Слайд 1Viral hepatitis - a large group of infectious diseases with
a primary lesion of the liver, which have similar clinic,
but differ in etiology, pathogenesis, severity and consequences.
In the 5th century BC, Hippocrates described the relationship of jaundice and ascites with liver disease;
1938 - the beginning of the study of viral hepatitis, when the British virologists
D. Findlay and F. McCallum described the outbreak of hepatitis following yellow fever vaccination.
Слайд 2Currently known 8 agents of viral hepatitis
- Hepatitis A virus (HAV) – viral hepatitis A
(VHA)
- Hepatitis E virus (HEV) - viral hepatitis E (VHE)
- Hepatitis B virus (HBV) - viral hepatitis B (VHB)
- Hepatitis C virus (HCV) - viral hepatitis C (VHC)
- Hepatitis D virus (HDV) - viral hepatitis D (VHD)
The most dangerous for the population are VH with
blood-contact and vertical transmission - B, C, D
(because of the high probability of development of chronic forms (in HCV – the highest), liver cirrhosis and hepatocellular carcinoma.
These effects lead to reduced life quality and significant economic loss.
Слайд 3Pathomorphological changes of VH
Mechanism of them is different:
HAV, HCV,
HDV - have a direct cytolytic effect;
HBV – indirectly via
the immune system.
Intoxication
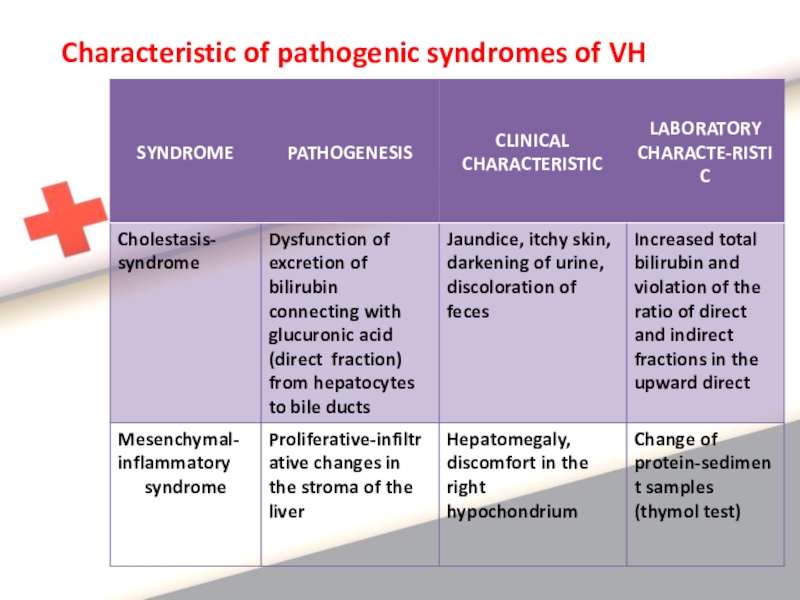
Syndrome of cytolysis of hepatocytes,
Сholestasis syndrome,
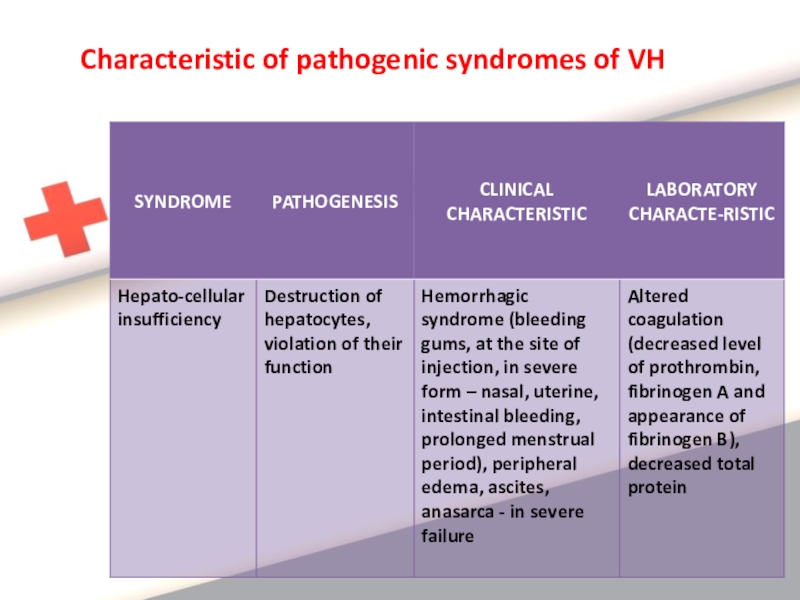
Hepato-cellular insufficiency,
Mesenchymal-inflammatory
syndrome
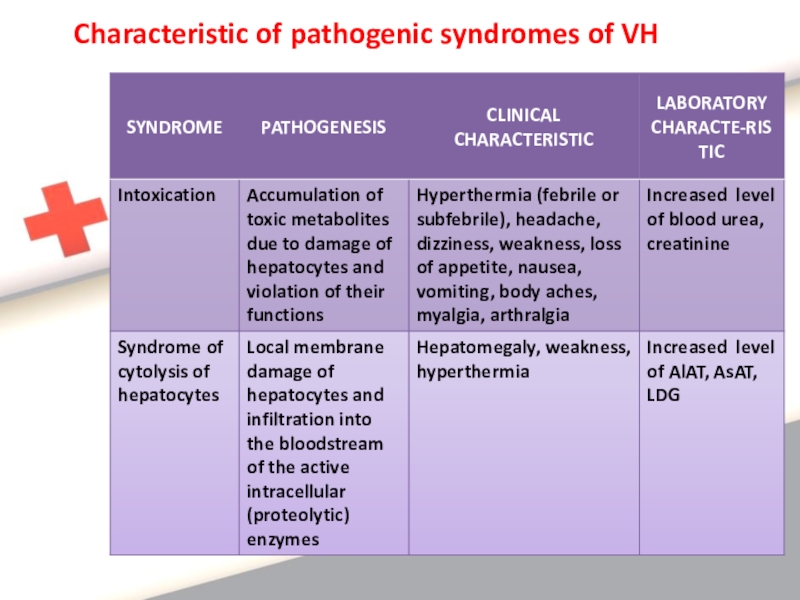
Слайд 4Characteristic of pathogenic syndromes of VH
Слайд 5Characteristic of pathogenic syndromes of VH
Слайд 6Characteristic of pathogenic syndromes of VH
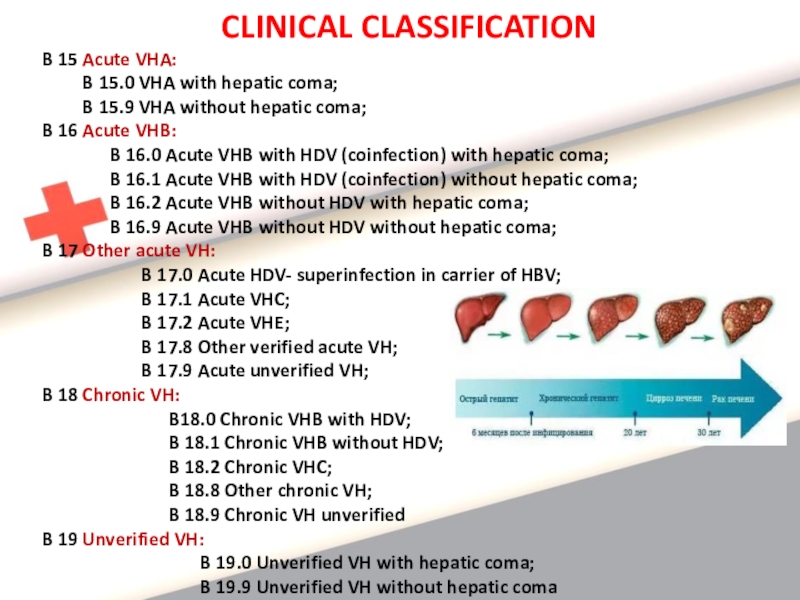
Слайд 7CLINICAL CLASSIFICATION
B 15 Acute VHA:
B
15.0 VHA with hepatic coma;
B
15.9 VHA without hepatic coma;
B 16 Acute VHB:
B 16.0 Acute VHB with HDV (coinfection) with hepatic coma;
B 16.1 Acute VHB with HDV (coinfection) without hepatic coma;
B 16.2 Acute VHB without HDV with hepatic coma;
B 16.9 Acute VHB without HDV without hepatic coma;
B 17 Other acute VH:
B 17.0 Acute HDV- superinfection in carrier of HBV;
B 17.1 Acute VHC;
B 17.2 Acute VHE;
B 17.8 Other verified acute VH;
B 17.9 Acute unverified VH;
B 18 Chronic VH:
B18.0 Chronic VHB with HDV;
B 18.1 Chronic VHB without HDV;
B 18.2 Chronic VHC;
B 18.8 Other chronic VH;
B 18.9 Chronic VH unverified
B 19 Unverified VH:
B 19.0 Unverified VH with hepatic coma;
B 19.9 Unverified VH without hepatic coma
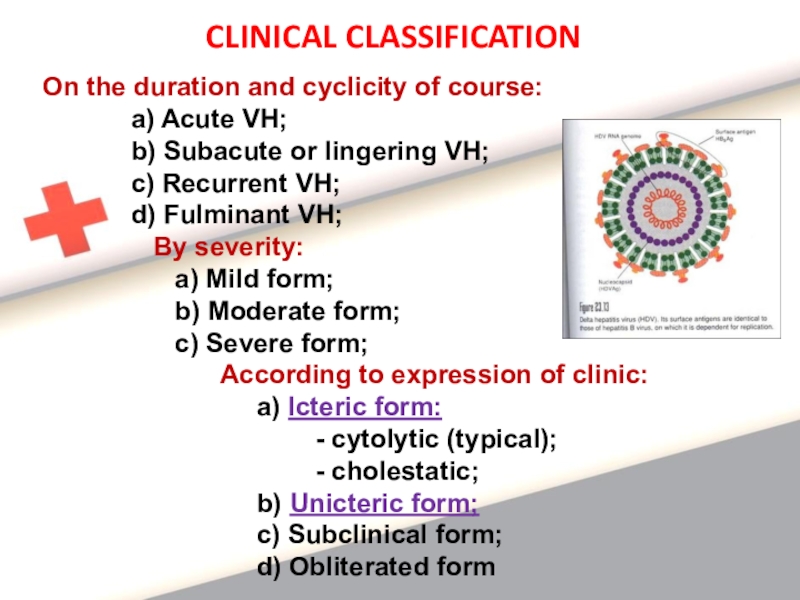
Слайд 8CLINICAL CLASSIFICATION
On the duration and cyclicity of course:
a) Acute VH;
b) Subacute or lingering VH;
c) Recurrent VH;
d) Fulminant VH;
By severity:
a) Mild form;
b) Moderate form;
c) Severe form;
According to expression of clinic:
a) Icteric form:
- cytolytic (typical);
- cholestatic;
b) Unicteric form;
c) Subclinical form;
d) Obliterated form
Слайд 9VIRAL HEPATITIS A
intestinal anthroponotic viral infection with fecal-oral mechanism
of
