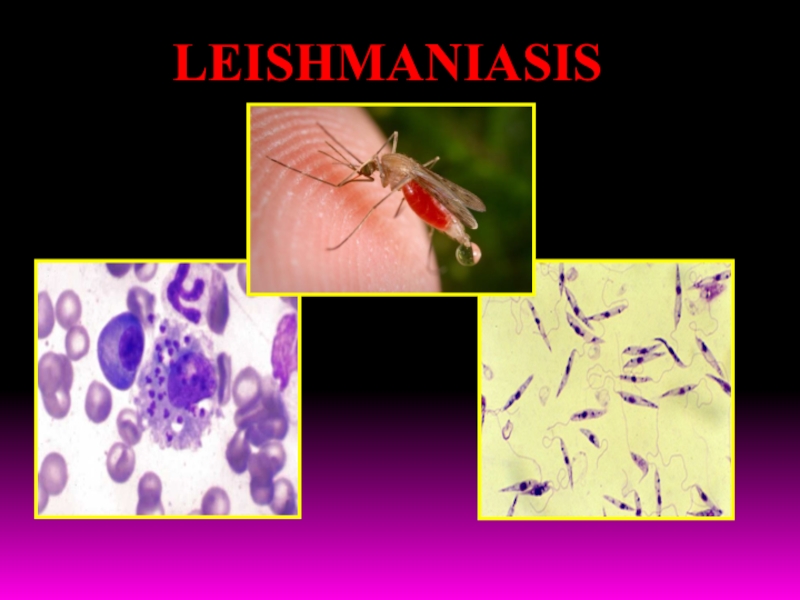
Слайд 2LEISHMANIASIS - a group of protozoan diseases of humans and
animals, caused by different species of the genus Leishmania, characterized
by affecting the internal organs (Visceral leishmaniasis) or mucous membranes and skin (Skin leishmaniasis).
It refers to diseases transmitted by mosquitoes of the genus Phlebotomus (Leishmaniasis of the Old world) and Lutzomyia (Leishmaniasis of the New world).
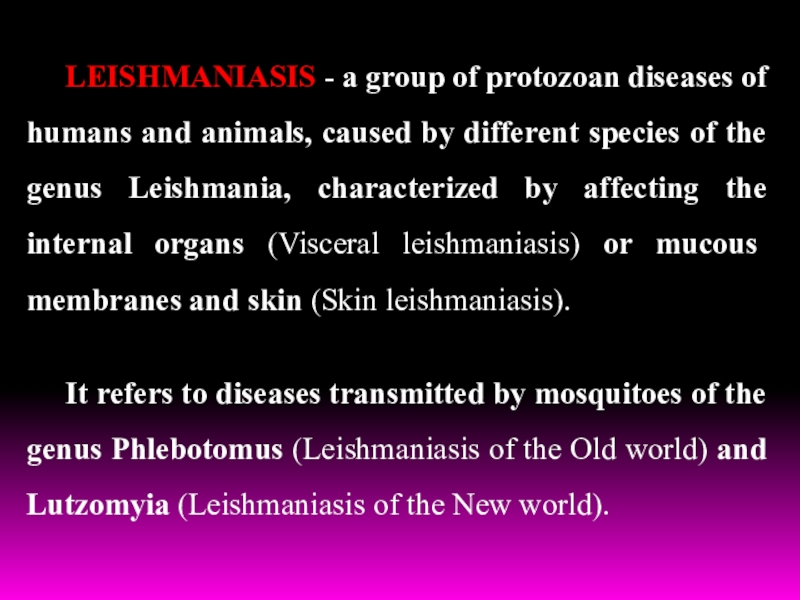
Слайд 3Leishmaniasis takes an important place in tropical pathology.
According to WHO,
leishmaniasis common in 88 countries of the world, in 32
countries – it is subject of obligatory registration.
According to expert estimates, the number of patients with Leishmaniasis in the world - more than 12 million people. There are 2million new cases annually.
Approximately 350 million people live in endemic area.
Leishmaniasis included in the special program of
WHO «Study and struggle with tropical diseases».
Leishmaniases is one of the most actual problems due to its ability to suppress immune system, especially in persons with HIV or AIDS.
