Слайд 2
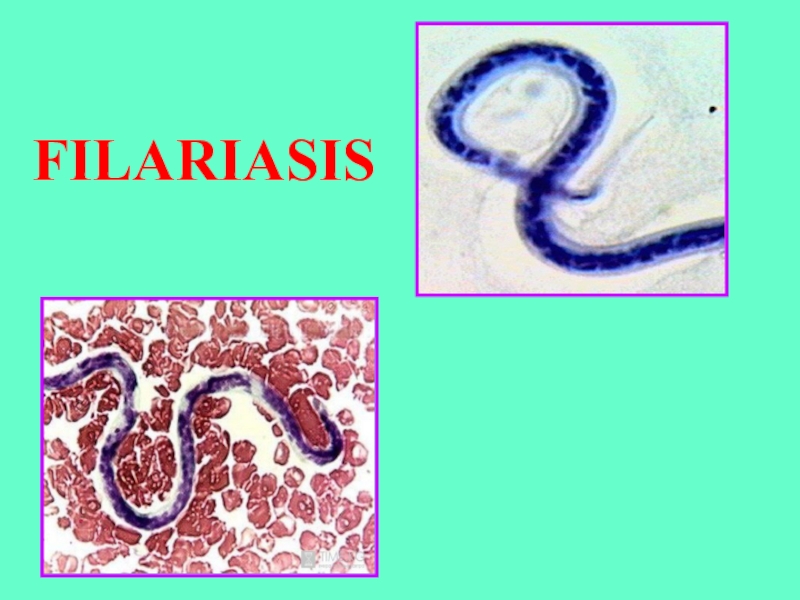
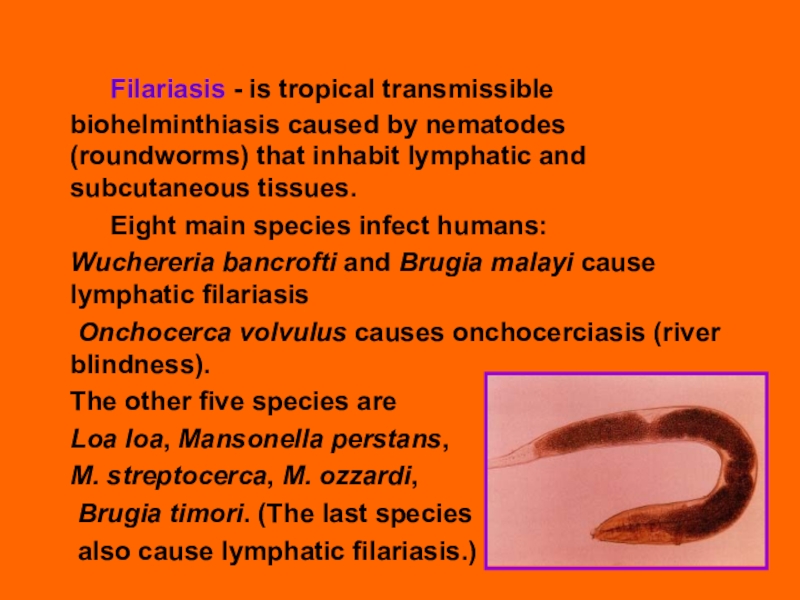
Filariasis - is tropical transmissible biohelminthiasis caused by nematodes
(roundworms) that inhabit lymphatic and subcutaneous tissues.
Eight main species
infect humans:
Wuchereria bancrofti and Brugia malayi cause lymphatic filariasis
Onchocerca volvulus causes onchocerciasis (river blindness).
The other five species are
Loa loa, Mansonella perstans,
M. streptocerca, M. ozzardi,
Brugia timori. (The last species
also cause lymphatic filariasis.)
Слайд 3
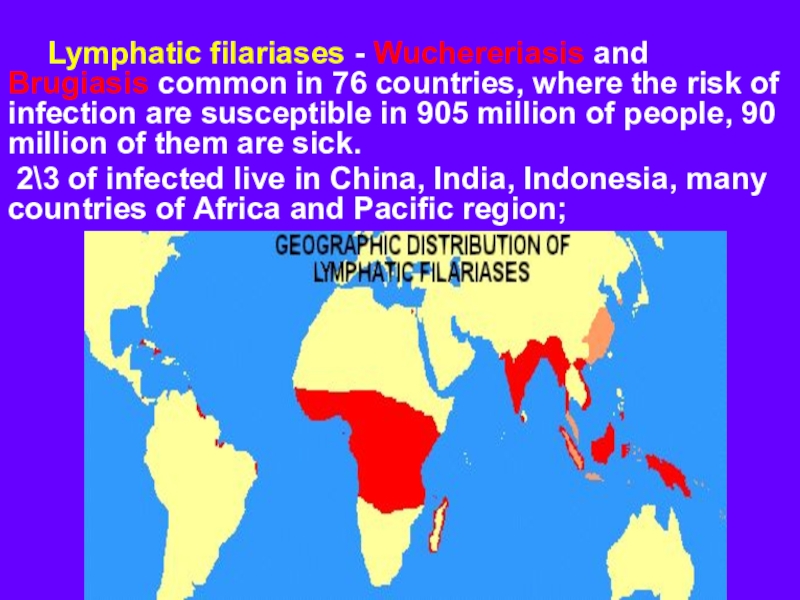
Lymphatic filariases - Wuchereriasis and Brugiasis common in 76 countries,
where the risk of infection are susceptible in 905 million
of people, 90 million of them are sick.
2\3 of infected live in China, India, Indonesia, many countries of Africa and Pacific region;
Слайд 4
Onchocerciasis - distributs in 34 countries, mainly in tropical
Africa, the Volta river basin, Mexico, Columbia, Guatemala.