transmission, characterized by hepatonecrosis, clinicaly – by intoxication, hepatomegaly, sometimes
jaundice.
Etiology:
Hepatovirus, Picornaviridae;
2. Has a rounded shape, a single chain of RNA;
3. Stable in the environment
(for items stored for about 1 month);
4. Not inactivated by stomach acid;
5. Sensitive for the ribavirin, amantadine;
Слайд 10Epidemiology:
Fecal-oral mechanism of transmission:
- watery
route;
- alimentary route;
- contact way (through dirty hands, towels, linen, dishes);
2. Source:
- patient in the incubation, prodromal period and climax of the disease;
- with inapparant, obliterated and unicteric (more dangerous) forms;
- after the appearance of jaundice the risk of infection is reduced;
3. Susceptibility:
- general;
- children (after the first year of life);
- teenagers, young people to 35 years;
- patients with immunosuppression;
4. Seasonality: summer-autumn;
5. Factors: contaminated water, infected food products, household items;
6. Epidemics occur every 4-7 years;
7. Repeated infection is not seen.
Слайд 11Pathogenesis
Damage of hepatocytes due to cell cytotoxic immune reactions and
direct cytopathic effect of the virus.
Main link of pathogenesis
– is biochemical reaction – peroxide oxygenation of lipids, leading to destraction of hepatocyte phospholipids and increased membrane permeability.
Phases:
Penetration of the virus into hepatocytes,
Reproduction
leads to cytolysis and degeneration of cells.
3. Excrection: virus enters from the affected cells via bile in the intestine and excreted with feces.
Слайд 12CLINICAL CHARACTERISTIC
Cyclical disease;
Incubation – asymptomatical, duration 10-50 days,
but on an average 28 days;
at watery and alimentary ways - is shorter, in contact – longer;
3. Initial period – duration 5-7 days:
a) Intoxication: - hyperthermia till 38-39ºC; headache,
weakness;
b) Dyspepsia: - loss of appetite, nausea, vomiting, feeling
of heaviness in the epigastrium and right hypochondrium;
c) Change (darkening) in color of urine;
Initial period of HAV may occur in 3 clinical variants:
- flu-like: - hyperthermia, nasal congestion, discomfort in the oropharynx, coughing,
- dispeptic: - anorexia, nausea, vomiting, stomach pain, diarrhea;
- astheno-vegetative: - general weakness, irritability, indifference, insomnia or drowsiness
Слайд 134. Climax (icteric) period:
a) jaundice:
- with its appearance patient's state is
improved
(additional diagnostic criteria),
- first painted the mucosa of the oropharynx and the sclera,
later - the skin of the trunk, and then extremities,
- continues 2-3 weeks;
- 3 phases: progression (3-4 days), peak (1-2 weeks) and
attenuation (2 weeks);
b) discolored stool, dark urine (dark brown, like root beer
or black tea, foamy);
c) enlarged liver and spleen (palpation is painful, dense liver
tissue);
d) cardiovascular sd: tendency to hypotension, bradycardia
5. Reconvalescence:
a) continues 3-6 month;
b) jaundice disappears gradually;
c) asthenovegetative syndrome.
