Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Chapter 15 – The Respiratory System
Содержание
- 1. Chapter 15 – The Respiratory System
- 2. SummaryIntroductionAnatomy and air flowRespirationMechanics of BreathingGas ExchangeRegulation of Breathing
- 3. IntroductionThe respiratory system is designed to perform
- 4. AnatomyThe respiratory system is often divided into
- 5. AnatomyRespiratory mucosaLines most of the air distribution
- 6. Слайд 6
- 7. AnatomyRespiratory mucosaThe layer of mucus traps dust,
- 8. Anatomy and Air FlowAir enters the respiratory
- 9. Anatomy and Air FlowNasal cavitiesParanasal sinuses: frontal,
- 10. Слайд 10
- 11. Слайд 11
- 12. Anatomy and Air FlowNasal cavitiesAs air moves
- 13. Anatomy and Air FlowPharynx – about 5
- 14. Anatomy and Air FlowPharynxThe right and left
- 15. Слайд 15
- 16. Anatomy and Air FlowLarynx = “voice box”Located
- 17. Слайд 17
- 18. Anatomy and Air FlowLarynxGlottis – space between
- 19. Слайд 19
- 20. Anatomy and Air FlowTrachea – “windpipe” is
- 21. Anatomy and Air FlowTracheaChoking on food and
- 22. Слайд 22
- 23. Anatomy and Air FlowBronchi, bronchioles and alveoli
- 24. Anatomy and Air FlowBronchi, bronchioles and alveoliBronchioles
- 25. Слайд 25
- 26. Anatomy and Air FlowBronchi, bronchioles and alveoliAlveoli
- 27. Слайд 27
- 28. Anatomy and Air FlowBronchi, bronchioles and alveoliThe
- 29. AnatomyLungsRight lung has 3 lobes, left lungs has 2 lobes.Apex =Base =
- 30. AnatomyPleuraSerous membranes that cover the outer surface
- 31. AnatomyPleuraPleurisy – inflammation of the pleura that
