Слайд 1Management of common infections in general practice:
Experiences from a
diagnose-prescribing survey in Sweden, Latvia and Lithuania
Uga Dumpis, Annika Hahlin,
Sonata Varvuolyte, Stephan Stenmark, Sarmīte Veide, Rolanda Valinteliene, Asta Jurkeviciene and Johan Struwe
European Journal of Clinical Microbiology & Infectious Diseases. https://doi.org/10.1007/s10096-017-3141-2
Слайд 4Ethical considerations
In Sweden, follow-up of antibiotic prescriptions is part of
ongoing quality assurance and patient
safety programs, and ethical approval is
not needed for collection of anonymized data.
In Lithuania, regulation was similar to that in Sweden and written consent from patient was not
required.
In Latvia, the study was approved by Pauls Stradins Clinical University Hospital Development Fund Ethical Committee as part of the National Research Programme BIOMEDICINE. In accordance with this decision, consent forms were not necessary since patients’ and doctors’ information was not collected.
Слайд 5Recruitment of participants
Centres and doctors in each participating region were
recruited through convenience sampling
In Sweden most GP practices had
a range of 3-10 GPs.
The Strama groups sent invitations the responsible doctor at every GP practise
In Stockholm also to each individual GP
The e-mail included invitations to a seminar for contact persons.
In Västerbotten invitation also via the county council´s intranet and also via e-mail.
In Latvia, family physicians are self-employed and usually located individually.
An e-mail signed by the head of the Latvian Family Physicians Association and chief investigator was sent to all selected GPs through the mailing list kept by the Family Physicians Association.
In Lithuania part of family physicians work in group practices, some in policlinics and very small number own single practices.
Invitations were sent via e-mail to primary health care centers and family physicians directly. Institute of Hygiene and Lithuanian Society of General Practitioners created the information-invitation form for study and invited all family doctors, who expressed willingness to participate, to introductory seminar.
Слайд 6Västerbotten county
Pop: 259.000
Perscription rate: 314/1000 inh/yr
(2nd lowest in
