Слайд 1Graves’ Disease:
An Overview
Matthew Volk
Morning Report
November 17th, 2009
Слайд 2Epidemiology
Prevalence of hyperthyroidism in the general population is 1.2%
0.7% subclinical
hyperthyroidism
0.4% Graves’ Disease – most common etiology; note there is
overlap with the subclinical group
Graves’ Disease is more common in females (7:1 ratio)
Слайд 3Pathogenesis
An autoimmune phenomenon – presentation determined by ratio of antibodies
TSH
Receptor
Thyroid
Stimulating
Ab (TSAb)
Thyroid Stimulation
Blocking Ab (TSBAb)
Thyroid
+
-
Graves’ Disease
Autoimmune
Hypothyroidism
(Hashimoto’s)
Thyroglobulin Ab
Thyroid peroxidase
Ab (anti TPO)
Слайд 4The Classic Triad of Graves’ Disease
Hyperthyroidism (90%)
Ophthalmopathy (20-40%)
proptosis, ophthalmoplegia, conjunctival
irritation
3-5% of cases require directed treatment
Dermopathy (0.5-4.3%)
localized myxedema, usually pretibial
especially
common with severe ophthalmopathy
There is also a close association with autoimmune findings (e.g. vitiligo) and other autoimmune diseases (e.g. ITP)
Слайд 5Syndrome of Hyperthyroidism
Weight loss, heat intolerance
Thinning of hair, softening of
nails
Stare and eyelid lag
Palpitations, symptoms of heart failure
Dyspnea, decreased exercise
tolerance
Diarrhea
Frequency, nocturia
Psychosis, agitation, depression
Слайд 6Graves’ Ophthalmopathy
Antibodies to the TSH receptor also target retroorbital tissues
T-cell
inflammatory infiltrate -> fibroblast growth
Severe: exposure keratopathy, diplopia, com-pressive optic
neuropathy
Strong link with tobacco
Слайд 7Myxedema of Graves’
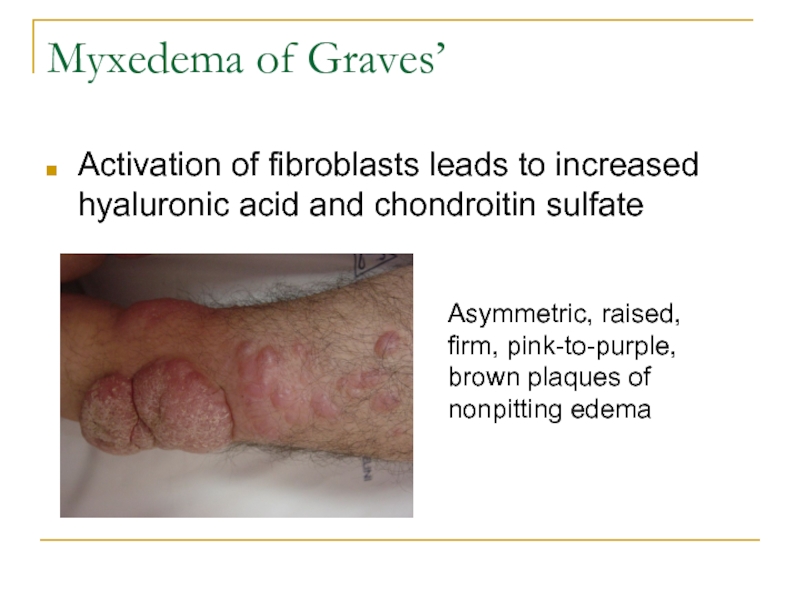
Activation of fibroblasts leads to increased hyaluronic acid
and chondroitin sulfate
Asymmetric, raised, firm, pink-to-purple, brown plaques of nonpitting
edema
Слайд 8Hyperthyroidism Differential
Graves’ Disease
Toxic Multinodular Goiter
Toxic Adenoma
Thyroiditis
silent (Hashimoto’s) – painless, often
post partum
subacute (de Quervain’s) – painful, post viral
drug-induced – amiodarone,
lithium, interferon
Thyrotoxicosis factitia
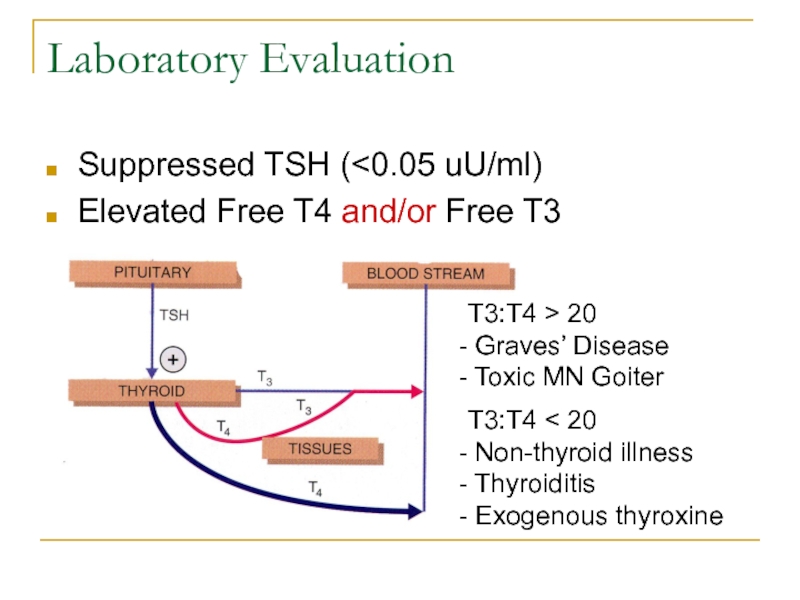
Слайд 9Laboratory Evaluation
Suppressed TSH (
> 20
Graves’ Disease
Toxic MN Goiter
T3:T4 < 20
Non-thyroid
illness
Thyroiditis
Exogenous thyroxine
Слайд 10It’s Good to be Free
Thyroxin is 99% bound to thyroid
binding globulin (TBG), albumin, and transthyretin
Elevated TBG in viral hepatitis,
pregnancy, and in patients taking estrogens and opiates
Decreased TBG binding with heparin, dilantin, valium, NSAIDs, lasix, carbamazepine, ASA
Measuring Free T4 instead of total T4 avoids this problem all together
Слайд 11Laboratory Evaluation
Direct measurement of TSH receptor antibodies (TSAb and TBAb)
