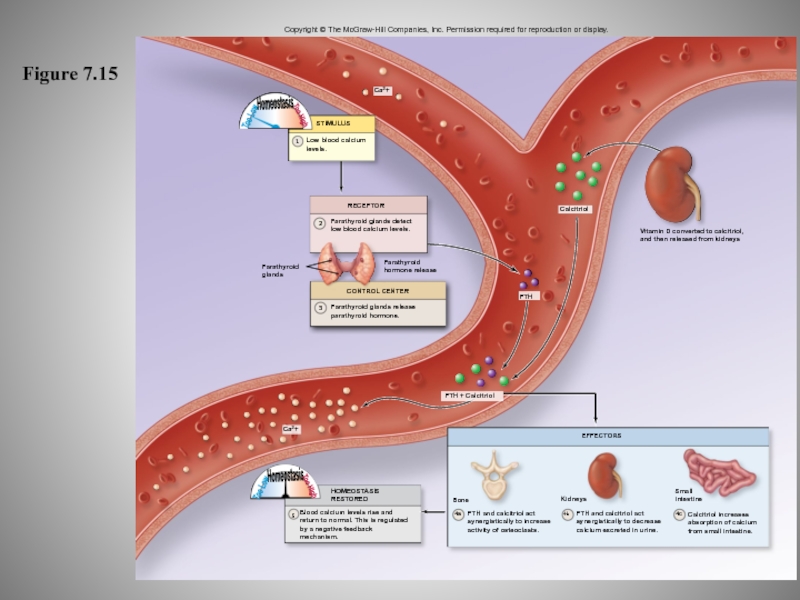
Слайд 89Figure 7.15
5
4b
1
Ca2+
EFFECTORS
Calcitriol increases
absorption of calcium
from small intestine.
4c
Small
intestine
PTH and calcitriol act
synergistically
to decrease
calcium excreted in urine.
PTH and calcitriol act
synergistically to increase
activity
of osteoclasts.
4a
Kidneys
Bone
Blood calcium levels rise and
return to normal. This is regulated
by a negative feedback
mechanism.
Ca2+
STIMULUS
Low blood calcium
levels.
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
HOMEOSTASIS
RESTORED
Too Low
Homeostasis
Too High
Too Low
Homeostasis
Too High
3
2
RECEPTOR
Parathyroid glands detect
low blood calcium levels.
Parathyroid
glands
CONTROL CENTER
Parathyroid glands release
parathyroid hormone.
Parathyroid
hormone release
PTH + Calcitriol
PTH
Vitamin D converted to calcitriol,
and then released from kidneys
Calcitriol
Слайд 90Effects of Aging on Bone
More bone is made than is
lost until age 25 (usually rapid until puberty, then slows)
About
as much bone is made as is lost 25-50 (can vary)
More bone is lost than is made 50-120
Yellow marrow replaces red marrow, reducing total RBC production
Слайд 91Effects of Aging
Osteopenia
Occurs slightly in all people with age
Begins as
early as age 35-40
Osteoblast activity declining; osteoclast activity at previous
levels