Sweden)
13/36 GP-stations participated
63 doctors
2150
visits,
405 patients with infections
Stockholm county
Pop: 2.019.000
Perscription rate: 419/1000 inh/yr
(highest in Sweden)
56/~230 GP-stations participated
464/~2000 doctors
4454 patients with infections
Lithuania
Pop: 3.390.000
21 GP-station participated
71 doctor participated
1472 patients with infections
Latvia
Pop: 2.200.000
~1500 GPs
69 doctors participated
1969 patients with infections
Слайд 7 Latvia Lithuania
Sweden
Number of patients with suspected
infection 1969 1524 4858
Source: Dumpis et al: European Journal of Clinical Microbiology & Infectious Diseases
https://doi.org/10.1007/s10096-017-3141-2
Слайд 8Most frequent reason for seeking a doctor
Source: Dumpis et al:
European Journal of Clinical Microbiology & Infectious Diseases
https://doi.org/10.1007/s10096-017-3141-2
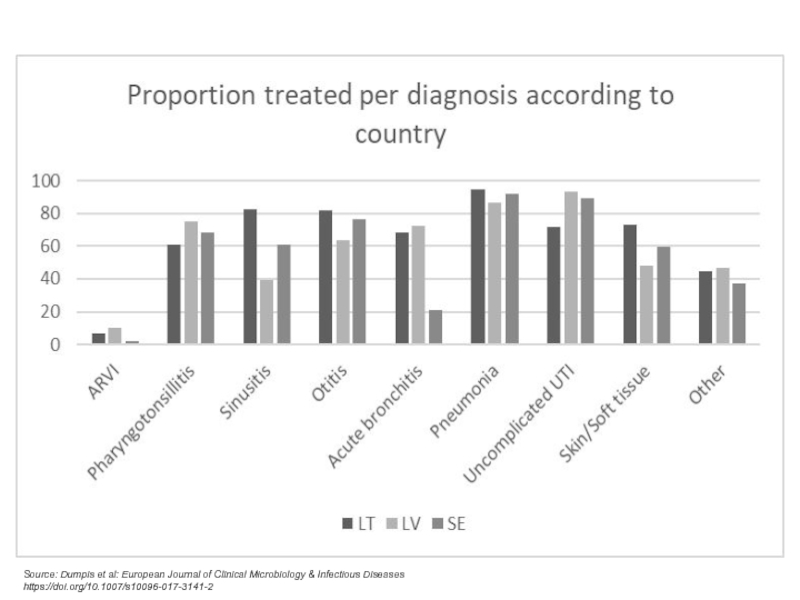
Слайд 9Source: Dumpis et al: European Journal of Clinical Microbiology &
Infectious Diseases
https://doi.org/10.1007/s10096-017-3141-2
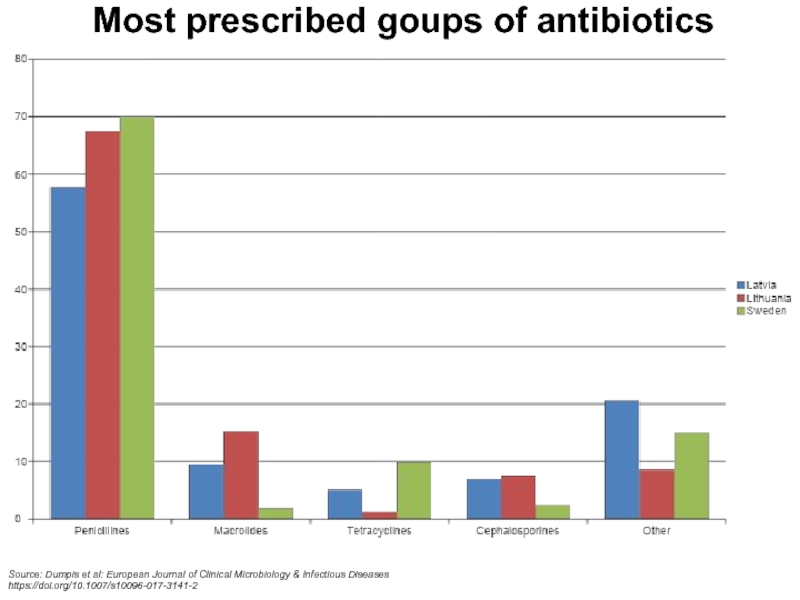
Слайд 10Most prescribed goups of antibiotics
Source: Dumpis et al: European Journal
of Clinical Microbiology & Infectious Diseases
https://doi.org/10.1007/s10096-017-3141-2
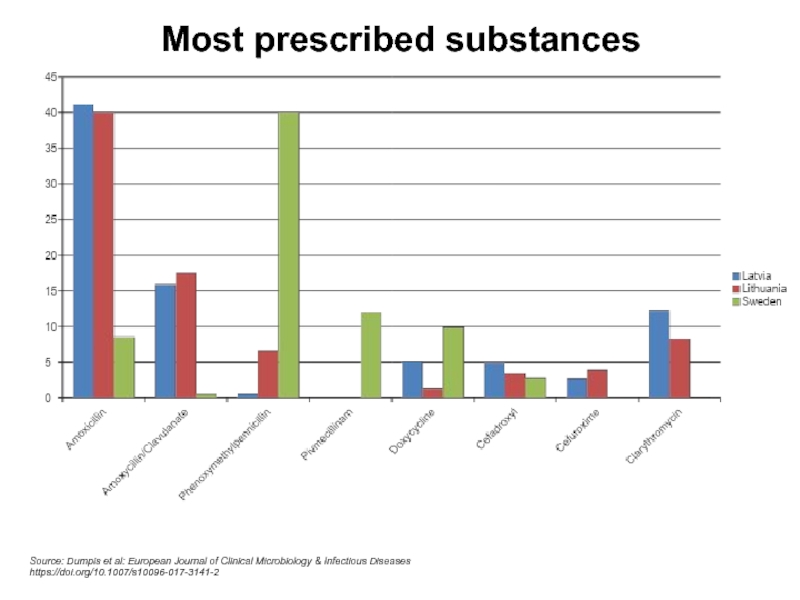
Слайд 11Most prescribed substances
Source: Dumpis et al: European Journal of Clinical
Microbiology & Infectious Diseases
https://doi.org/10.1007/s10096-017-3141-2
Слайд 12Main conclusions
On average, Swedish patients were older and waited longer
with symptoms
Latvia and Lithuania used more amoxicillin +/- clavulanante and
macrolides,
Sweden used more penicillin V and doxycykline
The protocol was easy to use and provided useful information for discussions about how to manage common infections in general practice
Important antibiotics were not avaiable, or comparatively expensive, in Latvia and Lithuania, increasing risk for use of more broad-spectrum antibiotics
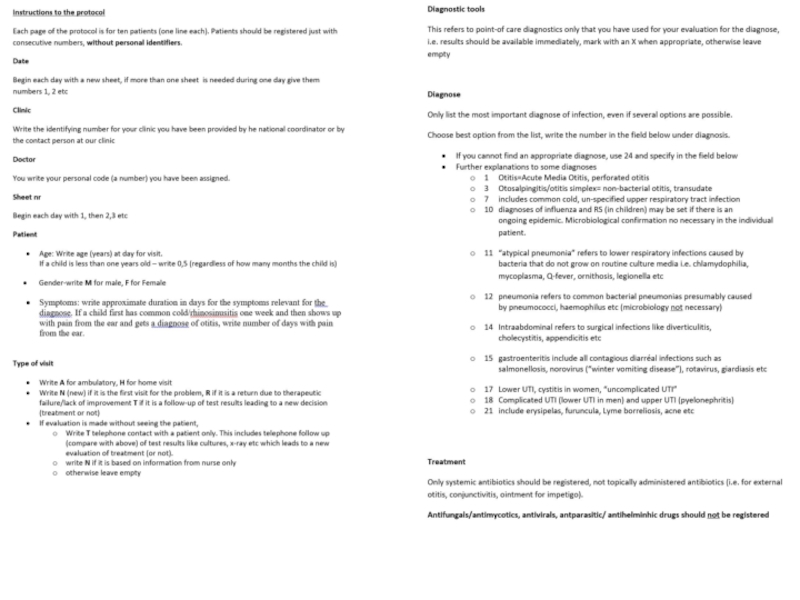
Слайд 14Planning and preparation for diagnose-prescribing survey in general practice
Define target
period for survey (one week, same in all regions)
Define coordinator/
trainer in each region
Define, and develop, database to enter manually completed protocols.