- 32. RespirationPulmonary ventilation (or ventilation): breathing, the process
- 33. RespirationInternal respiration – process by which an
- 34. Mechanics of BreathingMuscles – control the size
- 35. Mechanics of BreathingPulmonary ventilation has 2 phases:Inspiration
- 36. Mechanics of BreathingExpirationPassive process that begins when
- 37. Слайд 37
- 38. Gas ExchangeBlood is pumped out of the
- 39. Gas ExchangeBlood flowing toward the lungs is
- 40. Gas ExchangeCO2 moves into the lungs and
- 41. Слайд 41
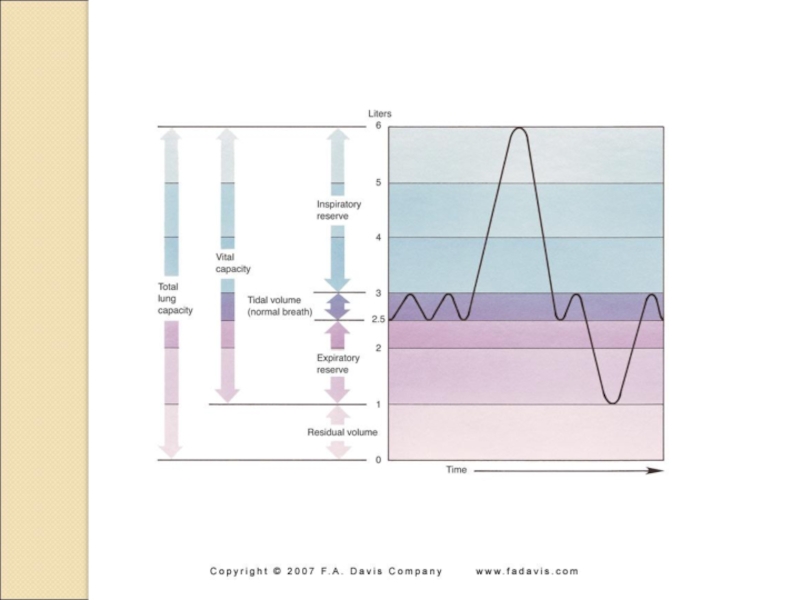
- 42. Respiratory FunctionSpirometer –Tidal volume – Vital capacity –
- 43. Respiratory FunctionExpiratory reserve – amount of air
- 44. Слайд 44
- 45. Regulation of RespirationNormal respiration depends on proper
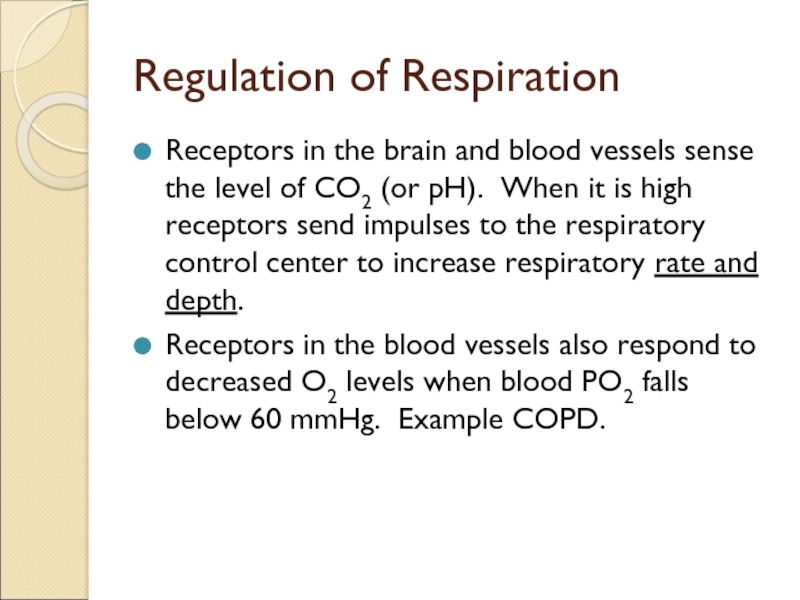
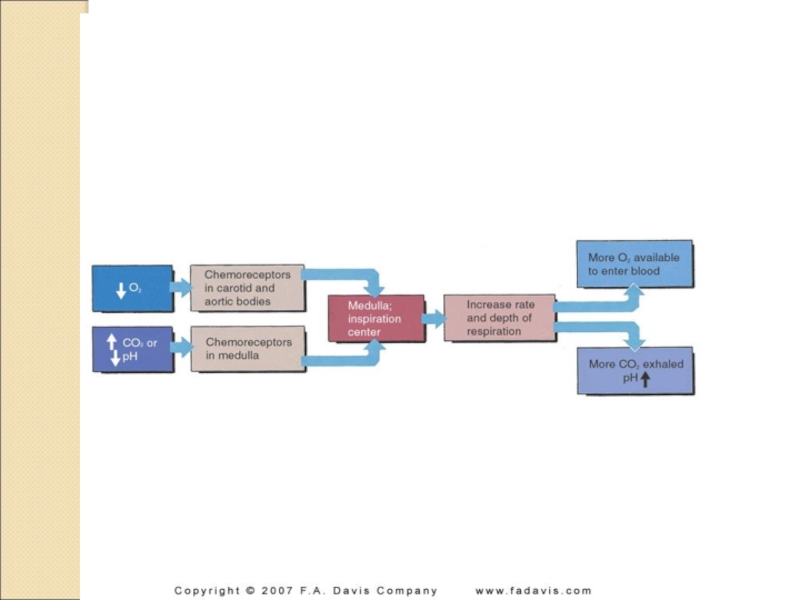
- 46. Regulation of RespirationReceptors in the brain and
- 47. Слайд 47
- 48. Regulation of RespirationThe 2 most important control
- 49. Слайд 49
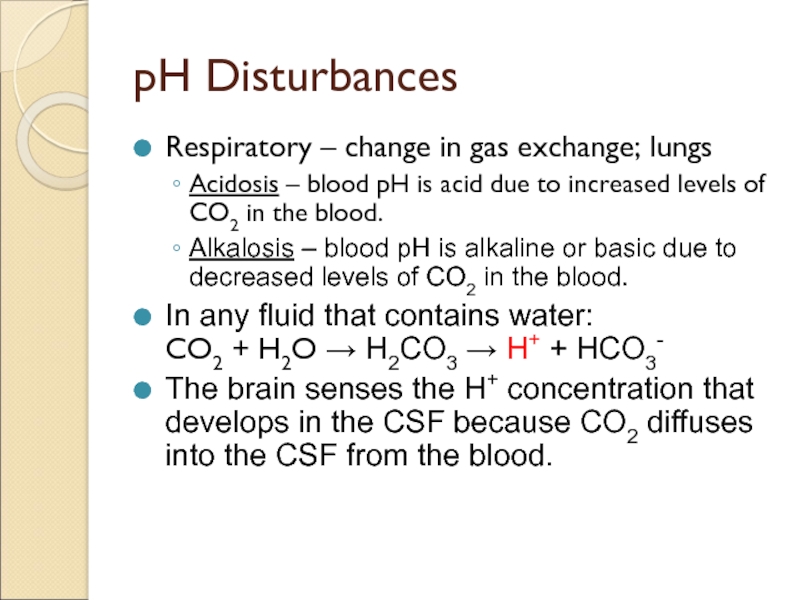
- 50. pH DisturbancesRespiratory – change in gas exchange;
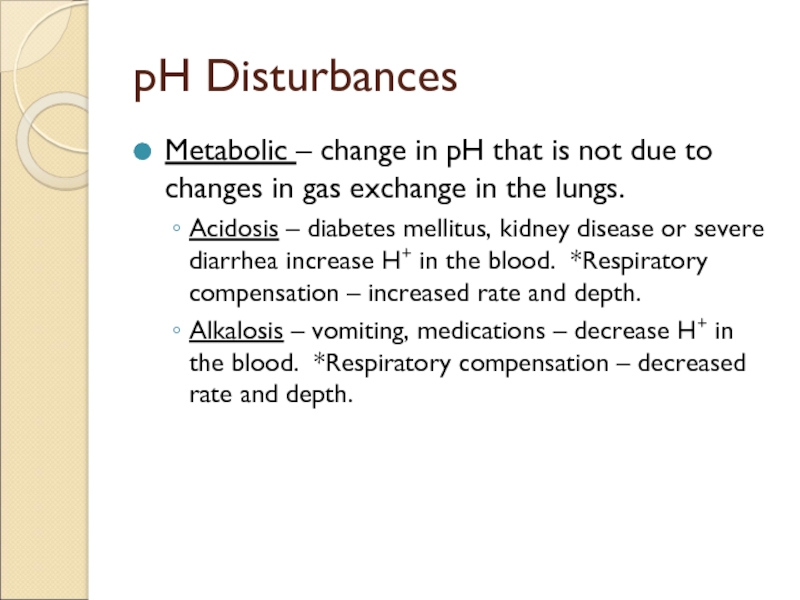
- 51. pH DisturbancesMetabolic – change in pH that
- 52. Скачать презентанцию
SummaryIntroductionAnatomy and air flowRespirationMechanics of BreathingGas ExchangeRegulation of Breathing
Слайды и текст этой презентации
Слайд 2Summary
Introduction
Anatomy and air flow
Respiration
Mechanics of Breathing
Gas Exchange
Regulation of Breathing
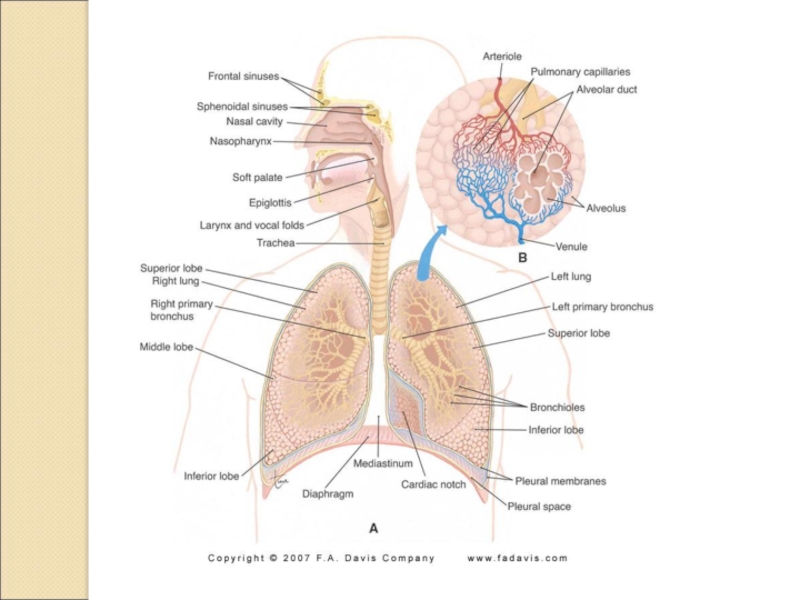
Слайд 4Anatomy
The respiratory system is often divided into upper and lower
tracts or divisions.
