Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Thyroid gland diseases
Содержание
- 1. Thyroid gland diseases
- 2. Слайд 2
- 3. IntroductionThyroid hormone is essential for the growth
- 4. Location: Located close to thyroid cartilage. Has
- 5.
- 6. Слайд 6
- 7. Thyroid Physiology
- 8. Pathways of thyroid Hormone metabolism
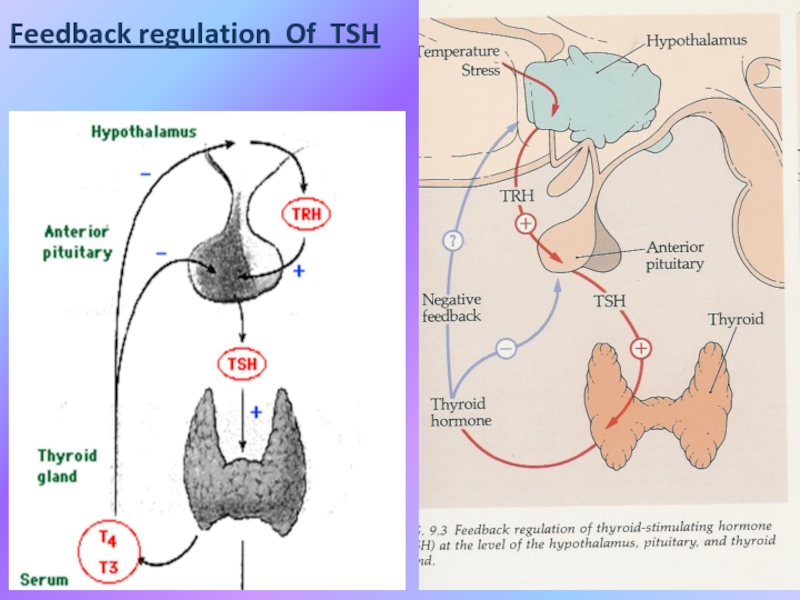
- 9. Feedback regulation Of TSH
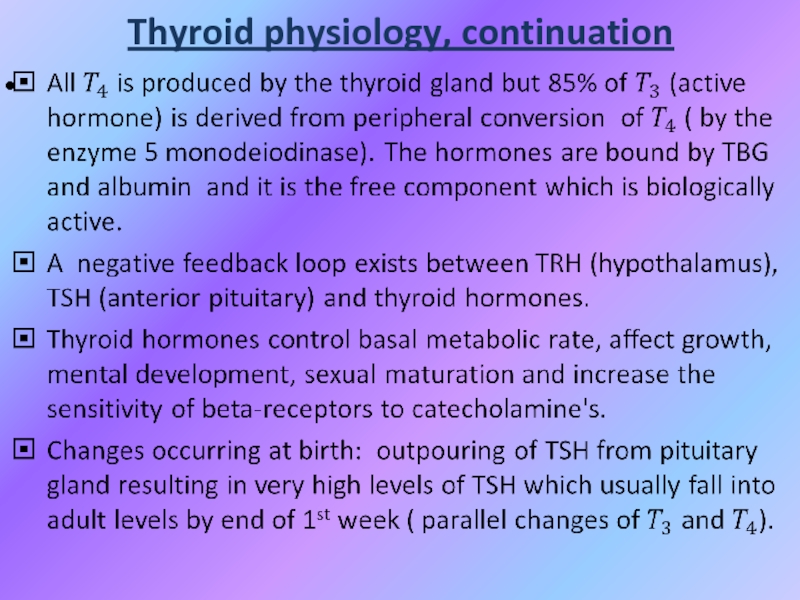
- 10. Thyroid physiology, continuation
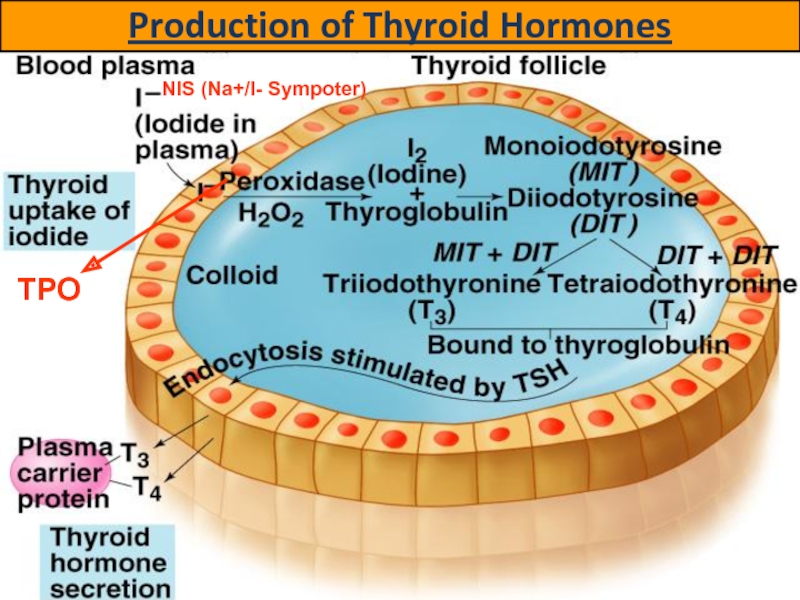
- 11. Production of Thyroid HormonesNIS (Na+/I- Sympoter)TPO
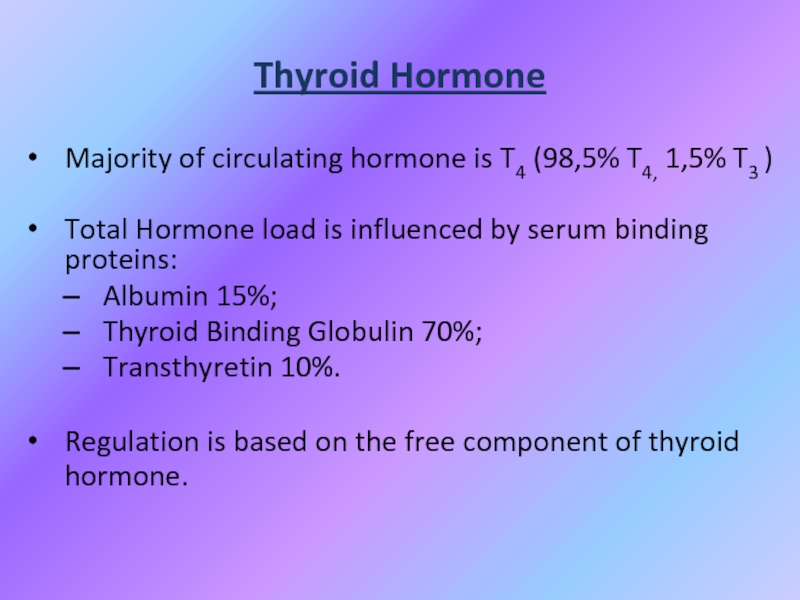
- 12. Thyroid HormoneMajority of circulating hormone is T4
- 13. Effects of thyroid hormonesFetal brain and skeletal
- 14. Thyroid hormones
- 15. Comparative analysis of thyroid hormones
- 16. THYROTOXICOSIS (Hyperthyroidism)Overproduction of thyroid hormones;HYPOTHYROIDISM (Gland destruction)Underproduction of thyroid hormones;NEOPLASTIC PROCESSESBenign;Malignant.THYROID GLAND DISORDERS DIVIDED INTO:
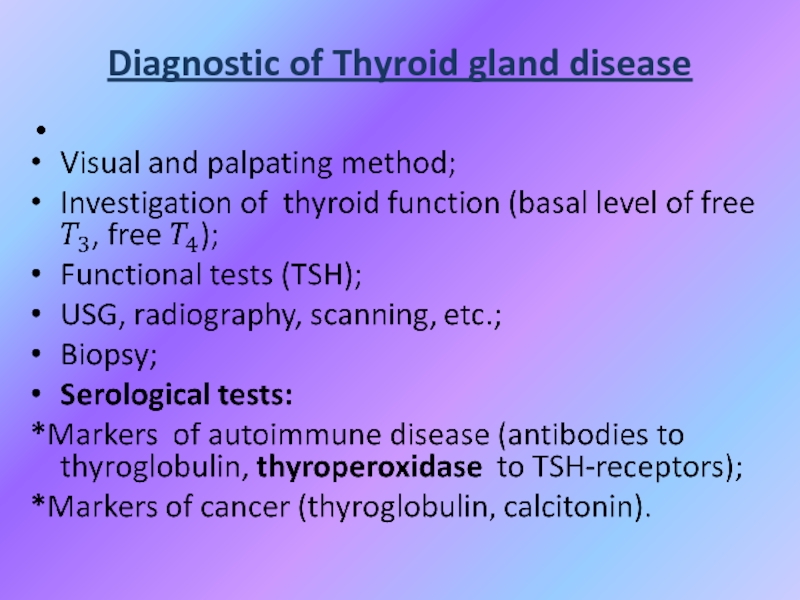
- 17. Diagnostic of Thyroid gland disease
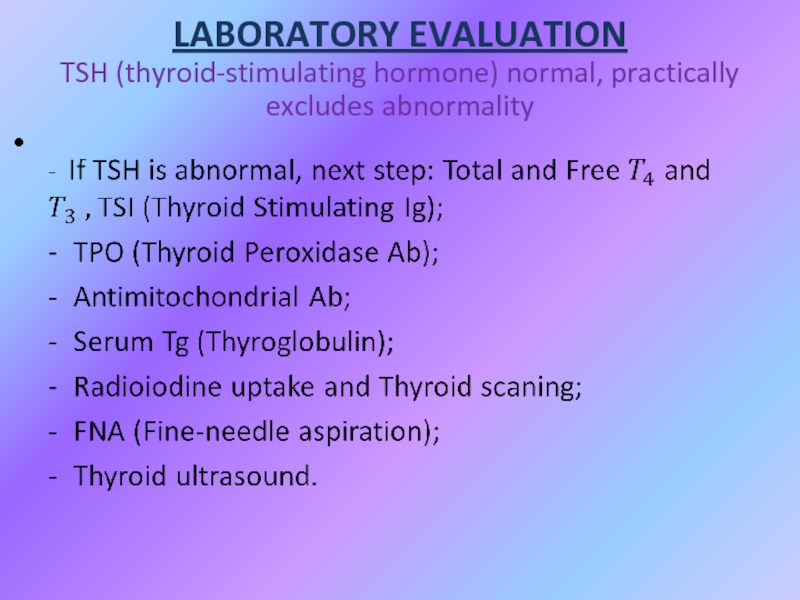
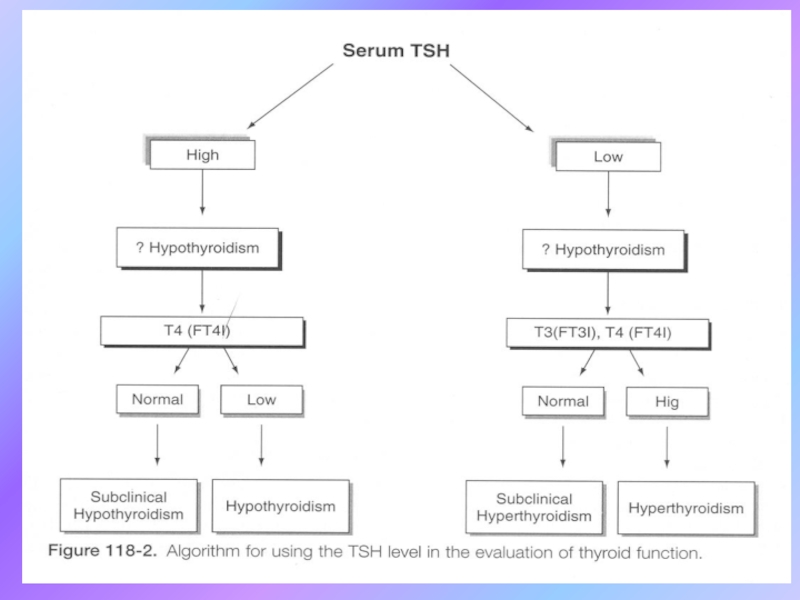
- 18. LABORATORY EVALUATION TSH (thyroid-stimulating hormone) normal, practically excludes abnormality
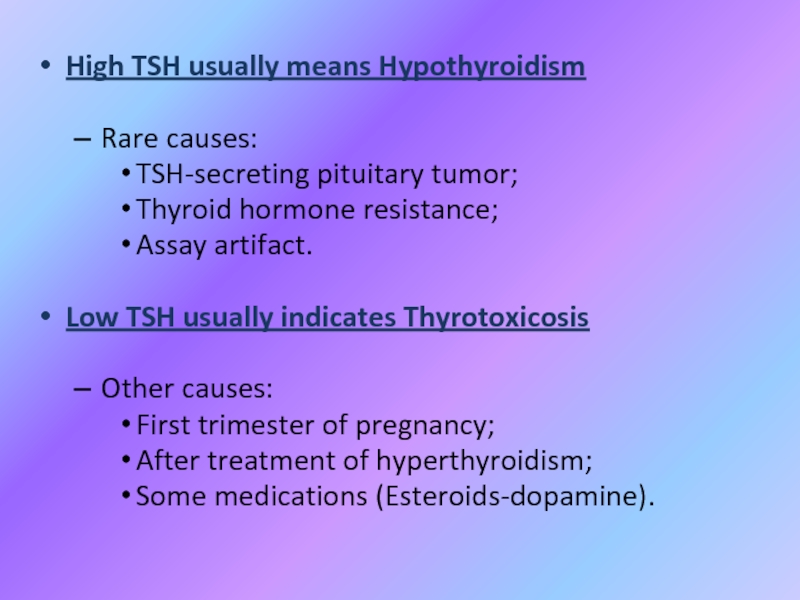
- 19. High TSH usually means HypothyroidismRare causes: TSH-secreting pituitary
- 20. Слайд 20
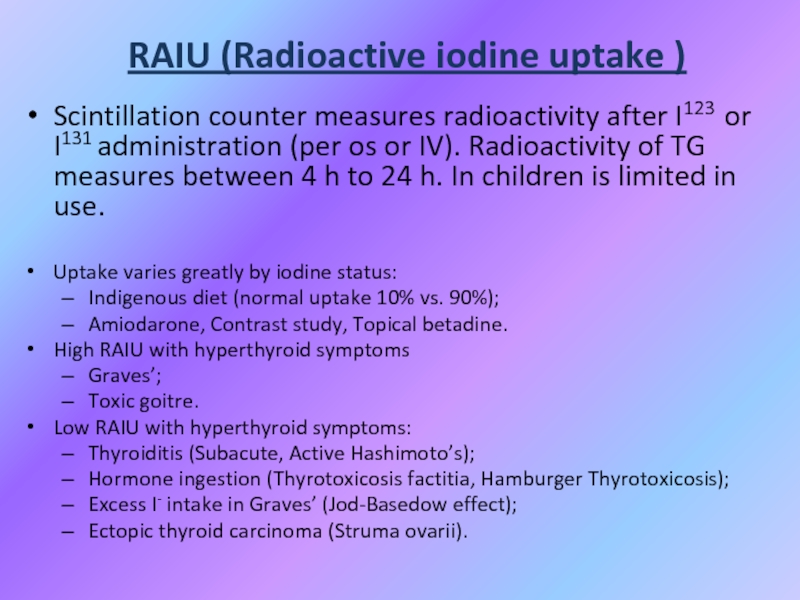
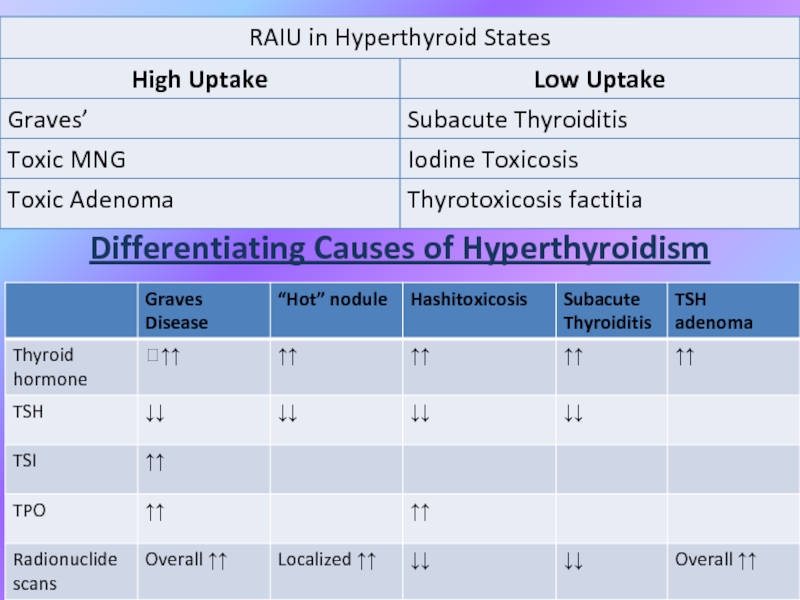
- 21. RAIU (Radioactive iodine uptake )Scintillation counter measures
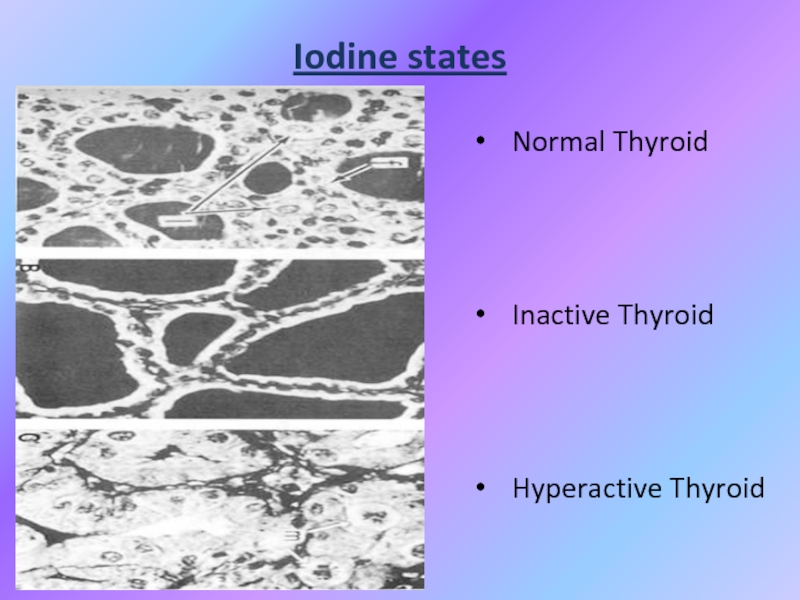
- 22. Iodine statesNormal ThyroidInactive ThyroidHyperactive Thyroid