The number of
patients 17.6 million, 26 000 of
them are blind.
Слайд 5Loa-loa disease (loasis, Сalabar disease) - is found only in
the forest zone of West and Central Africa;
Слайд 6
Features of filariases
1. Causative agent –
is small thin (thread-like)
biogelminth
2.
Cycle of development occurs with the participation of the definitive host (human)and intermediate – insect
3. Disease has a tendency to chronic course
4. All filariases have the same methods of diagnostics and treatment
5. Filariases are strictly endemic diseases registered only in the tropics and subtropics
Слайд 7
General properties of all filariaе:
1. They
are – larvaeparous bisexual biohelminths , developing
with the change of host.
2. The final host – is human, intermediate host – arthropods
(mosquitoes, midges, gadflies).
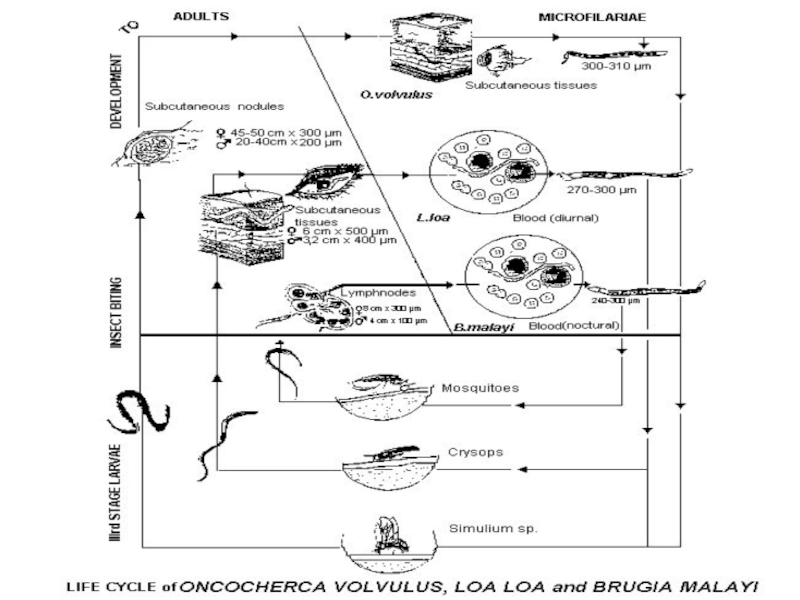
3. The adult warms (macrofilaria) dwell in various human tissues
where they can live for several years (subcutaneous tissue –
onchocerciasis, loasis, streptocerciasis, lymph vessels –
wuchereriasis and brugiasis connective tissue etc).
5. Females produce larvae (microfilaria) which penetrate into
blood stream or superficial skin layers (onchocercoiasis),
they do not grow and change morphologically.
6. Length of adult males up to 50 mm, females - up to 100 mm,
microfilaria - 0,3 mm.
Слайд 8
6. The cycle of development is the
same for all filariae:
a)
Mosquito ingests larvae during blood suction of sick man → larvae growth 5-10 days→ become mature in 2 month.
Vector swallowed the larva becomes contagious in 2-3 weeks.
b) Larvae enter the human body through mosquito bite → enter the blood stream and reach the lymph vessels and nodes → then mature to adult helminthe.
Female hatches microfilaria and they live as parasites in the blood or subcutaneous tissues.
7. All filariases have prolonged incubation period - 2-18 months, when helminthes reach sexual maturity.
8. Disease develops slowly.
9. Duration of the disease more than 10 years (the period of life of macrofilaria), microfilaria lives about 70 days.
Слайд 10
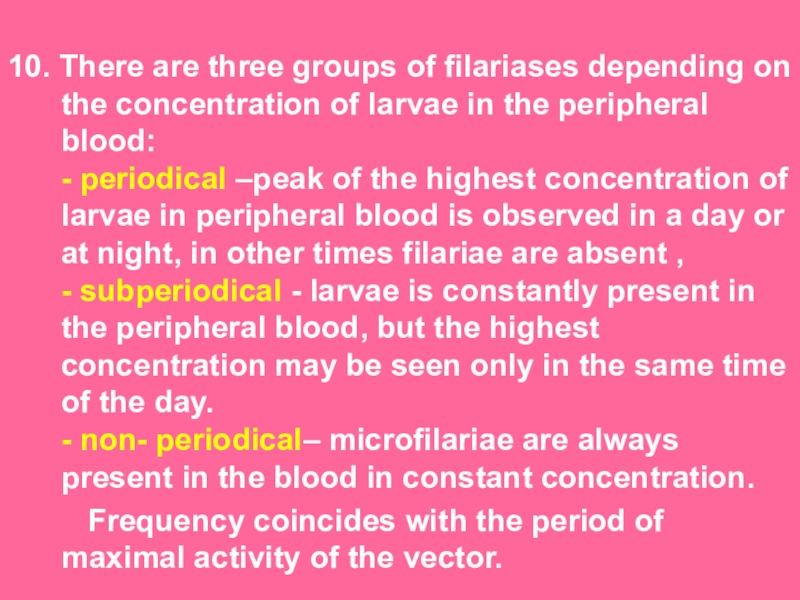
10. There are three groups of filariases depending on the
concentration of larvae in the peripheral blood:
- periodical –peak of
the highest concentration of larvae in peripheral blood is observed in a day or at night, in other times filariae are absent ,
- subperiodical - larvae is constantly present in the peripheral blood, but the highest concentration may be seen only in the same time of the day.
- non- periodical– microfilariae are always present in the blood in constant concentration.
Frequency coincides with the period of maximal activity of the vector.
