Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
ANGINA PECTORIS
Содержание
- 1. ANGINA PECTORIS
- 2. Sudden coronary deathAngina pectoris Acute myocardial infarctionPainless
- 3. Ischaemic heart disease . Anterior Heart ArteriesThe
- 4. Ischaemic heart disease . Posterior Heart ArteriesThe
- 5. Ischaemic heart diseaseIschaemic heart disease (Coronary artery
- 6. ANGINA PECTORIS-DEFINITIONAngina pectoris is
- 7. ANGINA PECTORIS-DEFINITION Angina pectoris is the medical
- 8. Слайд 8
- 9. RISK FACTORSNonmodifable :Age (> 45 )Male genderFamily
- 10. Слайд 10
- 11. Слайд 11
- 12. Слайд 12
- 13. Слайд 13
- 14. Identifying ischaemic cardiac chest painIschaemic cardiac chest
- 15. Слайд 15
- 16. Слайд 16
- 17. Слайд 17
- 18. Слайд 18
- 19. Слайд 19
- 20. CLASSIFICATIONTypes of Angina Pectoris Stable AnginaUnstable Angina Prinzmetal’s or variant angina Microvascular angina
- 21. Слайд 21
- 22. Сanadian Cardiovascular SocietyFunctional classification of AnginaССS separates
- 23. Сanadian Cardiovascular SocietyFunctional classification of Angina 3
- 24. Слайд 24
- 25. Слайд 25
- 26. Unstable angina New onset angina pectoris –
- 27. Stable anginaFixed stenosisDemand-led ischaemiaRelated to effotPredictableSymptoms over
- 28. Слайд 28
- 29. Слайд 29
- 30. Coronary Syndrome X Characterized by 3 specific,
- 31. Terminology Clarification One major association between microvascular
- 32. Diabetes and Angina Insulin resistance and secondary
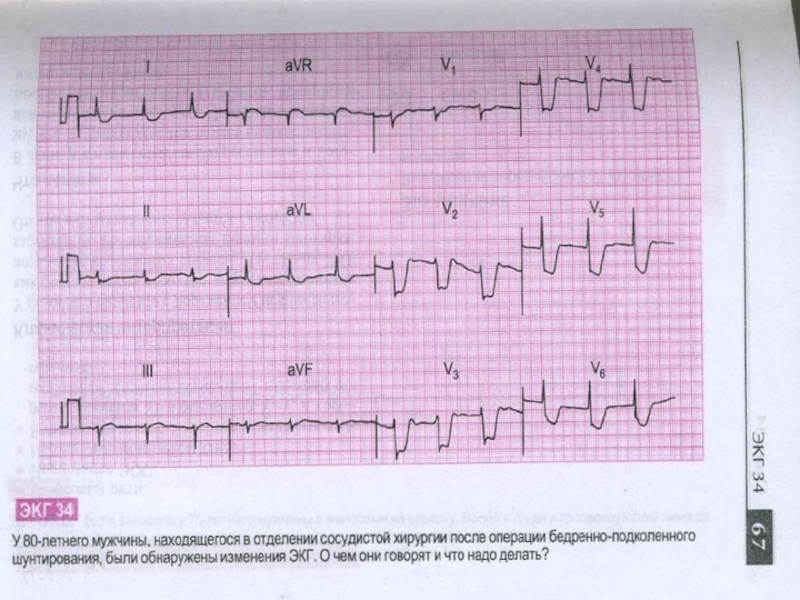
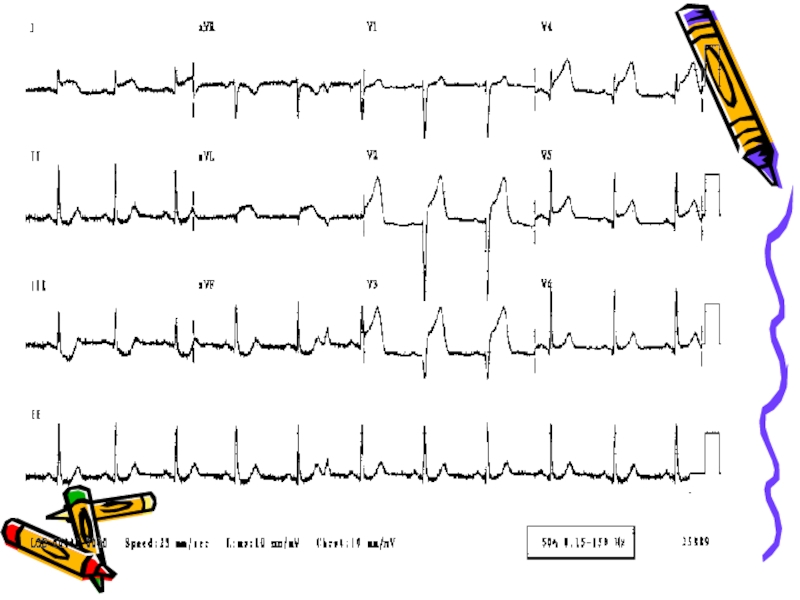
- 33. Diagnosis The diagnosis of angina pectoris
- 34. Laboratory investigationsObligatory indicators: Hb, Total Cholesterol,
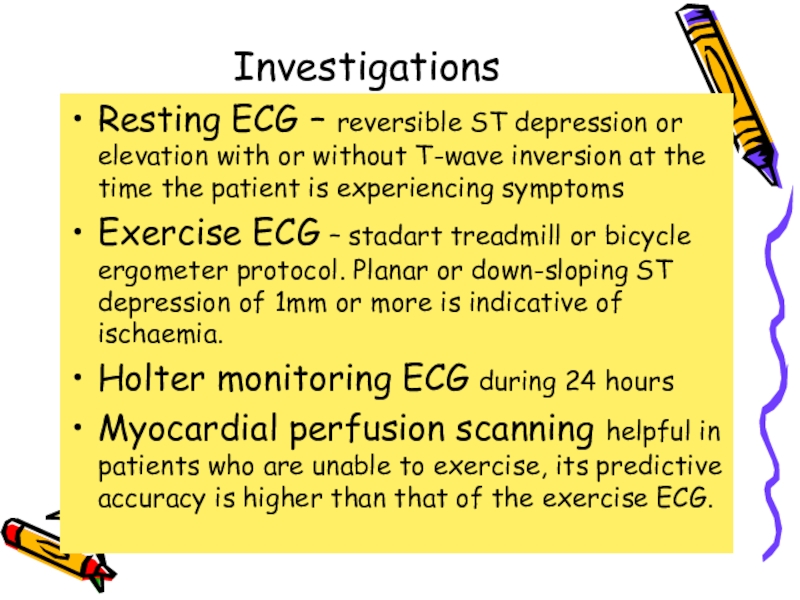
- 35. InvestigationsResting ECG – reversible ST depression or
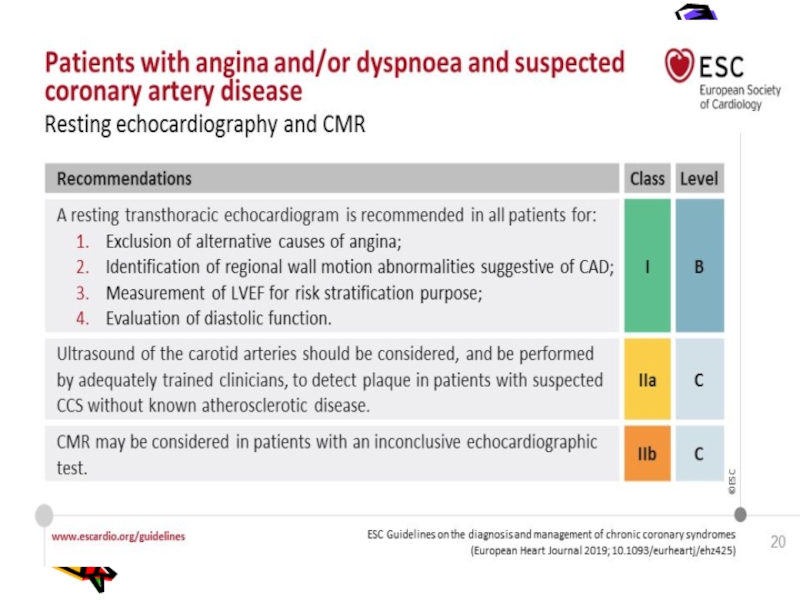
- 36. InvestigationsStress echocardiography – to identify ischaemic segments
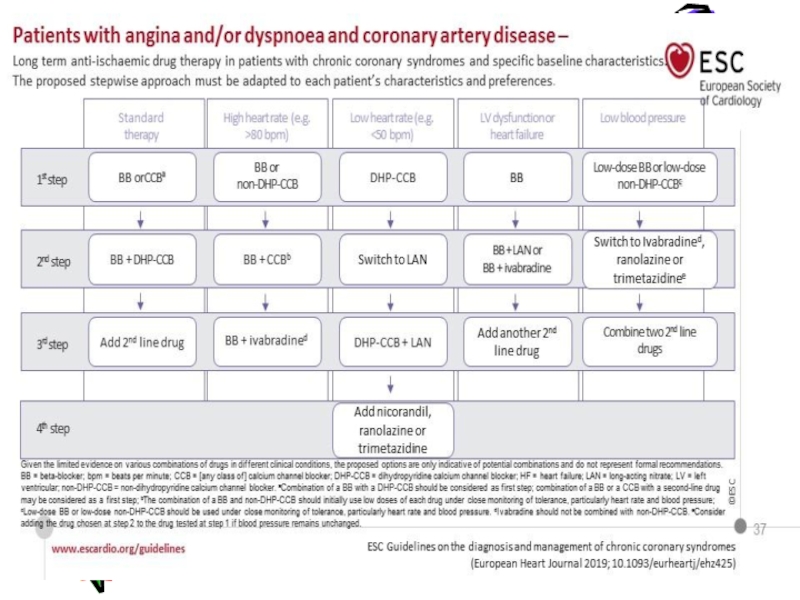
- 37. Слайд 37
- 38. Слайд 38
- 39. Слайд 39
- 40. Слайд 40
- 41. ManagementThe management of angina pectoris involves :A
- 42. Слайд 42
- 43. Слайд 43
- 44. Слайд 44
- 45. Слайд 45
- 46. TreatmentNitroglycerin is the drug most often used.