- 23. Thyrotoxicosis Primary;Secondary;Without Hyperthyroidism;Exogenous or factitious.HypothyroidismPrimary;Secondary;Peripheral.
- 24. HYPERTHYROIDISM or THYROTOXICOSIS: - is the result
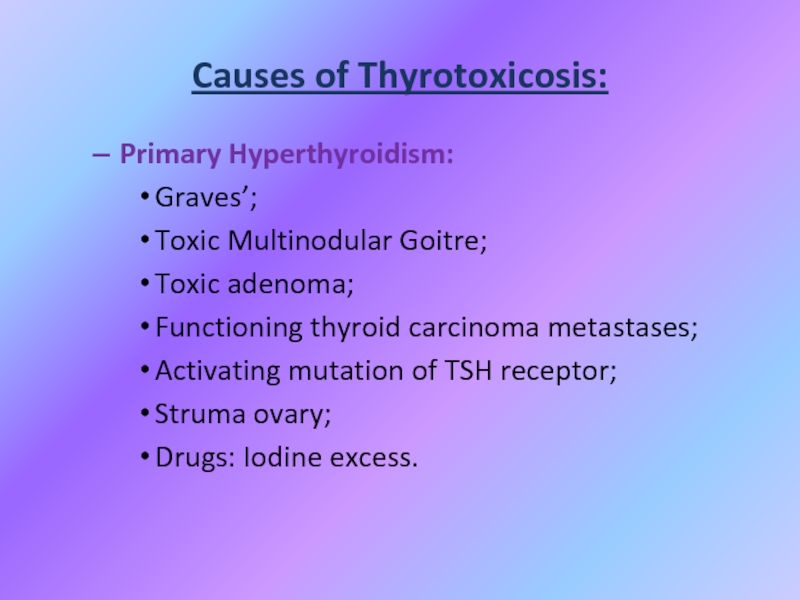
- 25. Primary Hyperthyroidism:Graves’;Toxic Multinodular Goitre;Toxic adenoma;Functioning thyroid carcinoma
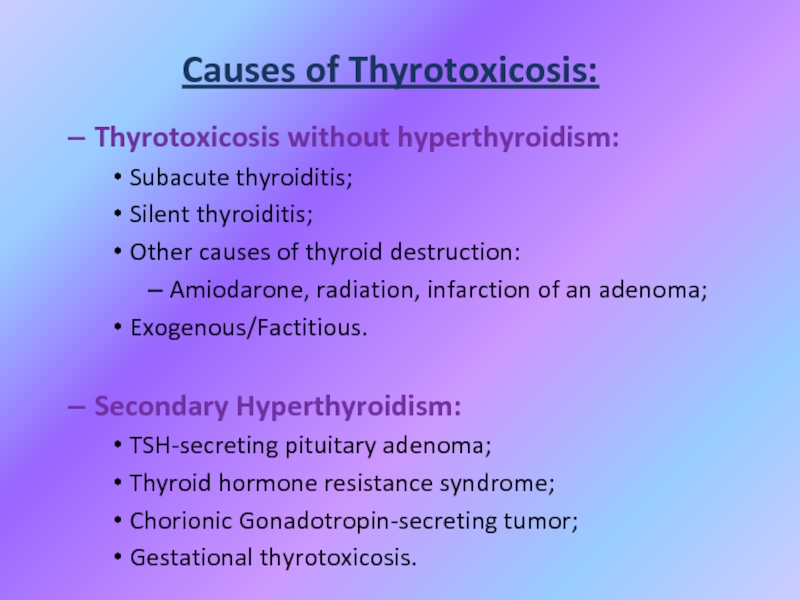
- 26. Causes of Thyrotoxicosis:Thyrotoxicosis without hyperthyroidism:Subacute thyroiditis;Silent thyroiditis;Other
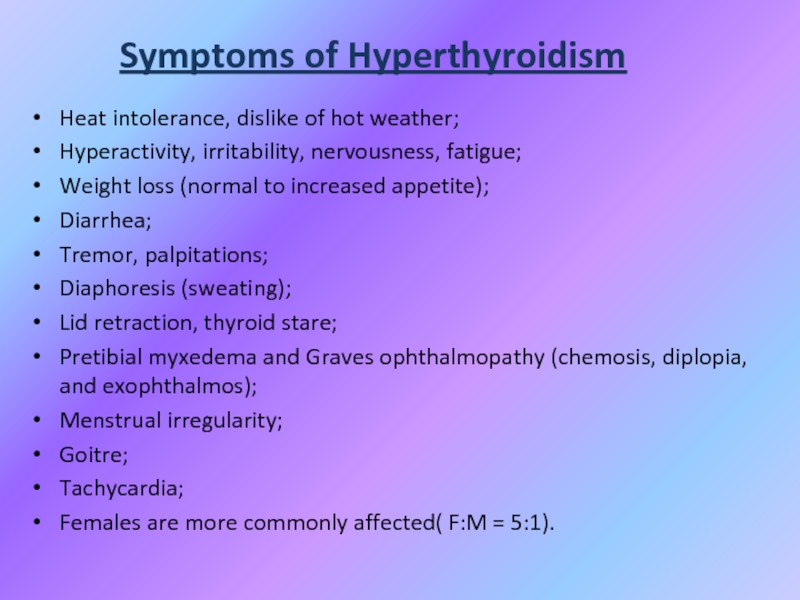
- 27. Symptoms of HyperthyroidismHeat intolerance, dislike of hot
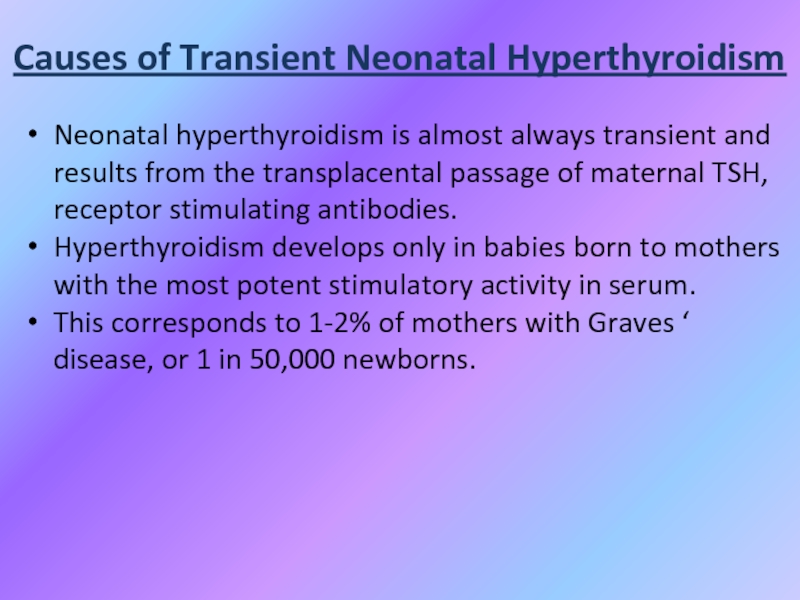
- 28. Causes of Transient Neonatal HyperthyroidismNeonatal hyperthyroidism is
- 29. Situations That Should Prompt Consideration of NeonatalHyperthyroidism:●
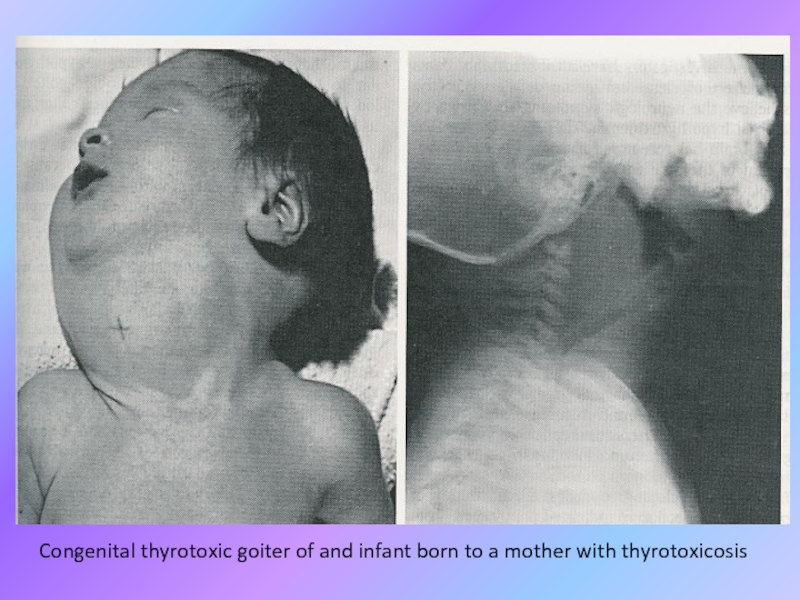
- 30. Congenital thyrotoxic goiter of and infant born to a mother with thyrotoxicosis
- 31. Therapy of Transient neonatal hyperthyroidismTreatment is accomplished
- 32. Therapy of Transient neonatal hyperthyroidismIn the neonate,
- 33. Therapy of Transient neonatal hyperthyroidismPropranolol (2
- 34. Permanent neonatal hyperthyroidismRarely, neonatal hyperthyroidism is inconvertible
- 35. Permanent neonatal hyperthyroidismEarly recognition is important because
- 36. Слайд 36
- 37. GoitreEndemic goitre:Areas where > 5% of children
- 38. GoitreEtiologyHashimoto’s thyroiditis:Early stages only, late stages show
- 39. Goitre
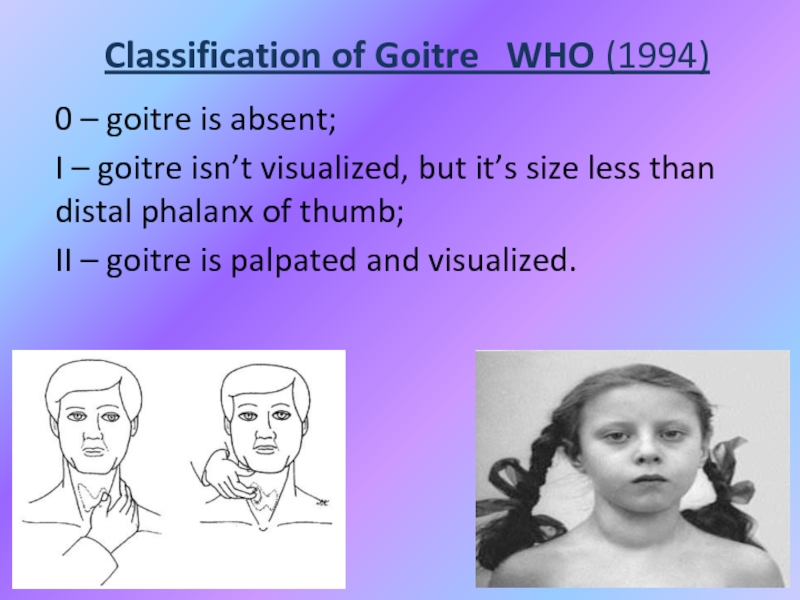
- 40. Classification of Goitre WHO (1994)0 –
- 41. Functional condition of Thyroid influence may be asEuthyroidism;Hypothyroidism;Hyperthyroidism.