Слайд 11
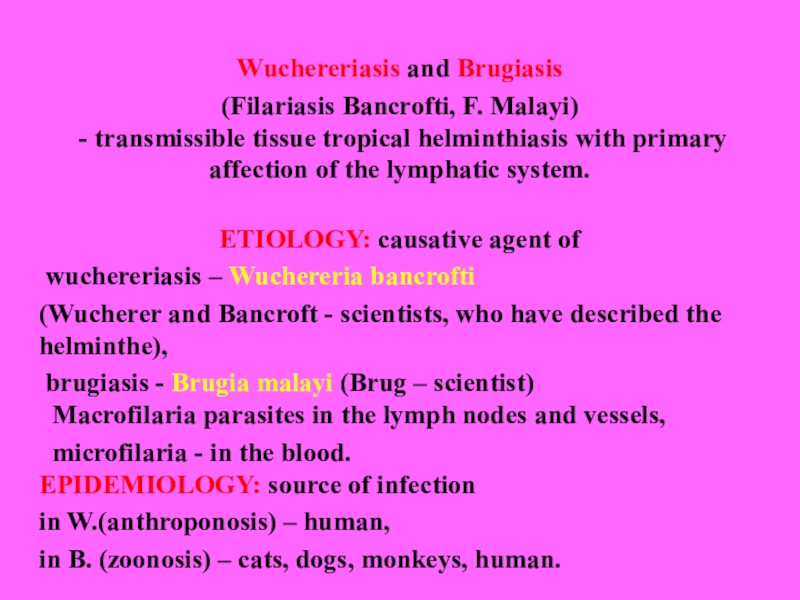
Wuchereriasis and Brugiasis
(Filariasis Bancrofti, F. Malayi)
- transmissible tissue
tropical helminthiasis with primary affection of the lymphatic system.
ETIOLOGY: causative
agent of
wuchereriasis – Wuchereria bancrofti
(Wucherer and Bancroft - scientists, who have described the helminthe),
brugiasis - Brugia malayi (Brug – scientist)
Macrofilaria parasites in the lymph nodes and vessels,
microfilaria - in the blood.
EPIDEMIOLOGY: source of infection
in W.(anthroponosis) – human,
in B. (zoonosis) – cats, dogs, monkeys, human.
Слайд 12
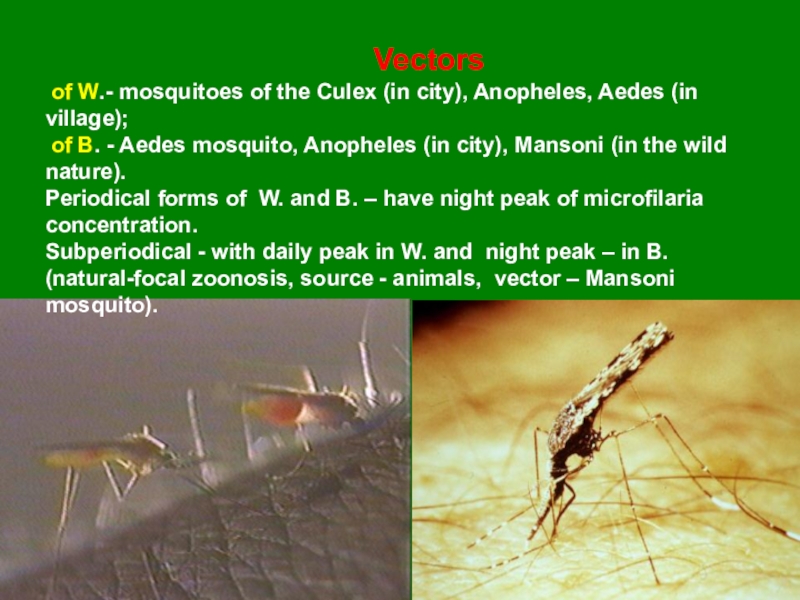
Vectors
of W.- mosquitoes of the Culex (in city), Anopheles,
Aedes (in village);
of B. - Aedes mosquito, Anopheles (in
city), Mansoni (in the wild nature).
Periodical forms of W. and B. – have night peak of microfilaria concentration.
Subperiodical - with daily peak in W. and night peak – in B. (natural-focal zoonosis, source - animals, vector – Mansoni mosquito).
Слайд 13
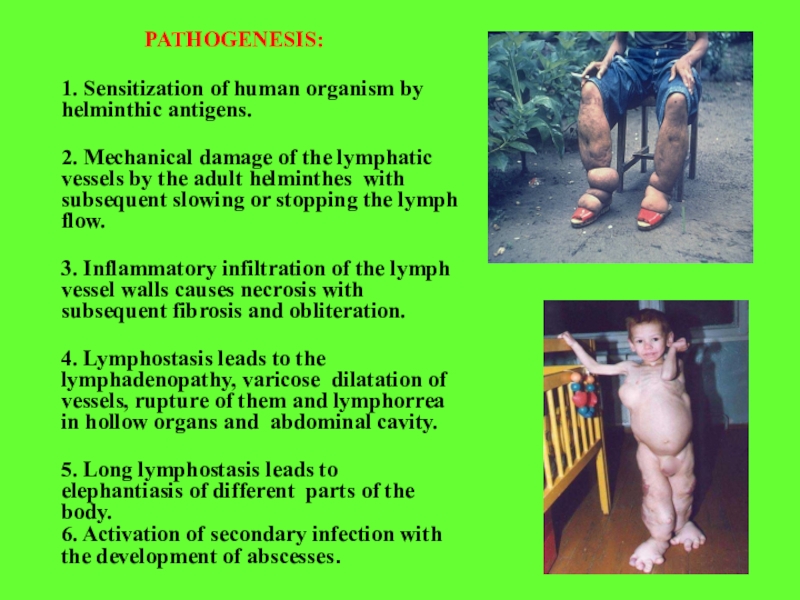
PATHOGENESIS:
1. Sensitization of human organism by helminthic antigens.
2. Mechanical damage
of the lymphatic vessels by the adult helminthes with subsequent
slowing or stopping the lymph flow.
