Слайд 1Cardiac Arrhythmias
Done by: Islamova Sh.
Group: 646 P.
Checked by: Seyitkaliev Zh.
Слайд 2PLAN
1. Impulse conduction of the heart
2. Mechanisms of cardiac arrhythmias
3.
Triggered activity, reentry arrhythmias, accelerated automaticity
4. Classification of arrhythmia and
their description
5. Management of arrhythmias
6. Classification of antiarrhythmic drugs based on drug action
7. Used references
Слайд 3SAN
AVN
Impulse conduction
Impulses originate regularly at a frequency of 60-100 beat/
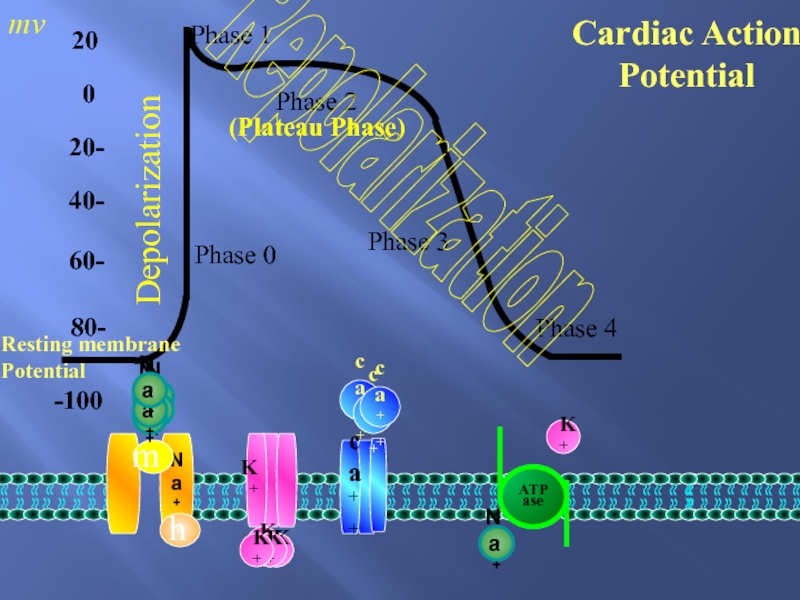
Слайд 4-100
-80
-60
-40
-20
0
20
Phase 0
Phase 1
Phase 2
Phase 3
Phase 4
Na+
ca++
ATPase
mv
Cardiac Action Potential
Resting
membrane Potential
Na+
m
Na+
Na+
Na+
Na+
Na+
h
K+
ca++
K+
K+
K+
ca++
ca++
(Plateau Phase)
K+
K+
K+
Na+
K+
Depolarization
Repolarization
Слайд 5Cardiac Arrhythmias
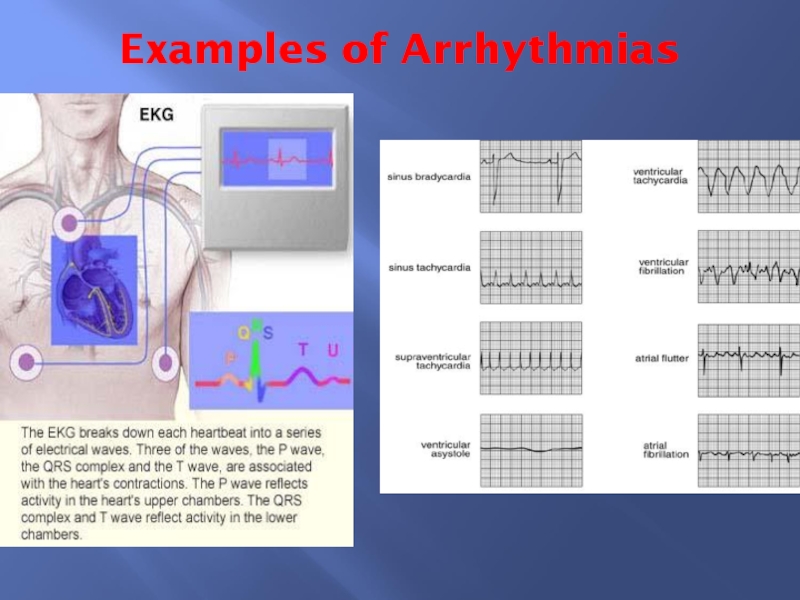
●An abnormality of the cardiac rhythm is called a
cardiac arrhythmia.
● Arrhythmias may cause sudden death, syncope, heart
failure, dizziness, palpitations or no symptoms at all.
● There are two main types of arrhythmia:
bradycardia: the heart rate is slow (< 60 b.p.m).
tachycardia: the heart rate is fast (> 100 b.p.m).
Слайд 6Mechanisms of Cardiac Arrhythmias
Mechanisms of bradicardias:
Sinus bradycardia is a result
of abnormally slow automaticity while bradycardia due to AV block
is caused by abnormal conduction within the AV node or the distal AV conduction system.
Mechanisms generating tachycardias include:
- Accelerated automaticity.
- Triggered activity
- Re-entry (or circus movements)
Слайд 7ACCELERATED AUYOMATICITY
It occurs due to increasing the rate of diastolic
depolarization or changing the threshold potential.
Abnormal automaticity can occur
in virtually all cardiac tissues and may initiate arrhythmias.
Such changes are thought to produce sinus tachycardia, escape rhythms and accelerated AV nodal (junctional) rhythms.
Слайд 8TRIGGERED ACTIVITY
Myocardial damage can result in oscillations of the transmembrane
potential at the end of the action potential. These oscillations,
which are called 'after depolarizations', may reach threshold potential and produce an arrhythmia.
The abnormal oscillations can be exaggerated by pacing, catecholamines, electrolyte disturbances, and some medications.
Examples as atrial tachycardias produced by digoxin toxicity and the initiation of ventricular arrhythmia in the long QT syndrome.
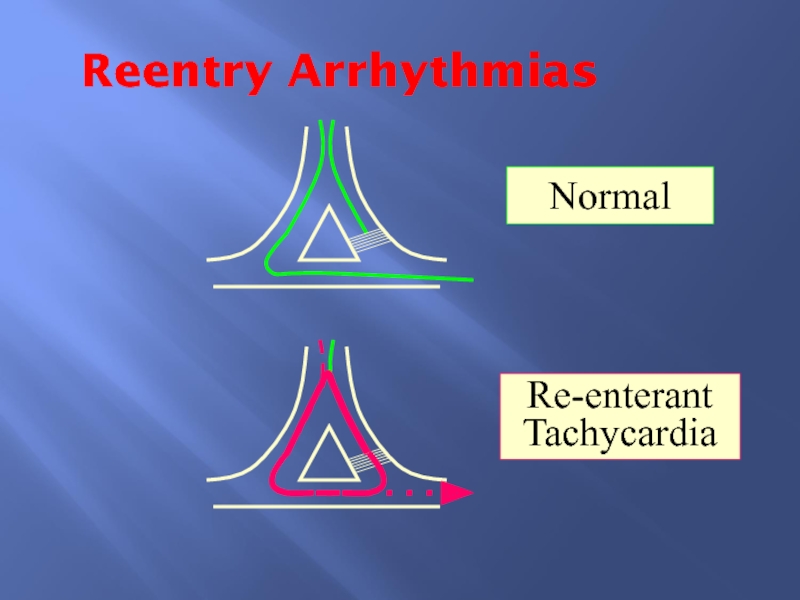
Слайд 9Re-entry (or circus movement)
The mechanism of re-entry occurs when a
'ring' of cardiac tissue surrounds an inexcitable core (e.g. in
a region of scarred myocardium). Tachycardia is initiated if an ectopic beat finds one limb refractory (α) resulting in unidirectional block and the other limb excitable. Provided conduction through the excitable limb (β) is slow enough, the other limb (α) will have recovered and will allow retrograde activation to complete the re-entry loop. If the time to conduct around the ring is longer than the recovery times (refractory periods) of the tissue within the ring, circus movement will be maintained, producing a run of tachycardia.