Upper tract - located outside the thoracic cavity
includes the nose, pharynx and larynx.Lower tract - located within the thoracic cavity includes the trachea, bronchial tree and the lungs.
URI or LRI?
Слайд 5Anatomy
Respiratory mucosa
Lines most of the air distribution tubes in the
system.
Layered with protective mucus that serves as the most important
air purification mechanism. More than 125 ml of respiratory mucus is produced daily.Слайд 7Anatomy
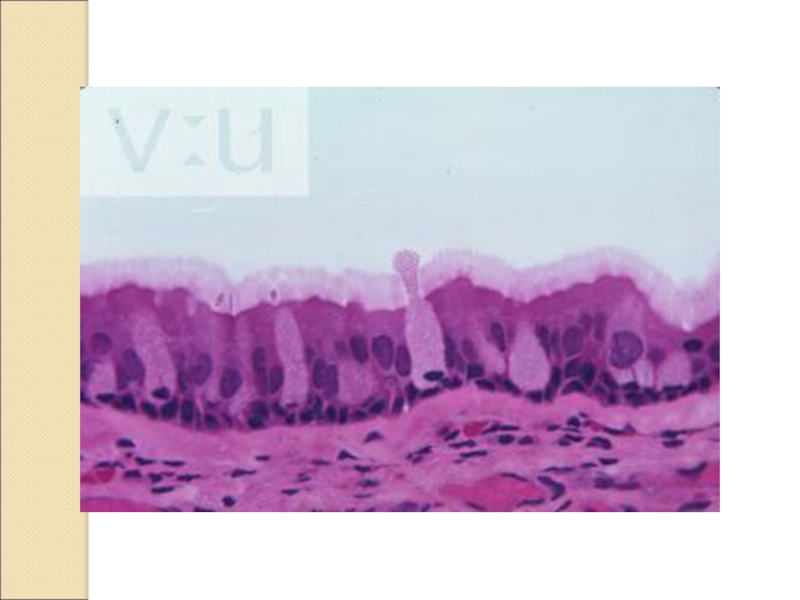
Respiratory mucosa
The layer of mucus traps dust, pathogens, etc and
moves upward to the pharynx with the help of the
cilia on the epithelial cells in the respiratory mucosa.Because the cilia beat or move in one direction, the mucus only moves upward.
Cigarette smoking paralyzes these cilia and results in accumulations of mucus and “smoker’s cough”.
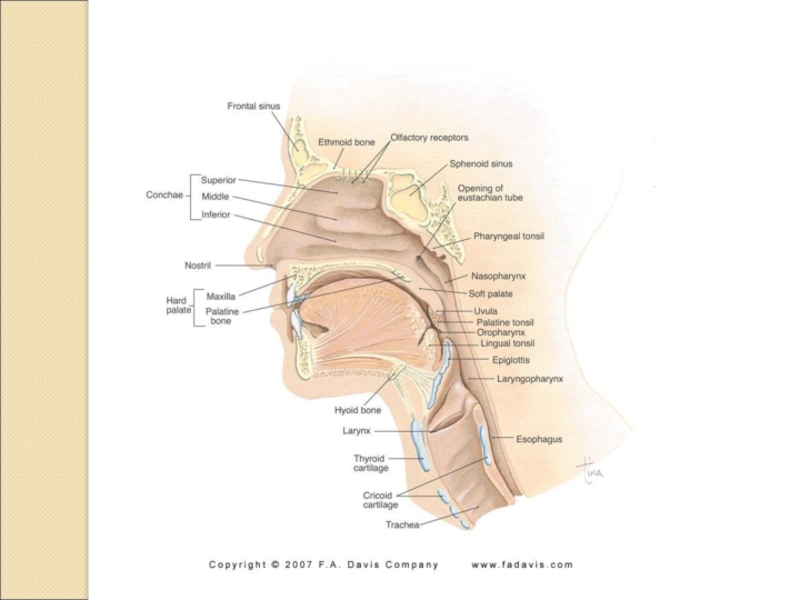
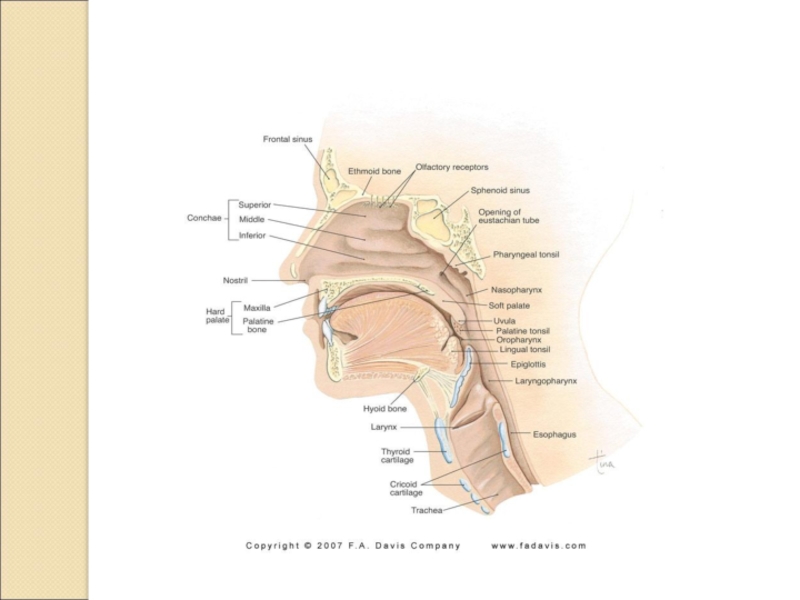
Слайд 8Anatomy and Air Flow
Air enters the respiratory tract through the
The surface of the nasal cavities is moist from
mucus and warm from blood flowing just under the surface. Nerve endings in the mucosa are responsible for the sense of smell (olfactory receptors).