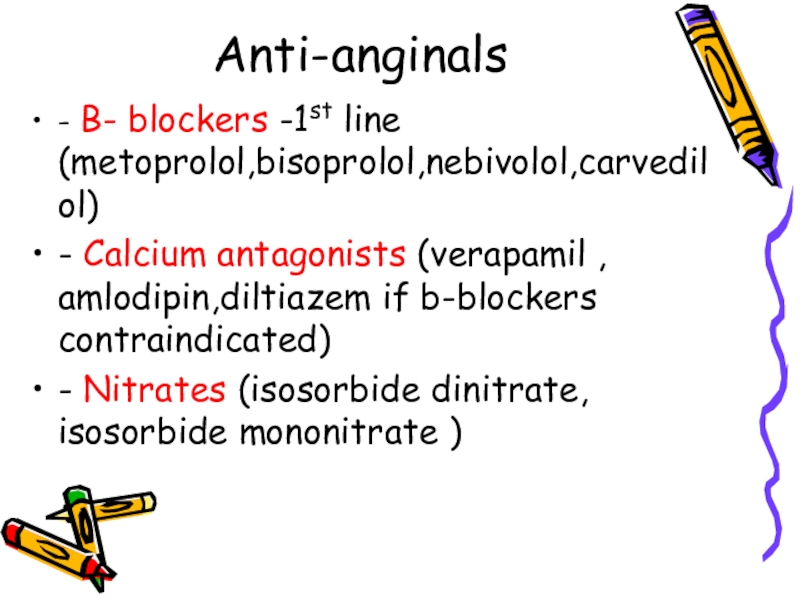
- 47. Anti-anginals- B- blockers -1st line (metoprolol,bisoprolol,nebivolol,carvedilol)- Calcium
- 48. TreatmentANTI-ANGINAL DRUG TREATMENT – GROUPS OF
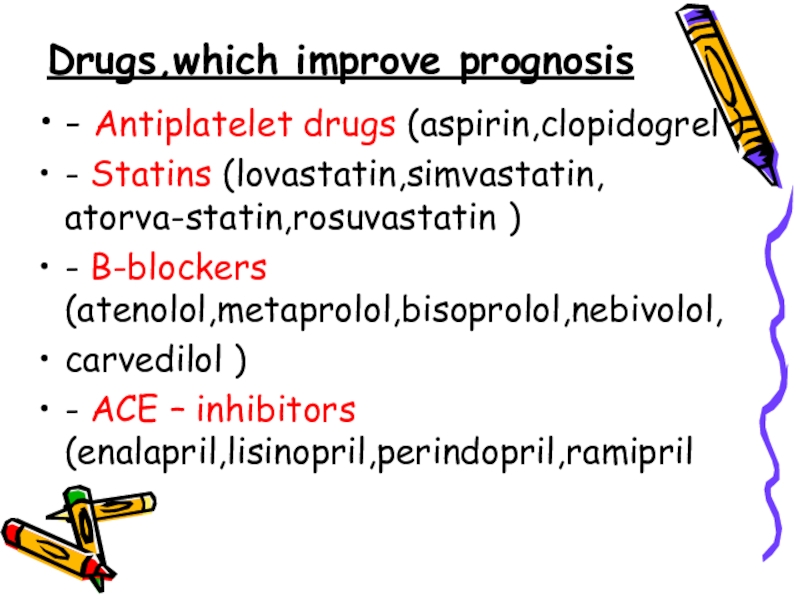
- 49. Drugs,which improve prognosis- Antiplatelet drugs (aspirin,clopidogrel )-
- 50. Treatment Controlling the risk factors for
- 51. What procedures are used to treat angina?Invasive
- 52. Coronary artery bypass graft surgery is also
- 53. How is variant angina or Prinzmetal's angina
- 54. Medical TreatmentIf you have come to the
- 55. Medical TreatmentRegardless of where you are sent,
- 56. Слайд 56
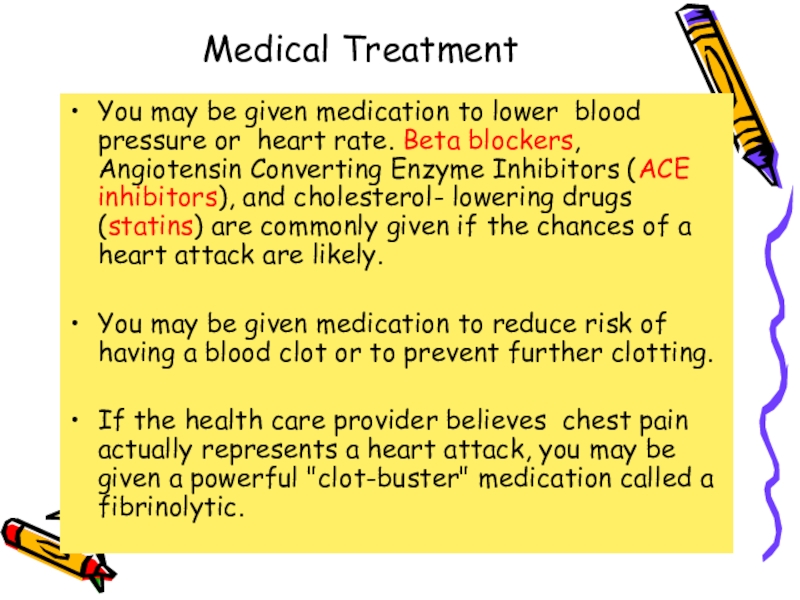
- 57. Medical TreatmentYou may be given medication to
- 58. Metabolic therapy- Trimetazidine (preductal)- Riboxin- Mildronate (vasonate)- Tiotriozaline- Vitamins- Antioxidantes