3. Inflammatory infiltration of the lymph vessel walls causes necrosis with subsequent fibrosis and obliteration.
4. Lymphostasis leads to the lymphadenopathy, varicose dilatation of vessels, rupture of them and lymphorrea in hollow organs and abdominal cavity.
5. Long lymphostasis leads to elephantiasis of different parts of the body.
6. Activation of secondary infection with the development of abscesses.
Слайд 14
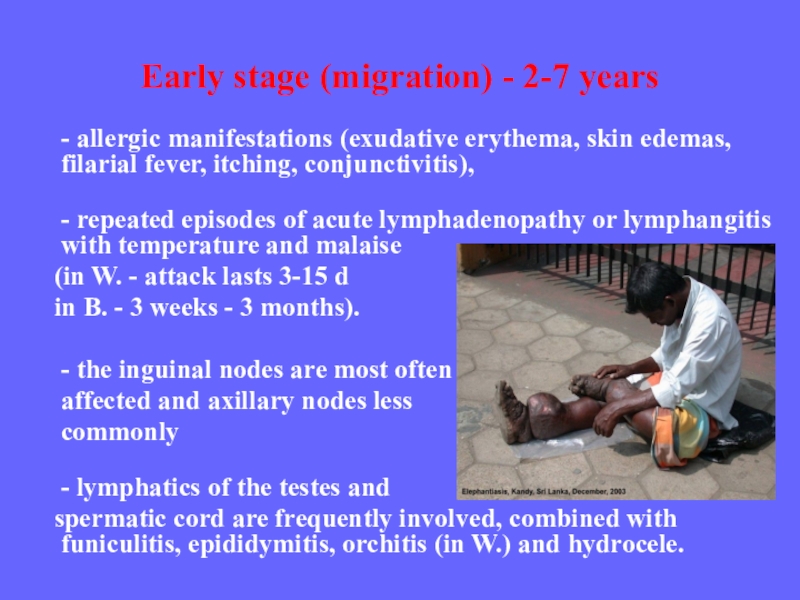
Early stage (migration) - 2-7 years
- allergic manifestations (exudative erythema,
skin edemas, filarial fever, itching, conjunctivitis),
- repeated episodes of acute
lymphadenopathy or lymphangitis with temperature and malaise
(in W. - attack lasts 3-15 d
in B. - 3 weeks - 3 months).
- the inguinal nodes are most often
affected and axillary nodes less
commonly
- lymphatics of the testes and
spermatic cord are frequently involved, combined with funiculitis, epididymitis, orchitis (in W.) and hydrocele.
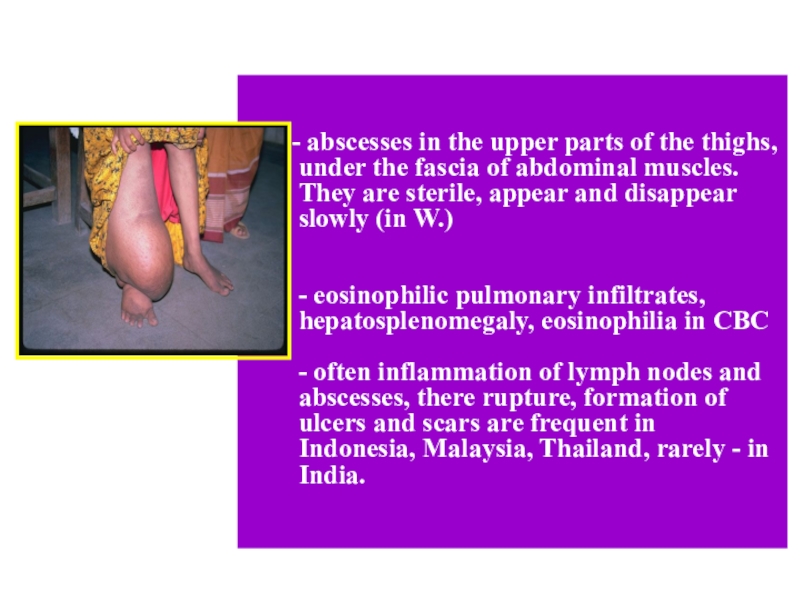
in the upper parts of the thighs, under the fascia
of abdominal muscles. They are sterile, appear and disappear slowly (in W.)
- eosinophilic pulmonary infiltrates, hepatosplenomegaly, eosinophilia in CBC
- often inflammation of lymph nodes and abscesses, there rupture, formation of ulcers and scars are frequent in Indonesia, Malaysia, Thailand, rarely - in India.
Слайд 16
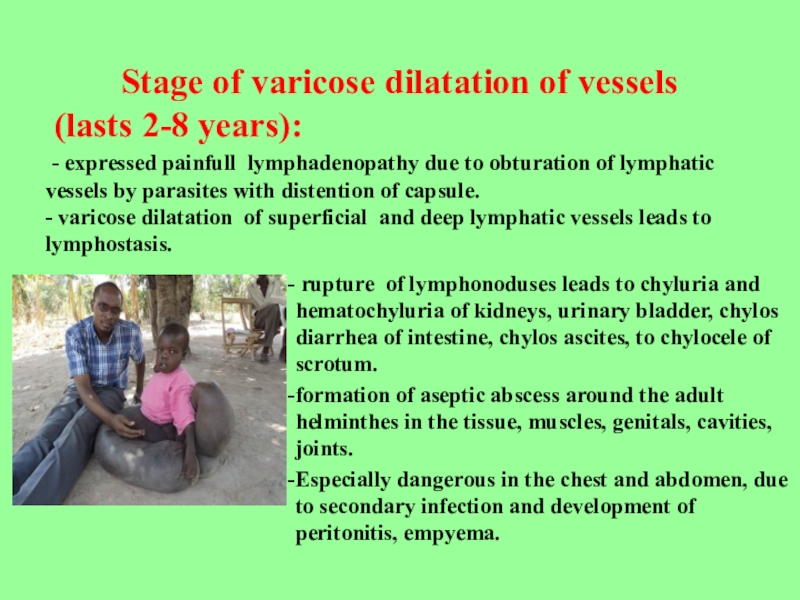
rupture of lymphonoduses leads to chyluria and hematochyluria of
kidneys, urinary bladder, chylos diarrhea of intestine, chylos ascites, to
chylocele of scrotum.
formation of aseptic abscess around the adult helminthes in the tissue, muscles, genitals, cavities, joints.