CLINICAL CHARACTERISTIC
Слайд 14LABORATORY CHARACTERISTIC
Specific methods:
Method of isolation of virus - virological
(detection of the virus in the feces during
initial period),
2. PCR - within 1 week of the disease,
3. Serological confirmation - ELISA
- revealing of anti-HAV IgM (determined in the acute period of the disease), the maximum titer in 2-3 months, persists for 2-6 months,
anti- HAV IgG identified in the lifetime.
Detection of anti-HAV IgM indicates the presence of
a current acute infection;
High titers of anti- HAV IgG confer immunity from
re-infection and indicate the carried VHA
Слайд 15Nonspecific methods:
CBC - leukopenia, neutropenia,
relative
lymphocytosis, normal ESR,
2.Biochemical test of blood:
- increased transaminases (initial period and climax), especially ALT (a marker of cytolysis) - above normal in 3-4 times, reduced in reconvalescence,
- hyperbilirubinemia due to direct fraction in icteric period (indicator of the severity of the disease),
- increased alkaline phosphatase, LDG,
- increased blood urea (sometimes in severe forms),
- coagulogramm - no change,
- urobilinogen - in urine
Слайд 16Complex of clinical-anamnestic data of VHA:
1. Cyclical development,
2.
Presence of prodromal (initial) period,
3.Sequence of development of intoxication,
jaundice
and hepatosplenomegaly,
4. Epidemiologic anamnesis:
- contact with patients with VHA,
- using of unboiled water,
- unhygienic behaviour,
5. Laboratory data:
- hyperbilirubinemia (direct fraction),
- increased transaminases,
- urobilinogen in urine,
- markers – anti-HAV IgM
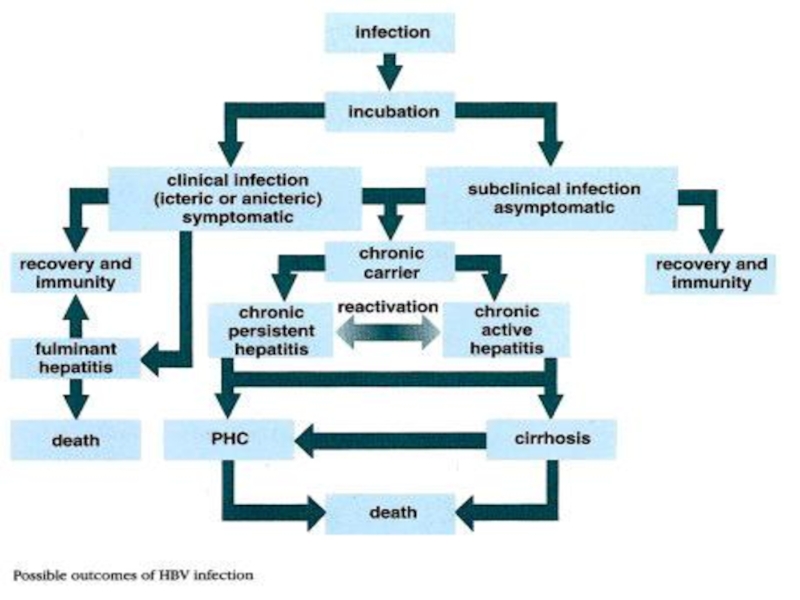
Слайд 17 Viral hepatitis B – mixed viral antroponotic infection from the
group of transfusion hepatitis, characterized by lesions of hepatocytes and
occurring in different clinical forms.
Hepatitis B occurs in chronic, lingering and acute forms.
In 1963 B. Blumberg isolated from the blood of Australian aborigines special "Australian antigen", which is considered a marker of serum hepatitis.
D. Dane (1970) identified a new virus of hepatitis, justifying the existence of new nosological forms - viral hepatitis B.
Слайд 18
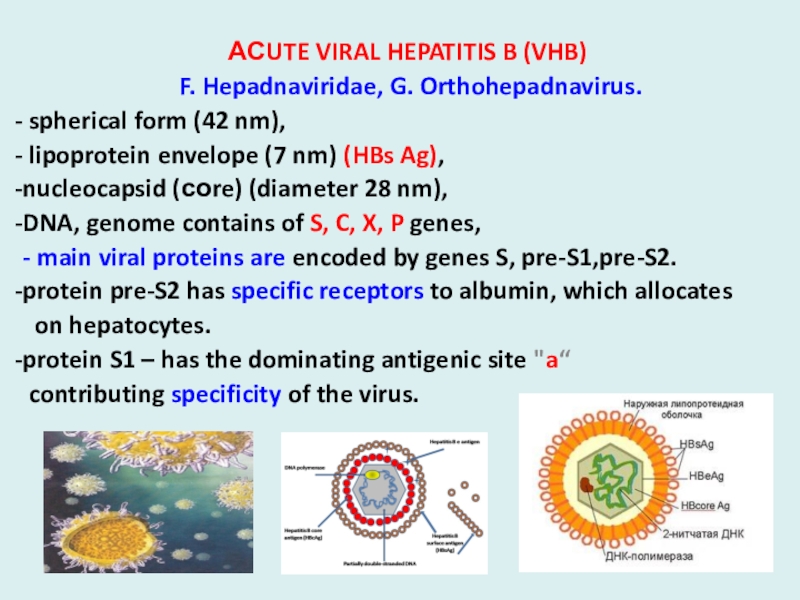
АСUTE VIRAL HEPATITIS B (VHB)
F. Hepadnaviridae, G. Orthohepadnavirus.
spherical
form (42 nm),
lipoprotein envelope (7 nm) (HBs Ag),
nucleocapsid (соre) (diameter 28 nm),
DNA, genome contains of S, C, X, P genes,
- main viral proteins are encoded by genes S, pre-S1,pre-S2.
protein pre-S2 has specific receptors to albumin, which allocates
on hepatocytes.
protein S1 – has the dominating antigenic site "a“
contributing specificity of the virus.