Vertebrae, jaw bones, epiphyses losing large amount of mass
Women losing more of their skeletal mass every decade than men
Слайд 92Effects of Aging
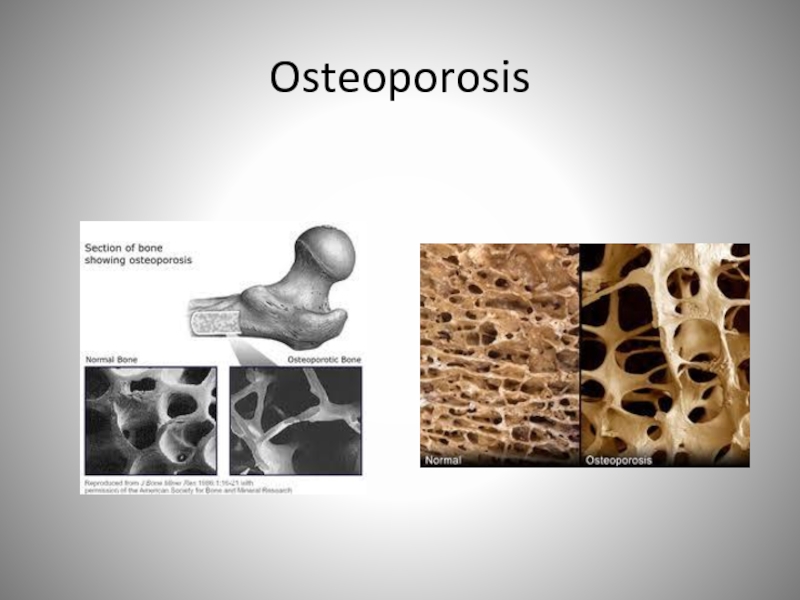
Osteoporosis
Reduced bone mass sufficient to compromise normal function
Occurs
in a significant percentage of older women
Occurs in a smaller
percentage of older men
Reduced hormones with age
Include growth hormone, estrogen, and testosterone
Contributes to reduction in bone mass
Reduced bone mass sufficient to compromise normal function
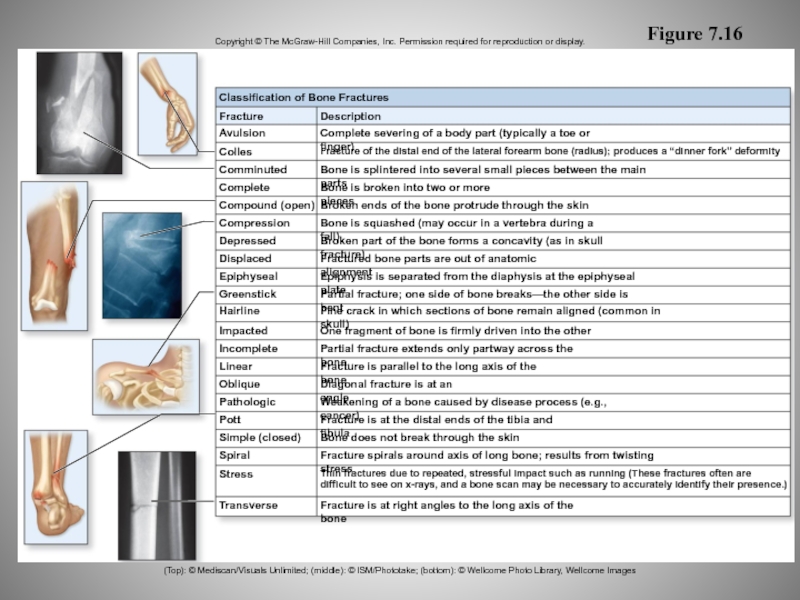
Слайд 94Bone Fracture and Repair
Breaks in bone
Termed fractures
Occur as result of
unusual stress or impact
Increased incidence with age
due to normal
thinning and weakening of bone
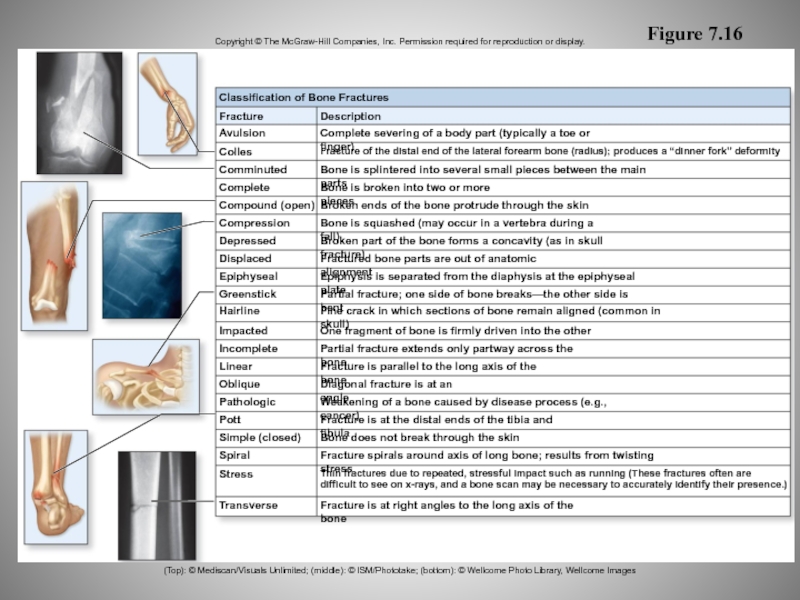
Слайд 95Figure 7.16
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
Classification of Bone Fractures
Description
Fracture
Avulsion
Colles
Comminuted
Complete
Compound (open)
Compression
Depressed
Displaced
Epiphyseal
Greenstick
Hairline
Impacted
Incomplete
Linear
Oblique
Pathologic
Pott
Simple (closed)
Spiral
Stress
Transverse
Fracture is at
right angles to the long axis of the bone
Thin fractures due to repeated, stressful impact such as running (These fractures often are
difficult to see on x-rays, and a bone scan may be necessary to accurately identify their presence.)