- 59. Слайд 59
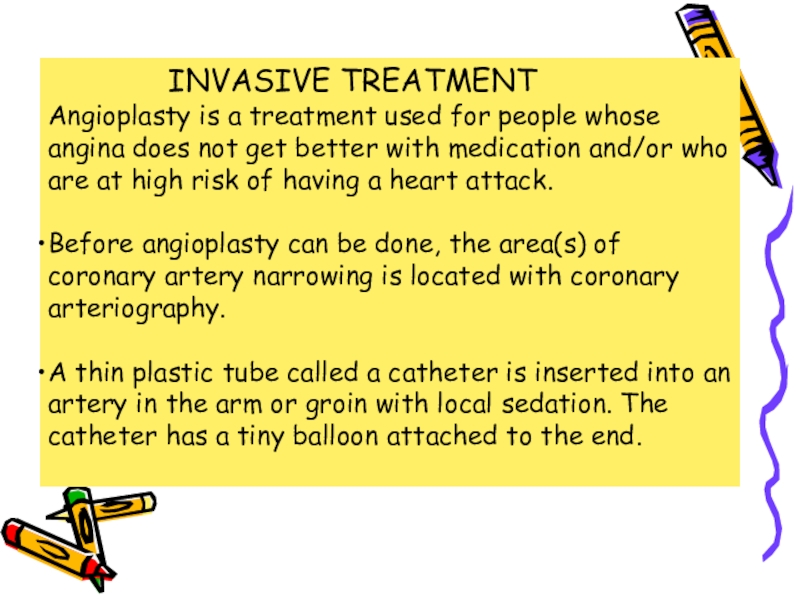
- 60. Medical TreatmentIf you keep having symptoms or
- 61. Слайд 61
- 62. INVASIVE TREATMENTThe catheter is threaded through the
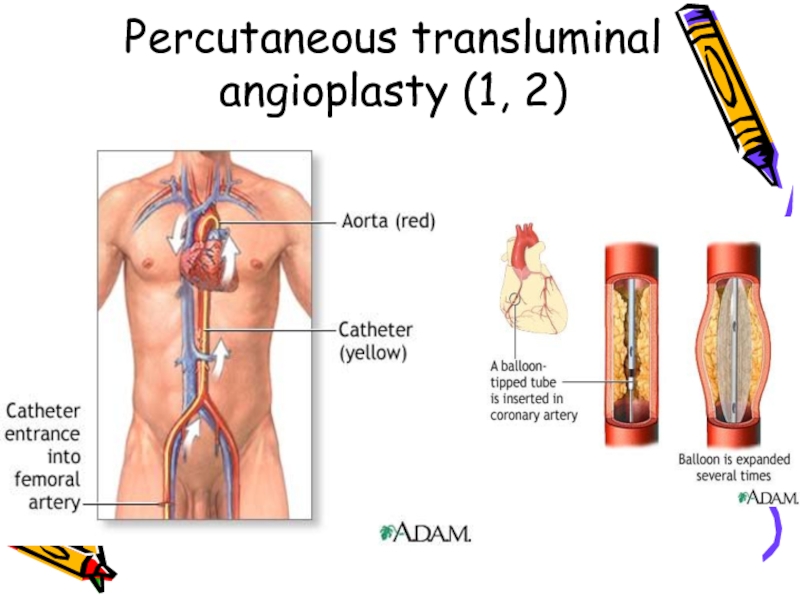
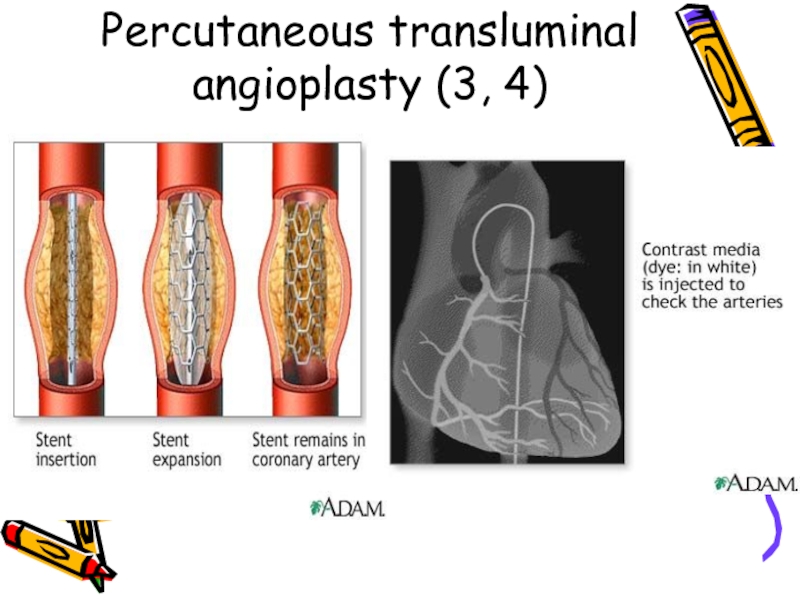
- 63. Percutaneous transluminal angioplasty (1, 2)
- 64. Percutaneous transluminal angioplasty (3, 4)
- 65. Слайд 65
- 66. Слайд 66
- 67. Слайд 67
- 68. Слайд 68
- 69. Слайд 69
- 70. Слайд 70
- 71. Thank you for attention !
- 72. Скачать презентанцию
Слайды и текст этой презентации
Слайд 2Sudden coronary death
Angina pectoris
Acute myocardial infarction
Painless myocardial ischaemia
Heart failure
Disturbences
of rhythm and conductivity
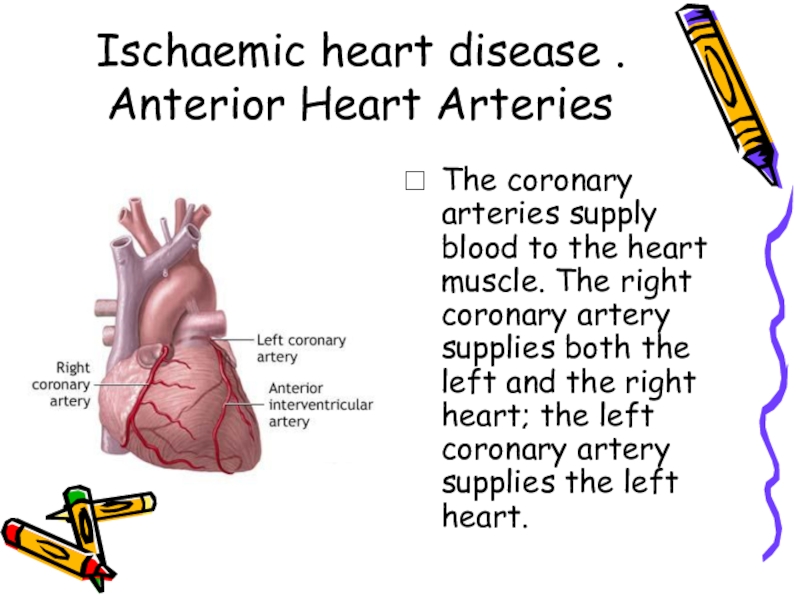
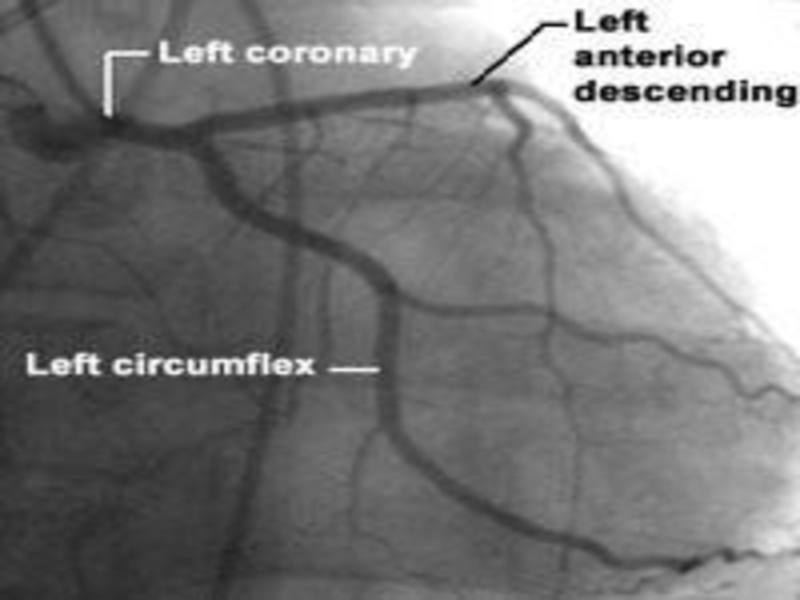
Слайд 3Ischaemic heart disease .