Especially dangerous in the chest and abdomen, due to secondary infection and development of peritonitis, empyema.
Stage of varicose dilatation of vessels
(lasts 2-8 years):
- expressed painfull lymphadenopathy due to obturation of lymphatic vessels by parasites with distention of capsule.
- varicose dilatation of superficial and deep lymphatic vessels leads to lymphostasis.
Слайд 17
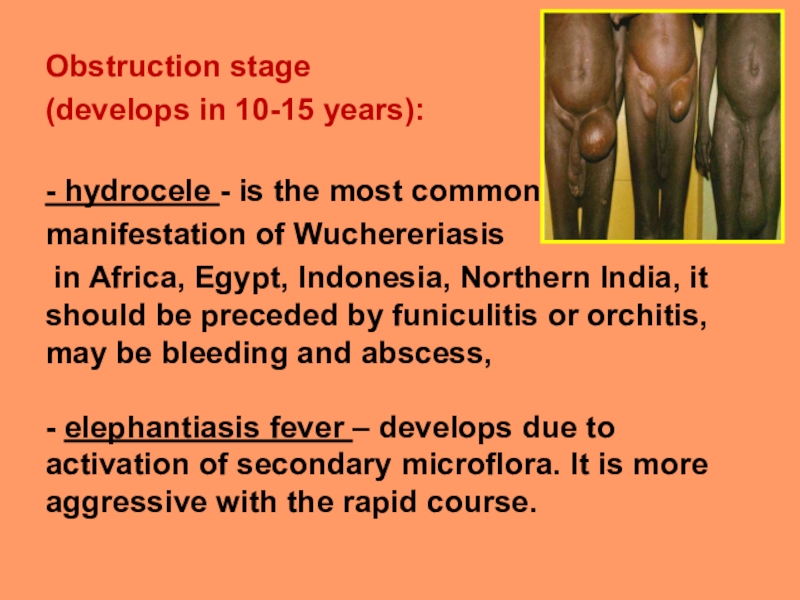
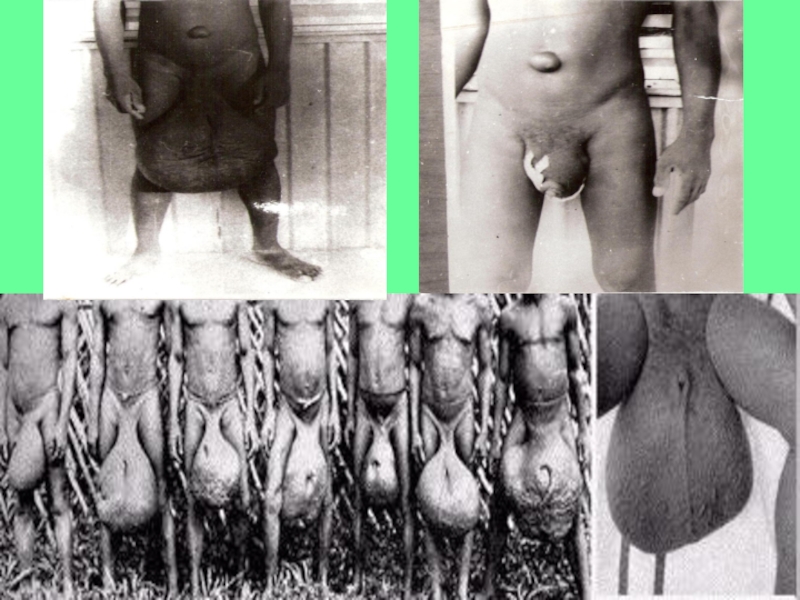
Obstruction stage
(develops in 10-15 years):
- hydrocele - is the
most common
manifestation of Wuchereriasis
in Africa, Egypt, Indonesia, Northern
India, it should be preceded by funiculitis or orchitis, may be bleeding and abscess,
- elephantiasis fever – develops due to activation of secondary microflora. It is more aggressive with the rapid course.
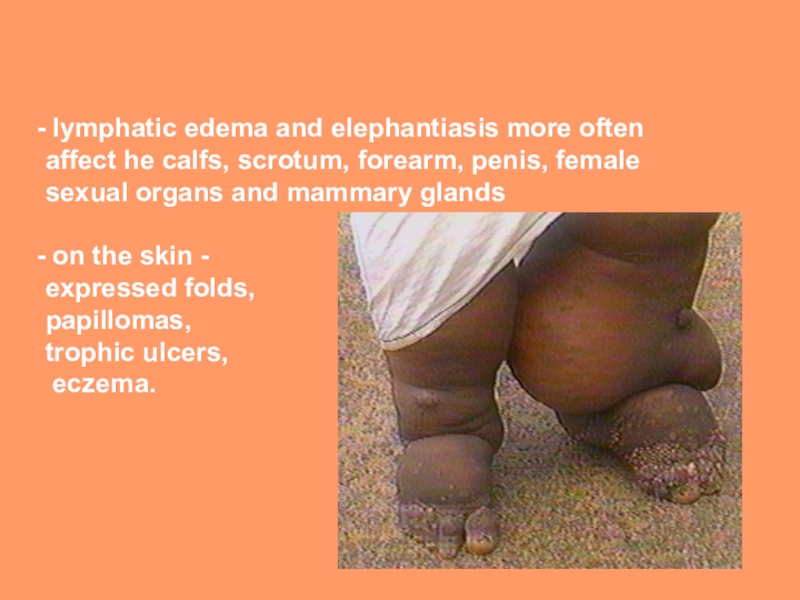
Слайд 19
lymphatic edema and elephantiasis more often affect he calfs,
scrotum, forearm, penis, female sexual organs and mammary glands
on
the skin -
expressed folds,
papillomas,
trophic ulcers,
eczema.