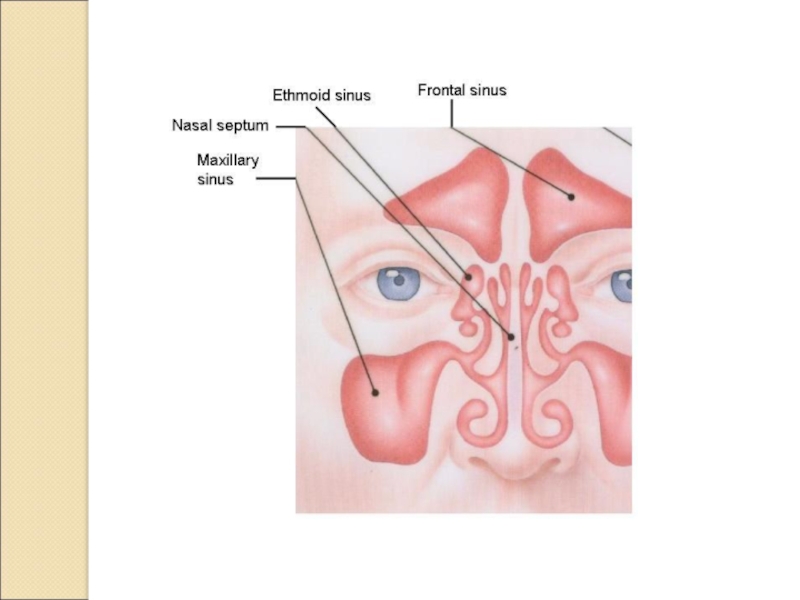
Слайд 9Anatomy and Air Flow
Nasal cavities
Paranasal sinuses: frontal, maxillary, sphenoidal, and
ethmoidal drain into the nasal cavities.
3 shelf-like structures, conchae, protrude
into each nasal cavity. The conchae are covered with mucosa and increase the surface area over which the air must flow as it passes through the nasal cavity.
Слайд 12Anatomy and Air Flow
Nasal cavities
As air moves through the nasal
cavities, it is warmed and humidified. ? Breathing through your
mouth.When delivering O2 to a patient it must be humidified or it will dry out the mucosa and cause discomfort and irritation. Drying of the mucosa can cause a nose bleed = epistaxis.
Слайд 13Anatomy and Air Flow
Pharynx – about 5 inches long; 3
sections:
Nasopharynx –
Oropharynx –
Laryngopharynx –
The pharynx provides a
passageway for food on its way to the esophagus and air on its way to the lungs.Слайд 14Anatomy and Air Flow
Pharynx
The right and left auditory or eustachian
tubes open into the nasopharynx. The lining is continuous with
the lining of the nasopharynx and middle ear. Infection in one area can spread easily to another.Pharyngeal tonsils (adenoids) are in the nasopharynx; palatine tonsils are in the oropharynx.
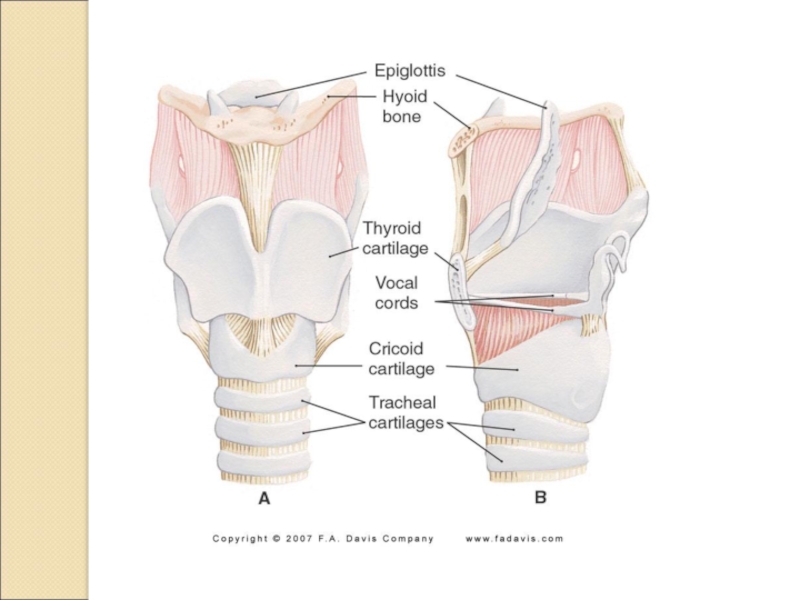
Слайд 16Anatomy and Air Flow
Larynx = “voice box”
Located just below the
pharynx and is composed of several pieces of cartilage.