- 42. Non-Toxic GoitreCancer screening in non-toxic MNG (Multinodular
- 43. Non-Toxic GoitreTreatment options (no compressive symptoms):Use follow-up
- 44. Non-Toxic GoitreTreatment options (compressive symptoms):Radioactive iodine (RAI)
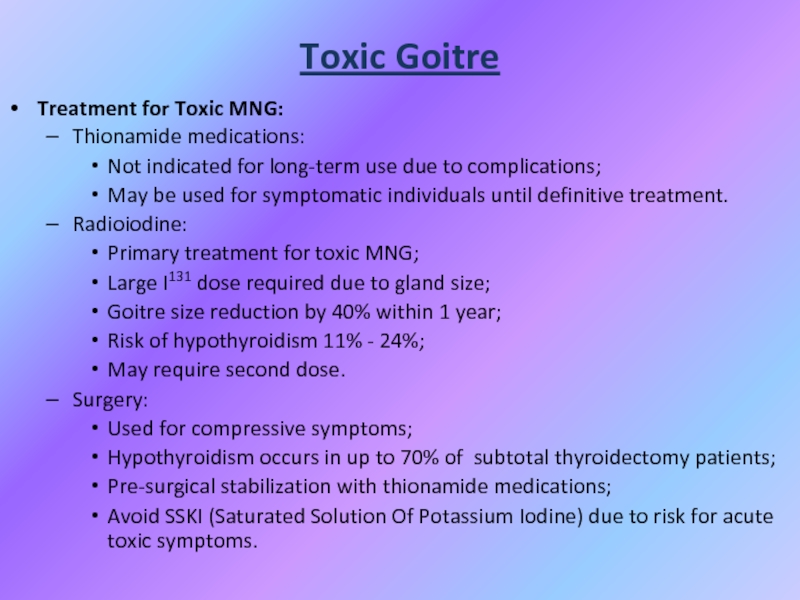
- 45. Toxic GoitreTreatment for Toxic MNG:Thionamide medications:Not indicated
- 46. Graves’ DiseaseDiffuse toxic goitre is an autoimmune
- 47. Слайд 47
- 48. Differentiating Causes of Hyperthyroidism
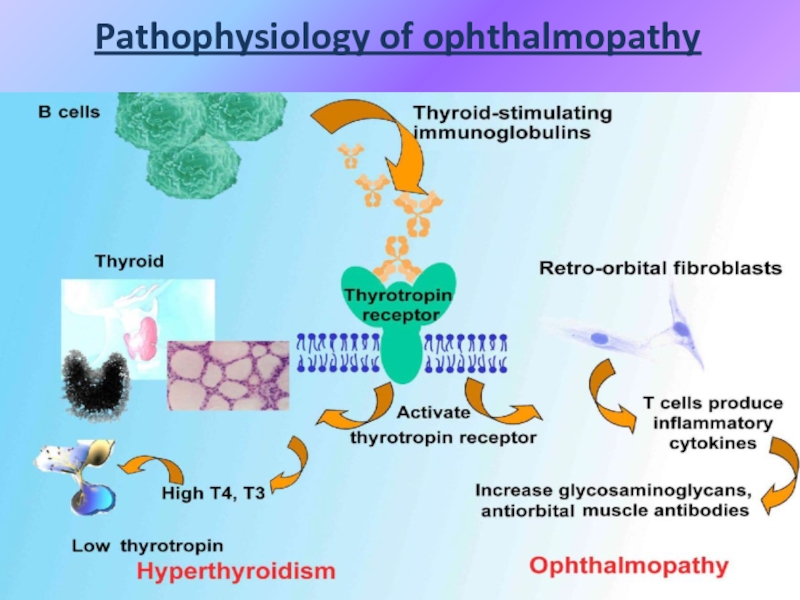
- 49. Pathophysiology of ophthalmopathy
- 50. Graves disease OphthalmopathyA feeling of "sandpaper" in
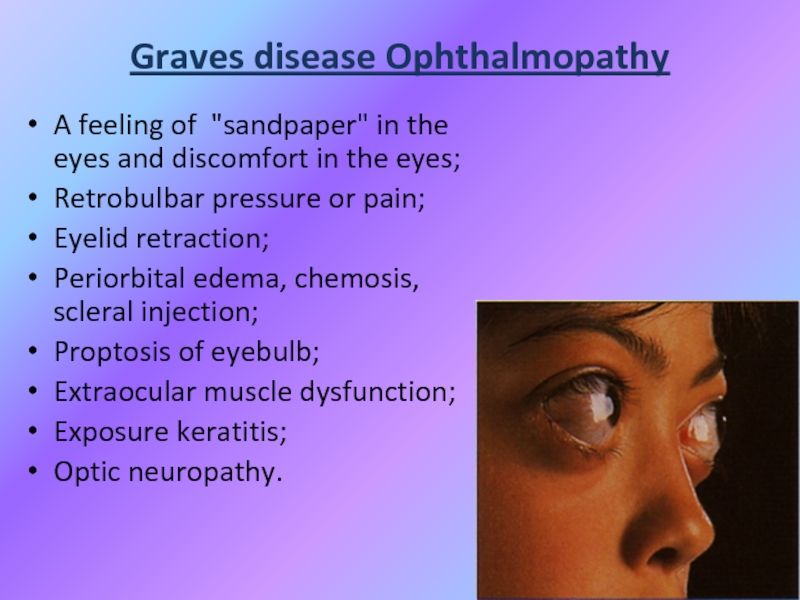
- 51. Graves Disease: Treatment• Medications:– Beta-blockers for symptoms
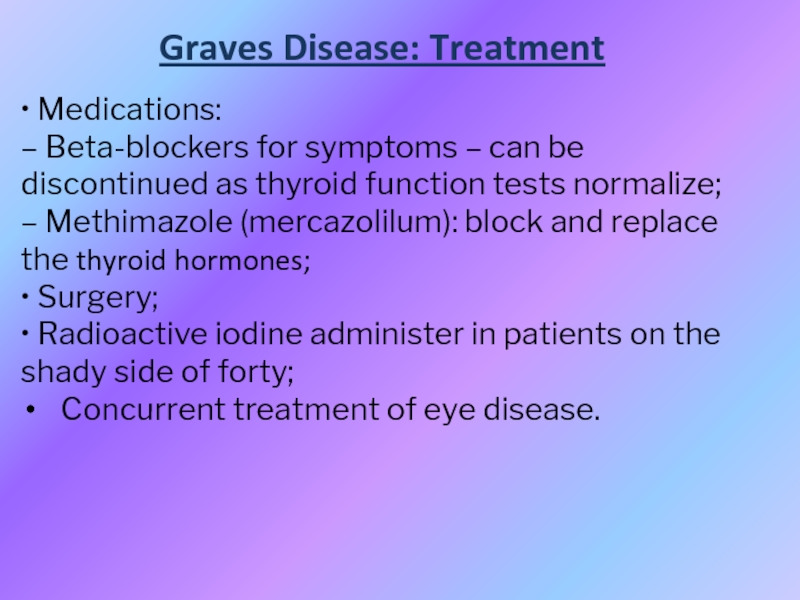
- 52. НypothyroidismHypothyroidism - syndrome with particular or total
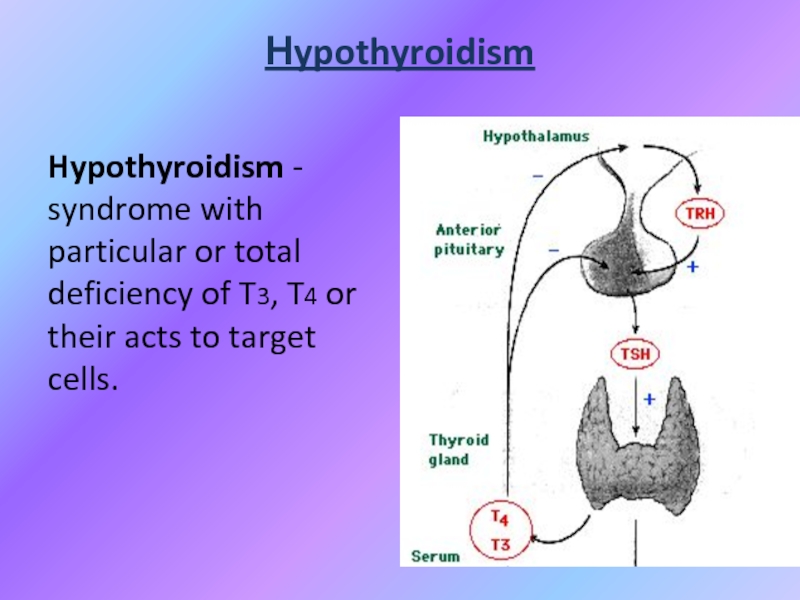
- 53. Classification of hypothyroidismPRIMARY - defects of biosynthesis
- 54. Primary:Autoimmune (Hashimoto´s);Iatrogenic Surgery or 131I administration;Drugs: amiodarone, lithium;Congenital (1 in 3000 to 4000);Iodine defficiency;Infiltrative disorders.
- 55. Secondary:Pituitary gland destruction;Isolated TSH deficiency;Bexarotene treatment;Hypothalamic disorders.Peripheral:Rare, familial tendency.
