Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
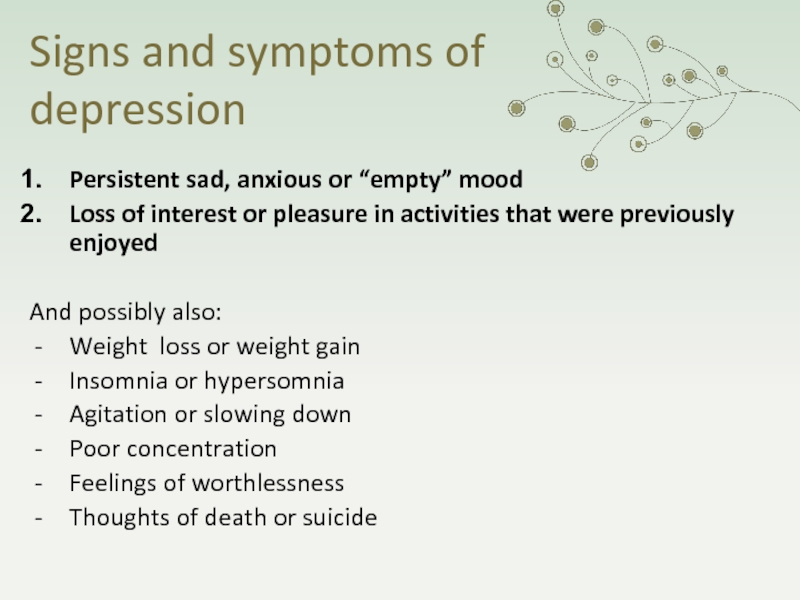
- Философия
- Химия
- Шаблоны, картинки для презентаций
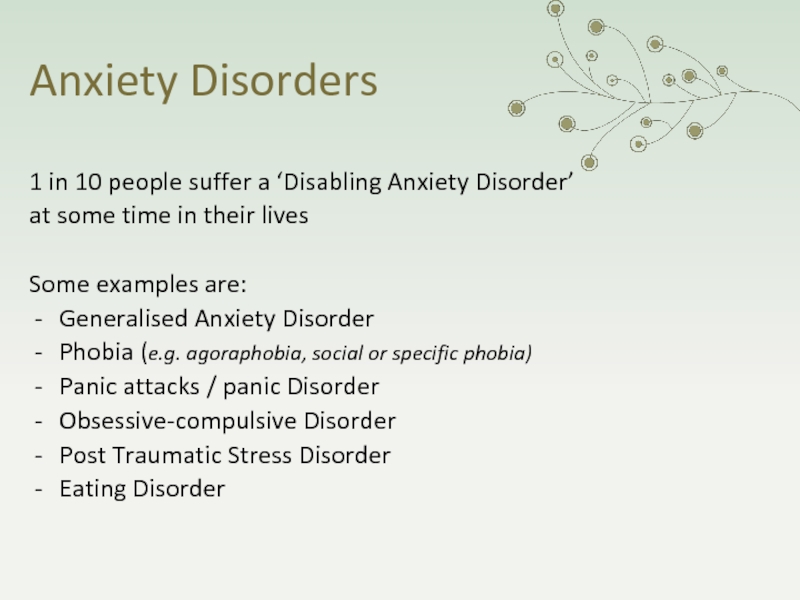
- Экология
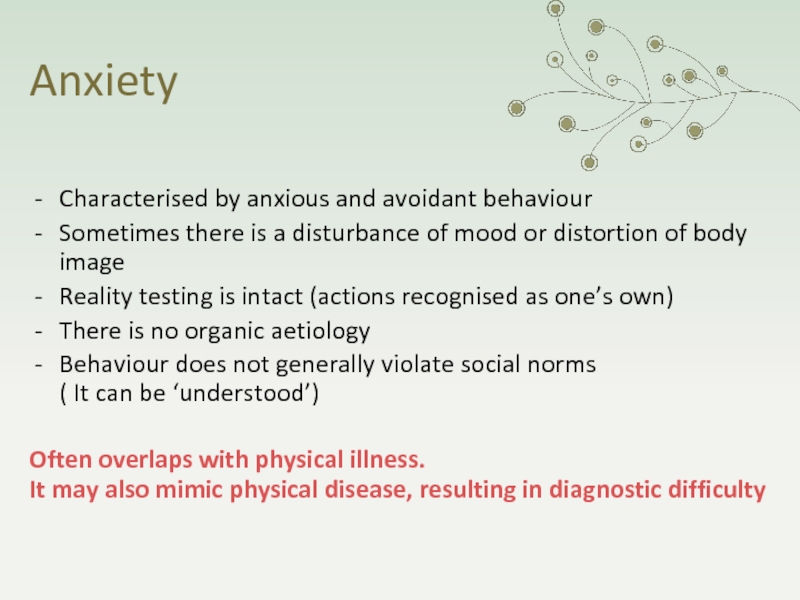
- Экономика
- Юриспруденция
Physiotherapy in Mental Health St. Petersburg May 2016 Josephine Bell Clinical
Содержание
- 1. Physiotherapy in Mental Health St. Petersburg May 2016 Josephine Bell Clinical