Vocal cords
– 2 short elastic tissue bands, covered with mucous membrane, that stretch across the interior of the larynx. Muscles that attach to the larynx cartilages can pull on these cords and increase the tension – higher pitched sound. When they relax – less tension and a lower pitched sound.
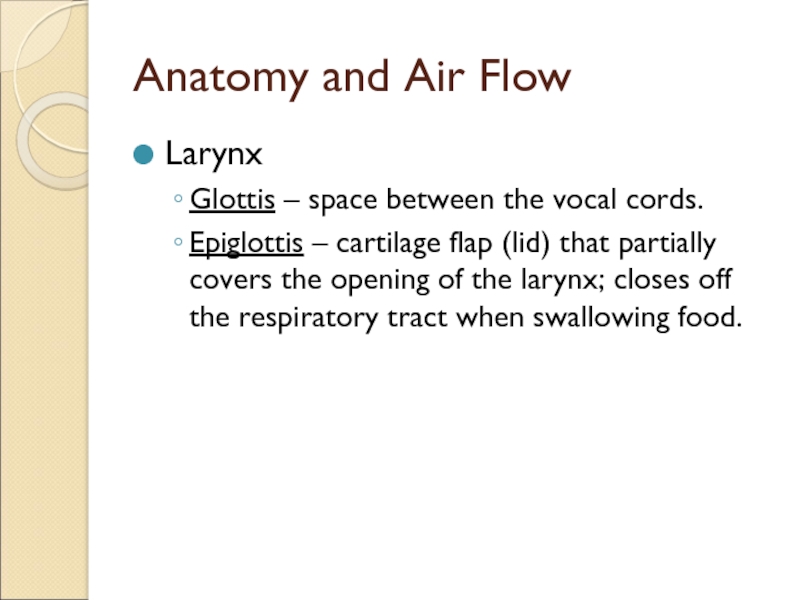
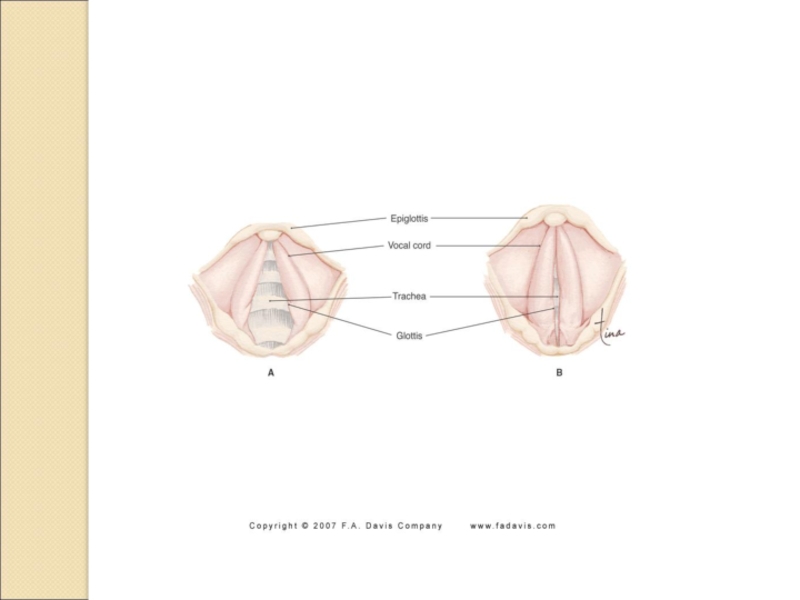
Слайд 18Anatomy and Air Flow
Larynx
Glottis – space between the vocal cords.
Epiglottis
– cartilage flap (lid) that partially covers the opening of
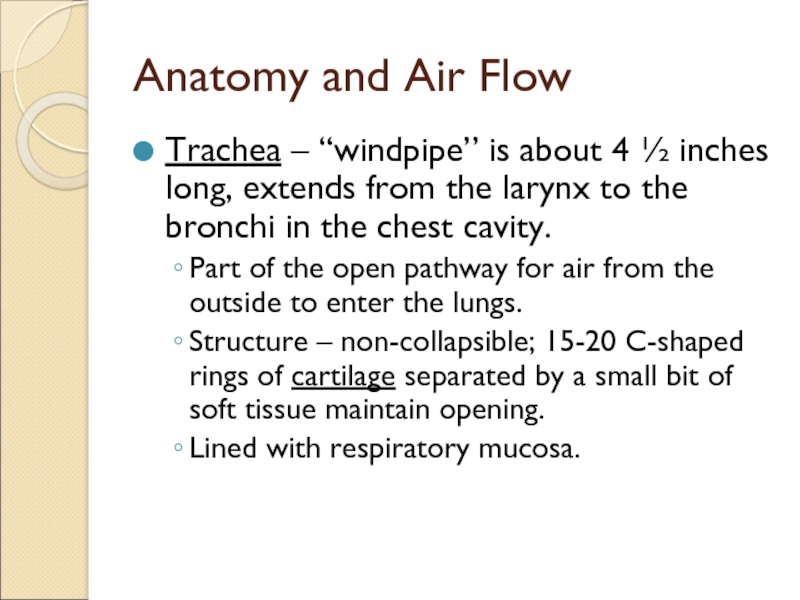
the larynx; closes off the respiratory tract when swallowing food.Слайд 20Anatomy and Air Flow
Trachea – “windpipe” is about 4 ½
inches long, extends from the larynx to the bronchi in
the chest cavity.Part of the open pathway for air from the outside to enter the lungs.
Structure – non-collapsible; 15-20 C-shaped rings of cartilage separated by a small bit of soft tissue maintain opening.
Lined with respiratory mucosa.