The majority of regular paroxysmal tachycardias are produced by this mechanism.
Слайд 10Reentry Arrhythmias
Normal
Re-enterant
Tachycardia
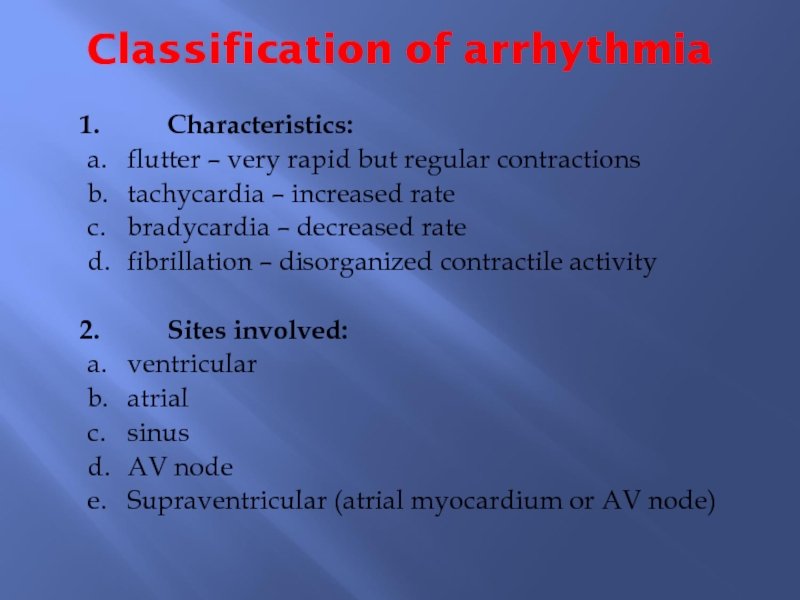
Слайд 11Classification of arrhythmia
1. Characteristics:
a. flutter – very rapid but regular contractions
b. tachycardia
– increased rate
c. bradycardia – decreased rate
d. fibrillation – disorganized contractile activity
2. Sites
involved:
a. ventricular
b. atrial
c. sinus
d. AV node
e. Supraventricular (atrial myocardium or AV node)
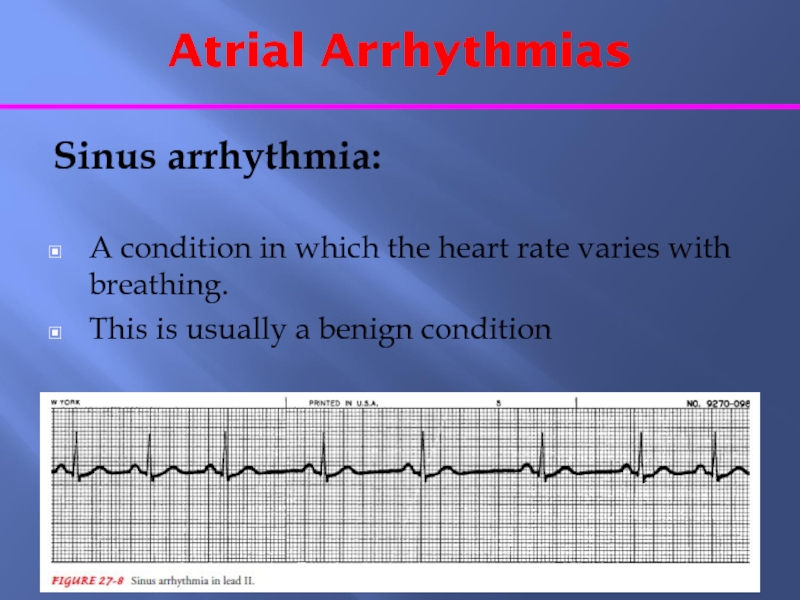
Слайд 13Atrial Arrhythmias
Sinus arrhythmia:
A condition in which the heart rate
varies with breathing.
This is usually a benign condition
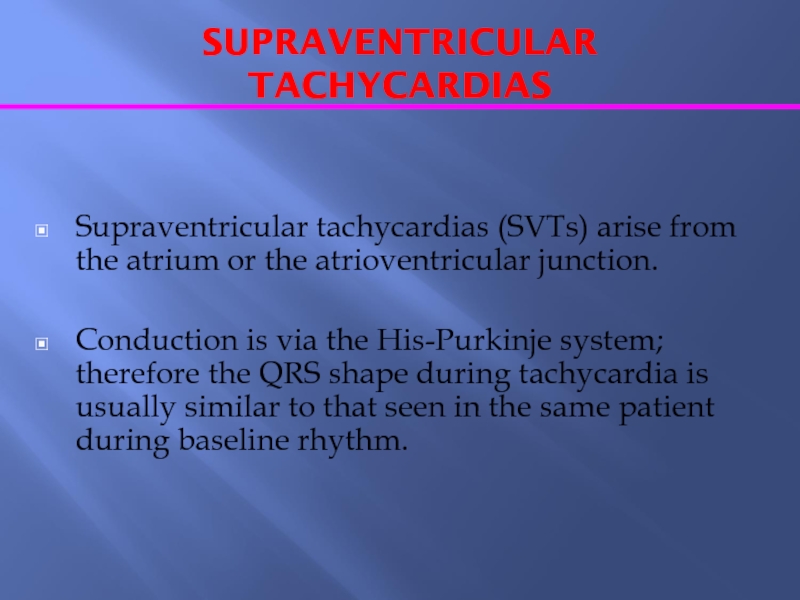
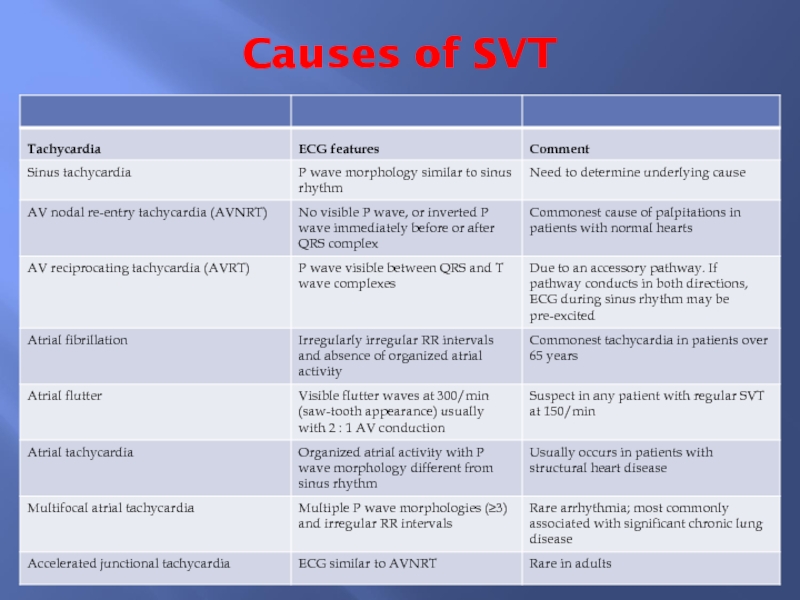
Слайд 14SUPRAVENTRICULAR TACHYCARDIAS
Supraventricular tachycardias (SVTs) arise from the atrium or the
atrioventricular junction.