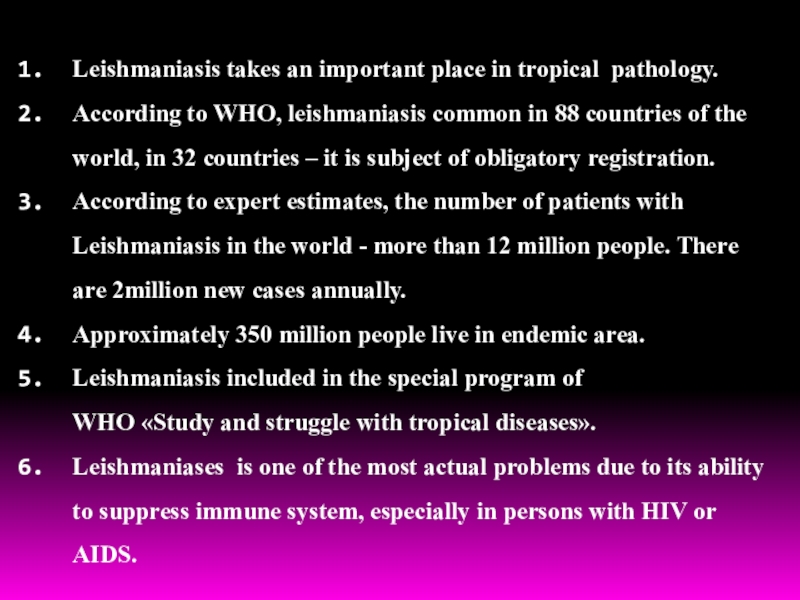
Слайд 4
В55 Leishmaniasis
В55.0 Visceral Leishmaniasis (Leishmaniosis visceralis).
By
type:
-
anthroponotic - Indian VL (Kala-Azar);
- zoonotic - Mediterranean, Central Asia
visceral leishmaniasis (children's Kala Azar),
- the East African leishmaniasis,
- visceral leishmaniasis of New world.
By duration: acute, subacute, chronic, latent, subclinical.
By periods: initial, climax, terminal (cachexia).
By severity: mild, moderate, severe.
Leading syndromes: exanthema, fever, polilymphadenopathy,
hepatosplenomegaly, haemorragic syndrom, cachexia
Classification
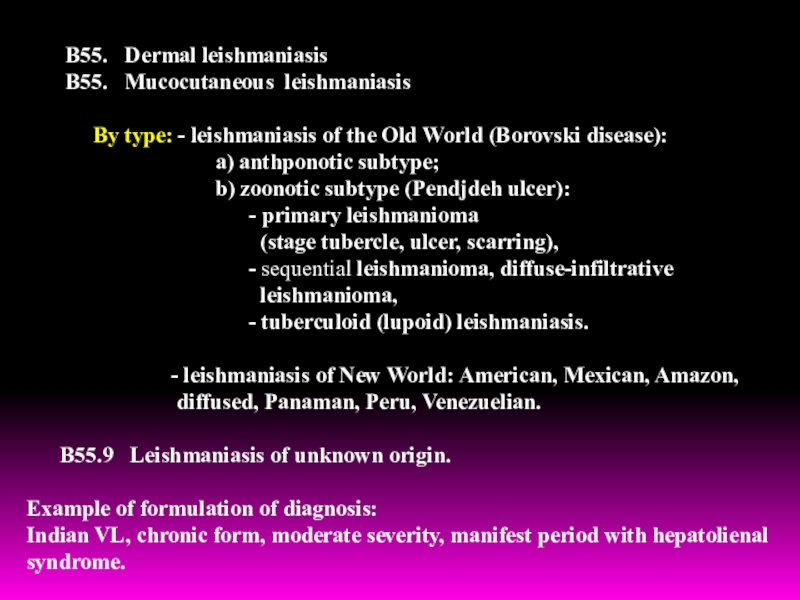
Слайд 5В55. Dermal leishmaniasis
В55. Mucocutaneous
leishmaniasis
By type: -
leishmaniasis of the Old World (Borovski disease):
a) anthponotic subtype;
b) zoonotic subtype (Pendjdeh ulcer):
- primary leishmanioma
(stage tubercle, ulcer, scarring),
- sequential leishmanioma, diffuse-infiltrative
leishmanioma,
- tuberculoid (lupoid) leishmaniasis.
- leishmaniasis of New World: American, Mexican, Amazon,
diffused, Panaman, Peru, Venezuelian.
В55.9 Leishmaniasis of unknown origin.
Example of formulation of diagnosis:
Indian VL, chronic form, moderate severity, manifest period with hepatolienal syndrome.