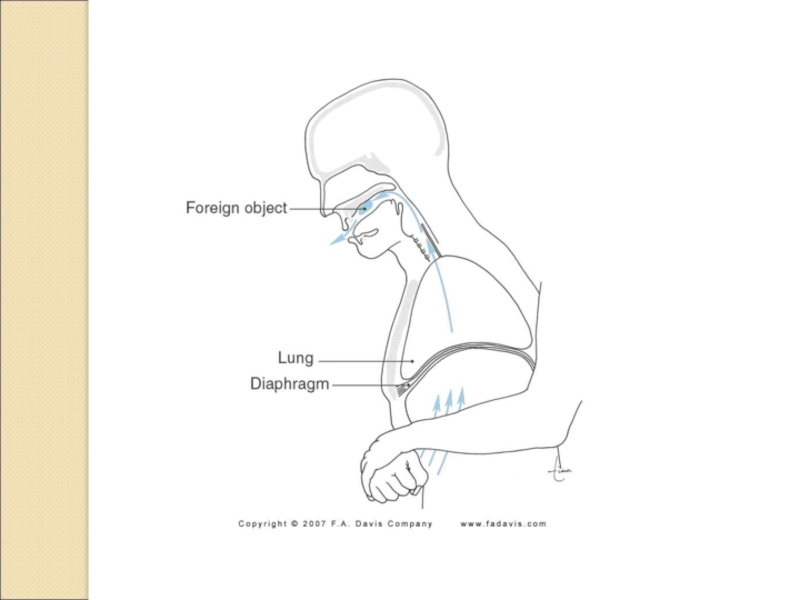
Слайд 21Anatomy and Air Flow
Trachea
Choking on food and other substances (caught
in the trachea) kills over 4000 people each year and
is the 5th major cause of accidental death in the US. ***Heimlich maneuver.Слайд 23Anatomy and Air Flow
Bronchi, bronchioles and alveoli – looks like
an upside down tree.
Trachea is the main trunk that divides
into Right bronchus and left bronchus. As the bronchi enter the lungs they divide into smaller and smaller branches.
The smallest tubes whose walls are made only of smooth muscle are called bronchioles.
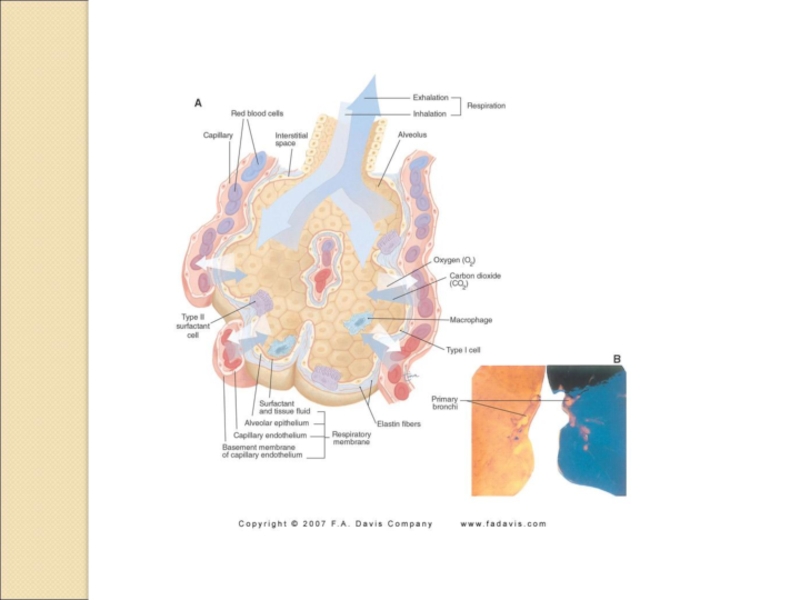
Слайд 24Anatomy and Air Flow
Bronchi, bronchioles and alveoli
Bronchioles further divide into
microscopic tubes called alveolar ducts which resemble the main stem
of a bunch of grapes.Alveolar ducts end in several alveolar sacs arranged like a clusters of grapes.
The walls of the alveolar sacs are made up of numerous alveoli each of which resembles a single grape.
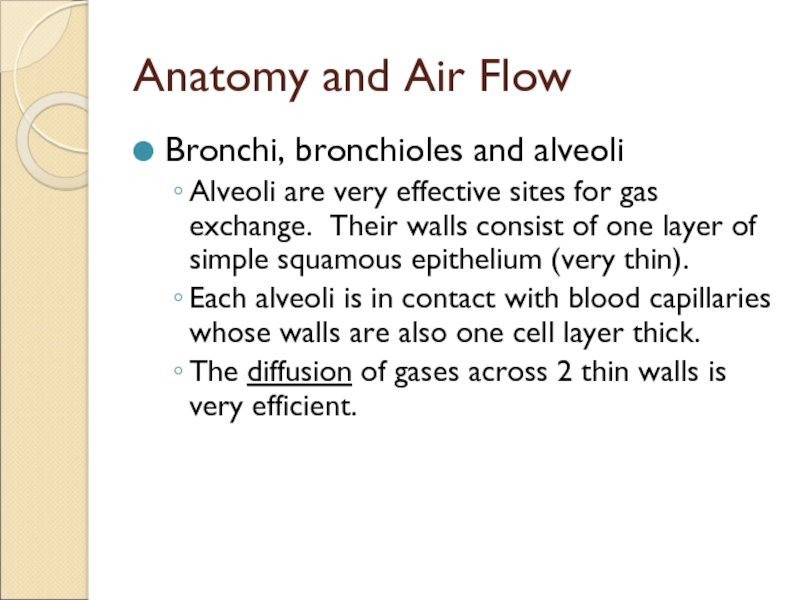
Слайд 26Anatomy and Air Flow
Bronchi, bronchioles and alveoli
Alveoli are very effective
sites for gas exchange. Their walls consist of one layer
of simple squamous epithelium (very thin).Each alveoli is in contact with blood capillaries whose walls are also one cell layer thick.
The diffusion of gases across 2 thin walls is very efficient.