- 2. ObjectivesTo gain an awareness of the most
- 3. Mental illness is distinct from learning disability
- 4. A brief history of mental health
- 5. In 1845 the Lunatics Act decreed that
- 6. Слайд 6
- 7. Слайд 7
- 8. Initially people were “ committed
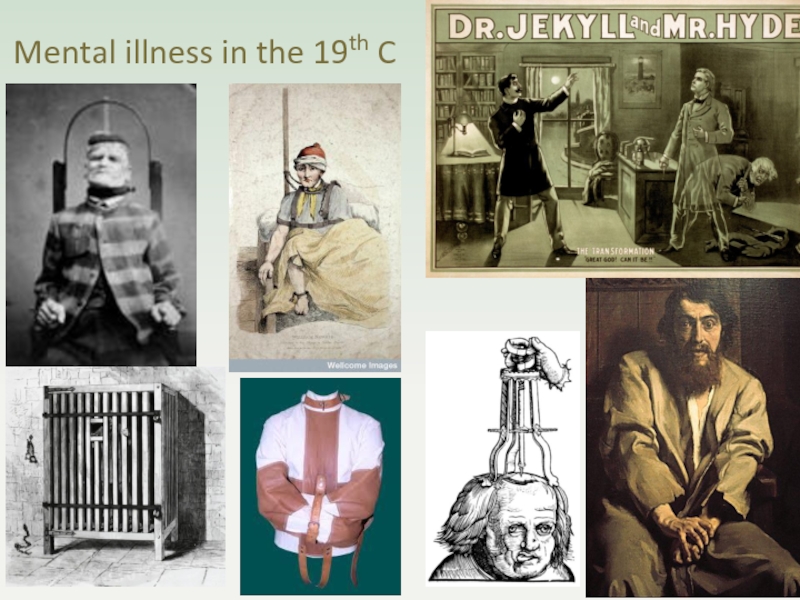
- 9. Mental illness in the 19th C
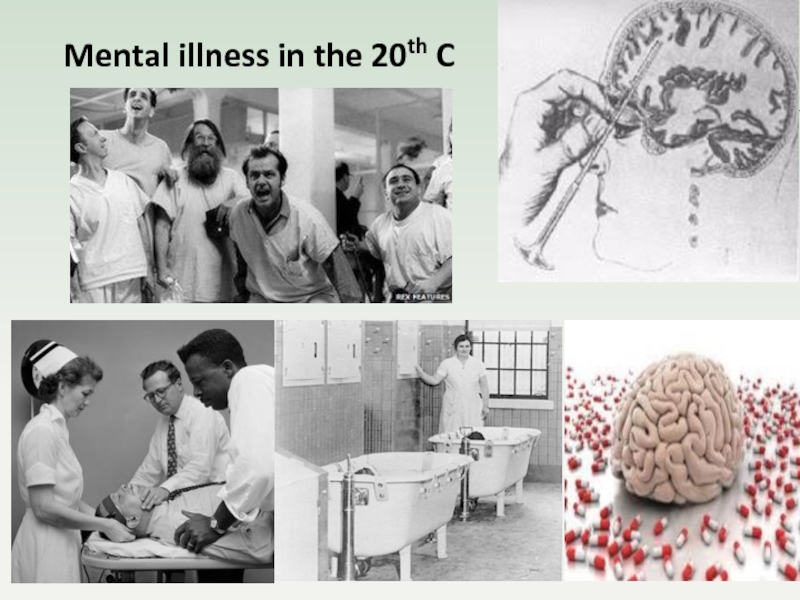
- 10. Mental illness in the 20th C
- 11. Слайд 11
- 12. Слайд 12
- 13. Is mental illness in the 21st C more fluffy?