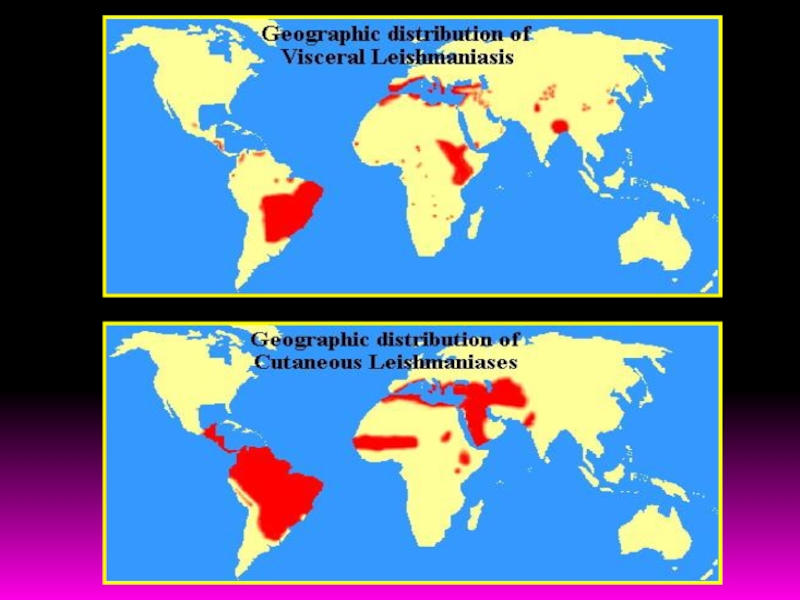
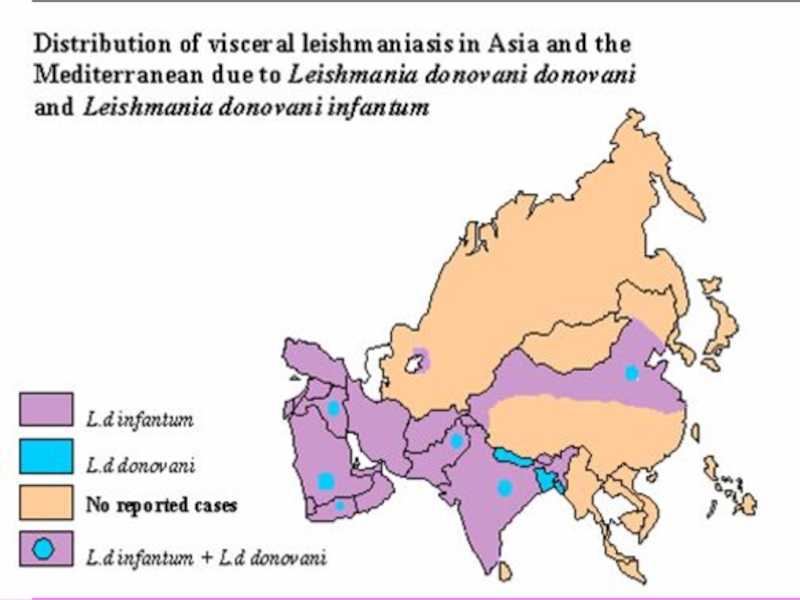
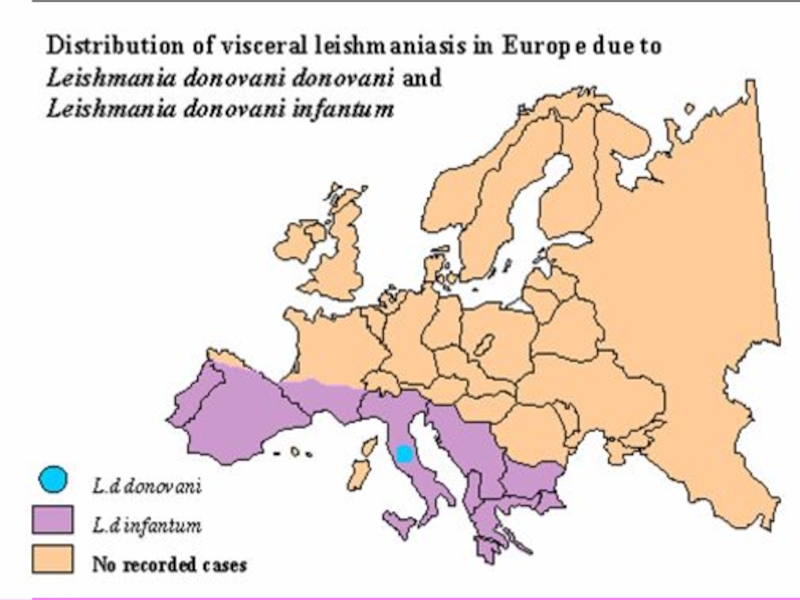
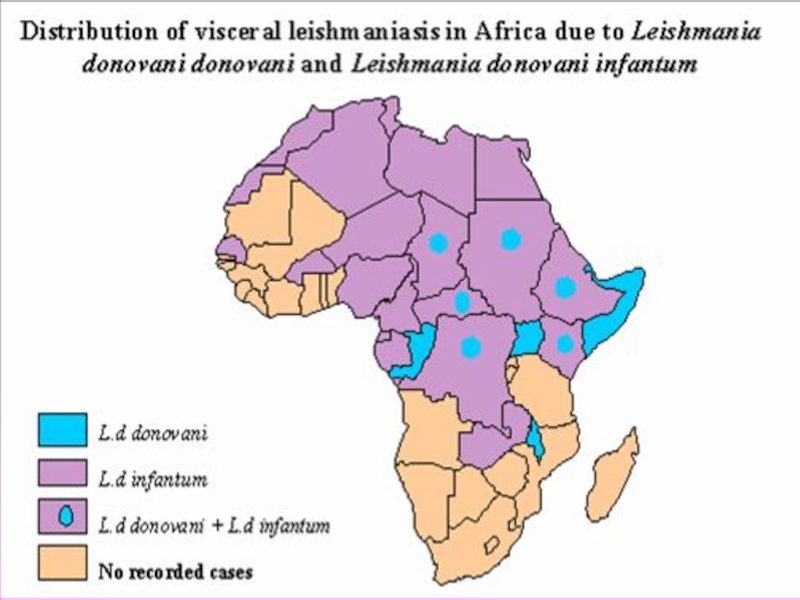
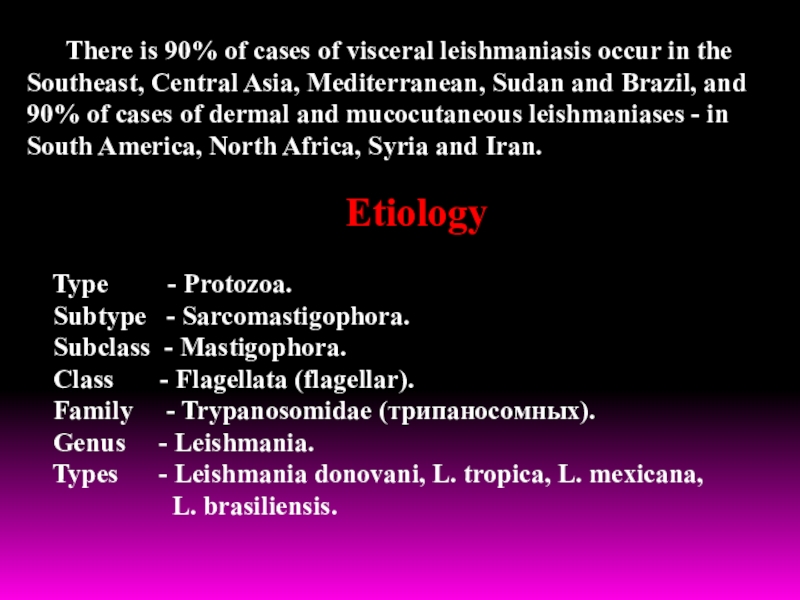
Слайд 11There is 90% of cases of visceral leishmaniasis occur in
the Southeast, Central Asia, Mediterranean, Sudan and Brazil, and 90%
of cases of dermal and mucocutaneous leishmaniases - in South America, North Africa, Syria and Iran.
Etiology
Type - Protozoa.
Subtype - Sarcomastigophora.
Subclass - Mastigophora.
Class - Flagellata (flagellar).
Family - Trypanosomidae (трипаносомных).
Genus - Leishmania.