Слайд 19
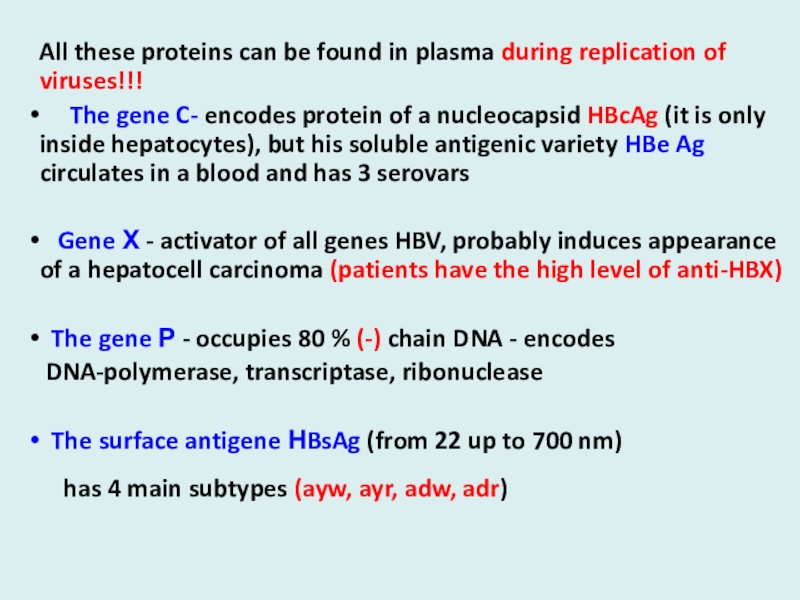
All these proteins can be found in plasma during replication
of viruses!!!
The gene C- encodes protein of
a nucleocapsid HBcAg (it is only inside hepatocytes), but his soluble antigenic variety HBe Ag circulates in a blood and has 3 serovars
Gene Х - activator of all genes HBV, probably induces appearance of a hepatocell carcinoma (patients have the high level of anti-HBX)
The gene Р - occupies 80 % (-) chain DNA - encodes
DNA-polymerase, transcriptase, ribonuclease
The surface antigene НBsAg (from 22 up to 700 nm)
has 4 main subtypes (ayw, ayr, adw, adr)
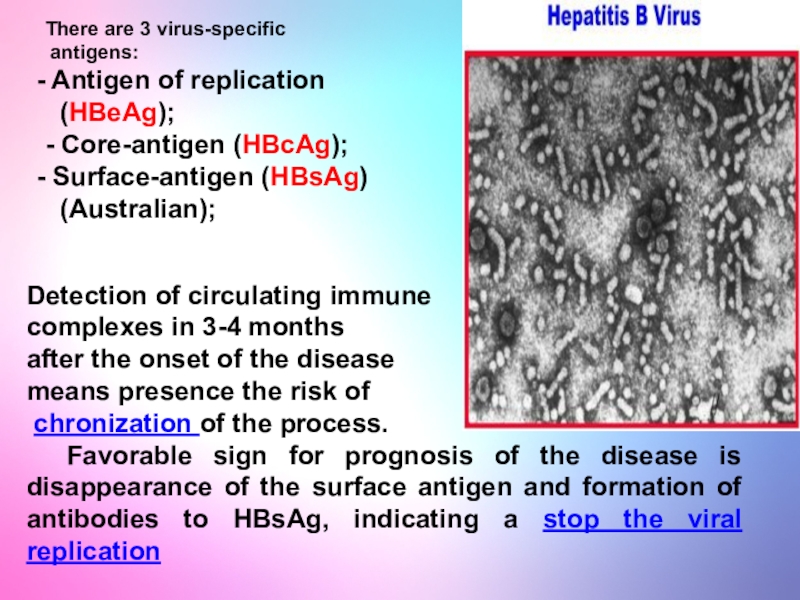
Слайд 20There are 3 virus-specific
antigens:
Antigen of replication
(HBeAg);
- Core-antigen
(HBcAg);
Surface-antigen (HBsAg)
(Australian);
Detection of circulating immune
complexes in 3-4
months
after the onset of the disease
means presence the risk of
chronization of the process.
Favorable sign for prognosis of the disease is disappearance of the surface antigen and formation of antibodies to HBsAg, indicating a stop the viral replication
Слайд 21Stable in the environment,
Can be inactivated:
- At room temperature
- in 6 months
- At 100º C- in 20
minutes
- At 160º C (dry fever) - in 1 hour
- At 120º С) - in 30 minutes
- In plasma- in 25 years
- In a refrigerator - in 6 months
- At рН 2.4 - in 2 hours
- In usual concentrations of disinfectant
solutions – in 2 - 7 days!!!
Слайд 22
EPIDEMIOLODY:
33 % of the population have VHB;
350 -
400 millions of them are the carriers of HBsAg!
(on Russia more then 1 million of carriers !)
Source - human with acute and chronic hepatitis;
- HBsAg-carrier.
Groups of high risk:
- Мedical workers, contacting with a blood
- Recipients of biological tissues
- Patients with often parenteral infusions
- Mentally retarded and looking after staff
- Patients with chronic diseases of a liver
- Children birthing from the mothers – carrier of HBsAg
- Drug addicts and prostitutes
- Homosexuals and persons with HIV-infection
- Inhabitants of hyperendemic by VHB regions
Слайд 23
In Russia– 188, 000 patients with chronic hepatitis and cirrhosis
are annually registered and 6000 of them died!!!
Frequency of revealing of markers of VHB:
- Among medical workers - 33.3 %
- Among the patients with venereal diseases – 49.3 %
- Among the donors of a blood - 14.5 %
- Among the population - 3.8 %
The mode of transmission – PARENTERAL
Modes of transmission:
- sexual (horizontal) - 51.9 %
- intranatal and postnatal (vertical) - 1% - 10% - 50 %
- transplacental - 6 - 10 %
- hemopercutaneus (home contact ) - 6 - 10 %
Слайд 24
Artificial modes of transmission:
- all medical manipulations
with damage of skin and
mucous
- IV drug addicts , tattoo, cosmetic procedures
Infection dose of blood in volume - 0,00004 - 0,000001 ml.
Frequency of newborn infection - 0,02 - 40 %
The risk of chronic HBsAg-carriage:
- at newborn infection - 90 %,
- 1-st year of life - 50 %,
- more than 1-st year 20 %
- in adults - 5 - 10 %
One injection of blood with HBsAg - causes a disease in 90 % of cases.
Hazard after one prick of infectious needle - 34 %
In 50 % of cases the source of infection is not revealed!