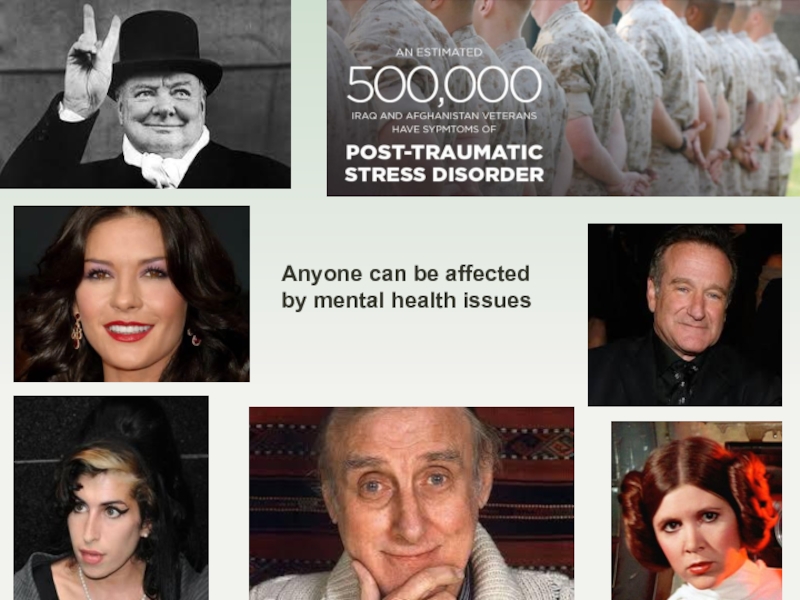
- 14. Anyone can be affected by mental health issues
- 15. 1 person in 4 in Britain
- 16. Mental state consists of:
- 17. Why do we need perceptions? They are
- 18. Examples of disorders of perceptionAuditory hallucinations
- 19. ThoughtsIdeasConceptsInternal dialogue
- 20. FeelingsSubjective emotional states that have psychological and physiological aspectse.g. happinesssadnessparanoiaangerfear
- 21. CognitionsMemory OrientationAttention and concentrationCalculationLanguage(insight)
- 22. BehavioursWhat we do: our ‘external’ actions in
- 23. Signs and symptoms of mental disorderDisordered
- 24. DepressionAffects 1 in 6 people, most commonly
- 25. Signs and symptoms of depressionPersistent sad,
- 26. Bipolar affective DisorderAffects about 1 in 100
- 27. Re. Bipolar Affective Disorder:
- 28. Anxiety Disorders1 in 10 people suffer a
- 29. AnxietyCharacterised by anxious and avoidant behaviourSometimes there
- 30. Physiological signs of anxietyIncreased muscle tension
- 31. PsychosisAffects 1 in 100 people at some
- 32. Symptoms are divided into positive &
- 33. What images do you get if you Google Schizophrenia in the UK?