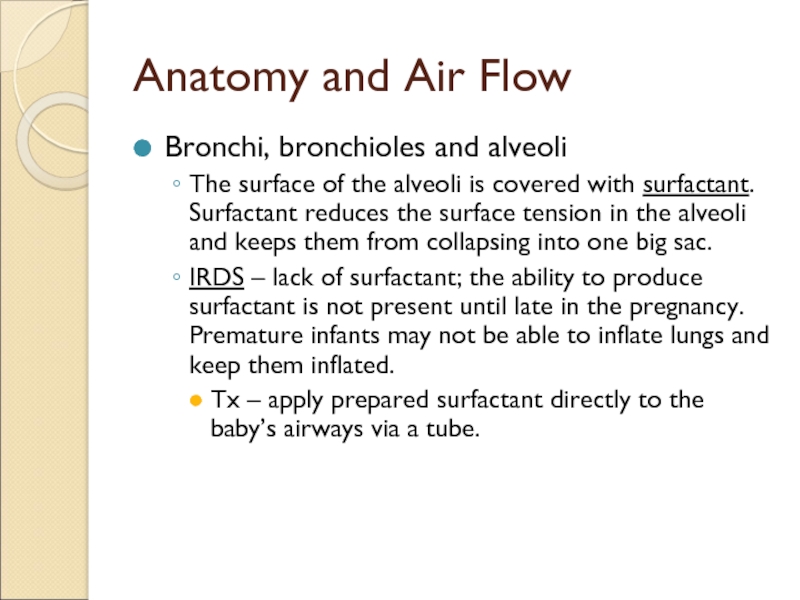
Слайд 28Anatomy and Air Flow
Bronchi, bronchioles and alveoli
The surface of the
alveoli is covered with surfactant. Surfactant reduces the surface tension
in the alveoli and keeps them from collapsing into one big sac.IRDS – lack of surfactant; the ability to produce surfactant is not present until late in the pregnancy. Premature infants may not be able to inflate lungs and keep them inflated.
Tx – apply prepared surfactant directly to the baby’s airways via a tube.
Слайд 30Anatomy
Pleura
Serous membranes that cover the outer surface of the lungs
and line the inner surface of the thoracic cavity. ?Names
Normally
the intrapleural space contains just enough fluid to make both layers of the pleura glide easily against each other as the lungs expand and deflate.Слайд 31Anatomy
Pleura
Pleurisy – inflammation of the pleura that causes pain when
the pleural membranes rub together.
Pneumothorax – presence of air in
the intrapleural space on 1 or both sides. The additional air causes pressures on the lungs and causes them to collapse. Spontaneous or traumatic.? Hemothorax, pyothorax.
Слайд 32Respiration
Pulmonary ventilation (or ventilation): breathing, the process that moves air
into and out of the lungs/alveoli. Also called external respiration.
Respiration:
exchange of gases (oxygen and carbon dioxide) between a living organism and its environment. In animals (people) this takes place in the lungs (alveoli) where the air and blood come in close contact.
Слайд 33Respiration
Internal respiration – process by which an exchange of gases
occurs between the blood and the cells of the body.
Cellular
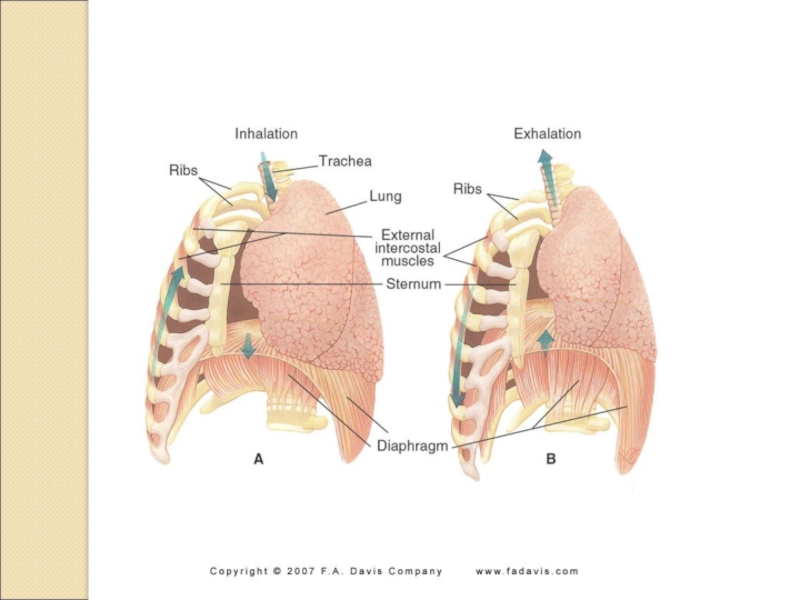
respiration – actual use of O2 by cells in the process of metabolism.Слайд 34Mechanics of Breathing
Muscles – control the size of the chest
cavity.
External intercostals – between the ribs move the chest up
and out when they contract.Diaphragm – dome shaped muscle between the thoracic and abdominal cavities, moves down when it contracts increasing the volume in the thorax.
Hiccups (singultus) – involuntary, spasmodic contraction of the diaphragm. Caused by irritation to the phrenic nerve or some types of brain injury.
Слайд 35Mechanics of Breathing
Pulmonary ventilation has 2 phases:
Inspiration or inhalation –
moving air into lungs.
Expiration or exhalation – moving air out
of the lungs.Inspiration occurs as the thorax enlarges (contraction of the external intercostals and diaphragm). Because of the positioning of the pleura, the lungs expand as the thorax expands and air rushes in and down to the alveoli.
Слайд 36Mechanics of Breathing
Expiration
Passive process that begins when the muscles relax
decreasing the size of the thorax and lungs – air
moves out of the lungs.Forceful expiration – internal intercostals and abdominal muscles contract and depress the rib cage decreasing the depth (front to back) of the thorax. Pressure increases and air flows out of the lungs.
Слайд 38Gas Exchange
Blood is pumped out of the ? ventricle into
the pulmonary ? to the capillaries that surround the alveoli.