Anterior Heart Arteries
The coronary arteries supply blood
to the heart muscle. The right coronary artery supplies both
the left and the right heart; the left coronary artery supplies the left heart.Слайд 4Ischaemic heart disease .
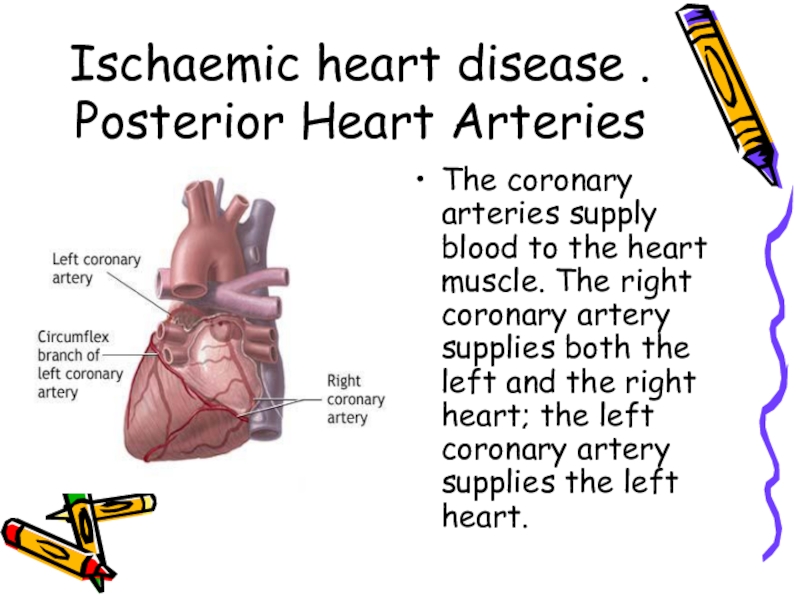
Posterior Heart Arteries
The coronary arteries supply blood
to the heart muscle. The right coronary artery supplies both
the left and the right heart; the left coronary artery supplies the left heart.Слайд 5Ischaemic heart disease
Ischaemic heart disease (Coronary artery disease) – is
the most common form of heart disease and the single
most important cause of premature death in Europe, Russia, North and South America, Australia and New Zealand.Ischaemic heart disease (IHD) – heart disease due to imbalance between myocardial oxygen supply and demand, which assotiated with atherosclerosis of coronary arteries in 95-96% cases.
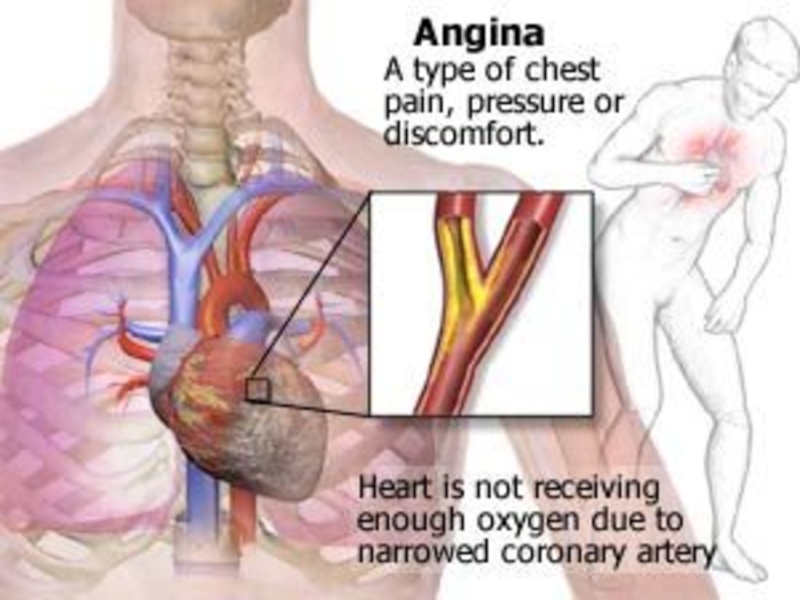
Слайд 6 ANGINA PECTORIS-DEFINITION
Angina pectoris is the clinical symptom
complex caused by transient myocardial ischaemia and may occur whenever
there is an imbalance between myocardial oxygen supply and demand.Слайд 7ANGINA PECTORIS-DEFINITION
Angina pectoris is the medical term used to describe
chest pains caused by poor blood flow to certain areas
of the heart muscle. Often, the name is shortened to angina. Having angina means patients have an increased risk of having a heart attack (myocardial infarction). Angina can be a useful warning sign if it makes patient seek timely medical help and avoid a heart attack. Prolonged or unchecked angina can lead to a heart attack or increase risk of having a heart rhythm abnormality. That could lead to sudden death.Слайд 9RISK FACTORS
Nonmodifable :
Age (> 45 )
Male gender
Family history
(genetic predisposition)
Aethnic origin
Modifable :
Dyslipidaemia
Arterial hypertension
Smoking
Diabetes mellitus
Obesity
Fatty food diet
Physical
inactivityStress
Hypoestrogenemia in female
Слайд 11
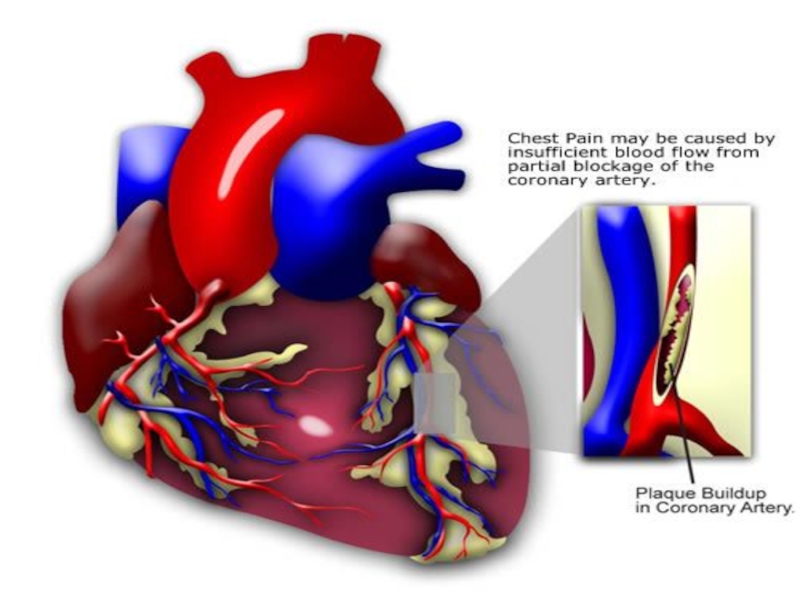
AETIOLOGY
There are 2 primary causes of angina.
Coronary (heart) artery atherosclerosis
In as many as 96% of cases, at least 1 blood vessel of heart has severe coronary blockage. Critical blockage of a coronary artery from atherosclerotic plaque buildup. When cholesterol or blood fats are too high, or patients have other risk factors, a fatlike material called atherosclerotic plaque builds up in blood vessels. Eventually the plaque will block blood flow through the vessel.
Exercise and emotional stress cause angina. Decreased oxygen content in the air you breathe (flying or being at high altitude) may trigger angina. Low blood flow to the heart, which occurs when you are in deep sleep, also can bring on angina. People commonly arrive at the Emergency Department in the early morning complaining of chest pain that awakened them from sleep, or the pain started after "just going to the bathroom."