Can
help with Graves diagnosis in confusing cases (as high as
98% sensitivity)
Can predict new-onset Graves’ in the post-partum period
Anti TPO Antibody and anti Tg Antibody
Can be mildly elevated in Graves’
Usually most active in Hashimoto’s
Слайд 12Diagnostic Imaging
Radioactive Iodine Uptake
Provides quantitative uptake (nl 5-25% after 24h)
Shows
distribution of uptake
Technetium-99 Pertechnetate Uptake
Distinguishes high-uptake from low-uptake
Faster scan –
only 30 minutes
Thyroid ultrasonography
Identifies nodules
Doppler can distinguish high from low-uptake
Слайд 13Immediate Medical Therapy
Thionamides – inhibit central production of T3 and
T4; immunosuppressive effect
Methimazole – once daily dosing
PTU – added peripheral
block of T4 to T3 conversion; preferred in pregnancy
Side effects: hives, itching; agranulocytosis, hepatotoxicity, vasculitis
Beta-blockade – decrease CV effects
High-dose iodine – Wolff-Chaikoff effect
Слайд 14Long-term Therapeutic Options
Continued Medical Management
Low dose (5-10mg/day of methimazole) for
12 to 18 months then withdraw therapy
Lasting remission in 50-60%
Radioiodine
Ablation
Discontinue any thionamides 3-5 days prior
Overall 1% chance of thyrotoxicosis exacerbation
Hypothyroidism in 10-20% at 1 yr, then 5% per yr
Lasting remission in 85%
Слайд 15Long-term Therapeutic Options
Total Thyroidectomy
Indications: suspicion for malignant nodule, comorbid need
for parathyroidectomy, radioactive ablation contraindicated, compressive goiter
Recent metaanalysis showed this
is the most cost effective if surgery is < $19,300.
Prep with 6 weeks thionamides, 2 weeks iodide
Hypoparathyroidism and/or laryngeal nerve damage in <2%
Lasting remission in 90%
Слайд 16Treatment of Ophthalmopathy
Mild Symptoms
Eye shades, artificial tears
Progressive symptoms (injection, pain)
Oral
steroids – typical dosage from 30-40mg/day for 4 weeks
Impending corneal
ulceration, loss of vision
Oral versus IV steroids
Orbital Decompression surgery
Слайд 17References
Alguire et al. MKSAP14 Endocrinology and Metabolism. 2006. 27-34.
Andreoli et
al. Cecil Essentials of Medicine. 6th Edition, 2004. 593-7.
Nayak, B
et al. Hyperthyroidism. Endocrinol Metab Clin N Am. 36 (2007) 617-656.
In H et al. Treatment options for Graves disease: a cost-effectiveness analysis. J Am Coll Surg. 2009 Aug;209(2):170-179.e1-2.
Stiebel-Kalish H et al. Treatment modalities for Graves' ophthalmopathy: systematic review and metaanalysis. J Clin Endocrinol Metab, August 2009, 94(8):2708–2716
Uptodate Online – Disorders that Cause Hyperthyroidism, Diagnosis of Hyperthyroidism, Cardiovascular Effects of Hyperthyroidism, Treatment of Graves Ophthalmopathy