Conduction is via the His-Purkinje system; therefore the
QRS shape during tachycardia is usually similar to that seen in the same patient during baseline rhythm.
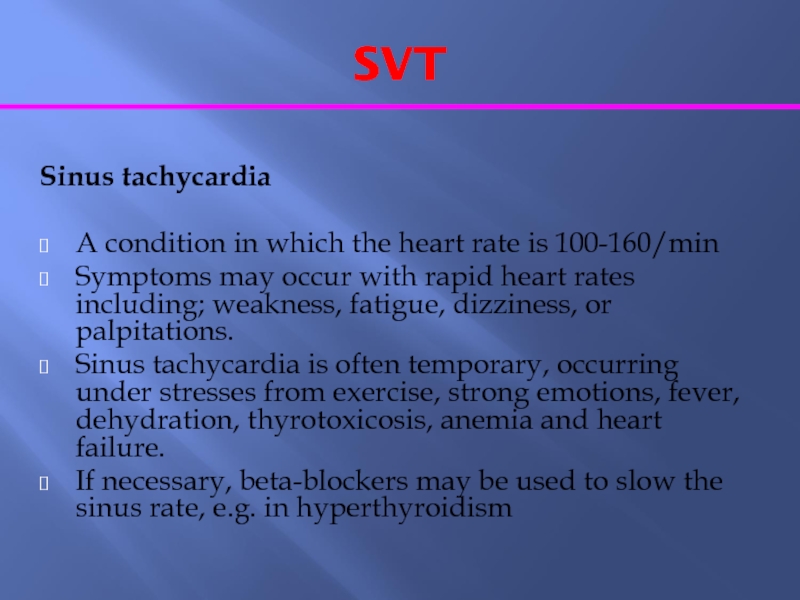
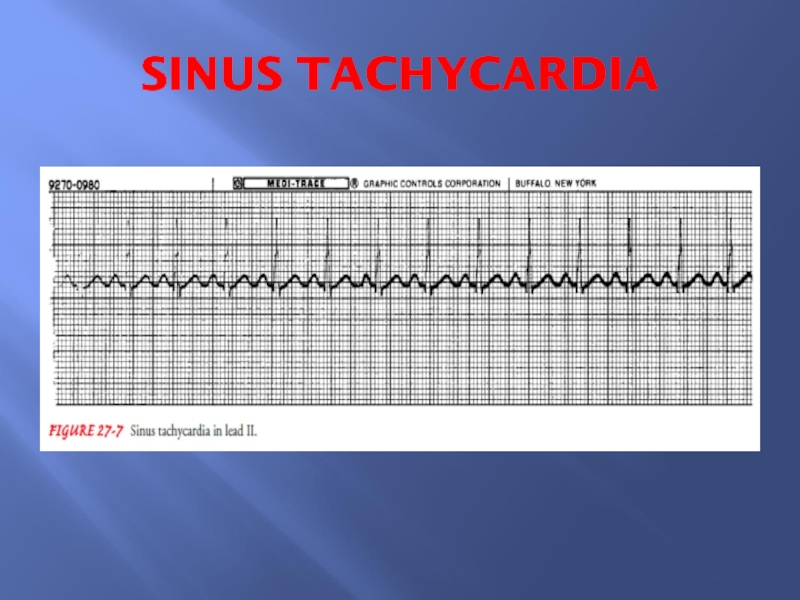
Слайд 16SVT
Sinus tachycardia
A condition in which the heart rate is
100-160/min
Symptoms may occur with rapid heart rates including; weakness,
fatigue, dizziness, or palpitations.
Sinus tachycardia is often temporary, occurring under stresses from exercise, strong emotions, fever, dehydration, thyrotoxicosis, anemia and heart failure.
If necessary, beta-blockers may be used to slow the sinus rate, e.g. in hyperthyroidism
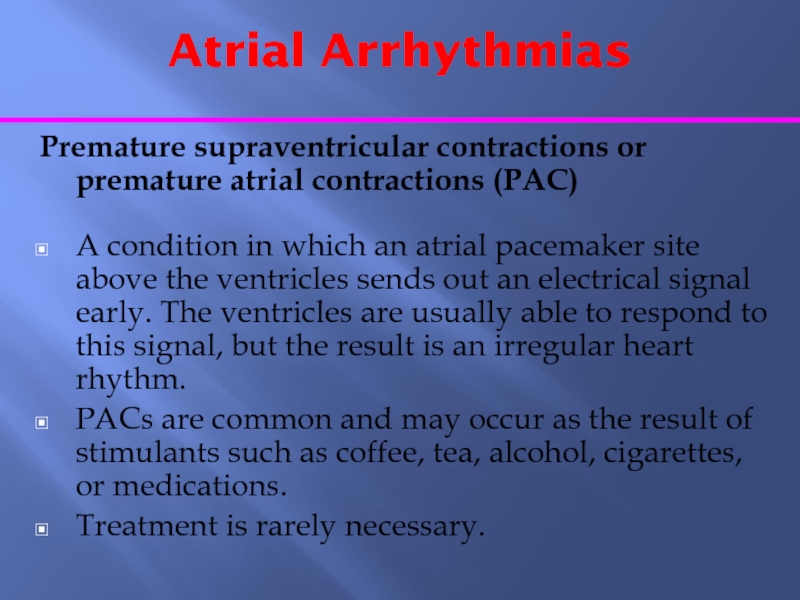
Слайд 18Atrial Arrhythmias
Premature supraventricular contractions or premature atrial contractions (PAC)
A
condition in which an atrial pacemaker site above the ventricles
sends out an electrical signal early. The ventricles are usually able to respond to this signal, but the result is an irregular heart rhythm.
PACs are common and may occur as the result of stimulants such as coffee, tea, alcohol, cigarettes, or medications.
Treatment is rarely necessary.
Слайд 19SVT
Paroxysmal Supraventricular tachycardia [HR 160-250/min]
Atrioventricular nodal re-entry tachycardia (AVNRT)
It usually begins and ends rapidly, occurring in repeated periods.
This condition can cause symptoms such as weakness, fatigue, dizziness, fainting, or palpitations if the heart rate becomes too fast.
In AVNRT, there are two functionally and anatomically different pathways within the AV node: one is characterized by a short effective refractory period and slow conduction, and the other has a longer effective refractory period and conducts faster.
In sinus rhythm, the atrial impulse that depolarizes the ventricles usually conducts through the fast pathway.
If the atrial impulse (e.g. an atrial premature beat) occurs early when the fast pathway is still refractory, the slow pathway takes over in propagating the atrial impulse to the ventricles. It then travels back through the fast pathway which has already recovered its excitability, thus initiating the most common 'slow-fast', or typical, AVNRT.