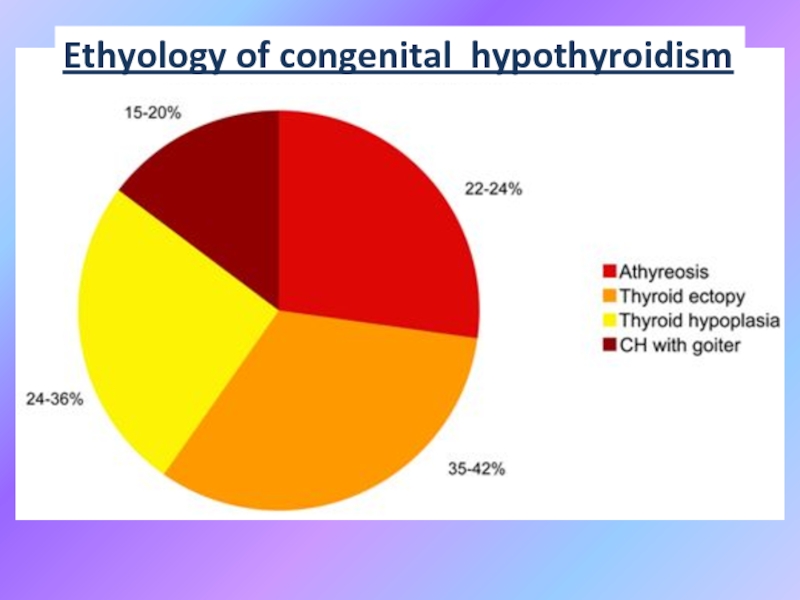
- 56. Ethyology of congenital hypothyroidism
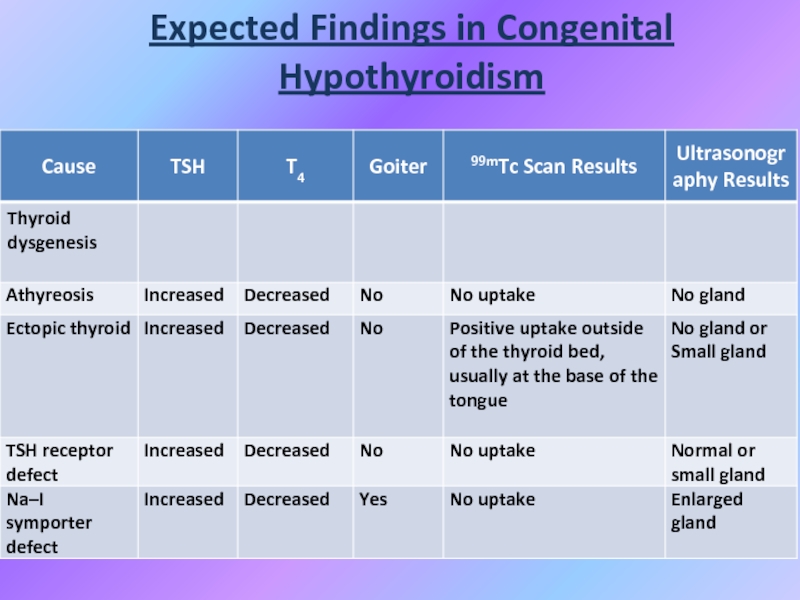
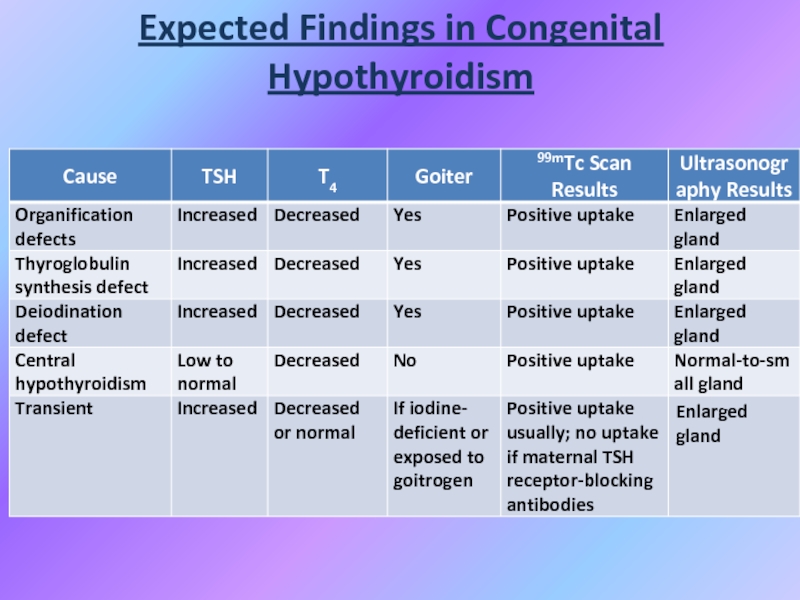
- 57. Expected Findings in Congenital Hypothyroidism
- 58. Expected Findings in Congenital Hypothyroidism
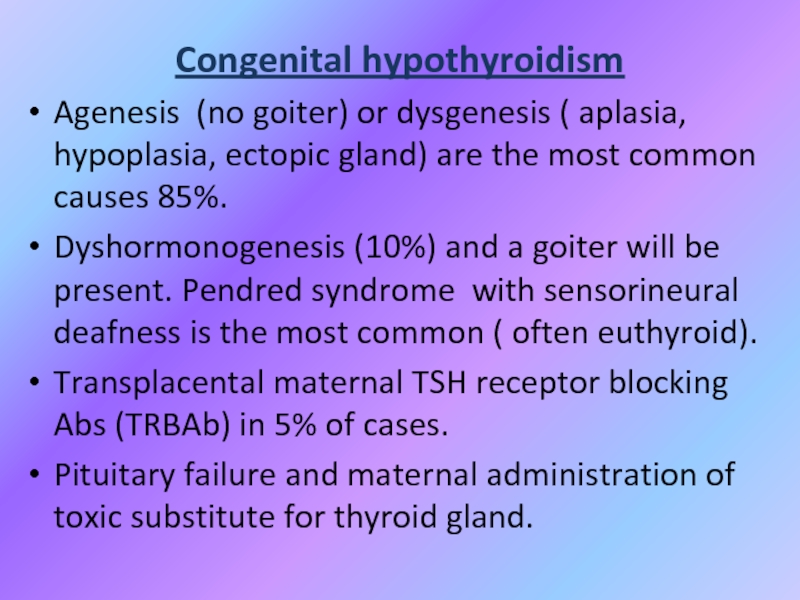
- 59. Congenital hypothyroidismAgenesis (no goiter) or dysgenesis (
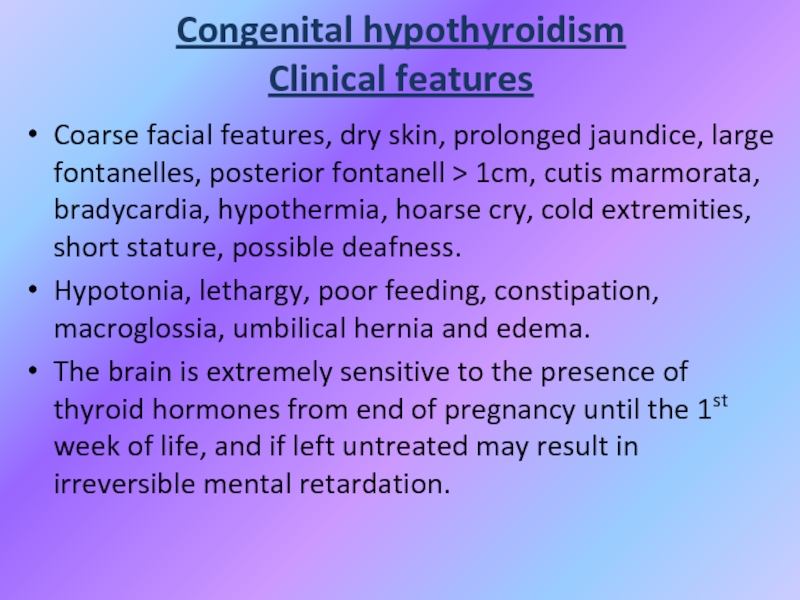
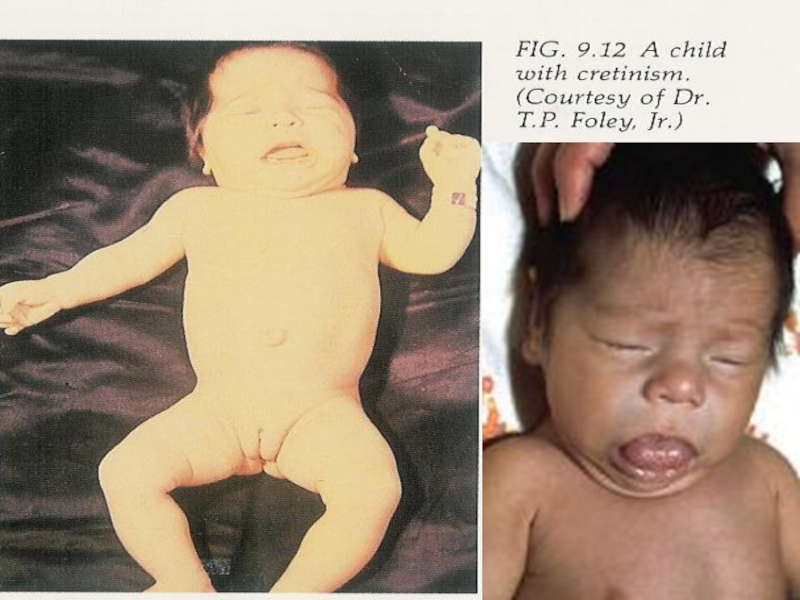
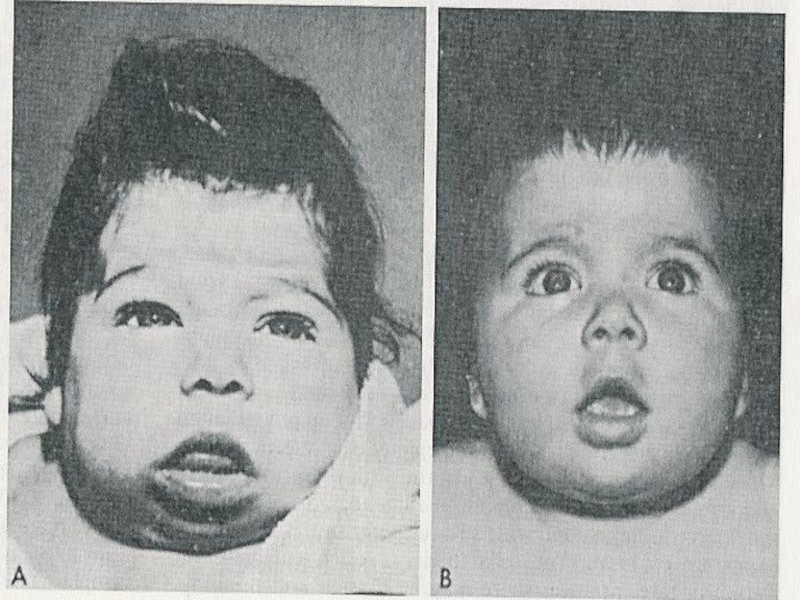
- 60. Congenital hypothyroidism Clinical featuresCoarse facial features, dry
- 61. Слайд 61
- 62. Слайд 62
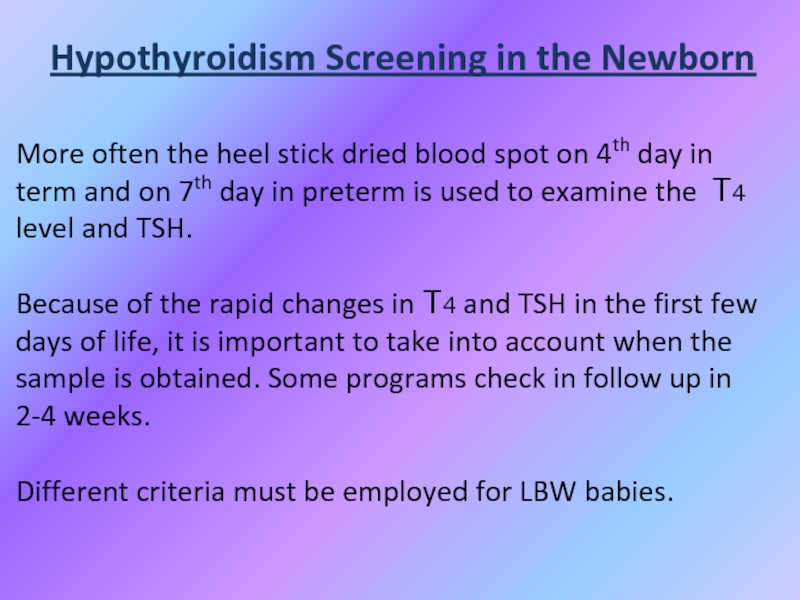
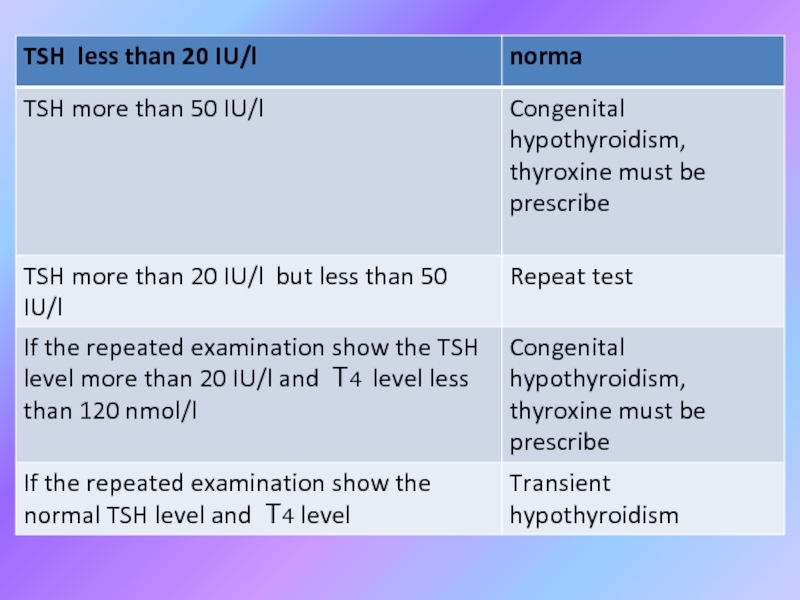
- 63. Hypothyroidism Screening in the NewbornMore often the
- 64. Слайд 64
- 65. Слайд 65
- 66. DIAGNOSTIC STUDIES IN HYPOTHYROIDISMThyroid scan – 99Tc
- 67. Biochemical markers of CHLow serum T4 level
- 68. Biochemical markers of CHOther:Elevated serum cholesterol;Elevated creatinphosphokinase;Hyponatriemia.