Слайд 20
IMMUNITY
- low reactivity antigens of filaria
- development of immunosuppression
(serum-factors,
T-lymphocytes, monocytes),
- high ratio of suppressors to helper T-cells,
-titles of
IgE are high, but signs of allergic
reactivity are not observed.
Антиген
Слайд 21
ONCHOCERCOSIS
River blindness
- transmissible tissue tropical helminthiasis with primary affection of
skin, eyes and subcutaneous lymph nodes
ETIOLOGY
- the causative agent
is Onchocerca volvulus. Macrofilaria parasites in the subcutaneous tissue usually in the pelvis, joints or head.
Female hatches about 2 million microfilaria per year, which live in the skin epidermis, eye-balls and lymph nodes.
EPIDEMIOLOGY
The source of infection and the final host- only human
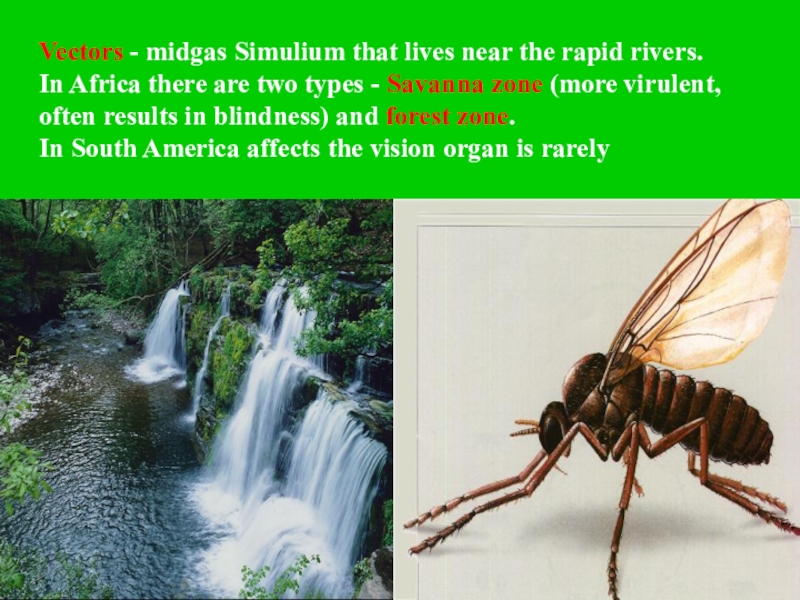
Слайд 22Vectors - midgas Simulium that lives near the rapid rivers.
In Africa there are two types - Savanna zone (more
virulent, often results in blindness) and forest zone.
In South America affects the vision organ is rarely
PATHOGENESIS
1. Mechanical influence of adult parasites, around which
onchocercoma is formed (connective tissue node)
2. Toxico-allergic effects of mature parasite and it’s larvae (especially dead worm)
3. Penetration of the larvae into eyeballs results in iritis or iridocyclitis («anterior uveitis») and/or chorioiditis or chorioretinitis («posterior uveitis»), keratitis, conjunctivitis with subsequent development of gradual sclerosis, atrophy of the optic nerve and blindness
4. Parasitizing microfilaria causes dermatitis with lymph swelling of the skin of genitals, lower extremities and elephantiasis
5. In the final stages depigmentation, atrophy, ulceration is developed
Слайд 24
CLINIC
Incubation period - is about a year.