Слайд 20AVNRT (continue)
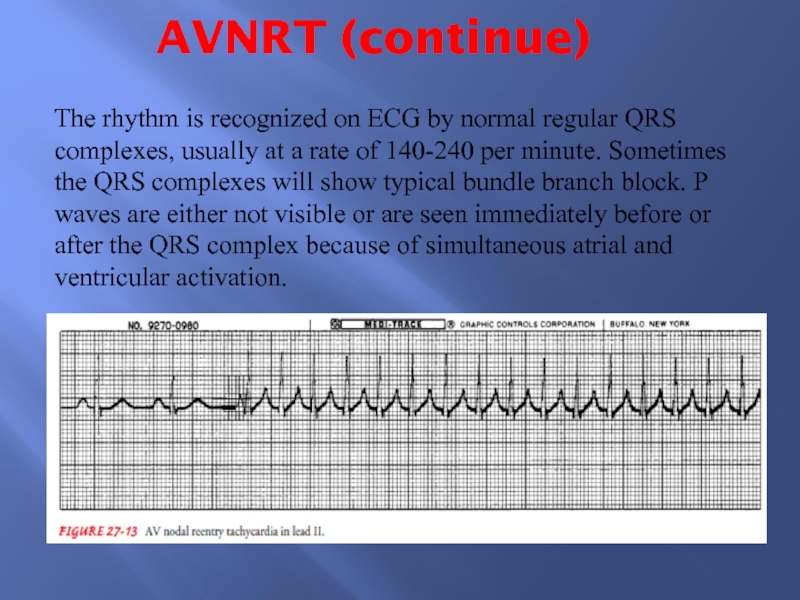
The rhythm is recognized on ECG by normal regular
QRS complexes, usually at a rate of 140-240 per minute.
Sometimes the QRS complexes will show typical bundle branch block. P waves are either not visible or are seen immediately before or after the QRS complex because of simultaneous atrial and ventricular activation.
Слайд 21SVT
Atrioventricular reciprocating tachycardia
(AVRT)
In AVRT there is a large circuit
comprising the AV node, the His bundle, the ventricle and
an abnormal connection from the ventricle back to the atrium. This abnormal connection is called an accessory pathway or bypass tract.
Bypass tracts result from incomplete separation of the atria and the ventricles during fetal development.
Atrial activation occurs after ventricular activation and the P wave is usually clearly seen between the QRS and T complexes
Слайд 22PSVT
Acute Management
Patients presenting with SVTs and haemodynamic instability require
emergency cardioversion.
If the patient is haemodynamically stable, vagal manoeuvres,
including right carotid massage, Valsalva manoeuvre and facial immersion in cold water can be successfully employed.
If not successful, intravenous adenosine (up to 0.25 mg/kg) , verapamil 5-10 mg i.v. over 5-10 minutes, i.v. diltiazem, or beta-blockers should be tried.
Long-term management
It includes ablation of an accessory pathway. Also, verapamil, diltiazem & β-blockers; are effective in 60-80% of patients.
Слайд 23
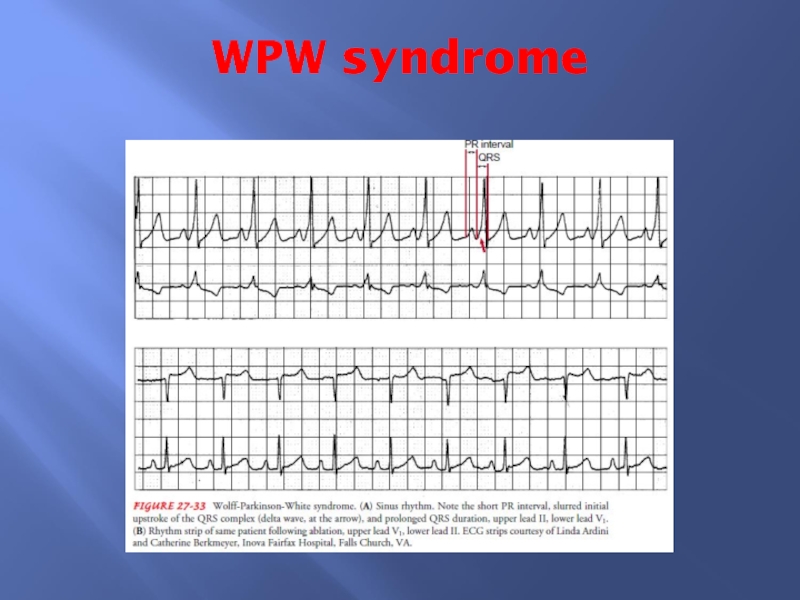
The Wolf Parkinson White Syndrome (WPW)
►An abnormal band of atrial
tissue connects the atria and ventricles and can electrically bypass
the normal pathways of conduction; a re-entry circuit can develop causing paroxysms of tachycardia.
►ECG shows:
- Short PR interval
- Delta wave on the upstroke of the QRS complex
►Drug treatment includes flecainamide, amiodarone or disopyramide.
►Digoxin and verapamil are contraindicated.
►Transvenous catheter radiofrequency ablation is the treatment of choice.
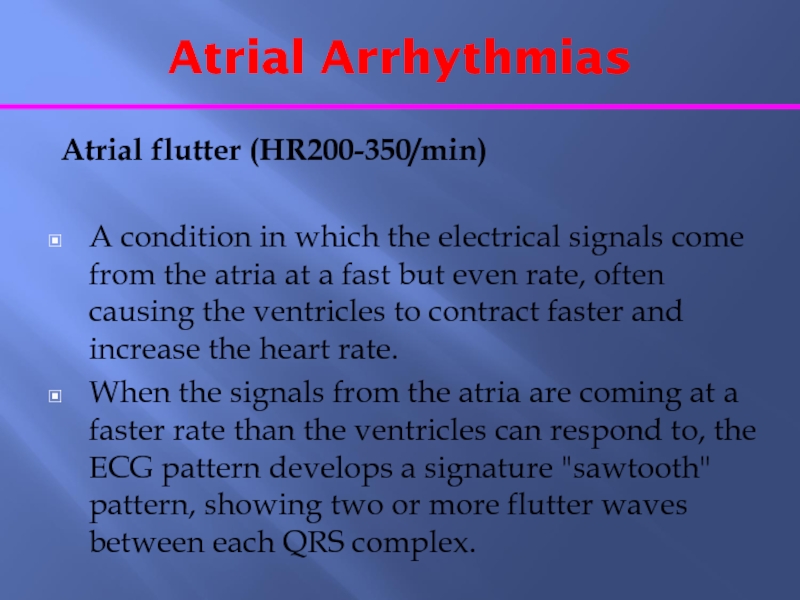
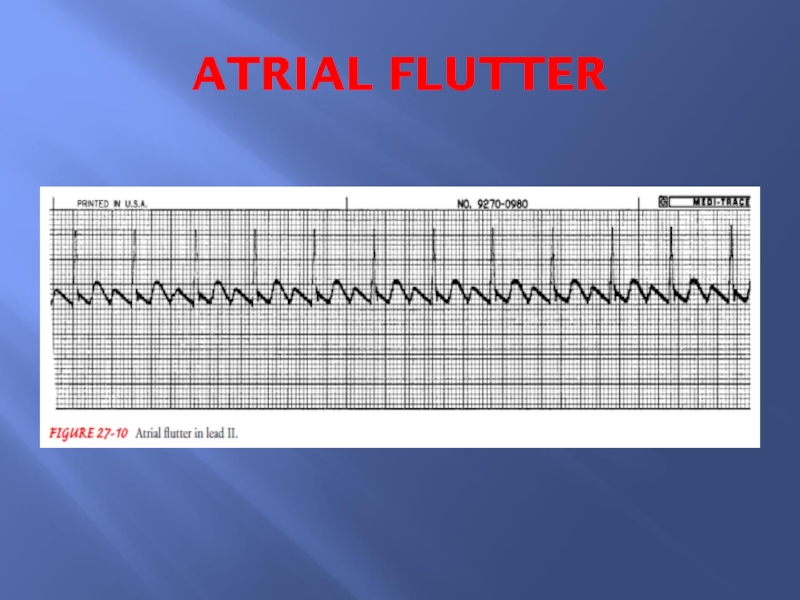
Слайд 25Atrial Arrhythmias
Atrial flutter (HR200-350/min)
A condition in which the electrical
signals come from the atria at a fast but even
rate, often causing the ventricles to contract faster and increase the heart rate.