- 34. The topics of mental health and illness
- 35. Mental illness is almost always multifactorial in
- 36. This fits well with the bio-psycho-social model adopted by physiotherapists... and allows for a holistic approach
- 37. Stigma and discriminationMany people in the UK
- 38. The best way to challenge stereotypes is
- 39. People with severe and enduring mental illness
- 40. Twice as likely to die from coronary
- 41. Why is this so?
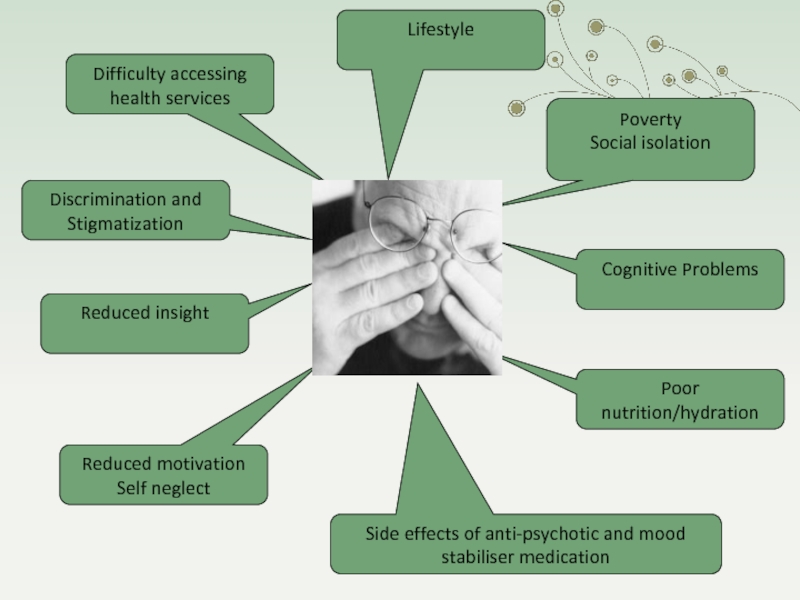
- 42. The inequalities cannot be explained by the
- 43. LifestyleDifficulty accessing health servicesPovertySocial isolationReduced motivationSelf neglectReduced
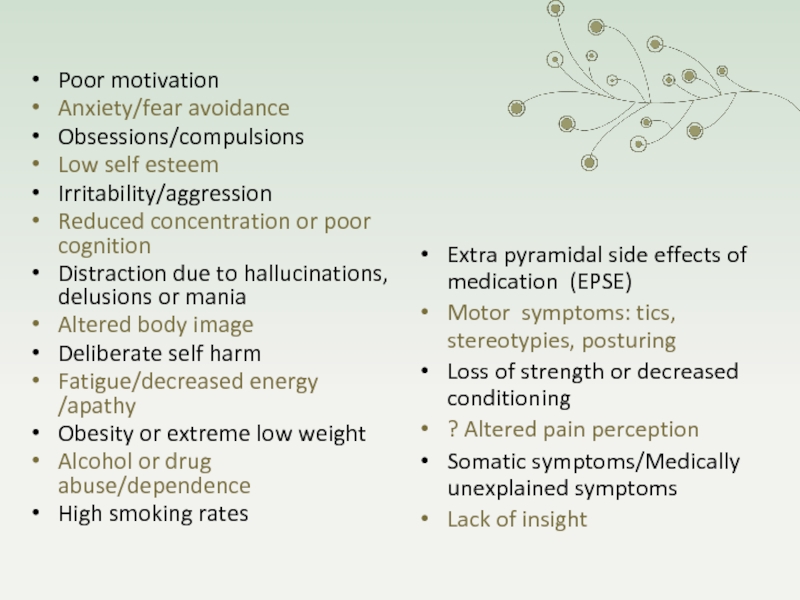
- 44. There are many problems secondary to mental illness that may challenge physiotherapeutic intervention
- 45. Слайд 45
- 46. Poor motivationAnxiety/fear avoidanceObsessions/compulsionsLow self esteemIrritability/aggressionReduced concentration or
- 47. Слайд 47
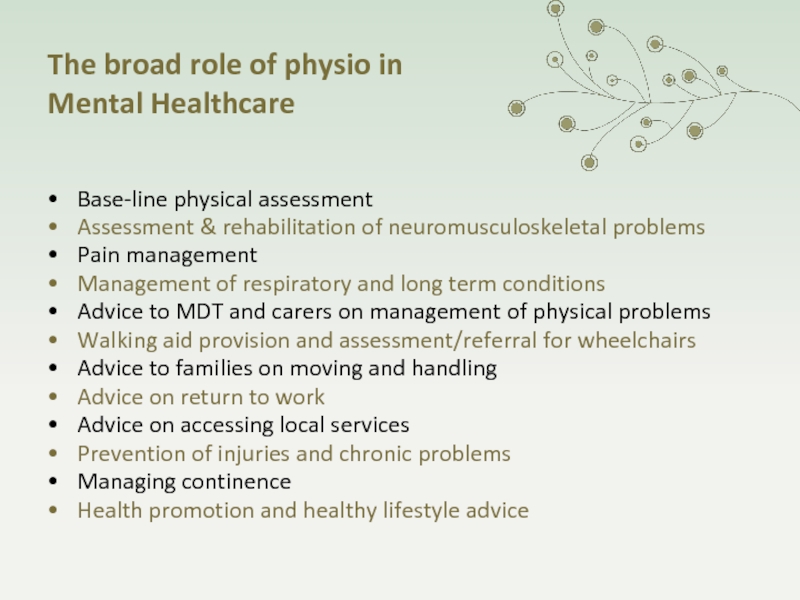
- 48. The broad role of physio
- 49. How do we adapt ?Provide a private
- 50. EngagementEngagement is always a priorityUse effective and
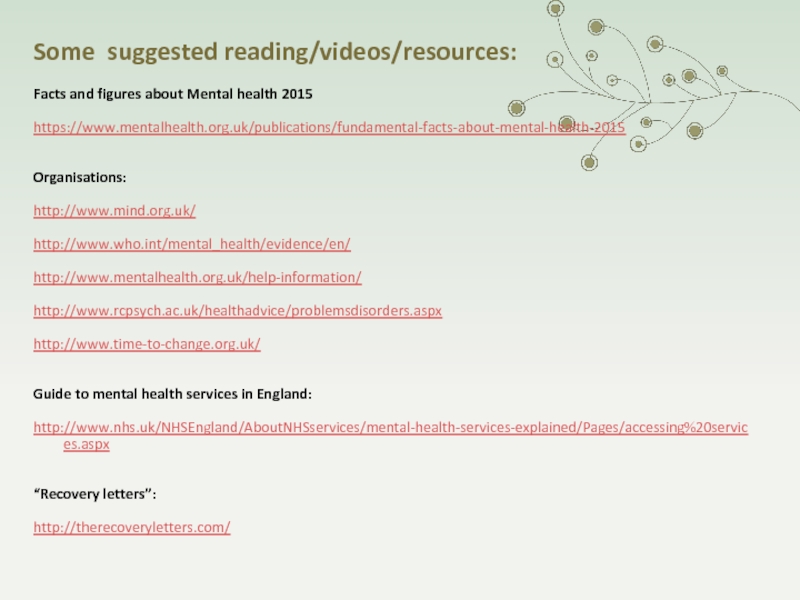