Слайд 27
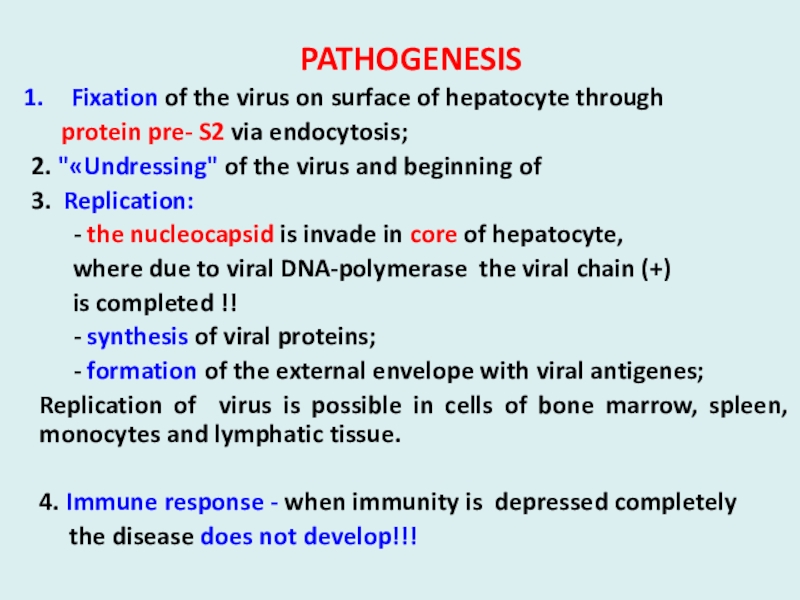
PATHOGENESIS
Fixation of the virus on surface of hepatocyte through
protein pre- S2 via endocytosis;
2. "«Undressing" of the virus
and beginning of
3. Replication:
- the nucleocapsid is invade in core of hepatocyte,
where due to viral DNA-polymerase the viral chain (+)
is completed !!
- synthesis of viral proteins;
- formation of the external envelope with viral antigenes;
Replication of virus is possible in cells of bone marrow, spleen, monocytes and lymphatic tissue.
4. Immune response - when immunity is depressed completely
the disease does not develop!!!
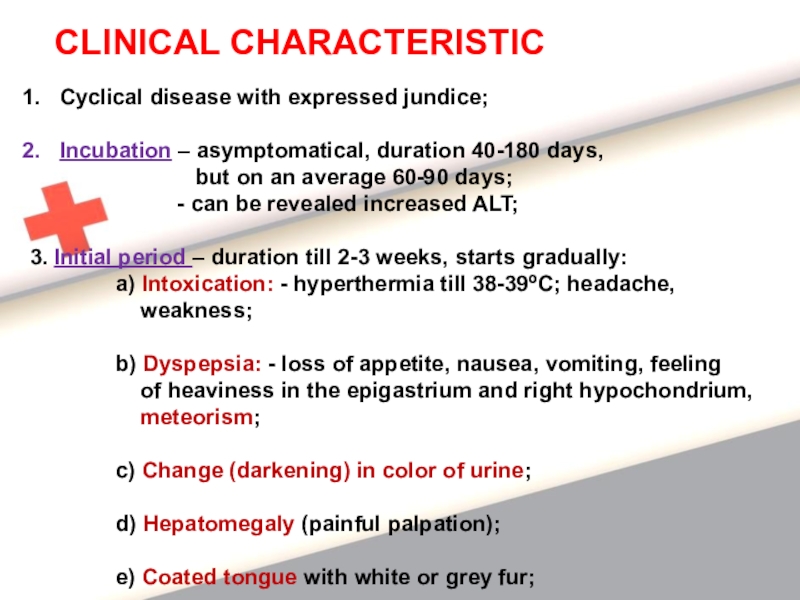
Слайд 29CLINICAL CHARACTERISTIC
Cyclical disease with expressed jundice;
Incubation – asymptomatical, duration 40-180
days,
but on an average 60-90 days;
- can be revealed increased ALT;
3. Initial period – duration till 2-3 weeks, starts gradually:
a) Intoxication: - hyperthermia till 38-39ºC; headache,
weakness;
b) Dyspepsia: - loss of appetite, nausea, vomiting, feeling
of heaviness in the epigastrium and right hypochondrium,
meteorism;
c) Change (darkening) in color of urine;
d) Hepatomegaly (painful palpation);
e) Coated tongue with white or grey fur;
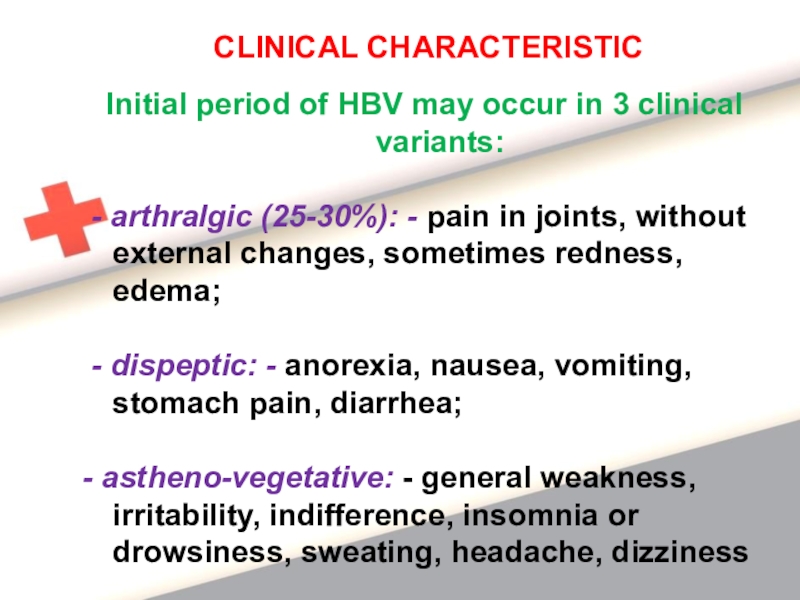
Слайд 30Initial period of HBV may occur in 3 clinical variants:
- arthralgic (25-30%): - pain in joints, without external changes,
sometimes redness, edema;
- dispeptic: - anorexia, nausea, vomiting, stomach pain, diarrhea;
- astheno-vegetative: - general weakness, irritability, indifference, insomnia or drowsiness, sweating, headache, dizziness