Fracture spirals around axis of long bone; results from twisting stress
Bone does not break through the skin
Fracture is at the distal ends of the tibia and fibula
Weakening of a bone caused by disease process (e.g., cancer)
Diagonal fracture is at an angle
Fracture is parallel to the long axis of the bone
Partial fracture extends only partway across the bone
One fragment of bone is firmly driven into the other
Fine crack in which sections of bone remain aligned (common in skull)
Partial fracture; one side of bone breaks—the other side is bent
Epiphysis is separated from the diaphysis at the epiphyseal plate
Fractured bone parts are out of anatomic alignment
Broken part of the bone forms a concavity (as in skull fracture)
Bone is squashed (may occur in a vertebra during a fall)
Broken ends of the bone protrude through the skin
Bone is broken into two or more pieces
Bone is splintered into several small pieces between the main parts
Fracture of the distal end of the lateral forearm bone (radius); produces a “dinner fork” deformity
Complete severing of a body part (typically a toe or finger)
(Top): © Mediscan/Visuals Unlimited; (middle): © ISM/Phototake; (bottom): © Wellcome Photo Library, Wellcome Images
Слайд 96Bone Fracture and Repair
Fracture healing
Simple fracture about 2 to 3
months to heal
Compound fracture longer to heal
Generally becomes slower with
age
Some require surgical intervention to heal correctly
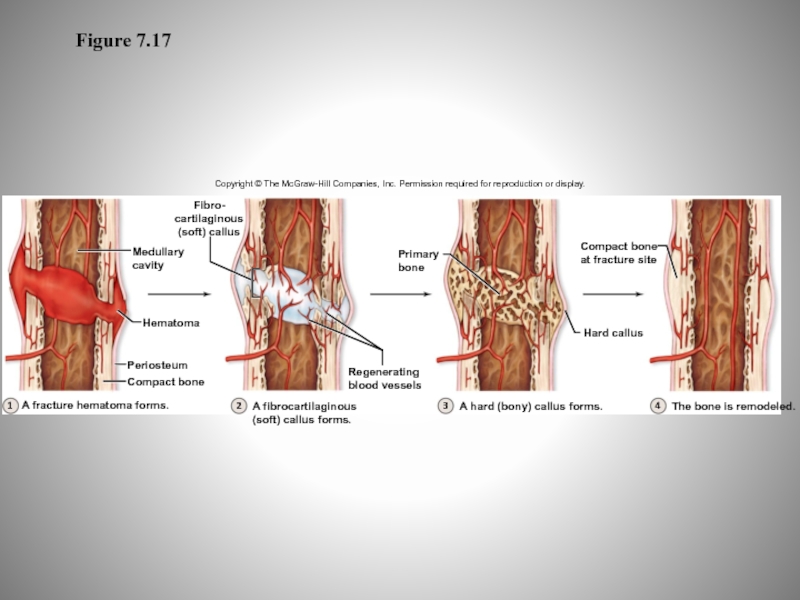
Слайд 97Figure 7.17
Copyright © The McGraw-Hill Companies, Inc. Permission required for
reproduction or display.
1
2
3
4
Fibro-
cartilaginous
(soft) callus
Medullary
cavity
Hematoma
A fracture hematoma forms.
Compact bone
Periosteum
A fibrocartilaginous
(soft) callus
forms.
Regenerating
blood vessels
A hard (bony) callus forms.
The bone is remodeled.
Compact bone
at fracture site
Primary
bone
Hard callus