- 51. Some suggested reading/videos/resources:Facts and figures about Mental health 2015https://www.mentalhealth.org.uk/publications/fundamental-facts-about-mental-health-2015Organisations:http://www.mind.org.uk/http://www.who.int/mental_health/evidence/en/http://www.mentalhealth.org.uk/help-information/http://www.rcpsych.ac.uk/healthadvice/problemsdisorders.aspxhttp://www.time-to-change.org.uk/Guide to mental health services in England:http://www.nhs.uk/NHSEngland/AboutNHSservices/mental-health-services-explained/Pages/accessing%20services.aspx“Recovery letters”:http://therecoveryletters.com/
- 52. Слайд 52
- 53. Thank you for listening
- 54. Скачать презентанцию
Слайды и текст этой презентации
Слайд 1 Physiotherapy in Mental Health St. Petersburg May 2016 Josephine Bell Clinical Specialist Physiotherapist South
West London & St. George’s Mental Health NHS Trust
Слайд 2Objectives
To gain an awareness of the most common mental health
problems and how people are affected by them
To develop and
understanding of how a physiotherapist can adapt their treatment to help people with significant mental health problems
Слайд 3
Mental illness is distinct from learning disability (although there may
be some overlap)
What types of problems are classed
as mental health
conditions?Слайд 4A brief history of mental health
in the United Kingdom
Prior
to the 19th © most people with mental illness were
cared for either by their families or the local parish, or they resorted to begging. Later they were assigned to the ‘Poorhouses’.There were a few private ‘madhouses’ but these were only for the privileged few and they were run by businessman for profit.
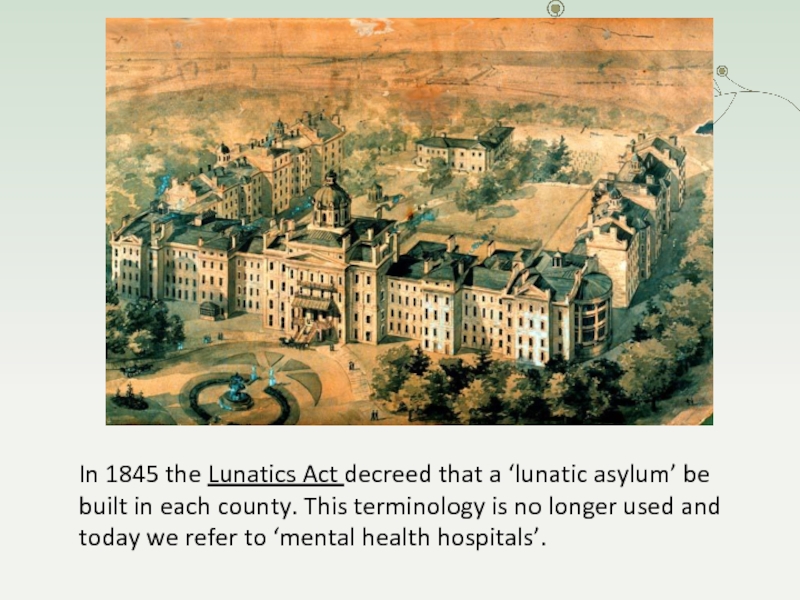
Слайд 5In 1845 the Lunatics Act decreed that a ‘lunatic asylum’
be built in each county. This terminology is no longer
used and today we refer to ‘mental health hospitals’.Слайд 8 Initially people were “ committed “ to an
asylum by family members or people of authority
It was not
until the ‘Mental Treatment Act’ of 1930 that voluntary admission became possibleHowever informal admission did not become the norm until the 1960s
Слайд 15 1 person in 4 in Britain will experience some
kind of mental health problem in the course of a
year90% are treated locally by their local doctors
The remaining 10% will require specialist services
Слайд 17Why do we need
perceptions?