When the signals from the atria are coming at a faster rate than the ventricles can respond to, the ECG pattern develops a signature "sawtooth" pattern, showing two or more flutter waves between each QRS complex.
Слайд 26Atrial Arrhythmias
Atrial flutter (TREATMENT)
Treatment of the symptomatic acute paroxysm
is electrical cardioversion.
Patients who have been in atrial flutter
more than 1-2 days should be treated in a similar manner to patients with atrial fibrillation and anticoagulated for 4 weeks prior to cardioversion.
Recurrent paroxysms may be prevented by class Ic and class III agents
The treatment of choice for patients with recurrent atrial flutter is radiofrequency catheter ablation
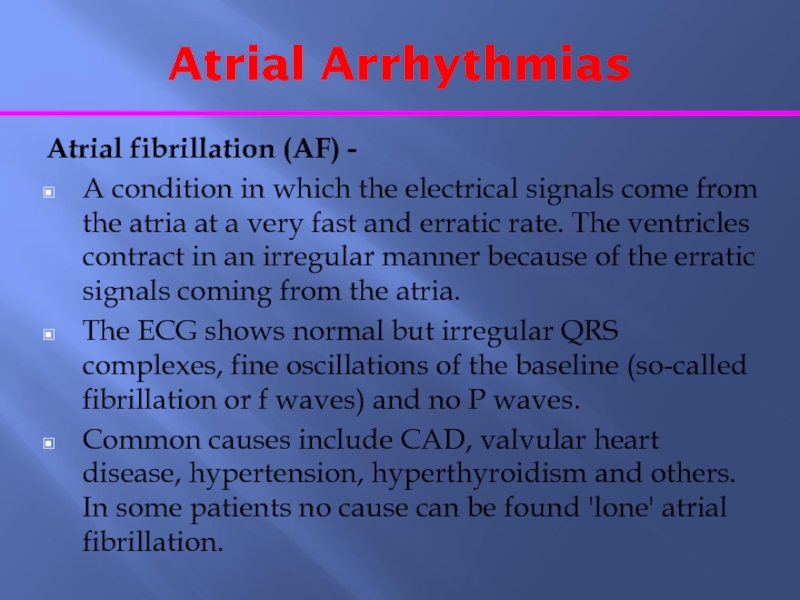
Слайд 28Atrial Arrhythmias
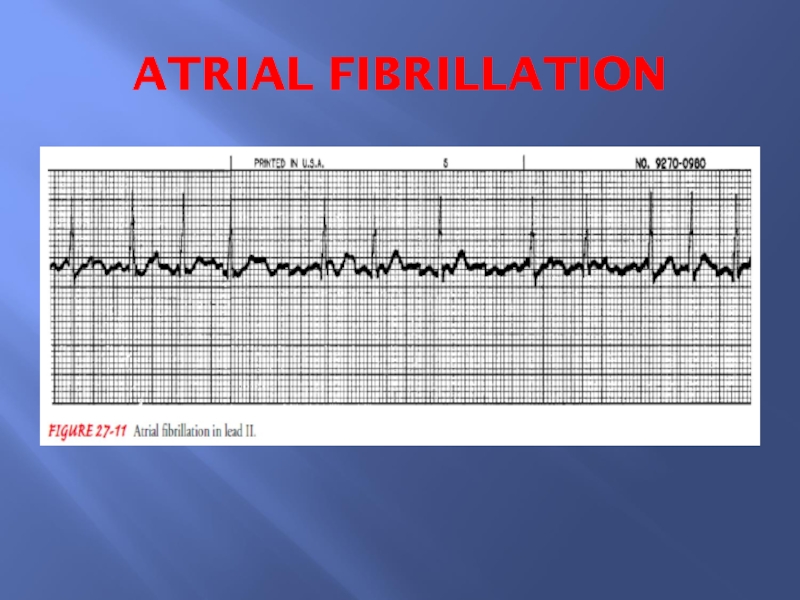
Atrial fibrillation (AF) -
A condition in which the electrical
signals come from the atria at a very fast and
erratic rate. The ventricles contract in an irregular manner because of the erratic signals coming from the atria.
The ECG shows normal but irregular QRS complexes, fine oscillations of the baseline (so-called fibrillation or f waves) and no P waves.
Common causes include CAD, valvular heart disease, hypertension, hyperthyroidism and others. In some patients no cause can be found 'lone' atrial fibrillation.
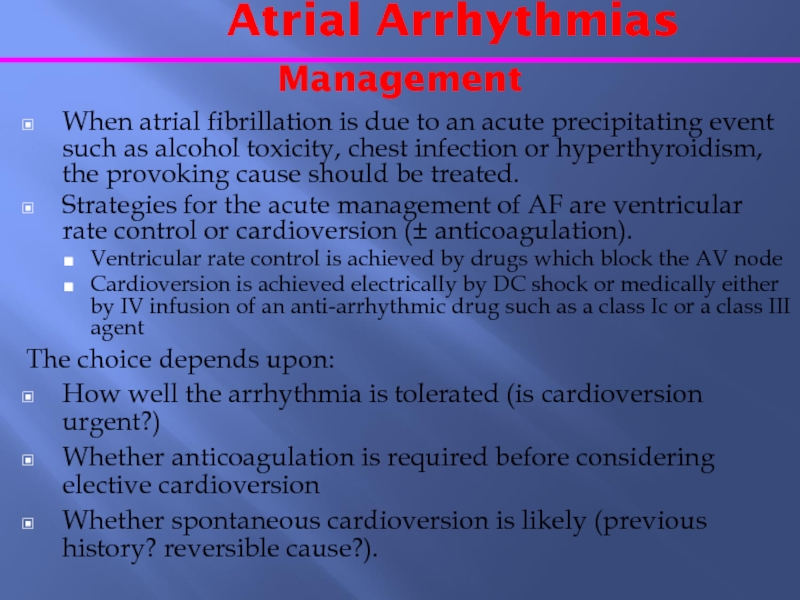
Слайд 30 Atrial Arrhythmias
Management
When atrial fibrillation is
due to an acute precipitating event such as alcohol toxicity,
chest infection or hyperthyroidism, the provoking cause should be treated.