- 69. Instrumental dataSlightly decrease heart rate and amplitude
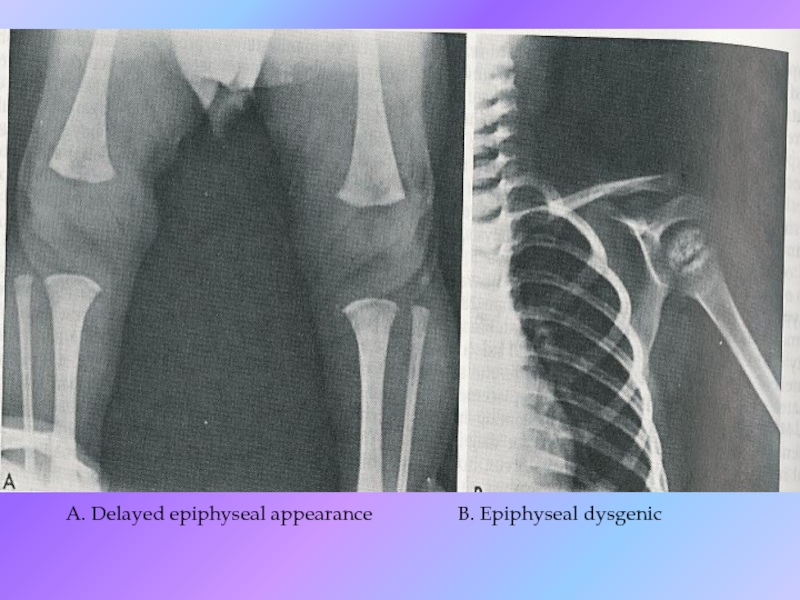
- 70. A. Delayed epiphyseal appearance B. Epiphyseal dysgenic
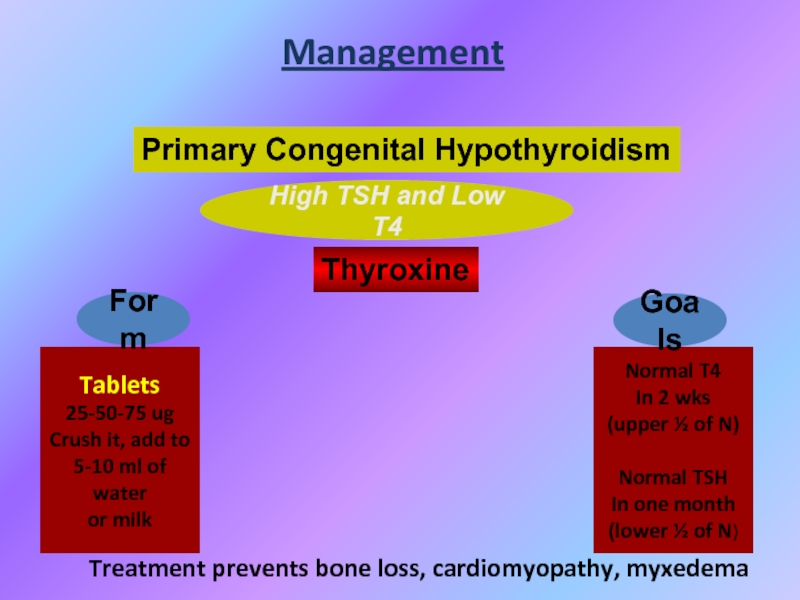
- 71. High TSH and Low T4Management Primary Congenital
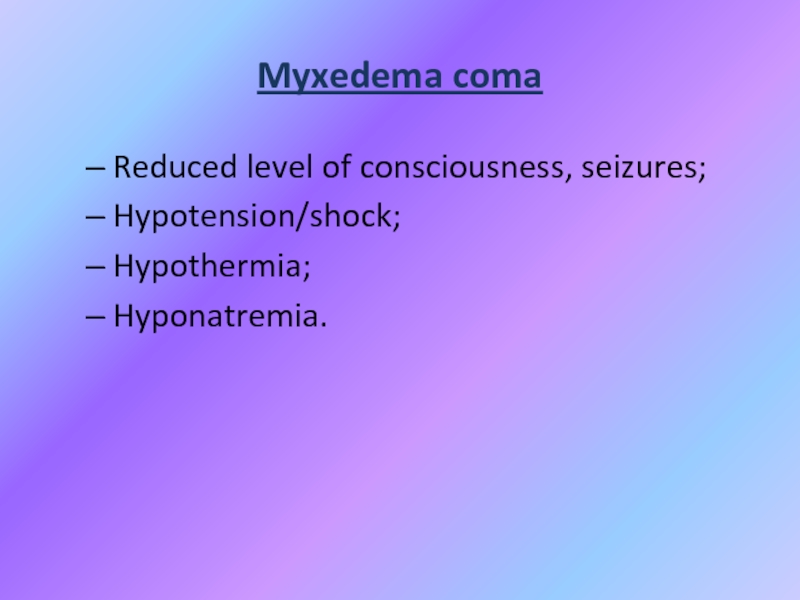
- 72. Myxedema comaReduced level of consciousness, seizures;Hypotension/shock;Hypothermia;Hyponatremia.
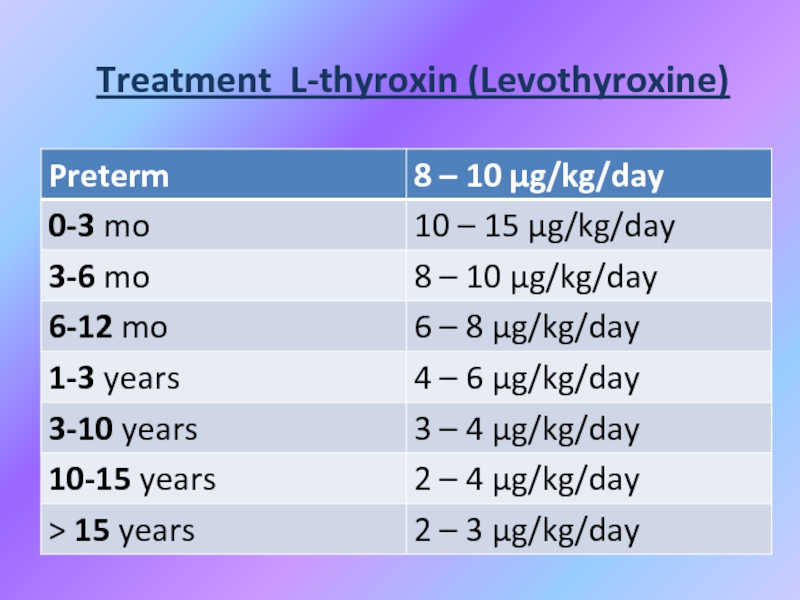
- 73. Treatment L-thyroxin (Levothyroxine)
- 74. PROGNOSISIf treatment is delayed, physical development can
- 75. Juvenile hypothyroidismA child with growth retardation, constipation,
- 76. Causes of juvenile hypothyroidismHashimoto thyroiditis. More common
- 77. JH investigations Antithyroglobulin and antimicrosomal antibodies are
- 78. ETIOLOGY OF ACQUIRED HYPOTHYROIDISMChronic lymphocytic (Hashimoto`s) thyroiditis
- 79. SYMPTOMS OF ACQUIRED HYPOTHYROIDISMSlow growth;Edema; Decreased appetite;Constipation;Swollen
- 80. SIGNS OF ACQUIRED HYPOTHYROIDISM Delayed reflex return;
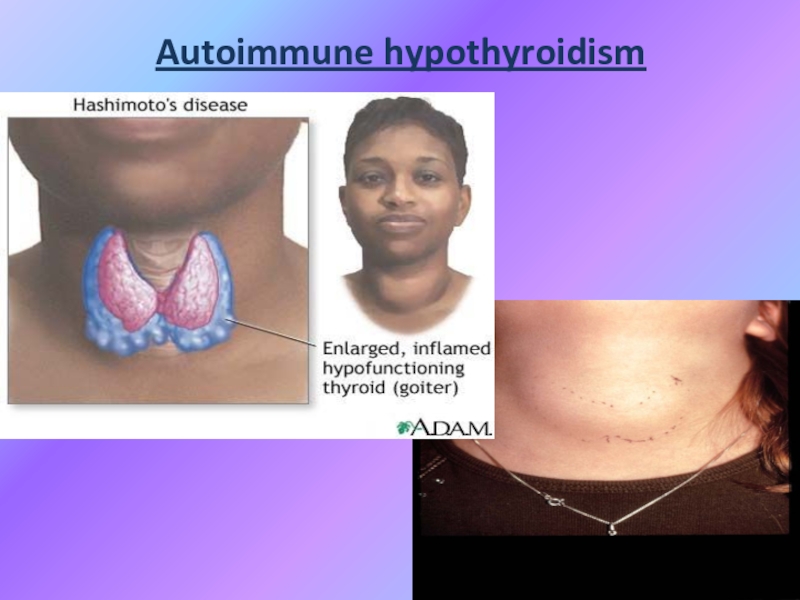
- 81. Chronic thyroiditis Hashimoto diseaseClinical presentation:Painless diffuse goiter;
- 82. Autoimmune hypothyroidism
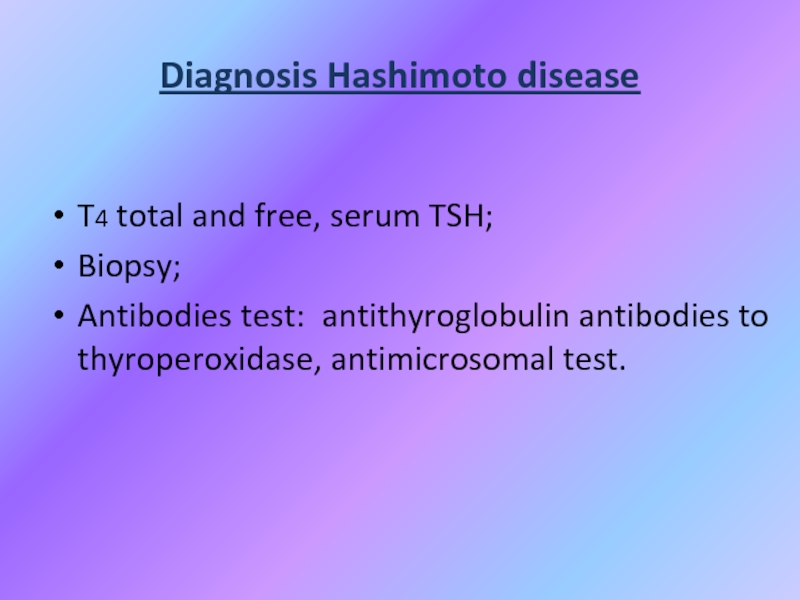
- 83. Diagnosis Hashimoto diseaseT4 total and free, serum TSH;Biopsy;Antibodies test: antithyroglobulin antibodies to thyroperoxidase, antimicrosomal test.