They are the means by which
we experience and make sense of the world about us:
vision
hearingtouch
taste
smell
kinaesthesis
Слайд 18Examples of disorders
of perception
Auditory hallucinations
(noises, music, voices heard
in the absence of external stimulus –
strongly associated
with schizophrenia)
Visual hallucinations
(should suggest the possibility of an organic disorder but also can
occur with severe depression or schizophrenia)
Tactile hallucinations (e.g. of insects crawling under the skin:
common in cocaine abuse and sometimes schizophrenia)
Hallucinations of taste and smell (less common in mental
health conditions. May occur with temporal lobe epilepsy)
Слайд 20Feelings
Subjective emotional states that have
psychological and physiological aspects
e.g.
happiness
sadness
paranoia
anger
fear
Слайд 22Behaviours
What we do:
our ‘external’ actions in relation to the
world about us (the physical and social world)
Слайд 23Signs and symptoms of
mental disorder
Disordered perception
(Auditory, visual or
tactile hallucinations)
Disordered thinking
(as in Schizophrenia, OCD & psychotic depression)
Disordered
mood(anxiety, depression, phobia, mania)
Disordered body image
(Anorexia Nervosa and Body Dysmorphic Disorder)
Слайд 24Depression
Affects 1 in 6 people, most commonly from 25 –
44 years of age
The Science of Depression:
https://www.youtube.com/watch?v=GOK1KFFIQI
Слайд 25Signs and symptoms of
depression
Persistent sad, anxious or “empty” mood
Loss
of interest or pleasure in activities that were previously enjoyed
And
possibly also:Weight loss or weight gain
Insomnia or hypersomnia
Agitation or slowing down
Poor concentration
Feelings of worthlessness
Thoughts of death or suicide
Слайд 26Bipolar affective Disorder
Affects about 1 in 100 adults
As well
as becoming low in mood, some people can also become
‘high’ as in bipolar affective disorder, the signs and symptoms of which are:Elated or exalted mood
Reduced need for sleep
Increased energy and ideas
Racing and/or grandiose thoughts
Rapid talking
Irritability
Increased sexual desire
Inappropriate social behaviour (disinhibition)
Слайд 28Anxiety Disorders
1 in 10 people suffer a ‘Disabling Anxiety Disorder’
at
some time in their lives
Some examples are:
Generalised Anxiety Disorder
Phobia
(e.g. agoraphobia, social or specific phobia)Panic attacks / panic Disorder
Obsessive-compulsive Disorder
Post Traumatic Stress Disorder
Eating Disorder
Слайд 29Anxiety
Characterised by anxious and avoidant behaviour
Sometimes there is a disturbance
of mood or distortion of body image
Reality testing is intact
(actions recognised as one’s own)There is no organic aetiology
Behaviour does not generally violate social norms ( It can be ‘understood’)
Often overlaps with physical illness.
It may also mimic physical disease, resulting in diagnostic difficulty
Слайд 30Physiological signs
of anxiety
Increased muscle tension
- including tension headaches, restlessness
and tremor
Autonomic arousal with a release of Adrenaline leading to:
-
Raised heart rate/palpitations
- Increased perspiration
- Raised heart rate/palpitation
- Raised respiratory rate
- Dryness of mouth, loss of appetite
- Bowel/bladder over-activityСлайд 31Psychosis
Affects 1 in 100 people at some time in their
lives
with 10-15% developing long term difficulties
(enduring mental illness,
usually Schizophrenia)The most difficult of all syndromes to describe and define:
- The definition has varied and is still under some dispute
- Not a ‘split personality’ or ‘multiple personalities’
- Many varieties of clinical picture
- A change in chemical messengers in the brain results in thought,
mood, perception and behavioural disturbance
- It is an episodic condition that usually fluctuates
- Many patients are not aware/do not accept that they are unwell
Слайд 32Symptoms are divided into
positive & negative
Positive
- Disordered
thinking
- Delusions
- Hallucinations
- Agitation
- Preoccupation or agitation
Negative- Poor motivation
- Depression
- Low self-esteem
- Social withdrawal
- Self-neglect
Слайд 34The topics of mental health and illness have always
roused
controversy and raised many questions.
Questions such as :
What behaviour
is ‘normal’? What is being ‘rational’?