Strategies for the acute management of AF are ventricular rate control or cardioversion (± anticoagulation).
Ventricular rate control is achieved by drugs which block the AV node
Cardioversion is achieved electrically by DC shock or medically either by IV infusion of an anti-arrhythmic drug such as a class Ic or a class III agent
The choice depends upon:
How well the arrhythmia is tolerated (is cardioversion urgent?)
Whether anticoagulation is required before considering elective cardioversion
Whether spontaneous cardioversion is likely (previous history? reversible cause?).
Слайд 31 Atrial Arrhythmias
Management (continue)
Patients are
anticoagulated with warfarin for 4 weeks before cardioversion.
Anticoagulants are
used to minimize the risk of thromboembolism associated with cardioversion unless atrial fibrillation is of less than 1-2 days' duration.
Transoesophageal echocardiography is being used to document the presence or absence of atrial thrombus as a guide to the necessity for long-term anticoagulation.
Слайд 32 Atrial Arrhythmias
Management
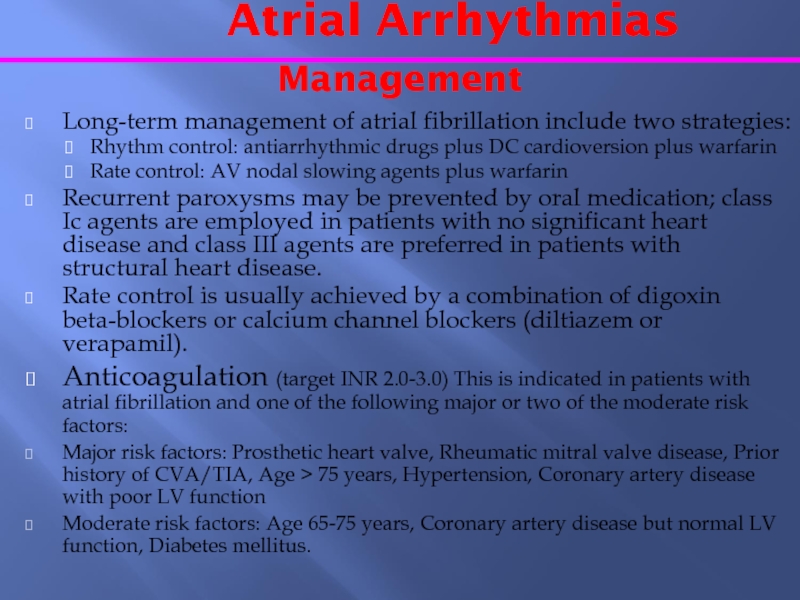
Long-term management of atrial
fibrillation include two strategies:
Rhythm control: antiarrhythmic drugs plus DC cardioversion
plus warfarin
Rate control: AV nodal slowing agents plus warfarin
Recurrent paroxysms may be prevented by oral medication; class Ic agents are employed in patients with no significant heart disease and class III agents are preferred in patients with structural heart disease.
Rate control is usually achieved by a combination of digoxin beta-blockers or calcium channel blockers (diltiazem or verapamil).
Anticoagulation (target INR 2.0-3.0) This is indicated in patients with atrial fibrillation and one of the following major or two of the moderate risk factors:
Major risk factors: Prosthetic heart valve, Rheumatic mitral valve disease, Prior history of CVA/TIA, Age > 75 years, Hypertension, Coronary artery disease with poor LV function
Moderate risk factors: Age 65-75 years, Coronary artery disease but normal LV function, Diabetes mellitus.
Слайд 33Ventricular Tachyarrhythmias
Ventricular tachyarrhythmias can be
considered under the following headings:
life-threatening
ventricular tachyarrhythmias (Sustained ventricular tachycardia and ventricular fibrillation)
torsades de
pointes
normal heart ventricular tachycardia
non-sustained ventricular tachycardia
ventricular premature beats
Слайд 34Ventricular Arrhythmias
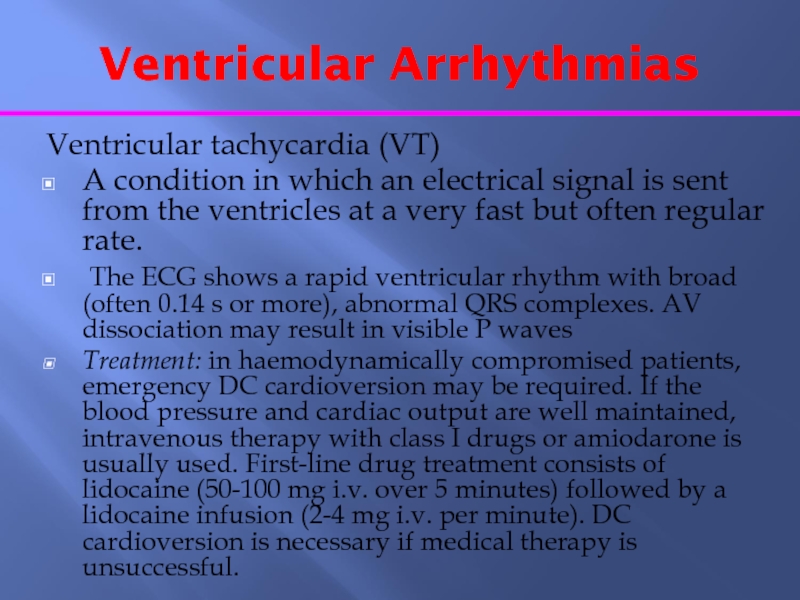
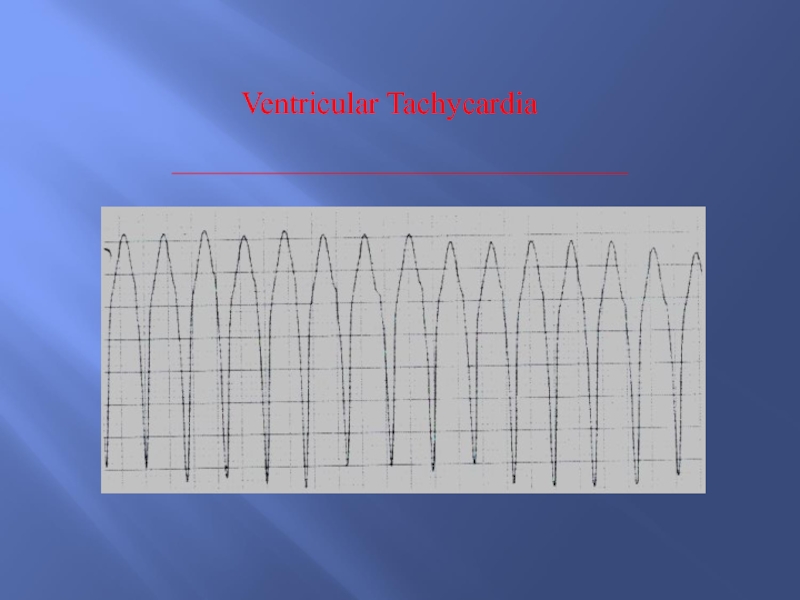
Ventricular tachycardia (VT)
A condition in which an electrical
signal is sent from the ventricles at a very fast
but often regular rate.