CLINICAL CHARACTERISTIC
Слайд 31
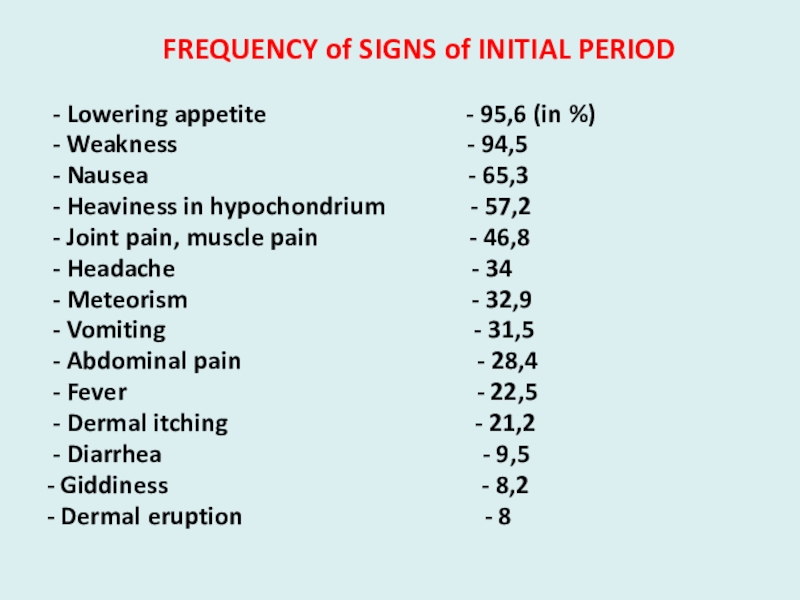
FREQUENCY of SIGNS of INITIAL PERIOD
- Lowering appetite
- 95,6 (in %)
- Weakness - 94,5
- Nausea - 65,3
- Heaviness in hypochondrium - 57,2
- Joint pain, muscle pain - 46,8
- Headache - 34
- Meteorism - 32,9
- Vomiting - 31,5
- Abdominal pain - 28,4
- Fever - 22,5
- Dermal itching - 21,2
- Diarrhea - 9,5
- Giddiness - 8,2
- Dermal eruption - 8
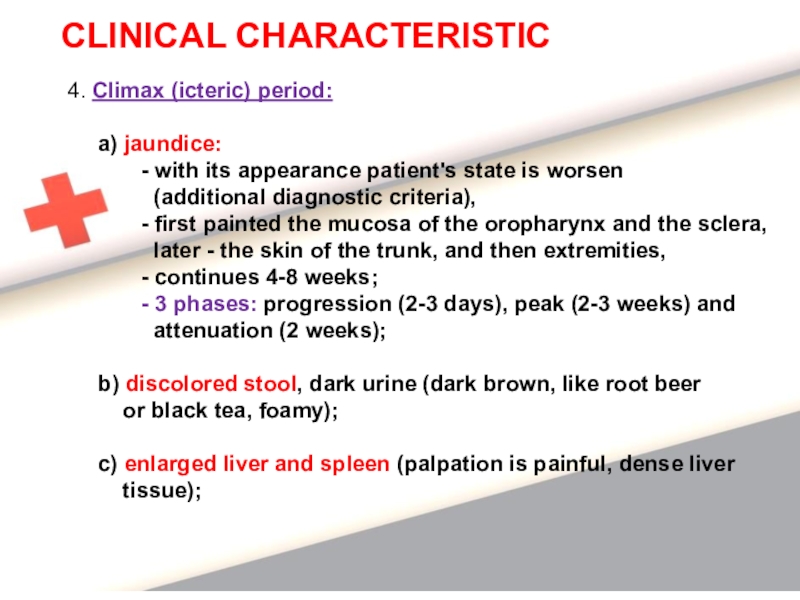
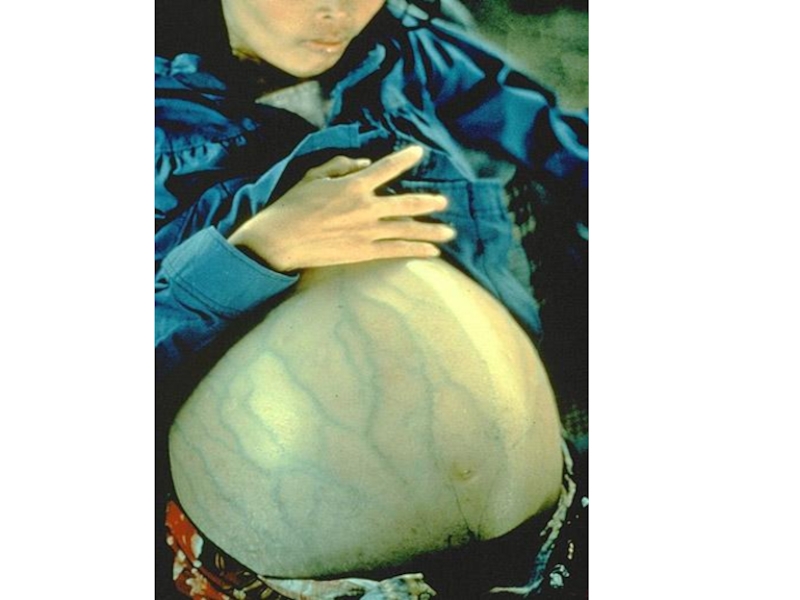
Слайд 334. Climax (icteric) period:
a) jaundice:
- with its appearance patient's state is
worsen
(additional diagnostic criteria),
- first painted the mucosa of the oropharynx and the sclera,
later - the skin of the trunk, and then extremities,
- continues 4-8 weeks;
- 3 phases: progression (2-3 days), peak (2-3 weeks) and
attenuation (2 weeks);
b) discolored stool, dark urine (dark brown, like root beer
or black tea, foamy);
c) enlarged liver and spleen (palpation is painful, dense liver
tissue);
CLINICAL CHARACTERISTIC
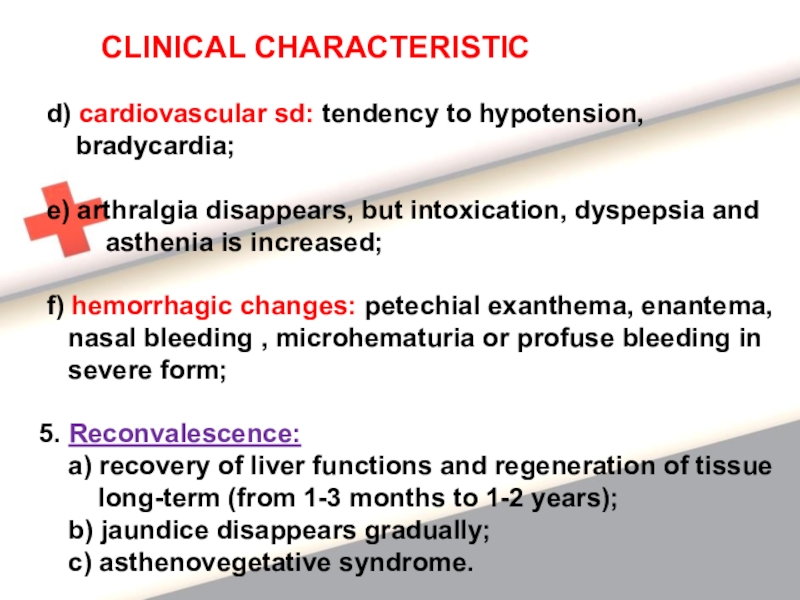
Слайд 34 d) cardiovascular sd: tendency to hypotension,
bradycardia;
e) arthralgia disappears, but intoxication, dyspepsia and
asthenia is increased;
f) hemorrhagic changes: petechial exanthema, enantema,
nasal bleeding , microhematuria or profuse bleeding in
severe form;
5. Reconvalescence:
a) recovery of liver functions and regeneration of tissue
long-term (from 1-3 months to 1-2 years);
b) jaundice disappears gradually;
c) asthenovegetative syndrome.