Are problems biological or functional?
- Should we treat patterns of thinking and behaviour as medical problems?
Opinions have, and probably always will, vary about the best way to define and treat mental health problems
Mental illness is controversial:
Слайд 35Mental illness is almost always
multifactorial in nature
Physiological
Psychological
Social, cultural & economic
factors
All need to be considered !
Слайд 36This fits well with the bio-psycho-social model adopted by physiotherapists
...
and allows for a holistic approach
Слайд 37Stigma and discrimination
Many people in the UK with mental health
problems report experiencing stigma and discrimination from society, friends, family
and health care professionalsStigma and discrimination have a negative impact on mental health problems and can trap people in a cycle of illness
However progress is being made and people are becoming more willing to disclose, talk about and seek treatment for mental health problems
Слайд 38The best way to challenge stereotypes is through first hand
contact with people with mental health problems
Слайд 39
People with severe and enduring mental illness have poor physical
health compared to the wider population
Their life expectancy is ~
10 - 20 years less than the averageСлайд 40Twice as likely to die from coronary heart disease as
the general population
Four times more likely to die from
respiratory diseaseTwice as likely to have Diabetes
(many people with Schizophrenia have multiple risk factors for type 2 Diabetes
such as a family history of Diabetes, obesity, sedentary lifestyle and smoking)
They also suffer more from hypertension, CVA, obesity and infections
Physical health problems
Слайд 42The inequalities cannot be explained by the mental health problem
alone.
The reasons are complex!
Слайд 43Lifestyle
Difficulty accessing health services
Poverty
Social isolation
Reduced motivation
Self neglect
Reduced insight
Poor nutrition/hydration
Side effects
of anti-psychotic and mood stabiliser medication
Discrimination and Stigmatization
Cognitive Problems
Слайд 44
There are many problems secondary to mental illness that may
challenge physiotherapeutic intervention
Слайд 46
Poor motivation
Anxiety/fear avoidance
Obsessions/compulsions
Low self esteem
Irritability/aggression
Reduced concentration or poor cognition
Distraction due
to hallucinations, delusions or mania
Altered body image
Deliberate self harm
Fatigue/decreased energy
/apathyObesity or extreme low weight
Alcohol or drug abuse/dependence
High smoking rates
Extra pyramidal side effects of medication (EPSE)
Motor symptoms: tics, stereotypies, posturing
Loss of strength or decreased conditioning
? Altered pain perception
Somatic symptoms/Medically unexplained symptoms
Lack of insight
Слайд 48
The broad role of physio in
Mental Healthcare
Base-line physical assessment
Assessment
& rehabilitation of neuromusculoskeletal problems
Pain management
Management of respiratory and long
term conditionsAdvice to MDT and carers on management of physical problems
Walking aid provision and assessment/referral for wheelchairs
Advice to families on moving and handling
Advice on return to work
Advice on accessing local services
Prevention of injuries and chronic problems
Managing continence
Health promotion and healthy lifestyle advice
Слайд 49How do we adapt ?
Provide a private and informal, but
safe environment
Try to build a therapeutic relationship based on honesty
and trustNon judgemental and empathic approach
Flexible appointment times and location
Flexible DNA/discharge policy
Longer/shorter treatment sessions, as needed
Adapt for cognitive factors: memory, attention etc.
Consider motivation, self esteem, insight
Adapt assessment and treatment techniques
Слайд 50Engagement
Engagement is always a priority
Use effective and sensitive communication
Initial aim
is to ‘hear about their story’
Facilitate them to set their
own goals and own their treatment programmeFacilitate motivation by demonstrating interest and making them feel valued
Make it informal: show empathy, curiosity
Assess in a ‘chatty’ style but help them to stay focussed
Make them feel understood and taken seriously
Cease if necessary (e.g. insufficient attention, irritability or aggression)
Don’t take rejection personally
Adopt a truly holistic approach