Decide whether data entry should be done at each unit or at regional level (recommended)
Define plan for feed-back to participating doctors/ centers
Слайд 15Plan recruitment and reach-out method
Define reach-out method
Invite practitioners/ practices to
participate.
Ask each practice interested in participation to nominate one
contact person
Participation should be voluntary and not involve financial incentives, except for costs for travel and housing for contact persons to attend work-shop/s
Слайд 16Prepare contact persons
Arrange information workshop for contact persons in each
region. Supply them with information material.
Assign each unit a
number for identification.
Contact persons go back and inform colleagues.
Give each doctor a random identifying number.
A second workshop/ information for contact persons a couple of weeks before survey might be useful
Distribute protocols unless they can be printed/ copied at participating clinics
Слайд 17Roles for contact persons before,
during and after the survey
Arrange
a meeting to inform colleagues and go the instructions for
the protocol,
answer (or pass on to the regional coordinator) questions regarding how to fill in the protocol
Contact person give heads up to colleagues,
remind them about their number, and
provide them with protocols and extra as needed
Contact person informs and regularly reminds during registration period
Denominator data: Collect data on total number of visits to all participating doctors during the study week (i.e. not only infections)
Contact person sends all completed protocols and denominator data to regional coordinator at the end of the study (unless it has been agreed that they should enter the data)
Participate in feed-back to participating doctors/ centers
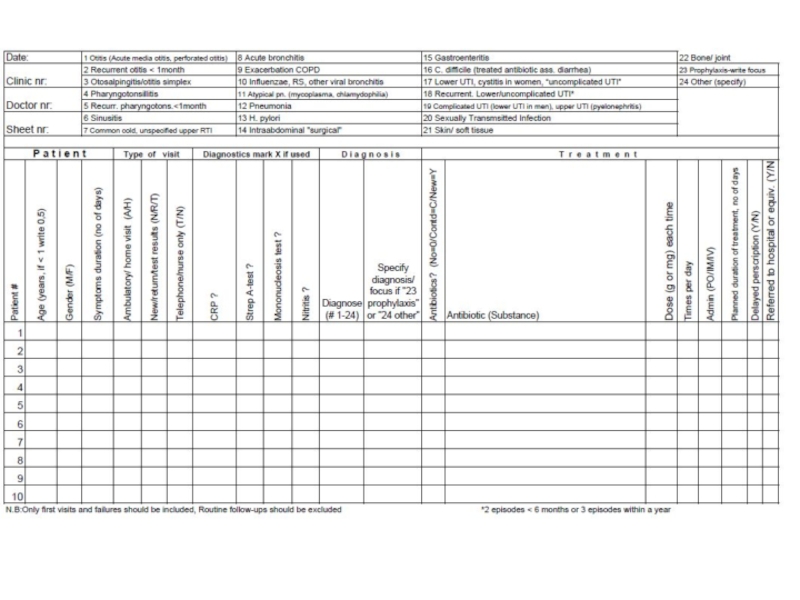
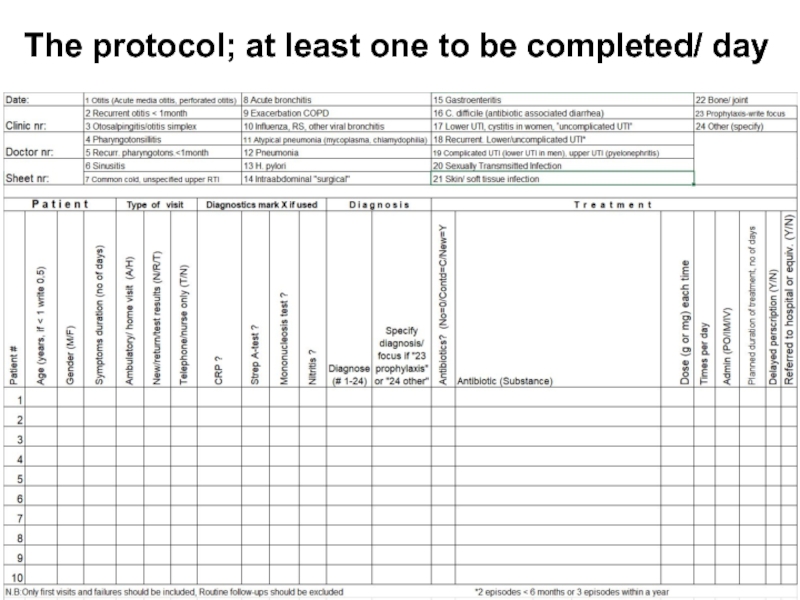
Слайд 18The protocol; at least one to be completed/ day