The ECG shows a rapid ventricular rhythm with broad (often 0.14 s or more), abnormal QRS complexes. AV dissociation may result in visible P waves
Treatment: in haemodynamically compromised patients, emergency DC cardioversion may be required. If the blood pressure and cardiac output are well maintained, intravenous therapy with class I drugs or amiodarone is usually used. First-line drug treatment consists of lidocaine (50-100 mg i.v. over 5 minutes) followed by a lidocaine infusion (2-4 mg i.v. per minute). DC cardioversion is necessary if medical therapy is unsuccessful.
Слайд 36Ventricular Arrhythmias
Ventricular fibrillation (VF)
A condition in which many electrical
signals are sent from the ventricles at a very fast
and erratic rate. As a result, the ventricles are unable to fill with blood and pump.
This rhythm is life-threatening because there is no pulse and complete loss of consciousness.
The ECG shows shapeless, rapid oscillations and there is no hint of organized complexes
A person in VF requires prompt defibrillation to restore the normal rhythm and function of the heart. It may cause sudden cardiac death. Basic and advanced cardiac life support is needed
Survivors of these ventricular tachyarrhythmias are, in the absence of an identifiable reversible cause (e.g. acute myocardial infarction, severe metabolic disturbance), at high risk of sudden death. Implantable cardioverter-defibrillators (ICDs) are first-line therapy in the management of these patients
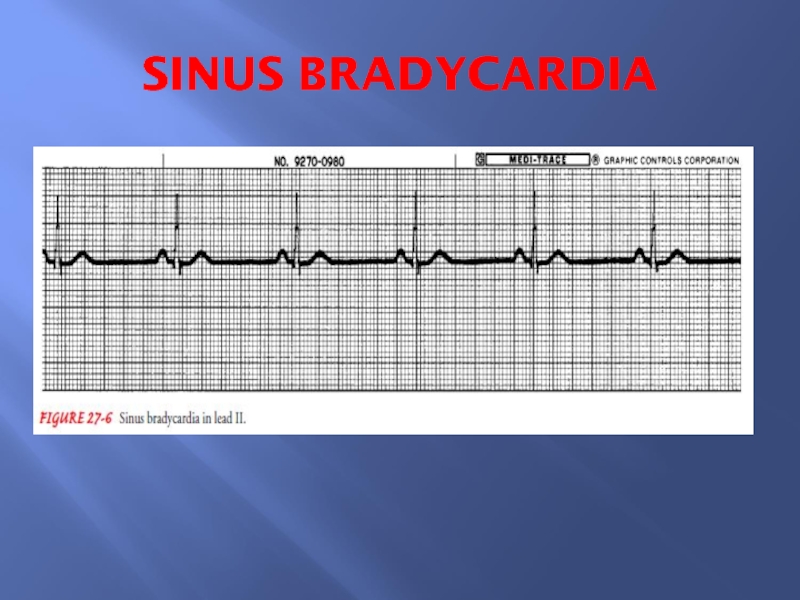
Слайд 38Bradycardias
Sinus Bradycardia
Physiological variant due to strong vagal tone or
atheletic training.
Rate as low as 50 at rest and 40
during sleep.
Common causes of sinus bradycardia include:
Extrinsic causes ;Hypothermia, hypothyroidism, cholestatic jaundice and raised intracranial pressure. Drug therapy with beta-blockers, digitalis and other antiarrhythmic drugs.
Intrinsic causes; Acute ischaemia and infarction of the sinus node (as a complication of acute myocardial infarction). Chronic degenerative changes such as fibrosis of the atrium and sinus node (sick sinus syndrome).
Слайд 40Bradycardias
Sick sinus syndrome
A condition in which the sinus node sends
out electrical signals either too slowly or too fast. There
may be alternation between too-fast and too-slow rates.
This condition may cause symptoms if the rate becomes too slow or too fast for the body to tolerate.
Chronic symptomatic sick sinus syndrome requires permanent pacing (AAI), with additional antiarrhythmic drugs (or ablation therapy) to manage any tachycardia element.
Thromboembolism is common in tachy-brady syndrome and patients should be anticoagulated unless there is a contraindication.
Слайд 41Atrioventricular (AV) Block
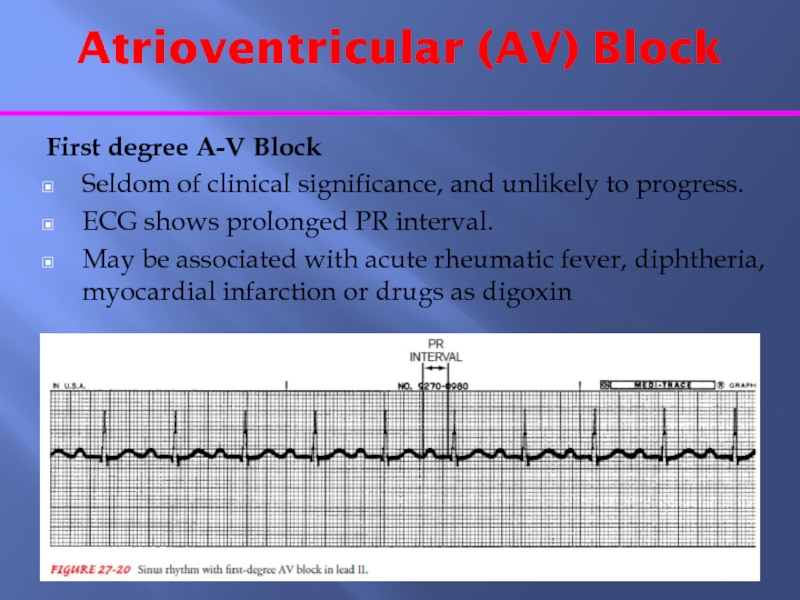
First degree A-V Block
Seldom of clinical significance,
and unlikely to progress.
ECG shows prolonged PR interval.
May be associated
with acute rheumatic fever, diphtheria, myocardial infarction or drugs as digoxin
Слайд 42Atrioventricular (AV) Block
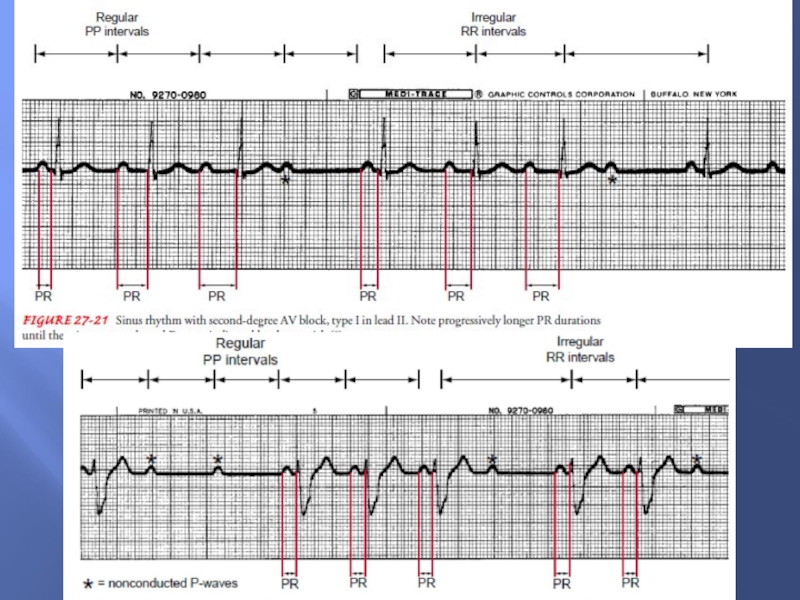
Second degree A-V Block
Mobitz type I (Wenchebach
phenomenon):
Gradually increasing P-R intervals culminating in an omission.