2. Vasoconstriction.
Coronary spasm is also called variant angina Prinzmetal angina. Variant angina typically occurs when patients are at rest.
Слайд 13
INCIDENCE
The incidence of angina
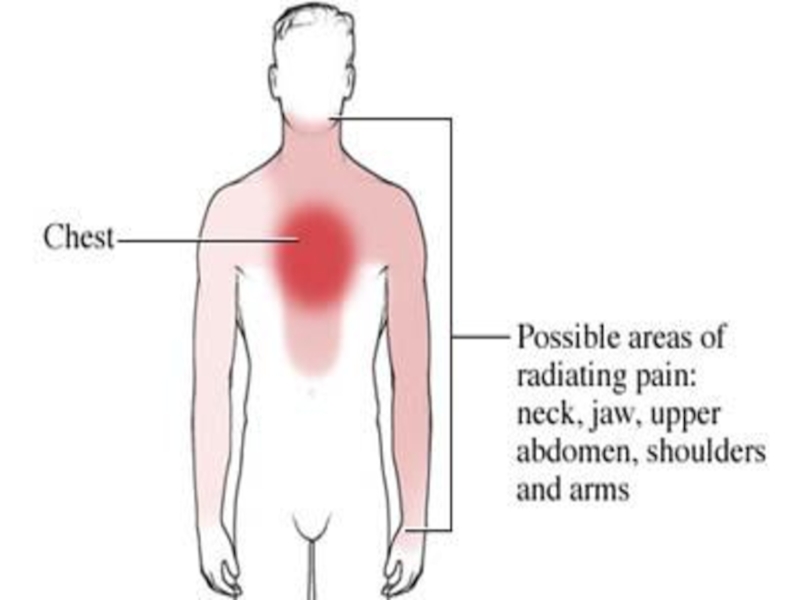
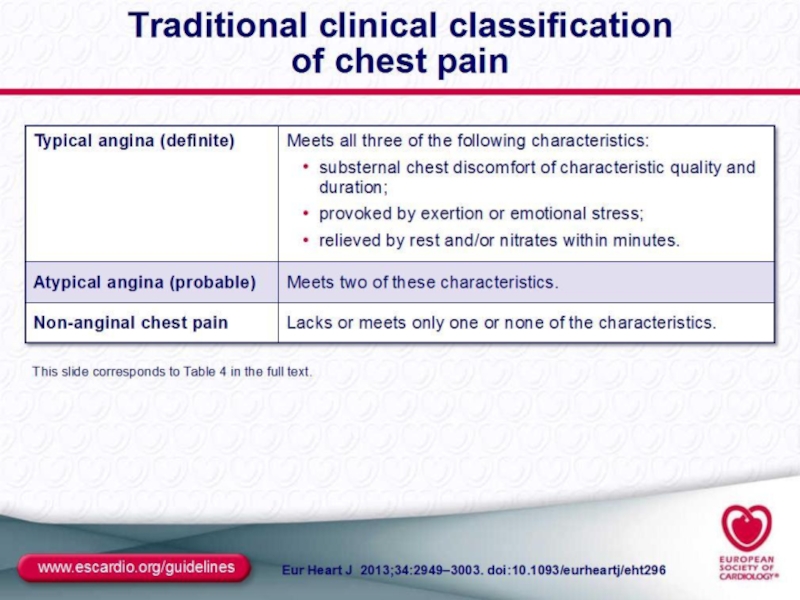
continuously rises with age in women while in men the incidence of angina peaks between 55 and 65 years of age before declining. Although angina pectoris is of great interest, there is a lack of data on a community wide basis because it is very difficult to study. Many cases are undetected and it is very likely that only a small fraction of cases reach specialist clinics. Слайд 14Identifying ischaemic cardiac chest pain
Ischaemic cardiac chest pain:
Location - central,
diffuse
Radiation -Jaw/neck/shoulder/ arm/back
Character -tight, burning ,squeezing, choking
Duration – less than
15 min (3-5 min)Precipitation -by exertion and/or emotion
Relieving factors - rest, quick response to nitrates
Associated features- Breathlessness
Слайд 15
SIGNS N SYMPTOMS
These are signs and symptoms of angina as
well:An uncomfortable pressure, fullness, squeezing or pain in the center of chest
Pain spreading to your shoulders, neck, or arms and lasting more than a few minutes.The pain may be mild to intense.
It may feel like pressure, tightness, burning, or a heavy weight.
It may be located in the chest, upper abdomen, back, neck, jaw, or inside your arms or shoulders.
Chest discomfort with light headedness
Anxiety, nervousness or fainting, sweating, nausea, or shortness of breath
Increased or irregular heart rate
Paleness
Cold sweaty skin
Feeling of impending doom
Слайд 20
CLASSIFICATION
Types of Angina Pectoris
Stable Angina
Unstable Angina
Prinzmetal’s or variant
angina
Microvascular angina
Слайд 21
Stable Angina
Stable angina is a repeating pattern of chest pain which has not changed in character, frequency, intensity or duration for several weeks. The level of activity or stress that provokes angina is predictable and the pattern changes slowly. Stable angina is the most common form and it appears gradually. These patients have an increased risk of a heart attack, but an episode of stable angina does not indicate that a heart attack is about to happen. A crucial component of the management of the pain associated with angina pectoris is Identifying sources of stress and creating effective methods to minimize stress. Relaxation techniques to reduce stress include meditation, listening to music, prayer, and exercise. The reasons for the benefits that emerge after a coronary patient implements relaxation techniques are not clear. However, important roles appear to be played by central neural transmitters, including serotonin, melatonin, epinephrine, and dopamine.
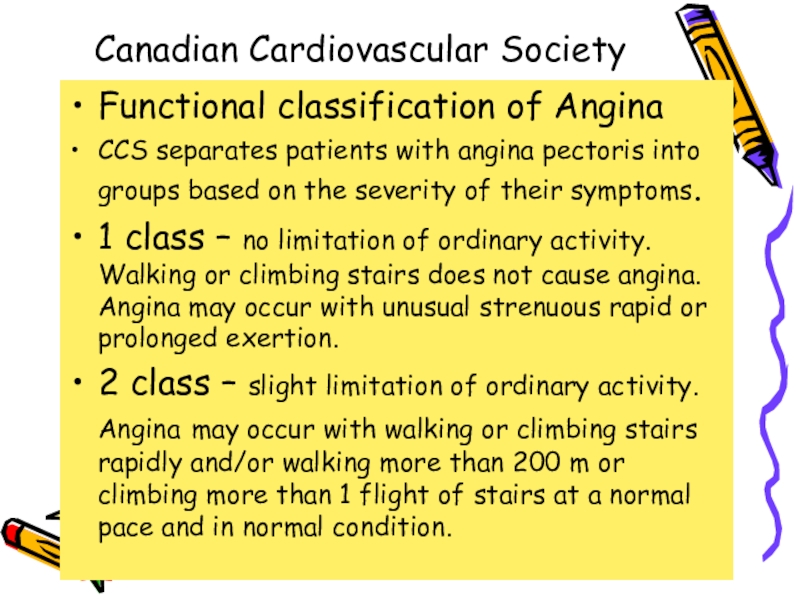
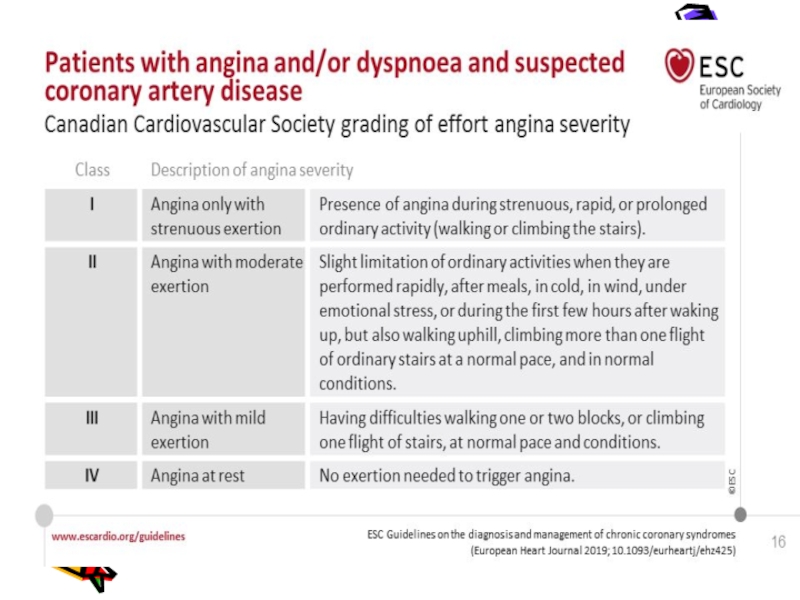
Слайд 22Сanadian Cardiovascular Society
Functional classification of Angina
ССS separates patients with angina
pectoris into groups based on the severity of their symptoms.