- Itching, local edema in the site of bite
- urticarial rash,
- subfebral fever,
- increased lymph nodes,
- spleenomegaly,
- eosinophilia
Слайд 25
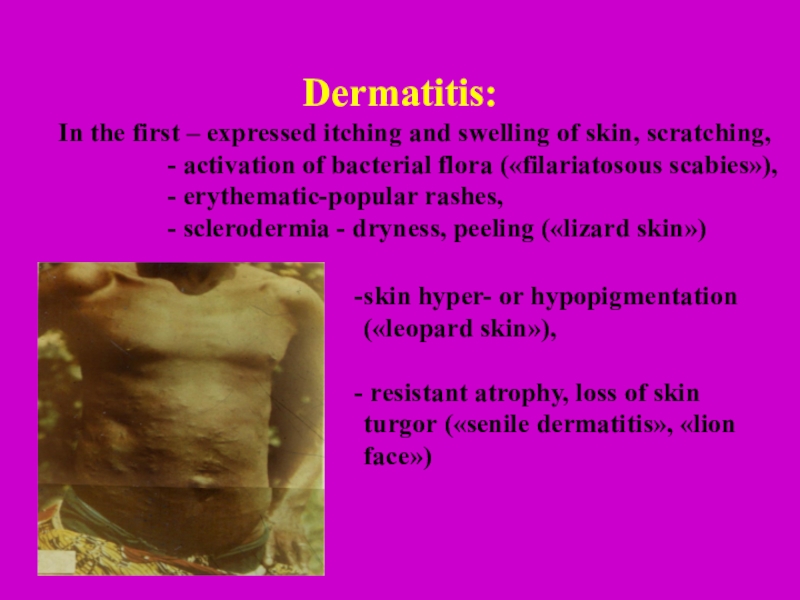
Dermatitis:
In the first – expressed itching and swelling of
skin, scratching,
- activation of bacterial flora («filariatosous scabies»),
- erythematic-popular rashes,
- sclerodermia - dryness, peeling («lizard skin»)
skin hyper- or hypopigmentation («leopard skin»),
resistant atrophy, loss of skin turgor («senile dermatitis», «lion face»)
Слайд 26pseudoadanitis – skin bags or pouch with subcutaneous tissues and
lymph nodes - «gotentog apron», «hanging groins», «hanging armpit», hernia
(due to involvement of the inguinocrural lymph nodes in hypersensitivity reaction to dead larvae),
- dermatitis may occur
as erysipelas with edema,
conjunctivitis and fever
Слайд 27
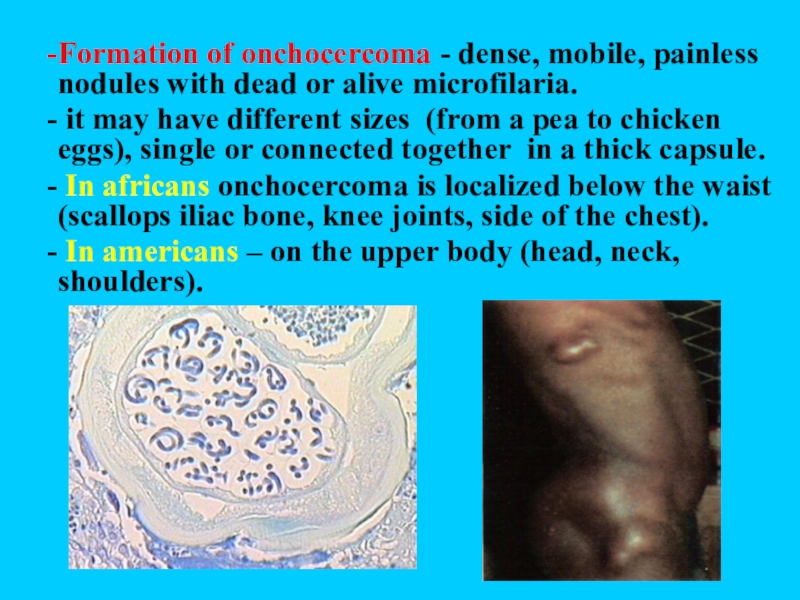
Formation of onchocercoma - dense, mobile, painless nodules with dead
or alive microfilaria.
it may have different sizes (from a
pea to chicken eggs), single or connected together in a thick capsule.
In africans onchocercoma is localized below the waist (scallops iliac bone, knee joints, side of the chest).
In americans – on the upper body (head, neck, shoulders).
Слайд 28affection of lymphatic system - lymphadenitis (groin and armpit), lymph
edema, orchitis, hydrocele, elephantiasis of the lower limbs and genitals
- microfilaria is detected in urine, sputum, vaginal discharge, lymphatic and blood circulation system, saliva, cerebrospinal fluid, liver, kidneys, lungs, spleen
Onchocercosis is a systemic disease
Слайд 29
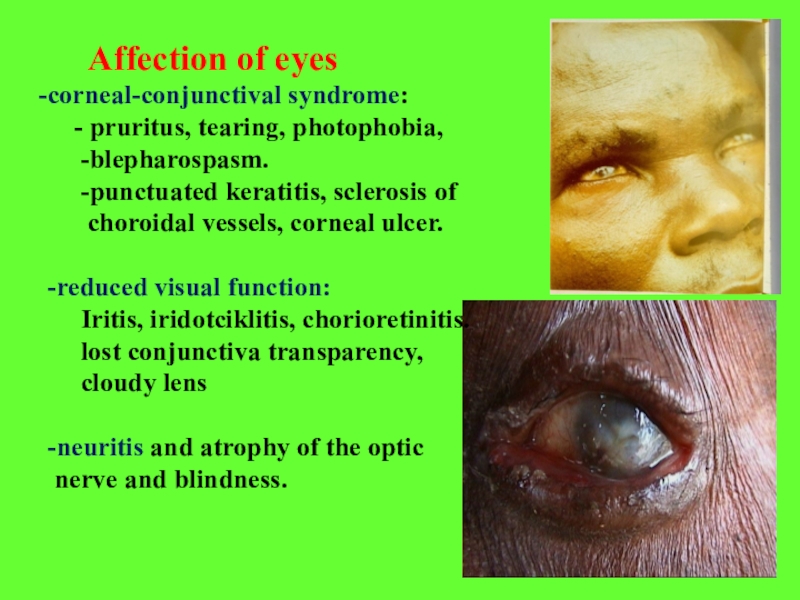
Affection of eyes
corneal-conjunctival syndrome:
- pruritus, tearing, photophobia,
-blepharospasm.
-punctuated keratitis, sclerosis of
choroidal vessels, corneal ulcer.
-reduced visual function:
Iritis, iridotciklitis, chorioretinitis.
lost conjunctiva transparency,
cloudy lens
-neuritis and atrophy of the optic
nerve and blindness.
LOASIS
(Calabar swelling disease)
- transmissible tissue tropical helminthiasis, characterized by different allergic reactions, edema of soft tissues, affection of eyes and genital organs.
ETIOLOGY
Pathogen - Loa loa, adult worm parasites under the conjunctiva of the eye and pericardium, microfilaria – in the blood in afternoon.
Слайд 31
EPIDEMIOLOGY
Source of invasion - man (sometimes monkeys)
Vectors - gadflies of the
genus Chrysops that lives
in
small water reservoirs.
Adult flies live in trees and
attack in the afternoon,
more often the people with
dark skin.