When isolated, usually
physiological and due to increased vagal tone and abolished by exercise and atropine.
Mobitz type II
The P wave is sporadically not conducted. Occurs when a dropped QRS complex is not preceded by progressive PR interval prolongation.
Pacing is usually indicated in Mobitz II block, whereas patients with Wenckebach AV block are usually monitored.
Слайд 44Atrioventricular (AV) Block
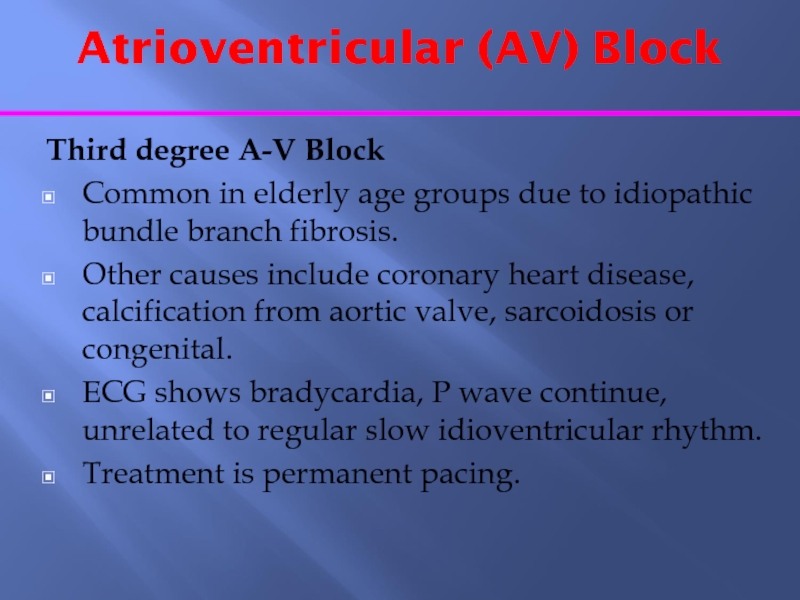
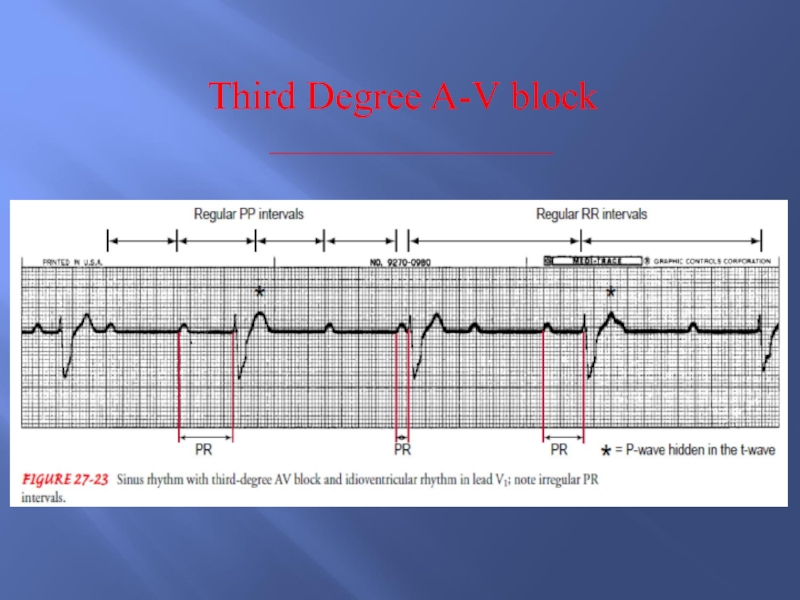
Third degree A-V Block
Common in elderly age
groups due to idiopathic bundle branch fibrosis.
Other causes include coronary
heart disease, calcification from aortic valve, sarcoidosis or congenital.
ECG shows bradycardia, P wave continue, unrelated to regular slow idioventricular rhythm.
Treatment is permanent pacing.
Слайд 46MANAGEMENT OF ARRHYTHMIAS
Pharmacological therapy.
Cardioversion.
Pacemaker therapy.
Surgical therapy e.g. aneurysmal excision.
Interventional
therapy “ablation”.
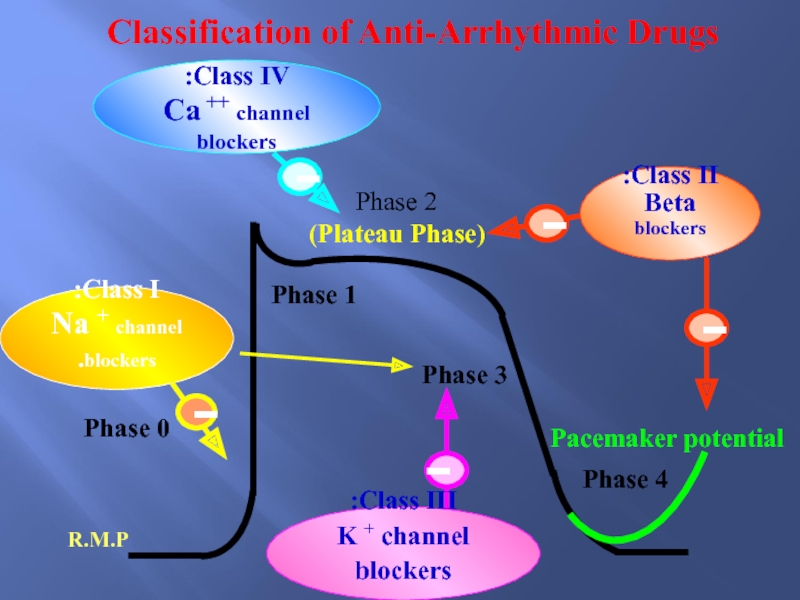
Слайд 47Phase 0
Phase 1
Phase 2
Phase 3
Phase 4
R.M.P
(Plateau Phase)
Class I:
Na +
channel blockers.
Pacemaker potential
Class III:
K + channel blockers
Class IV:
Ca ++
channel blockers
Class II:
Beta blockers
Classification of Anti-Arrhythmic Drugs
Слайд 48Classification of Antiarrhythmic Drugs
based on Drug Action
Слайд 49References
http://www.rnceus.com/ekg/ekgsecond2.html
ACLS Guidelines 2005
www.EMS-ED.net
http://www.doctorshangout.com/forum/topics/acls-algorithms-1
Слайд 50THANK YOU FOR YOUR
ATTENENTION!!!


![Cardiac Arrhythmias
Done by: Islamova Sh.
Group: 646 P.
Checked by: Seyitkaliev SVT Paroxysmal Supraventricular tachycardia [HR 160-250/min] Atrioventricular nodal re-entry tachycardia (AVNRT) It SVT Paroxysmal Supraventricular tachycardia [HR 160-250/min] Atrioventricular nodal re-entry tachycardia (AVNRT) It usually begins and ends rapidly, occurring](/img/thumbs/5f346aba20459e3401b5ad1cc2aeccbe-800x.jpg)