CLINICAL CHARACTERISTIC
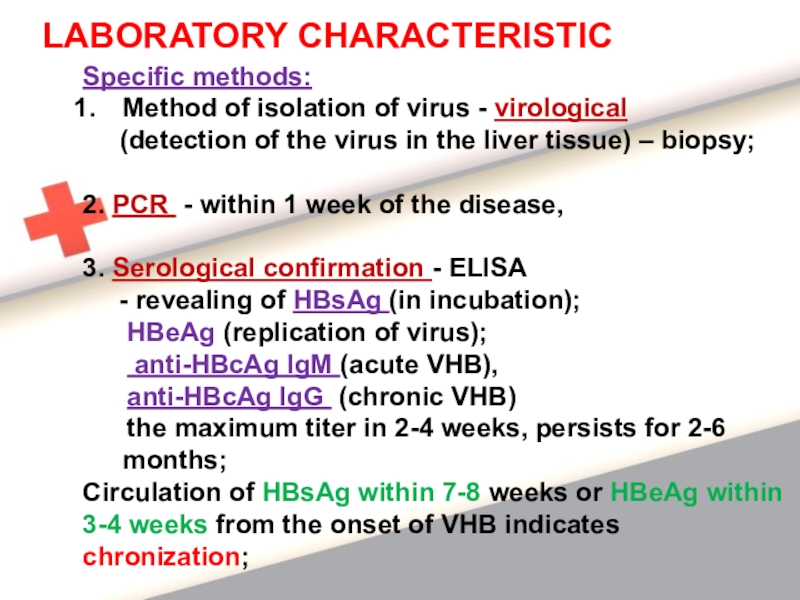
Слайд 37LABORATORY CHARACTERISTIC
Specific methods:
Method of isolation of virus - virological
(detection of the virus in the liver tissue)
– biopsy;
2. PCR - within 1 week of the disease,
3. Serological confirmation - ELISA
- revealing of HBsAg (in incubation);
HBeAg (replication of virus);
anti-HBcAg IgM (acute VHB),
anti-HBcAg IgG (chronic VHB)
the maximum titer in 2-4 weeks, persists for 2-6 months;
Circulation of HBsAg within 7-8 weeks or HBeAg within
3-4 weeks from the onset of VHB indicates
chronization;
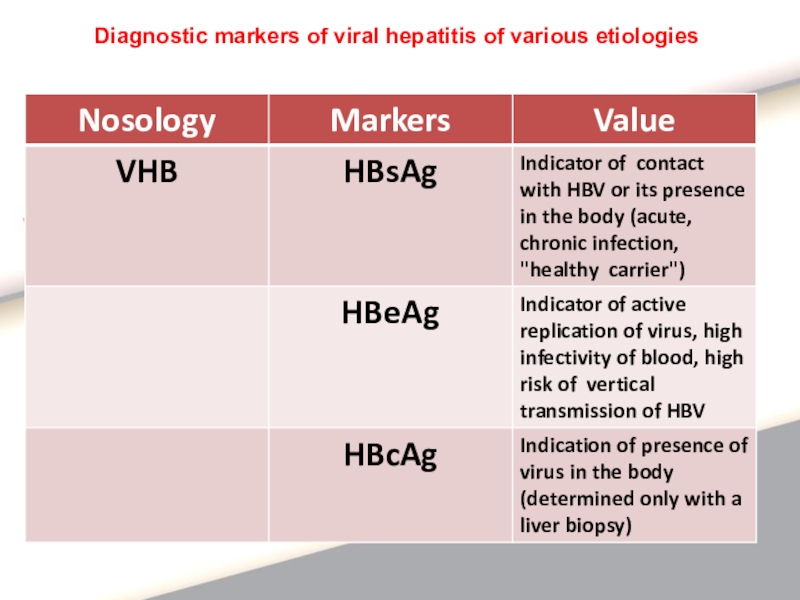
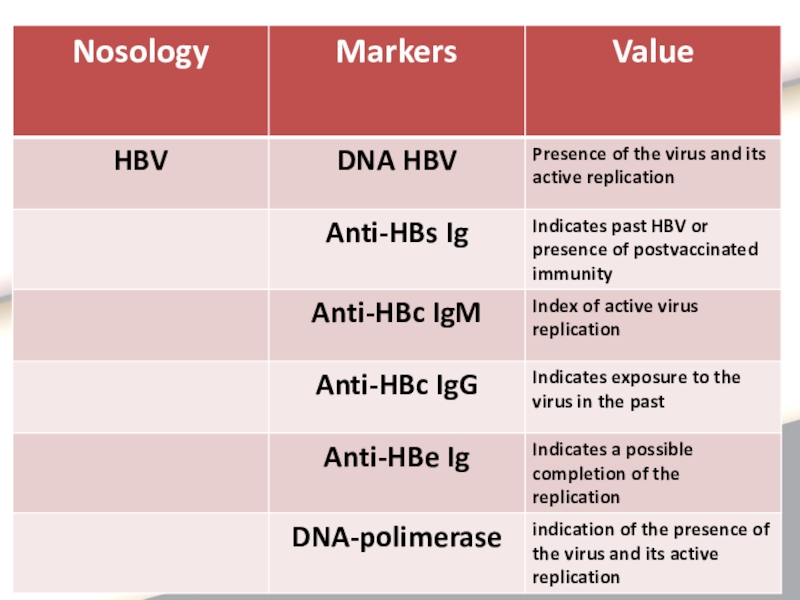
Слайд 38Diagnostic markers of viral hepatitis of various etiologies
Слайд 40Nonspecific methods:
CBC – leukopenia or normocytosis, neutropenia,
lymphocytosis, decreased platelets,
increased ESR;
2.Biochemical test of blood:
- increased transaminases (initial period and climax), ALT, AST (markers of cytolysis) - above normal in 3-4 times, reduced in reconvalescence,
- hyperbilirubinemia due to direct fraction in icteric period (indicator of the severity of the disease),
- increased significantly alkaline phosphatase, LDG,
- increased blood urea (sometimes in severe forms),
- coagulogramm - no change,
- urobilinogen - in urine
Слайд 41Diagnosis of VHB is based on a combination of factors:
Cyclical
development,
2. Presence of prodromal (initial) period,
3. Sequence of
development of severe intoxication,
jaundice and hepatosplenomegaly,
4. Hemorrhagic sd;
5. Laboratory data:
- hyperbilirubinemia (direct fraction),
- increased transaminases, Aph,
- urobilinogen in urine,
- markers – HBsAg, HBeAg, anti-HBsAg IgM,
anti-HBeAg IgM, anti-HBcAg IgM