- 84. TreatmentLevothyroxine if hypothyroid;Triiodothyronine (for myxedema coma);Thyroid suppression
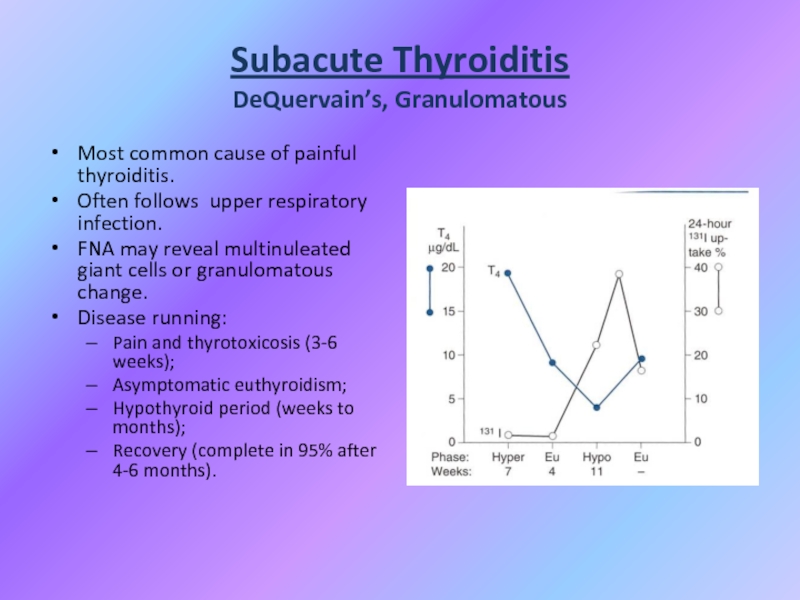
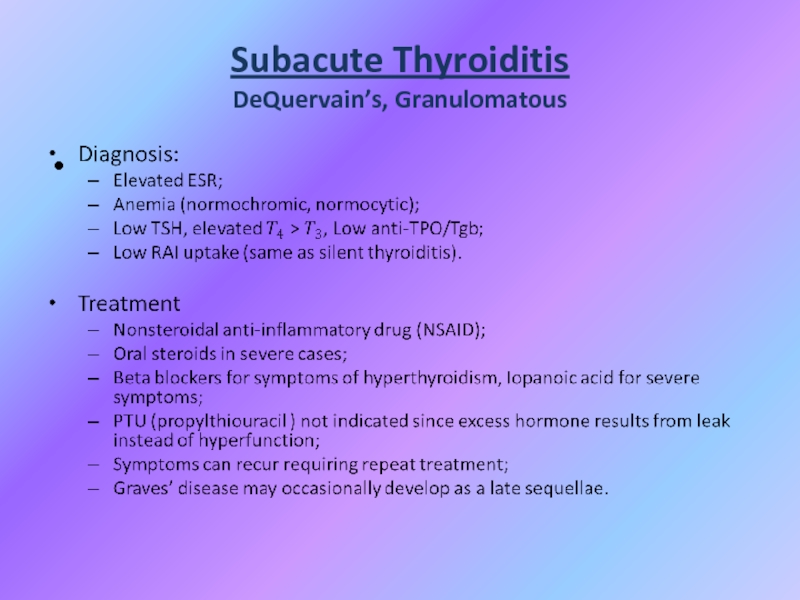
- 85. Subacute Thyroiditis DeQuervain’s, GranulomatousMost common cause of
- 86. Subacute Thyroiditis DeQuervain’s, Granulomatous
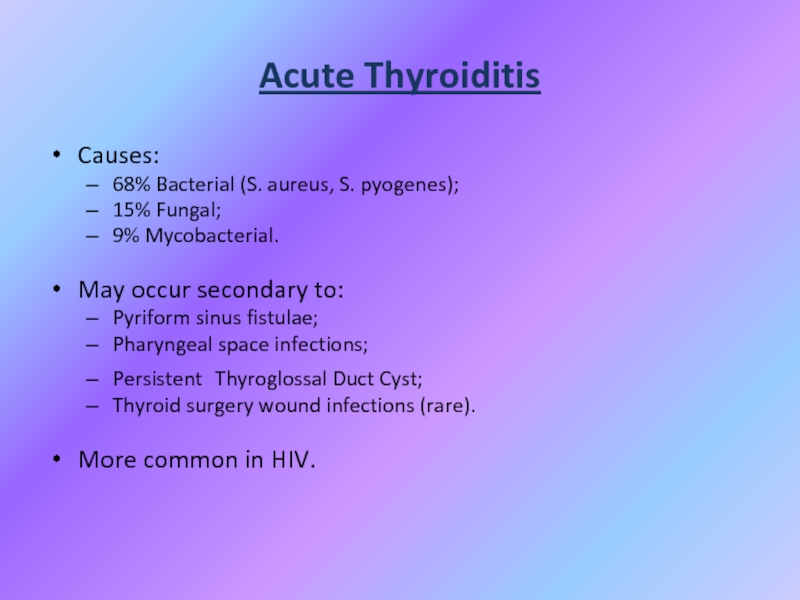
- 87. Acute ThyroiditisCauses:68% Bacterial (S. aureus, S. pyogenes);15%
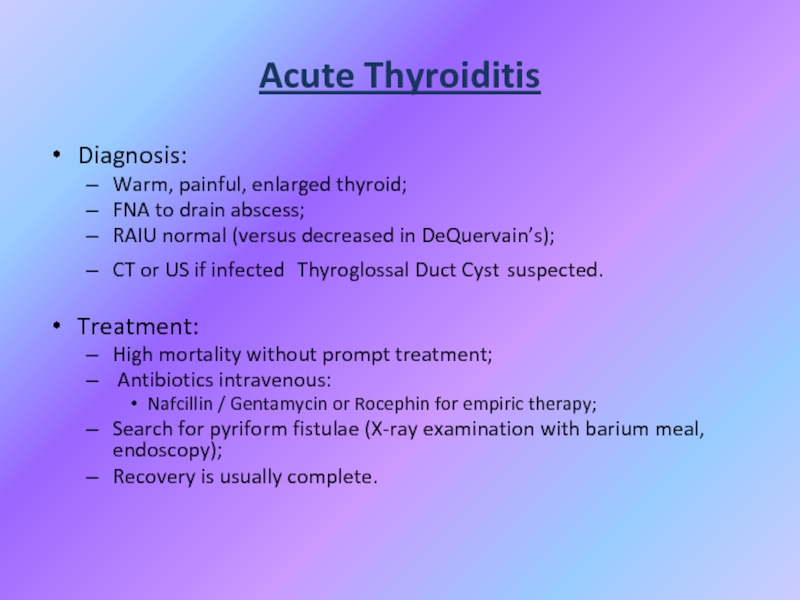
- 88. Acute ThyroiditisDiagnosis:Warm, painful, enlarged thyroid;FNA to drain
- 89. Thank you for listening!!!
- 90. Скачать презентанцию
IntroductionThyroid hormone is essential for the growth and maturation of many target tissues, including the brain and skeleton.As a result, abnormalities of thyroid gland function in infancy and childhood is a
Слайды и текст этой презентации
Слайд 1Thyroid gland diseases
Karazin Kharkiv National University
Department of Pediatrics
Assistant
Tatyana Golovko
Слайд 3Introduction
Thyroid hormone is essential for the growth and maturation of
many target tissues, including the brain and skeleton.
As a result,
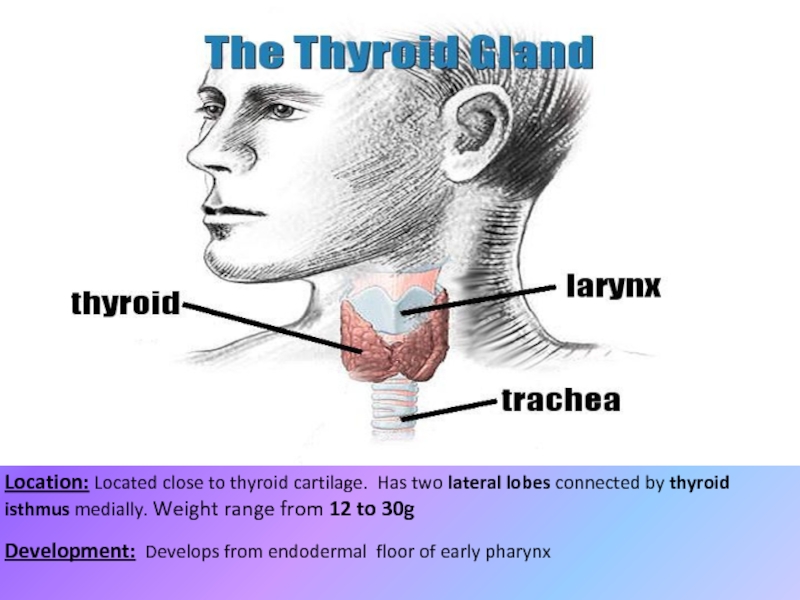
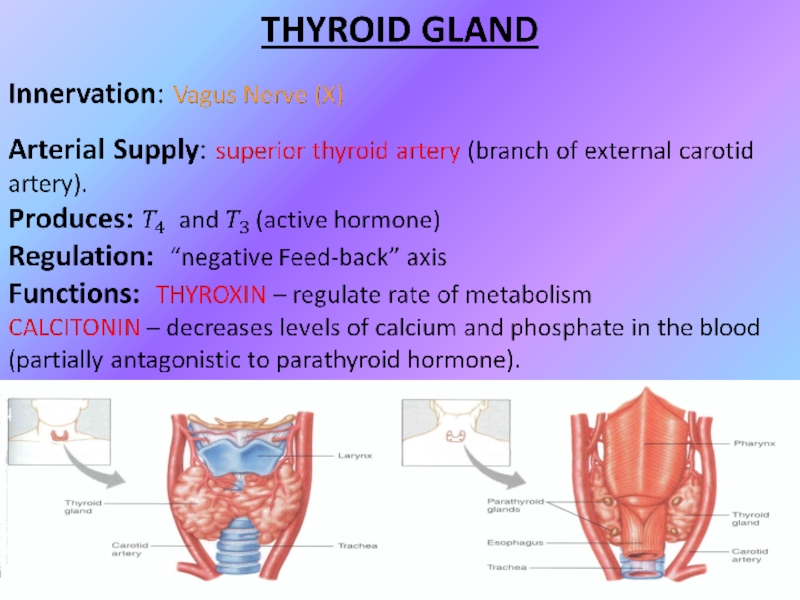
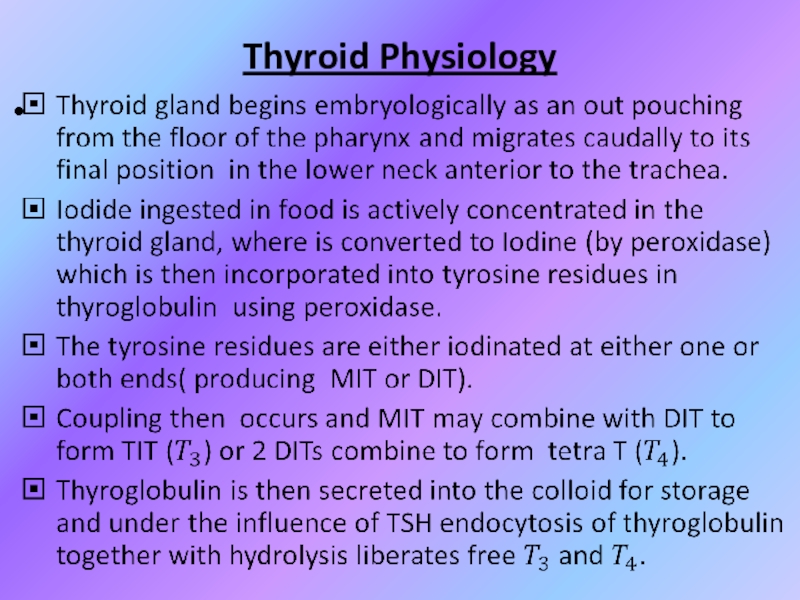
abnormalities of thyroid gland function in infancy and childhood is a result not only in the metabolic consequences of thyroid dysfunction seen in adult patients, but in unique effects on the growth and /or maturation of these thyroid hormone-dependent tissues as well.Слайд 4Location: Located close to thyroid cartilage. Has two lateral lobes
connected by thyroid isthmus medially. Weight range from 12 to
30gDevelopment: Develops from endodermal floor of early pharynx
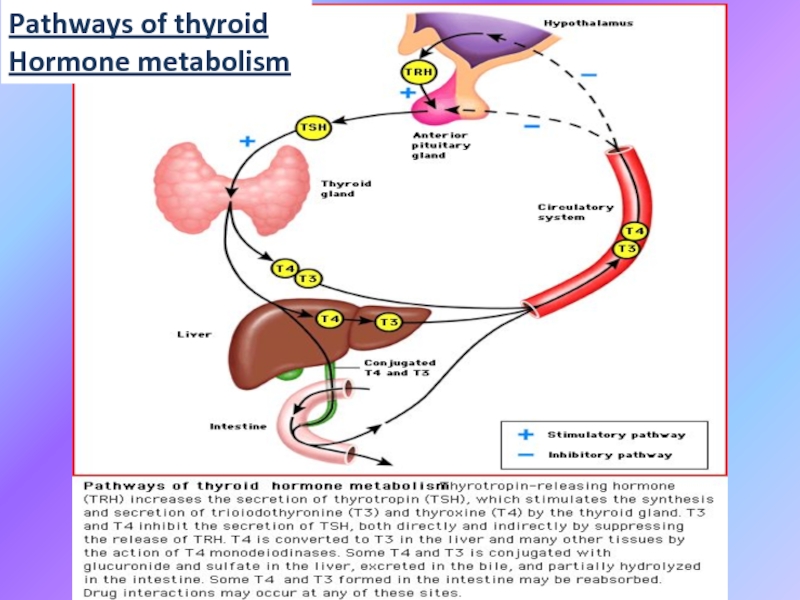
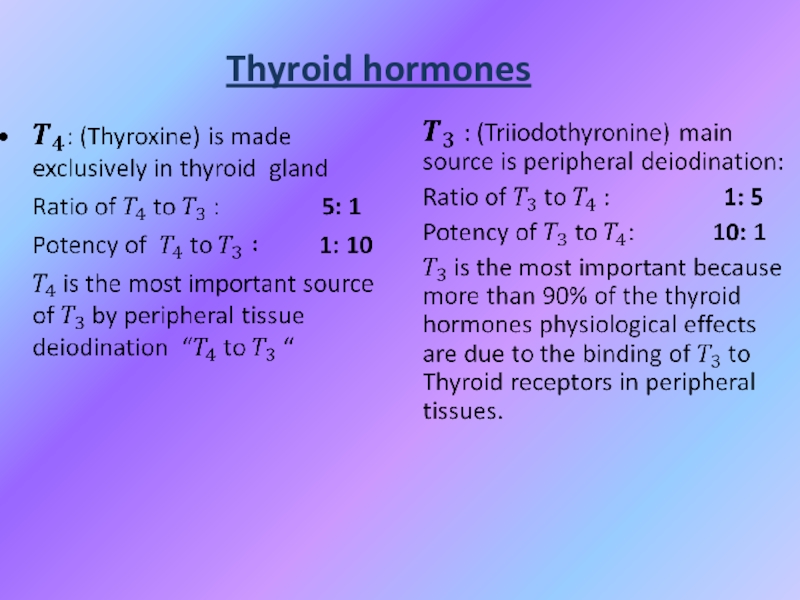
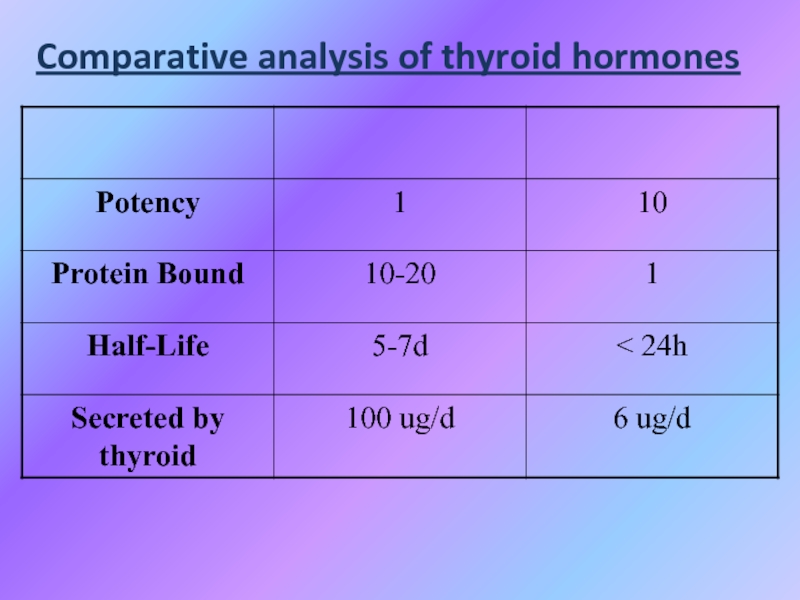
Слайд 12Thyroid Hormone
Majority of circulating hormone is T4 (98,5% T4, 1,5%
T3 )
Total Hormone load is influenced by serum binding
proteins:Albumin 15%;
Thyroid Binding Globulin 70%;
Transthyretin 10%.