1
class – no limitation of ordinary activity. Walking or climbing stairs does not cause angina. Angina may occur with unusual strenuous rapid or prolonged exertion.2 class – slight limitation of ordinary activity. Angina may occur with walking or climbing stairs rapidly and/or walking more than 200 m or climbing more than 1 flight of stairs at a normal pace and in normal condition.
Слайд 23Сanadian Cardiovascular Society
Functional classification of Angina
3 class – marked
limitation of ordinary activity. Angina may occur after walking from
100 to 200 m or climbing 1 flight of stairs at a normal pace and in normal condition.4 class – unable to carry on any physical activity without chest discomfort. Angina may occur after walking less than 100m, may be present at rest.
Слайд 25
Unstable Angina
Unstable angina is chest pain that is variable, either increasing in frequency or intensity and with irregular timing or duration. Unlike stable angina, unstable angina does not appear gradually, it first appears as a severe episode. An established stable angina might change suddenly or be provoked by less stress than in the past or an episode might suddenly occur while at rest. If the pattern of an episode changes, for example if a previous episode was only brought on during physical exertion, but an episode suddenly occurred at rest it is likely to be unstable angina.
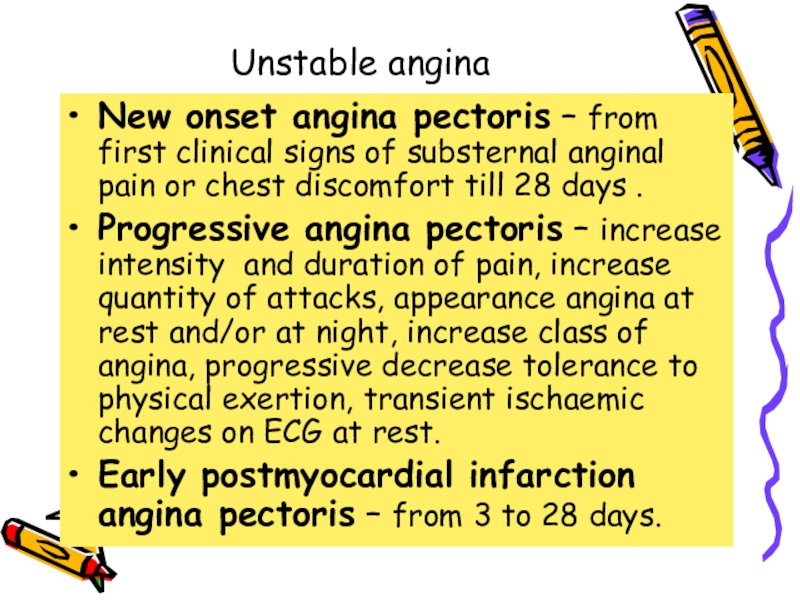
Слайд 26Unstable angina
New onset angina pectoris – from first clinical
signs of substernal anginal pain or chest discomfort till 28
days .Progressive angina pectoris – increase intensity and duration of pain, increase quantity of attacks, appearance angina at rest and/or at night, increase class of angina, progressive decrease tolerance to physical exertion, transient ischaemic changes on ECG at rest.
Early postmyocardial infarction angina pectoris – from 3 to 28 days.
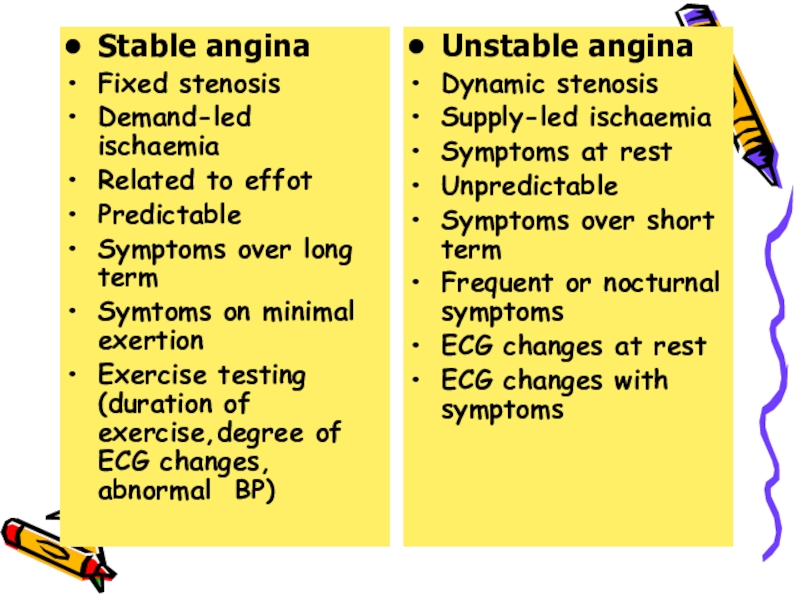
Слайд 27Stable angina
Fixed stenosis
Demand-led ischaemia
Related to effot
Predictable
Symptoms over long term
Symtoms on
minimal exertion
Exercise testing (duration of exercise,degree of ECG changes, abnormal
BP)Unstable angina
Dynamic stenosis
Supply-led ischaemia
Symptoms at rest
Unpredictable
Symptoms over short term
Frequent or nocturnal symptoms
ECG changes at rest
ECG changes with symptoms
Stable angina
Fixed stenosis
Demand-led ischaemia
Related to effot
Predictable
Symptoms over long term
Symtoms on minimal exertion
Exercise testing (duration of exercise,degree of ECG changes, abnormal BP)
Слайд 28
Prinzmetal's Angina
Prinzmetal’s or spontaneous or angiospastic angina is caused by a vasospasm, a spasm that narrows the coronary artery and lessens the blood flow to the heart. Prinzmetal's Angina usually occurs in arteries already narrowed by atherolsclerosis, in fact most people with it have severe coronary atherosclerosis in at least one major vessel. The spasm usually occurs very close to the blockage. Unlike stable and unstable angina, Prinzmetal's Angina usually occurs when a person is at rest or sleep (often at night) and not after physical exertion or emotional stress. It is associated with acute myocardial infarction, severe cardiac arrhythmias including ventricular tachycardia and fibrillation, and sudden cardiac death.
Слайд 29 Microvascular Angina
or
Stable Angina Pectoris on angiographycally intact vessels or Coronary Syndrome XMicrovascular angina, or Syndrome X, occurs when the patient experiences chest pain but has no apparent coronary artery blockage. This condition results from poor functioning of the tiny blood vessels that nourish the heart, arms and legs. Microvascular angina can occur during exercise or at rest. Reduced vasodilator capacity of the coronary microvessels is thought to be a cause of angina during exercise, but the mechanism of angina at rest is not known. Coronary microvascular spasm and resultant myocardial ischemia may be the cause of chest pain in a subgroup of patients with microvascular angina.