Слайд 32PATHOGENESIS – the same to other filariasis
CLINIC
Incubation period -
4 months, till one year.
1. Skin itching, rash, neuropathic pain,
subfibrale fever, hypereosinophilia – allergic syndrom.
2. Colabar swelling (dense, painless, slowly disappearing) on local open parts of body (often on the extremities), skin above is pale, hot, fossa does not remain.
3. Edema of eyelids, hyperemia of conjunctiva, pain in eyes, lacrimation. Helminth is visible by eyes.
4. Symptoms correspond to the place of helminth migration (dysuria, meningoencephalitis, neuritis, nephritic syndrome, hydrocele).
5. Abscesses around the dead worms.
6. Sometimes parasites visible under the skin and come out through the skin.
Слайд 33O.volvulus без чехлика
Brugia malayi
с чехликом
LOA LOA
M. Perstans
без
чехлика
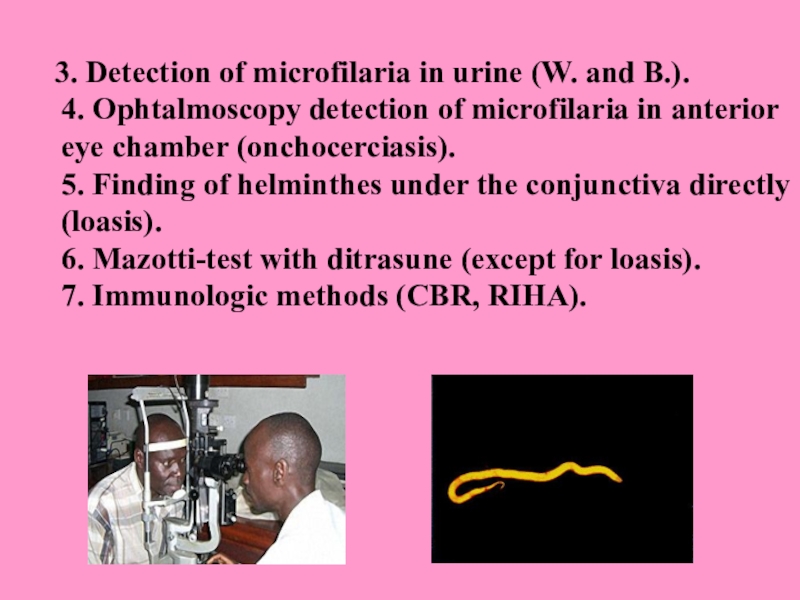
LABORATORY
DIAGNOSTICS
1. Detection of microfilaria in the blood smear and thick drops in the painted and unpainted preparations with a quantitative assessment of microfilariemia.
2. Detection of microfilaria in the
skin sections
received with sclera –corneal perforator
(onchocerciasis).
Слайд 35
3. Detection of microfilaria in urine (W.
and B.).
4. Ophtalmoscopy detection of microfilaria in anterior eye chamber
(onchocerciasis).
5. Finding of helminthes under the conjunctiva directly (loasis).
6. Маzоtti-test with ditrasune (except for loasis).
7. Immunologic methods (CBR, RIHA).
TREATMENT
Dietylcarbamasine
- is effective in acute and chronic stage, in latent filariasis
6 mg /kg /day (after meal) - 12 days (from 3 to 6 mg / kg / day).
In loasis - on the first day - 1\2 of doses, gradually increasing to 0.1 (3-4 times) - 2-3 weeks.
Onchocerciasis:
Dietylcarbamasine (initial dose reduced) -12 days
Antripol (suramin)- 10% - 5ml - 1st day
10% - 10 ml - 2nd day
10% - 10 ml -1 times in 7 days -
5-7 weeks
Ivermectine (mektisane) 150 mg\kg 1 time in 6 months.
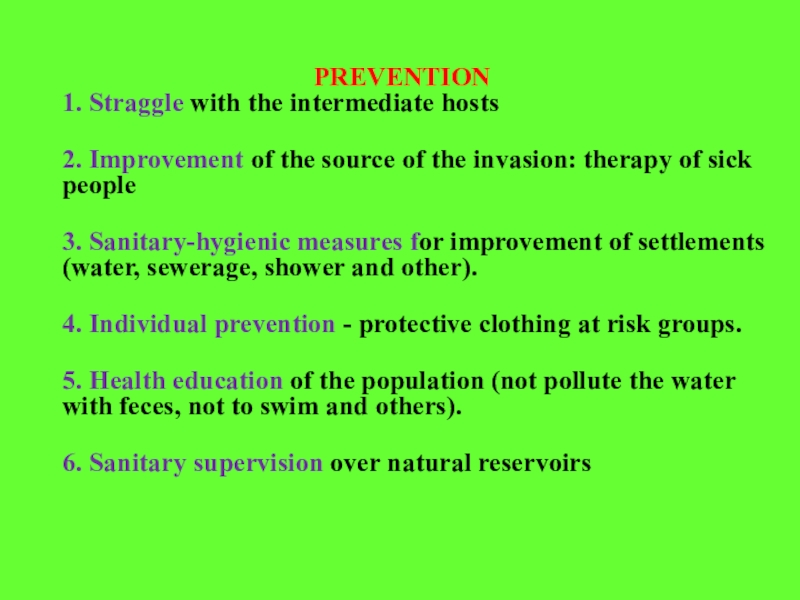
PREVENTION
1. Straggle with the intermediate hosts
2. Improvement of the source of the invasion: therapy of sick people
3. Sanitary-hygienic measures for improvement of settlements (water, sewerage, shower and other).
4. Individual prevention - protective clothing at risk groups.
5. Health education of the population (not pollute the water with feces, not to swim and others).
6. Sanitary supervision over natural reservoirs