Regulation is based on the free component of thyroid hormone.
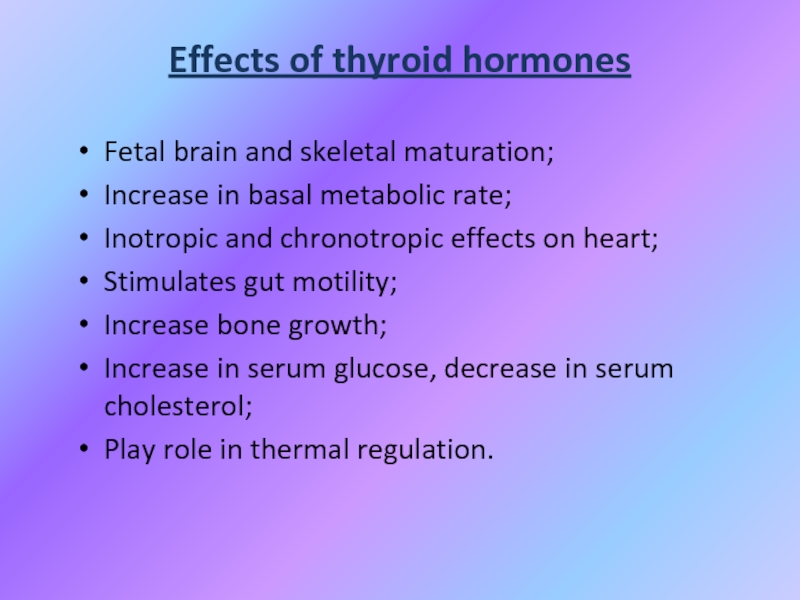
Слайд 13Effects of thyroid hormones
Fetal brain and skeletal maturation;
Increase in basal
metabolic rate;
Inotropic and chronotropic effects on heart;
Stimulates gut motility;
Increase bone
growth;Increase in serum glucose, decrease in serum cholesterol;
Play role in thermal regulation.
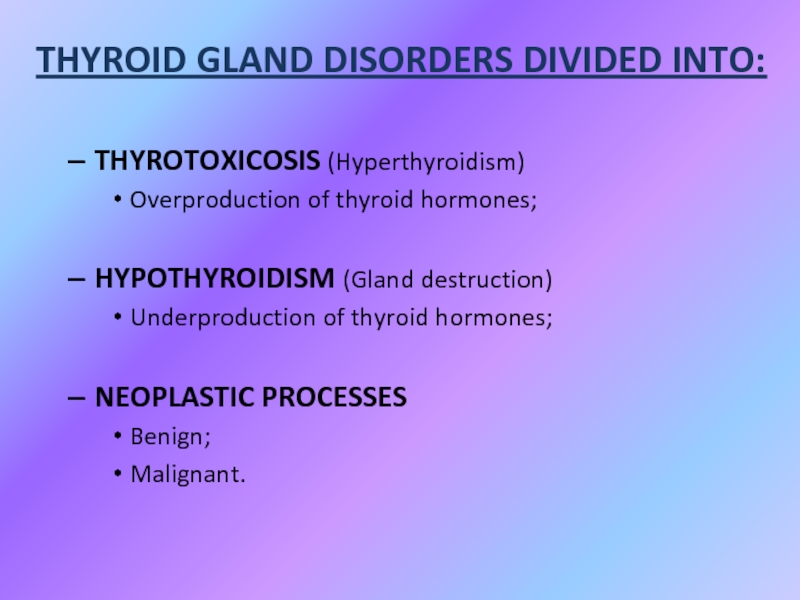
Слайд 16
THYROTOXICOSIS (Hyperthyroidism)
Overproduction of thyroid hormones;
HYPOTHYROIDISM (Gland destruction)
Underproduction of thyroid hormones;
NEOPLASTIC
PROCESSES
Benign;
Malignant.
THYROID GLAND DISORDERS DIVIDED INTO:
Слайд 18LABORATORY EVALUATION
TSH (thyroid-stimulating hormone) normal, practically excludes abnormality
Слайд 19High TSH usually means Hypothyroidism
Rare causes:
TSH-secreting pituitary tumor;
Thyroid hormone resistance;
Assay
artifact.
Low TSH usually indicates Thyrotoxicosis
Other causes:
First trimester of pregnancy;
After treatment
of hyperthyroidism;Some medications (Esteroids-dopamine).
Слайд 21RAIU (Radioactive iodine uptake )
Scintillation counter measures radioactivity after I123
or I131 administration (per os or IV). Radioactivity of TG
measures between 4 h to 24 h. In children is limited in use.Uptake varies greatly by iodine status:
Indigenous diet (normal uptake 10% vs. 90%);
Amiodarone, Contrast study, Topical betadine.
High RAIU with hyperthyroid symptoms
Graves’;
Toxic goitre.
Low RAIU with hyperthyroid symptoms:
Thyroiditis (Subacute, Active Hashimoto’s);
Hormone ingestion (Thyrotoxicosis factitia, Hamburger Thyrotoxicosis);
Excess I- intake in Graves’ (Jod-Basedow effect);
Ectopic thyroid carcinoma (Struma ovarii).
Слайд 23
Thyrotoxicosis
Primary;
Secondary;
Without Hyperthyroidism;
Exogenous or factitious.
Hypothyroidism
Primary;
Secondary;
Peripheral.
Слайд 24HYPERTHYROIDISM or THYROTOXICOSIS:
- is the result of excessive thyroid
gland function because is defined as the state of thyroid
hormone excess.GOITRE
- is a chronic enlargement of the thyroid gland, that is not due to malignant neoplasm.
Слайд 25Primary Hyperthyroidism:
Graves’;
Toxic Multinodular Goitre;
Toxic adenoma;
Functioning thyroid carcinoma metastases;
Activating mutation of
TSH receptor;
Struma ovary;
Drugs: Iodine excess.
Causes of Thyrotoxicosis:
Слайд 26Causes of Thyrotoxicosis:
Thyrotoxicosis without hyperthyroidism:
Subacute thyroiditis;
Silent thyroiditis;
Other causes of thyroid
destruction:
Amiodarone, radiation, infarction of an adenoma;
Exogenous/Factitious.
Secondary Hyperthyroidism:
TSH-secreting pituitary adenoma;
Thyroid hormone
resistance syndrome;Chorionic Gonadotropin-secreting tumor;
Gestational thyrotoxicosis.
Слайд 27Symptoms of Hyperthyroidism
Heat intolerance, dislike of hot weather;
Hyperactivity, irritability, nervousness,
fatigue;
Weight loss (normal to increased appetite);
Diarrhea;
Tremor, palpitations;
Diaphoresis (sweating);
Lid retraction, thyroid
stare;Pretibial myxedema and Graves ophthalmopathy (chemosis, diplopia, and exophthalmos);
Menstrual irregularity;
Goitre;
Tachycardia;
Females are more commonly affected( F:M = 5:1).
Слайд 28Causes of Transient Neonatal Hyperthyroidism
Neonatal hyperthyroidism is almost always transient
and results from the transplacental passage of maternal TSH, receptor
stimulating antibodies.Hyperthyroidism develops only in babies born to mothers with the most potent stimulatory activity in serum.
This corresponds to 1-2% of mothers with Graves ‘ disease, or 1 in 50,000 newborns.
Слайд 29Situations That Should Prompt Consideration of Neonatal
Hyperthyroidism:
● Unexplained tachycardia, goitre
or stare;
● Unexplained petechiae, hyperbilirubinemia, or hepatosplenomegaly;
● There is a
persistently high TSH receptor antibody titer in mother during pregnancy in history;● There is a persistently high requirement for antithyroid medication in mother during pregnancy in history;
● There is a thyroid ablation for hyperthyroidism in mother in history;
● There are previously affected sibling in history.
Слайд 31Therapy of Transient neonatal hyperthyroidism
Treatment is accomplished by maternal administration
of antithyroid medication in fetus.
Till nowadays propylthiouracil (PTU) was
the preferred drug for pregnant women in North America, but current recommendations suggest the use of mercazolilum rather than PTU after the first trimester because of concerns about potential PTU-induced hepatotoxicity.The goals of therapy are to utilize the minimal dosage which is necessary to normalize the fetal heart rate and render the mother euthyroid or slightly hyperthyroid.
Слайд 32Therapy of Transient neonatal hyperthyroidism
In the neonate, treatment is the
follows: either PTU
(5 to10 mg/kg/day) or mercazolilum
(0.5 to 0.7 mg/kg/day) has been used initially in 3 divided doses. If the hyperthyroidism is severe, a strong iodine solution (Lugol’s solution or SSKI, 1 drop every 8 hours) is added to block the release of thyroid hormone immediately.
Often the effect of PTU and mercazolilum is not as delayed in infants as it is in older children or adults.
Слайд 33Therapy of Transient neonatal
hyperthyroidism
Propranolol (2 mg/kg/day in 2 or
3 divided doses) is added if sympathetic overstimulation is severe,
particularly in the presence of pronounced tachycardia.If cardiac failure develops, treatment with digoxin should be initiated, and propranolol should be discontinued.
Rarely, prednisone (2 mg/kg/day) is added for immediate inhibition of thyroid hormone secretion.
Measurement of TSH receptor antibodies in treated babies may be helpful in predicting when antithyroid medication can be safely discontinued.
Lactating mothers on antithyroid medication must continue nursing as long as the dosage of PTU or mercazolilum does not exceed 400 mg or 40 mg respectively.
Слайд 34Permanent neonatal hyperthyroidism
Rarely, neonatal hyperthyroidism is inconvertible and is due
to a germline mutation in the TSH receptor resulting in
its constitutive activation.Function mutation of the TSH receptor should be suspected if persistent neonatal hyperthyroidism occurs in the absence of detectable TSH receptor antibodies in the maternal circulation.
An autosomal dominant inheritance has been noted in many of these infants. Other cases have been sporadic, arising from new mutation.
Слайд 35Permanent neonatal hyperthyroidism
Early recognition is important because the thyroid function
of affected infants is frequently difficult to manage medically, and,
when diagnosis and therapy is delayed, irreversible sequelae, such as cranial synostosis and developmental delay may result.For this reason early, aggressive therapy with either thyroidectomy or even radioablation has been recommended.
Слайд 37Goitre
Endemic goitre:
Areas where > 5% of children 6-12 years old
have goiter
Common in China and central Africa
Sporadic goitre:
Areas where
< 5% of children 6-12 years old have goiterMultinodular goiter in sporadic areas often denotes the presence of multiple nodules rather than gross gland enlargement
Familial.
Слайд 38Goitre
Etiology
Hashimoto’s thyroiditis:
Early stages only, late stages show atrophic changes;
May present
with hypo, hyper or euthyroid states;
Graves’:
Due to chronic stimulation of
TSH receptor;Diet: vegetarian with mainly usage of various types cabbage;
Chronic iodine excess:
iodine excess leads to increased colloid formation and can prevent hormone release;
If a patient does not develop iodine leak, excess iodine can lead to goiter;
Medications:
Lithium prevents release of hormone, causes goiter in 6% of chronic users;
Neoplasm.
Слайд 40Classification of Goitre WHO (1994)
0 – goitre is absent;
I
– goitre isn’t visualized, but it’s size less than distal
phalanx of thumb;II – goitre is palpated and visualized.
Слайд 41Functional condition of Thyroid influence may be as
Euthyroidism;
Hypothyroidism;
Hyperthyroidism.
Слайд 42Non-Toxic Goitre
Cancer screening in non-toxic MNG (Multinodular goitre )
Longstanding MNG
has a risk of malignancy of solitary nodules (
nodules < 1.5 cm may be followed clinically;MNG with non-functioning nodules > 4cm should be excised:
No FNA needed due to poor sensitivity;
Incidence of cancer (up to 40%);
Fine-needle aspiration (FNA) in MNG:
Sensitivity 85% - 95%;
Specificity 95%;
Negative FNA can be followed with annual US (ultrasound);
Insufficient FNA’s should be repeated;
While FNA hyperfunctioning nodules may mimic follicular neoplasm.
Слайд 43Non-Toxic Goitre
Treatment options (no compressive symptoms):
Use follow-up to monitor for
progression;
Thyroid suppression therapy:
May be used for progressive growth;
May reduce gland
volume up to 50%;Goitre regrowth occurs rapidly following therapy cessation.
Surgery indications:
Suspicious neck lymphadenopathy;
There is a radiation to the cervical region in history;
Rapid enlargement of nodules;
Papillary histology;
Microfollicular histology.
Слайд 44Non-Toxic Goitre
Treatment options (compressive symptoms):
Radioactive iodine (RAI) ablation:
Volume reduction 33%
- 66% in 80% of patients
Improvement of dysphagia or dyspnea
in 70% - 90%Post RAI hypothyroidism 60% of patients during 8 years
Post RAI Graves’ disease 10% of patients
Post RAI lifetime cancer risk 1.6% of patients
Surgery treatment apply rare:
Most commonly recommended treatment if conservative treatment noneffective.