Слайд 30Coronary Syndrome X
Characterized by 3 specific, typical signs as :
Classic
anginal chest pain
ST segment depression on ECG during stress-test
Angiographically normal
coronary arteries without LV dysfunctionСлайд 31Terminology Clarification
One major association between microvascular angina and the
insulin resistance syndrome has arisen from terminological confusion
The
term syndrome X was first used in the 1970’s to refer to a heterogeneous group of patients with chest pain and normal coronary angiograms. In the late 1980’s this concurrence of myocardial ischaemia and normal angiograms was called microvascular angina.
The term "metabolic" syndrome X was first used in the late 1980’s to describe a pathological insulin-resistant condition, characterised by high prevalences of non-insulin-dependent diabetes, hypertension, obesity, dyslipidaemia, and cardiovascular disease.
The term insulin resistance syndrome is now preferred by many to refer to this pathological insulin resistant condition.
Слайд 32Diabetes and Angina
Insulin resistance and secondary hyperinsulinemia are recognized
risk factors for development of atherosclerosis. Hyperinsulinemia (high insulin levels
in the blood) is a marker for the Insulin Resistance Syndrome. Hyperinsulinemia results from the body’s attempt to overcome insulin resistance by secreting more insulin from the pancreas.Insulin Resistance Syndrome has been demonstrated in patients with angina pectoris irrespective of detectable atherosclerosis at coronary angiograms. A study conducted by Botker et al provided clear evidence that patients with microvascular angina are insulin resistant, independent of body mass index and physical fitness.
Research by Fava et al indicated that diabetic patients with unstable angina have a higher mortality than non-diabetic patients. The presence of diabetes is a strong risk factor for coronary artery disease and cardiac death in elderly hemodialysis patients. Both symptomatic and silent ischemic heart disease may occur frequently during hemodialysis because hemodialysis simultaneously reduces coronary artery oxygen delivery while increasing myocardial oxygen demand.
Слайд 33Diagnosis
The diagnosis of angina pectoris usually involves a careful
assessment and history of signs and symptoms. Diagnostic procedures to
exclude angina or establish the severity of coronary heart disease include electrocardiogram (ECG ), a stress test, and coronary arteriogram (or angiogram). The ECG records electrical impulses of the heart which enables one to assess if the heart muscle is not getting sufficient oxygen or if there are abnormal features of the heart. A stress test is used to detect coronary artery disease and to determine safe levels of exercise. In a coronary arteriogram (or angiogram), x-rays are taken after a contrast agent is injected into an artery to locate the narrowing, occlusions, and other abnormalities of specific arteries. There are a few conditions which mimic angina. Sources of pain most often confused with cardiac pain are gastrointestinal (esophageal and hiatal hernia, biliary), musculoskeletal, pulmonary, and pericardial.Слайд 34Laboratory investigations
Obligatory indicators:
Hb, Total Cholesterol, HDL-C, LDL-C, triglycerides, glucose,
AST, ALT, creatinine (GFR)
Additional indicators:
Cardiac troponins, thyroid function
Слайд 35Investigations
Resting ECG – reversible ST depression or elevation with or
without T-wave inversion at the time the patient is experiencing
symptomsExercise ECG – stadart treadmill or bicycle ergometer protocol. Planar or down-sloping ST depression of 1mm or more is indicative of ischaemia.
Holter monitoring ECG during 24 hours
Myocardial perfusion scanning helpful in patients who are unable to exercise, its predictive accuracy is higher than that of the exercise ECG.
Слайд 36Investigations
Stress echocardiography – to identify ischaemic segments of myocardium and
areas of infarction ( exhibit reversible defects in contrac-tility during
exercise or pharmacological stress with a dobutamine)Coronary arteriography – provides detailed anatomical information about the extent and nature of coronary artery disease and is usually performed with a view to coronary bypass grafting or PCI. May be indicated when non-invasive tests have failed to elucidate the cause of atypical chest pain.
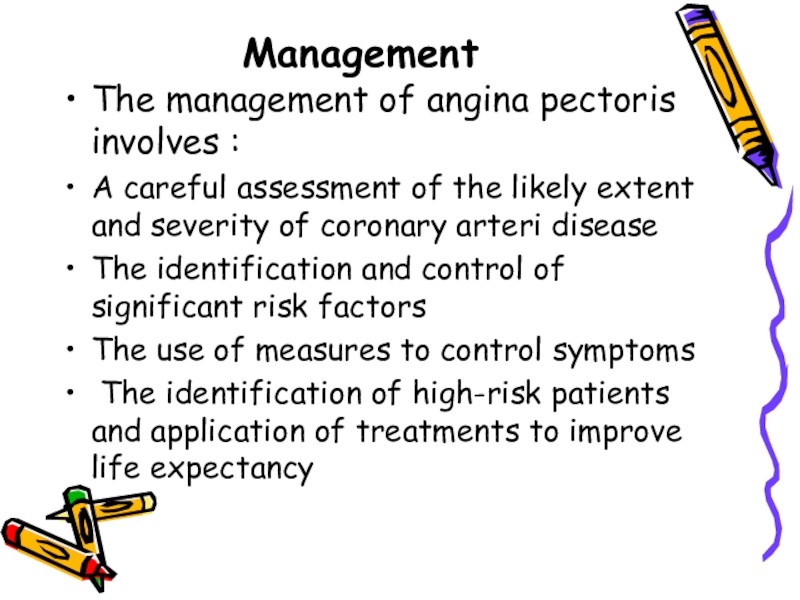
Слайд 41Management
The management of angina pectoris involves :
A careful assessment of
the likely extent and severity of coronary arteri disease
The identification
and control of significant risk factors The use of measures to control symptoms
The identification of high-risk patients and application of treatments to improve life expectancy
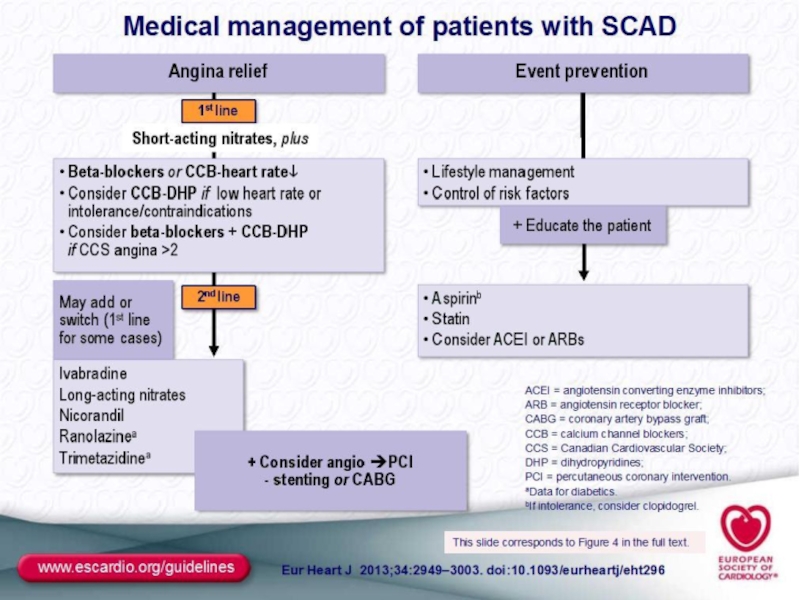
Слайд 46Treatment
Nitroglycerin is the drug most often used. It mainly relaxes
the veins and relaxes the coronary arteries a little. By
relaxing the veins, it reduces the amount of blood that returns to the heart and eases the heart's workload. By relaxing the coronary arteries, it increases the heart's blood supply.The heart's demand for oxygen also can be modified with drugs that reduce blood pressure. This reduces the heart's workload and need for oxygen. Drugs that slow the heart rate have a similar effect. Drugs called beta-blockers and calcium antagonists are used for these effects. There are many different beta-blockers and calcium antagonists, and the specific ones used are selected depending on the individual characteristics of each patient.