Gases
move by diffusion. What is diffusion?Слайд 39Gas Exchange
Blood flowing toward the lungs is low in O2
and rich in CO2 the air in the alveoli is
rich in O2 and low in CO2. Which way does O2 move? CO2?O2 combines with the hemoglobin in the RBCs to form oxyhemoglobin and is transported to the tissues where the cells use it in cellular respiration.
Слайд 40Gas Exchange
CO2 moves into the lungs and leaves the body
during expiration.
At the tissues O2 is low and CO2 high
whereas the blood reaching them is just the opposite. O2 moves out of and CO2 moves into the blood.Most of the CO2 is carried in the blood as a bicarbonate ion, some is dissolved in the plasma and some combines with hemoglobin to form carbaminohemoglobin.
Слайд 43Respiratory Function
Expiratory reserve – amount of air that can be
forcibly exhaled after exhaling the tidal volume.
Inspiratory reserve –
amount of air that can be forcibly inhaled over and above normal inhalation.Residual volume – air that remains in the lungs after the most forceful expiration.
Residual volume + Vital Capacity =
Слайд 45Regulation of Respiration
Normal respiration depends on proper functioning of the
muscles of respiration. Normal respiratory rate – 12-20 (or 10-14,
or 16-18) breaths/min.The muscles are stimulated by nervous impulses that originate in the respiratory control centers located in the medulla and pons of the brain.
Слайд 46Regulation of Respiration
Receptors in the brain and blood vessels sense
the level of CO2 (or pH). When it is high
receptors send impulses to the respiratory control center to increase respiratory rate and depth.Receptors in the blood vessels also respond to decreased O2 levels when blood PO2 falls below 60 mmHg. Example COPD.
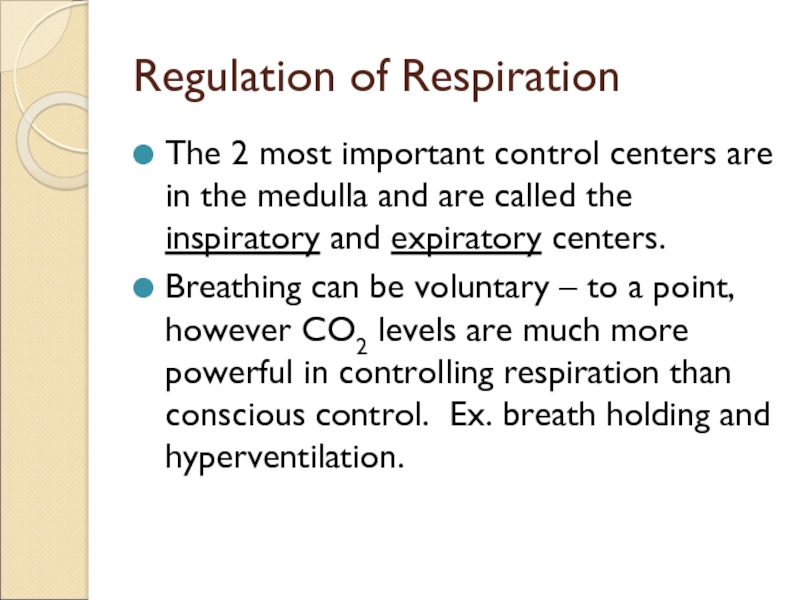
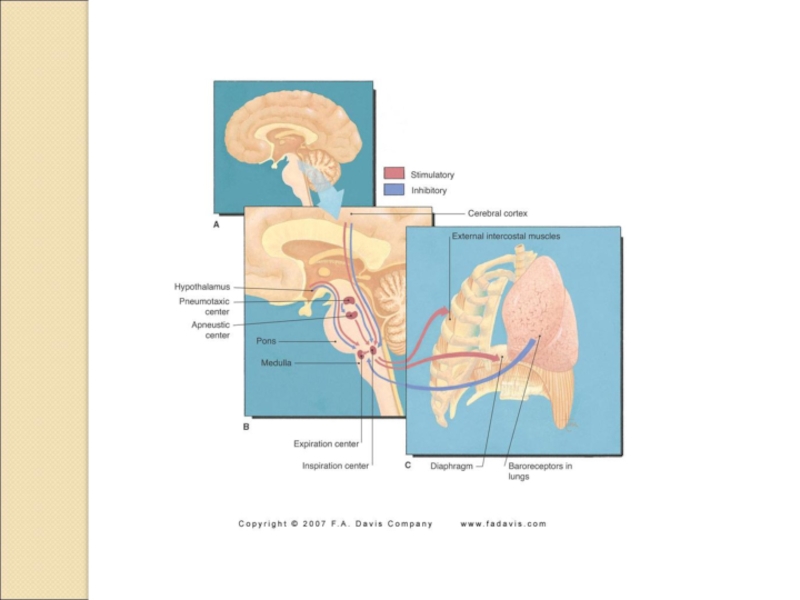
Слайд 48Regulation of Respiration
The 2 most important control centers are in
the medulla and are called the inspiratory and expiratory centers.
Breathing
can be voluntary – to a point, however CO2 levels are much more powerful in controlling respiration than conscious control. Ex. breath holding and hyperventilation.Слайд 50pH Disturbances
Respiratory – change in gas exchange; lungs
Acidosis – blood
pH is acid due to increased levels of CO2 in
the blood.Alkalosis – blood pH is alkaline or basic due to decreased levels of CO2 in the blood.
In any fluid that contains water: CO2 + H2O → H2CO3 → H+ + HCO3-
The brain senses the H+ concentration that develops in the CSF because CO2 diffuses into the CSF from the blood.
Слайд 51pH Disturbances
Metabolic – change in pH that is not due
to changes in gas exchange in the lungs.
Acidosis – diabetes
mellitus, kidney disease or severe diarrhea increase H+ in the blood. *Respiratory compensation – increased rate and depth.Alkalosis – vomiting, medications – decrease H+ in the blood. *Respiratory compensation – decreased rate and depth.