Слайд 45Toxic Goitre
Treatment for Toxic MNG:
Thionamide medications:
Not indicated for long-term use
due to complications;
May be used for symptomatic individuals until definitive
treatment.Radioiodine:
Primary treatment for toxic MNG;
Large I131 dose required due to gland size;
Goitre size reduction by 40% within 1 year;
Risk of hypothyroidism 11% - 24%;
May require second dose.
Surgery:
Used for compressive symptoms;
Hypothyroidism occurs in up to 70% of subtotal thyroidectomy patients;
Pre-surgical stabilization with thionamide medications;
Avoid SSKI (Saturated Solution Of Potassium Iodine) due to risk for acute toxic symptoms.
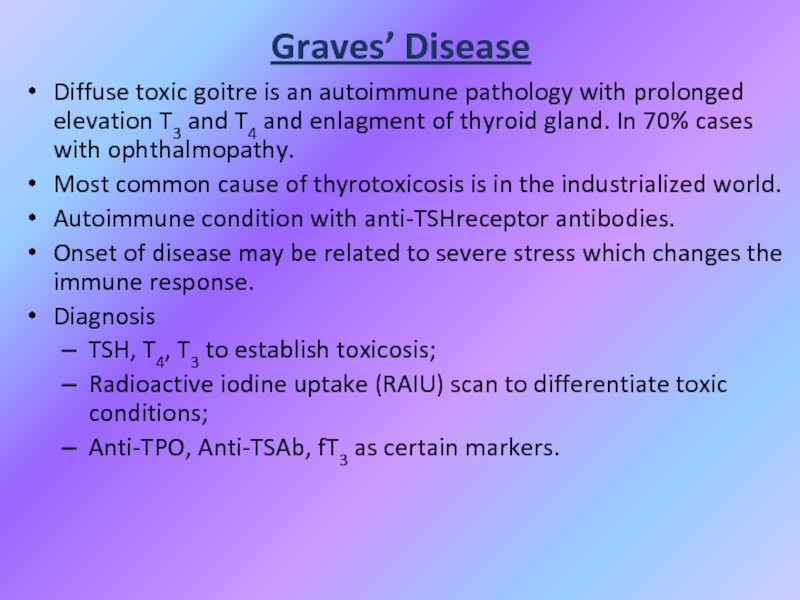
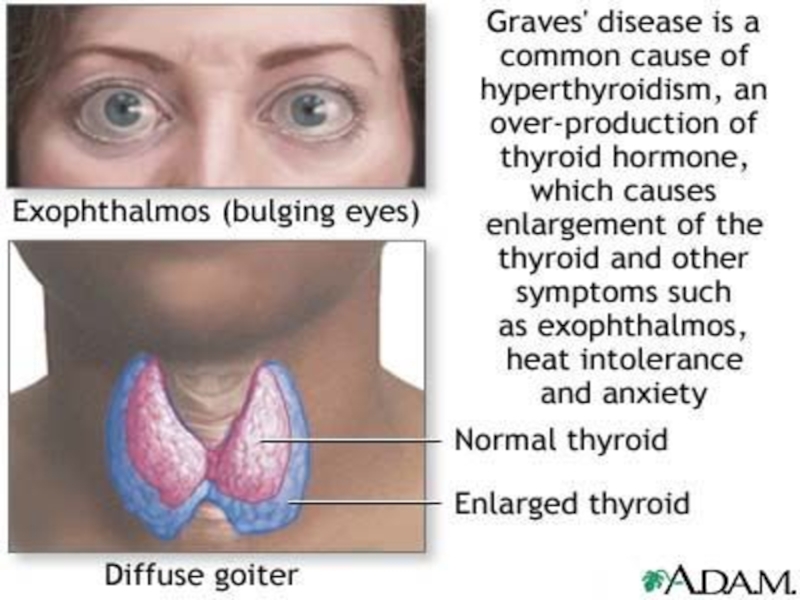
Слайд 46Graves’ Disease
Diffuse toxic goitre is an autoimmune pathology with prolonged
elevation T3 and T4 and enlagment of thyroid gland. In
70% cases with ophthalmopathy.Most common cause of thyrotoxicosis is in the industrialized world.
Autoimmune condition with anti-TSHreceptor antibodies.
Onset of disease may be related to severe stress which changes the immune response.
Diagnosis
TSH, T4, T3 to establish toxicosis;
Radioactive iodine uptake (RAIU) scan to differentiate toxic conditions;
Anti-TPO, Anti-TSAb, fT3 as certain markers.
Слайд 50Graves disease Ophthalmopathy
A feeling of "sandpaper" in the eyes and
discomfort in the eyes;
Retrobulbar pressure or pain;
Eyelid retraction;
Periorbital edema, chemosis,
scleral injection;Proptosis of eyebulb;
Extraocular muscle dysfunction;
Exposure keratitis;
Optic neuropathy.
Слайд 51Graves Disease: Treatment
• Medications:
– Beta-blockers for symptoms – can be
discontinued as thyroid function tests normalize;
– Methimazole (mercazolilum): block and
replace the thyroid hormones;• Surgery;
• Radioactive iodine administer in patients on the shady side of forty;
Concurrent treatment of eye disease.
Слайд 52Нypothyroidism
Hypothyroidism - syndrome with particular or total deficiency of T3,
T4 or their acts to target cells.
Слайд 53Classification of hypothyroidism
PRIMARY - defects of biosynthesis of T3, T4
due
to pathology of thyroid gland.
SECONDARY - decreasing T3, T4
level due todeficiency of TSH (pituitary) or TRH (hypothalamus)
or resistance of receptors for T3, T4 .
Слайд 54Primary:
Autoimmune (Hashimoto´s);
Iatrogenic Surgery or 131I administration;
Drugs: amiodarone, lithium;
Congenital (1 in
3000 to 4000);
Iodine defficiency;
Infiltrative disorders.
Слайд 55
Secondary:
Pituitary gland destruction;
Isolated TSH deficiency;
Bexarotene treatment;
Hypothalamic disorders.
Peripheral:
Rare, familial tendency.
Слайд 59Congenital hypothyroidism
Agenesis (no goiter) or dysgenesis ( aplasia, hypoplasia, ectopic
gland) are the most common causes 85%.
Dyshormonogenesis (10%) and a
goiter will be present. Pendred syndrome with sensorineural deafness is the most common ( often euthyroid).Transplacental maternal TSH receptor blocking Abs (TRBAb) in 5% of cases.
Pituitary failure and maternal administration of toxic substitute for thyroid gland.
Слайд 60Congenital hypothyroidism
Clinical features
Coarse facial features, dry skin, prolonged jaundice, large
fontanelles, posterior fontanell > 1cm, cutis marmorata, bradycardia, hypothermia, hoarse
cry, cold extremities, short stature, possible deafness.Hypotonia, lethargy, poor feeding, constipation, macroglossia, umbilical hernia and edema.
The brain is extremely sensitive to the presence of thyroid hormones from end of pregnancy until the 1st week of life, and if left untreated may result in irreversible mental retardation.
Слайд 63Hypothyroidism Screening in the Newborn
More often the heel stick dried
blood spot on 4th day in term and on 7th
day in preterm is used to examine the T4 level and TSH.Because of the rapid changes in T4 and TSH in the first few days of life, it is important to take into account when the sample is obtained. Some programs check in follow up in 2-4 weeks.
Different criteria must be employed for LBW babies.
Слайд 66DIAGNOSTIC STUDIES IN HYPOTHYROIDISM
Thyroid scan – 99Tc or I123 uptake;
Bone age;
TSH level!!!
Free T4 level – if hypothalamic-pituitary hypothyroidism
suspected;
TBG (Thyroid
Binding Globulin) – if TBG deficiency issuspected;
Anti-thyroid antibodies – if there is thyroiditis in
maternal history.
Слайд 67Biochemical markers of CH
Low serum T4 level and T3 level
with evaluated TSH (primary) level;
T3 –normal, T4 ↓- severe or
longstanding;T4 –normal but TSH is elevated – compensative CH, transient or subclinical hyperthyroidism;
T4 ↓ but TSH normal- congenital TBG-deficiency or hypothalamic-pituitary hypothyroidism.
Слайд 68Biochemical markers of CH
Other:
Elevated serum cholesterol;
Elevated creatinphosphokinase;
Hyponatriemia.
Слайд 69Instrumental data
Slightly decrease heart rate and amplitude of R wave
(ECG);
Increased left ventricular wall thickness, decrease LV chamber size and
decrease cardiac output (EchoCG);Low-amplitude diffuse slowing (EEG).
Слайд 71High TSH and Low T4
Management
Primary Congenital Hypothyroidism
Thyroxine
Tablets
25-50-75 ug
Crush it,
add to
5-10 ml of water
or milk
Normal T4
In 2 wks
(upper
½ of N)Normal TSH
In one month
(lower ½ of N)
Form
Goals
Treatment prevents bone loss, cardiomyopathy, myxedema
Слайд 72Myxedema coma
Reduced level of consciousness, seizures;
Hypotension/shock;
Hypothermia;
Hyponatremia.
Слайд 74PROGNOSIS
If treatment is delayed, physical development can be hurt slightly.
Early treatment is crucial to prevent mental and intellectual retardation.
Early
treatment of pregnant woman with thyroiditis may prevent mental subnormality in her child.Слайд 75Juvenile hypothyroidism
A child with growth retardation, constipation, becomes less sociable,
gain weight; his school performance is deteriorating and he is
intolerant to cold. He may also has goiter.Typical face with dry pale skin and periorbital edema.
Typically no effect on intellect.
Слайд 76Causes of juvenile hypothyroidism
Hashimoto thyroiditis. More common in girls who
may have initial thyrotoxicosis or be euthyroid or hypothyroid.
Hashimoto may
be associated with Down, Turner and Klinefelter syndromes as well as SLE (systemic lupus erythematosus) and other autoimmune disorders.A goiter may be present initially with no clinical features of disturbed thyroid function.
Other causes of JH include administration of goitrogens, iodine deficiency, hypothalamic/pituitary disorders and post thyroidectomy.
Слайд 77JH investigations
Antithyroglobulin and antimicrosomal antibodies are found.
Serum T4 is
low (earlier than T3).
Bone age is delayed.
Treatment is with thyroxine.
Слайд 78ETIOLOGY OF ACQUIRED HYPOTHYROIDISM
Chronic lymphocytic (Hashimoto`s) thyroiditis (CLT);
Subacute thyroiditis (De
Quervain`s);
Goitrogens (iodide, thiouracil, etc.);
Thyroidectomy or ablation following radioactive iodine;
Infiltrative disease
(e.g., cystinosis, histiocytosis X);Systemic disease.
Hypothalamic or pituitary disease;
Congenital thyroid disorders, e.g., ectopia, may not decompensate until later childhood and thus may appear acquired;
Peripheral resistance to thyroid hormones, including receptor defects;
Jatrogenic (propylthiouracil, methimazole, iodides, lithium,amiodarone);
Hemangiomas of the liver.
Слайд 79SYMPTOMS OF ACQUIRED HYPOTHYROIDISM
Slow growth;
Edema;
Decreased appetite;
Constipation;
Swollen thyroid gland;
Lethargy;
Drop in
school performance;
Cold Intolerance;
Short stature;
Delayed dentition;
Myxedema or mildly overweight;
Goiter;
Galactorrhea;
Menometrorrhagia.
Слайд 80SIGNS OF ACQUIRED HYPOTHYROIDISM
Delayed reflex return;
Mental depression;
Pale, thick,
or cool skin;
Muscle pseudohypertrophy;
Delayed puberty or precocious puberty;
Treatment – same
CH.Слайд 81Chronic thyroiditis Hashimoto disease
Clinical presentation:
Painless diffuse goiter;
Goiter with euthyroidism;
Toxic thyroiditis;
Hypothyroidism with or without thyromegaly;
Dysphagia, pain or
pressure sensation in the neck, cough and headache.Слайд 83Diagnosis Hashimoto disease
T4 total and free, serum TSH;
Biopsy;
Antibodies test: antithyroglobulin
antibodies to thyroperoxidase, antimicrosomal test.
Слайд 84Treatment
Levothyroxine if hypothyroid;
Triiodothyronine (for myxedema coma);
Thyroid suppression (levothyroxine) to decrease
goiter size;
Surgery treatment if compression or pain take place.
Слайд 85Subacute Thyroiditis
DeQuervain’s, Granulomatous
Most common cause of painful thyroiditis.
Often follows upper
respiratory infection.
FNA may reveal multinuleated giant cells or granulomatous change.
Disease
running:Pain and thyrotoxicosis (3-6 weeks);
Asymptomatic euthyroidism;
Hypothyroid period (weeks to months);
Recovery (complete in 95% after 4-6 months).
Слайд 87Acute Thyroiditis
Causes:
68% Bacterial (S. aureus, S. pyogenes);
15% Fungal;
9% Mycobacterial.
May occur
secondary to:
Pyriform sinus fistulae;
Pharyngeal space infections;
Persistent Thyroglossal Duct Cyst;
Thyroid
surgery wound infections (rare).More common in HIV.
Слайд 88Acute Thyroiditis
Diagnosis:
Warm, painful, enlarged thyroid;
FNA to drain abscess;
RAIU normal (versus
decreased in DeQuervain’s);
CT or US if infected Thyroglossal Duct Cyst
suspected.Treatment:
High mortality without prompt treatment;
Antibiotics intravenous:
Nafcillin / Gentamycin or Rocephin for empiric therapy;
Search for pyriform fistulae (X-ray examination with barium meal, endoscopy);
Recovery is usually complete.