Слайд 426. Epidemiologic anamnesis:
- blood transfusion,
- surgical and dental treatment,
tattooing,
manicure, pedicure for the
last 6-8 months,
- unknown sexual contact,
- intravenous drug use,
- homosexuality, prostitution,
- sexual contact with a carrier of HBsAg,
- the mother carrier of HBsAg
Diagnosis of VHB is based on a combination of factors:
Слайд 43Principles of treatment of viral hepatitis
Purpose - reducing the physical,
emotional and dietary stress;
2. Etiotropic antiviral therapy – is not
assigned,
only at tendency of chronization;
3. Obligatory hospitalization and isolation of the
patient;
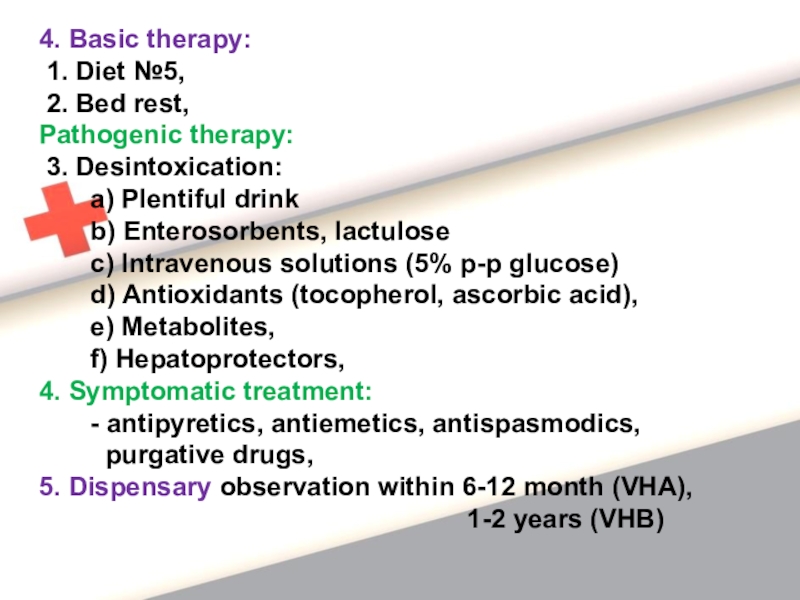
Слайд 444. Basic therapy:
1. Diet №5,
2. Bed rest,
Pathogenic therapy:
3. Desintoxication:
a) Plentiful drink
b) Enterosorbents, lactulose
c) Intravenous solutions (5% p-p glucose)
d) Antioxidants (tocopherol, ascorbic acid),
e) Metabolites,
f) Hepatoprotectors,
4. Symptomatic treatment:
- antipyretics, antiemetics, antispasmodics,
purgative drugs,
5. Dispensary observation within 6-12 month (VHA),
1-2 years (VHB)
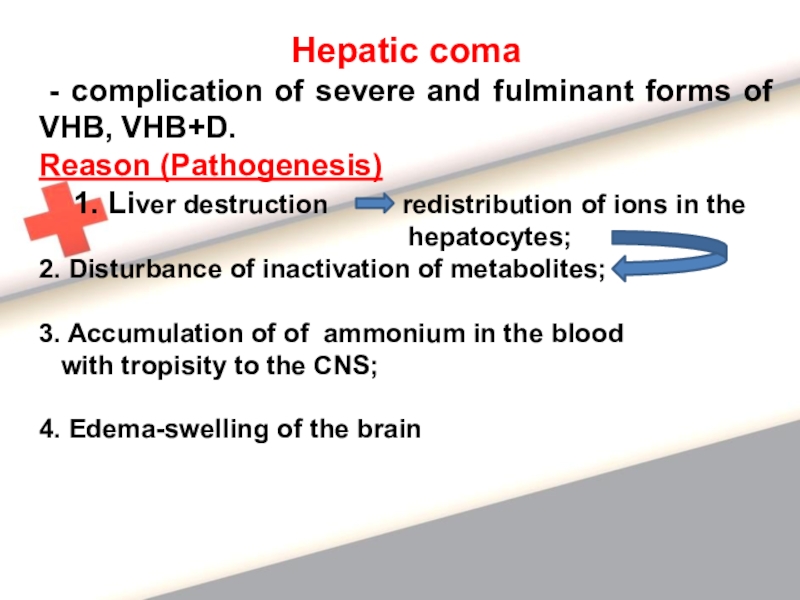
Слайд 45Hepatic coma
- complication of severe and fulminant forms of
VHB, VHB+D.
Reason (Pathogenesis)
1. Liver destruction
redistribution of ions in the
hepatocytes;
2. Disturbance of inactivation of metabolites;
3. Accumulation of of ammonium in the blood
with tropisity to the CNS;
4. Edema-swelling of the brain
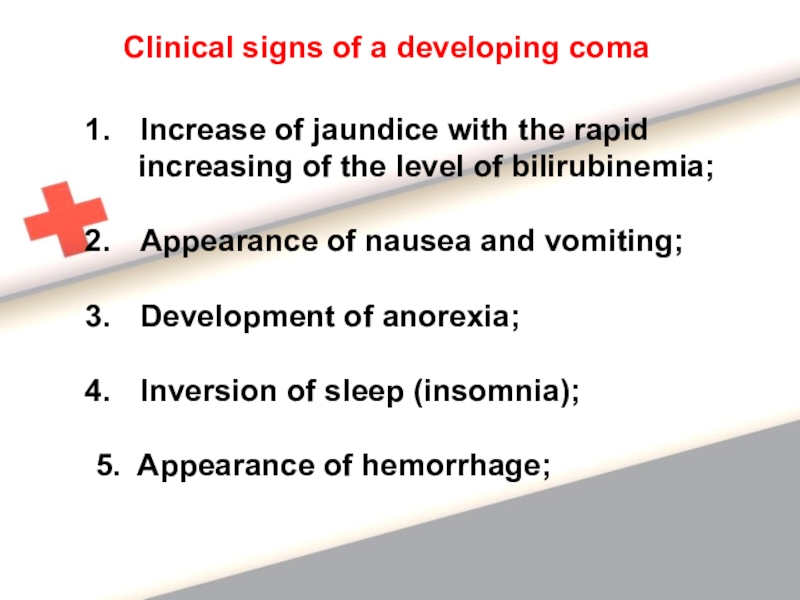
Слайд 46Clinical signs of a developing coma
Increase of jaundice with the
rapid
increasing of the level of bilirubinemia;
Appearance of
nausea and vomiting;
Development of anorexia;
Inversion of sleep (insomnia);
5. Appearance of hemorrhage;