Слайд 47Anti-anginals
- B- blockers -1st line (metoprolol,bisoprolol,nebivolol,carvedilol)
- Calcium antagonists (verapamil ,
amlodipin,diltiazem if b-blockers contraindicated)
- Nitrates (isosorbide dinitrate, isosorbide mononitrate )
Слайд 48Treatment
ANTI-ANGINAL DRUG TREATMENT – GROUPS OF DRUGS ARE USED
TO HELP RELIEVE OR PREVENT THE SYMPTOMS OF ANGINA:
NITRATES, B-BLOCKERS, CALCIUM ANTAGONISTS , POTASSIUM CHANNEL ACTIVATORS. Angina pectoris can be treated with drugs that affect the blood supply to the heart muscle or the heart's demand for oxygen or both. Drugs that affect the blood supply are coronary vasodilators; they cause blood vessels to relax. When this happens, the opening inside the vessels (the lumen) gets bigger. Then blood flow improves, letting more oxygen and nutrients reach the heart muscle.Слайд 49Drugs,which improve prognosis
- Antiplatelet drugs (aspirin,clopidogrel )
- Statins (lovastatin,simvastatin, atorva-statin,rosuvastatin
)
- B-blockers (atenolol,metaprolol,bisoprolol,nebivolol,
carvedilol )
- ACE – inhibitors (enalapril,lisinopril,perindopril,ramipril
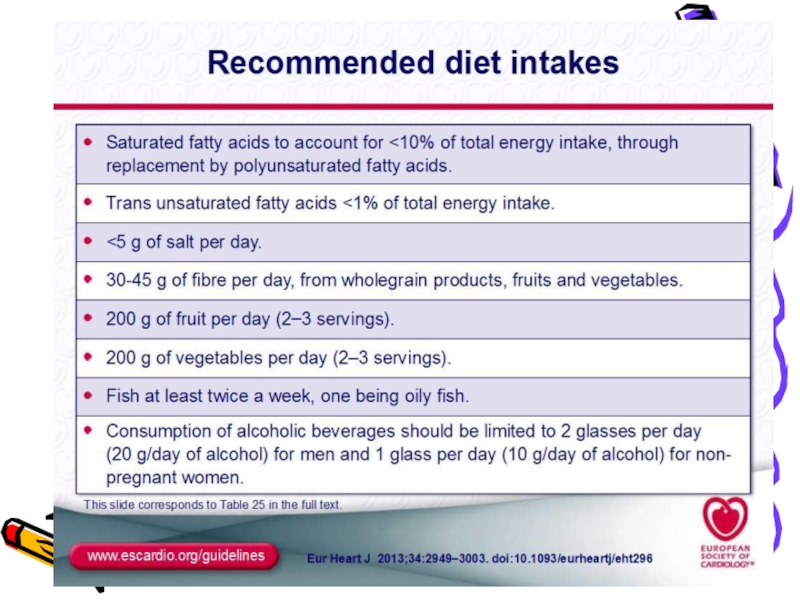
Слайд 50Treatment Controlling the risk factors for angina pectoris, such as
high blood pressure, cigarette smoking, high cholesterol levels, and excess
weight is an essential part of treatment.ANTIPLATELET THERAPY -low-dose aspirin(75-150mg) reduces the risk of adverse events such as MI and should be prescribed for all patients. Clopidogrel (75mg) is an equally effective agent that can be prescribed if aspirin causes dyspepsia or other side-effects.
Слайд 51What procedures are used to treat angina?
Invasive techniques that improve
the heart and the heart's blood supply also may be
used. One of these is percutaneous transluminal coronary angioplasty. It's also known as PCI, PTCA, angioplasty, balloon dilation or balloon angioplasty. In it, a thin, flexible plastic tube (catheter) with a balloon is inserted into an artery and advanced to the blockage. Then the balloon is inflated, squeezing open the fatty plaque deposit. Then the balloon is deflated and the catheter is withdrawn. Often a stent is also placed to hold the artery open. Two additional techniques used to reduce coronary blockages are laser angioplasty and atherectomy. In laser angioplasty, a catheter with a laser on its tip is used to open the blockage. In atherectomy, a catheter has a rotating shaver on its tip to cut away the plaque. These techniques also may be accompanied by stent placement.Слайд 52Coronary artery bypass graft surgery is also used. In it,
a blood vessel is used to route blood around the
blocked part of the artery, forming a kind of detour. Before performing any of these procedures, a doctor must find the blocked part(s) of the coronary arteries. This requires coronary arteriography, which is done during cardiac catheterization. In this procedure a doctor guides a catheter through an artery in the arm or leg and into the coronary arteries. Then the doctor injects a liquid dye through the catheter. High-speed X-ray movies record the course of the dye as it flows through the arteries. Doctors can identify blockages by tracing the flow. An evaluation of how the heart works also can be done during cardiac catheterization. Other tests can be used to evaluate how well the heart works, and may be done before or after a heart attack.Слайд 53How is variant angina or Prinzmetal's angina treated?
Calcium antagonists are
extremely effective in preventing the coronary spasm of variant or
Prinzmetal's angina. These drugs, along with nitrates, are the mainstays of treatment. Prinzmetal's angina tends to be cyclic, appearing for a time, then going away. Because of this, after six to 12 months of treatment, the calcium antagonists may be gradually reduced. In some cases PTCA or surgery are used when blockages exist along with spasm.Слайд 54Medical Treatment
If you have come to the hospital emergency department,
you may be sent to another care area for further
testing, treatment, or observation. On the basis of your provider's preliminary diagnosis, you may be sent to the following units:An observation unit pending test results or further testing
A cardiac care unit
A cardiac catheterization unit
The operating room for emergency cardiac bypass surgery
Слайд 55Medical Treatment
Regardless of where you are sent, several basic treatments
may be started. Which are given to you depends on
the severity of your symptoms and the underlying disease.You will have at least one intravenous line started. This line is used to give medication or fluids.
You will probably be given an aspirin if you haven't already taken one.
You may be given oxygen through a face mask or a tube in your nose. This will help you feel better if you are having trouble breathing or feeling uncomfortably short of breath by raising the oxygen content of your blood.
Слайд 56
Medical Treatment
Treatment will depend on the severity of symptoms, severity of the underlying disease, and extent of damage to the heart muscle, if any.Simple rest and observation, an aspirin, breathing oxygen, and sublingual nitroglycerin may be all that you need, if it is only angina.
You may be given medication to reduce anxiety or to treat pain.
Слайд 57Medical Treatment
You may be given medication to lower blood pressure
or heart rate. Beta blockers, Angiotensin Converting Enzyme Inhibitors (ACE
inhibitors), and cholesterol- lowering drugs (statins) are commonly given if the chances of a heart attack are likely.You may be given medication to reduce risk of having a blood clot or to prevent further clotting.
If the health care provider believes chest pain actually represents a heart attack, you may be given a powerful "clot-buster" medication called a fibrinolytic.
Слайд 58Metabolic therapy
- Trimetazidine (preductal)
- Riboxin
- Mildronate (vasonate)
- Tiotriozaline
- Vitamins
- Antioxidantes
Слайд 59 Medical Treatment
After reviewing your immediate test results, the hospital health care provider will make a decision about where you should be for the next hours and days.
If you are feeling better, your condition is stable, and this was only an angina attack, you may be allowed to go home. You may be given medications to take. You will be told to follow up with your primary care provider within the next day or two.
Слайд 60Medical Treatment
If you keep having symptoms or your condition is
unstable, you will be admitted to the hospital. You will
probably undergo further tests and possibly coronary angiography, coronary artery angioplasty, or even coronary artery bypass surgery, if all your arteries are critically blocked.Слайд 61 INVASIVE TREATMENT
Angioplasty is a treatment used for people whose angina does not get better with medication and/or who are at high risk of having a heart attack.
Before angioplasty can be done, the area(s) of coronary artery narrowing is located with coronary arteriography.
A thin plastic tube called a catheter is inserted into an artery in the arm or groin with local sedation. The catheter has a tiny balloon attached to the end.
Слайд 62INVASIVE TREATMENT
The catheter is threaded through the arteries and into
the artery where the narrowing is.
The balloon is inflated,
opening up the narrowing. This is not a permanent solution for most people. Many require placement of a "stent," a small metal sleeve that is placed in the narrowed artery. The stent holds the artery open.