Types - Leishmania donovani, L. tropica, L. mexicana,
L. brasiliensis.
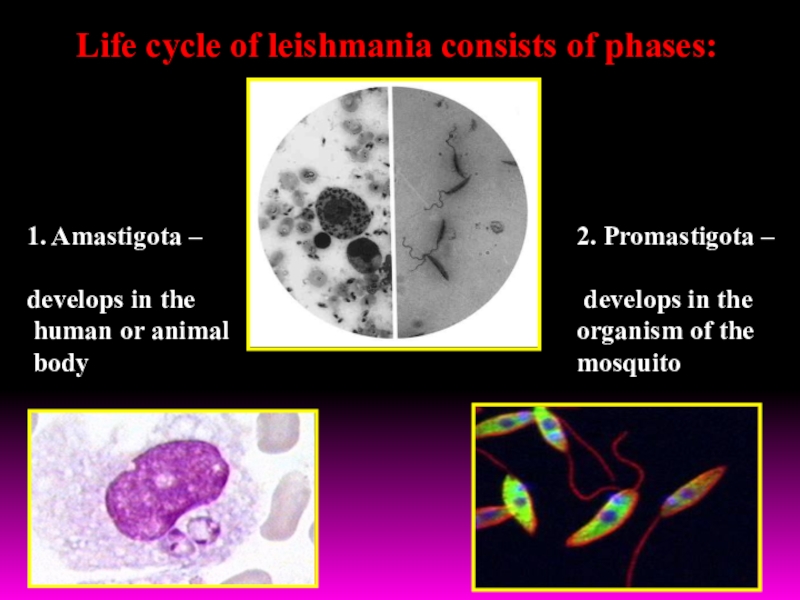
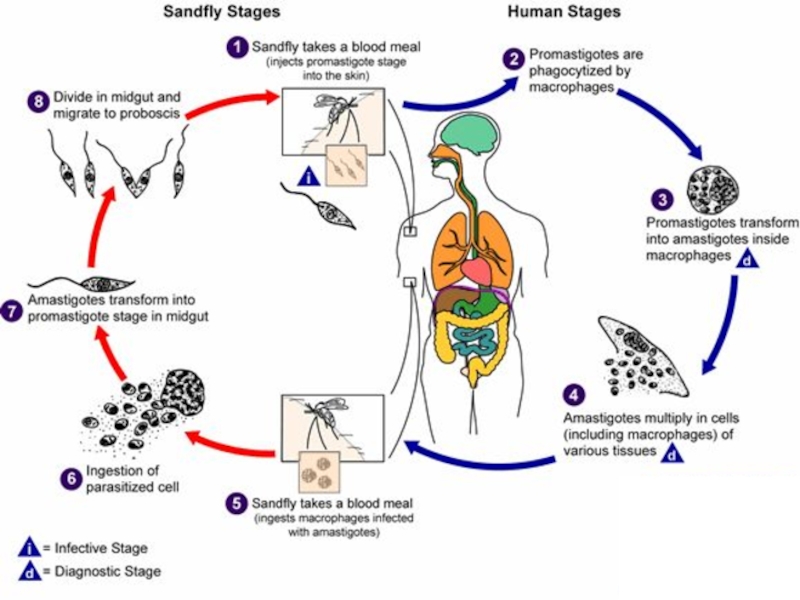
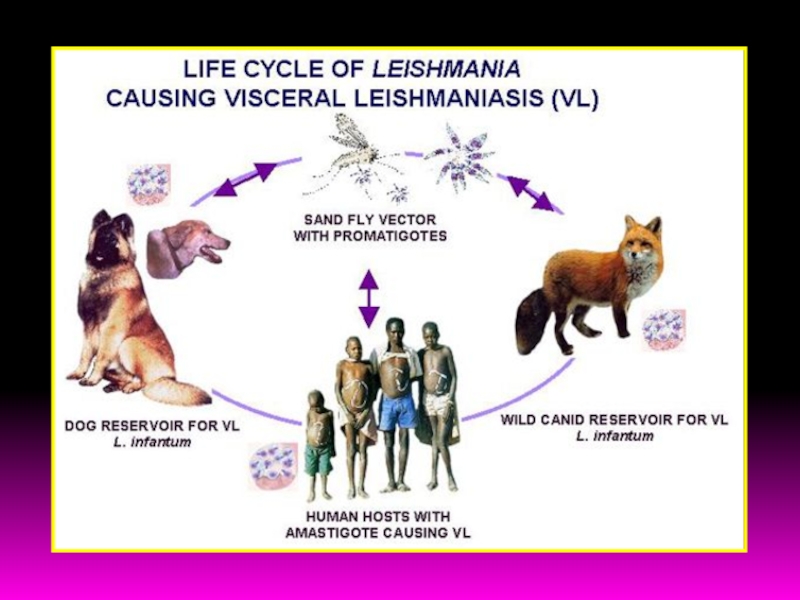
Слайд 12Life cycle of leishmania consists of phases:
1. Amastigota –
develops
in the
human or animal
body
2. Promastigota –
develops in
the
organism of the
mosquito
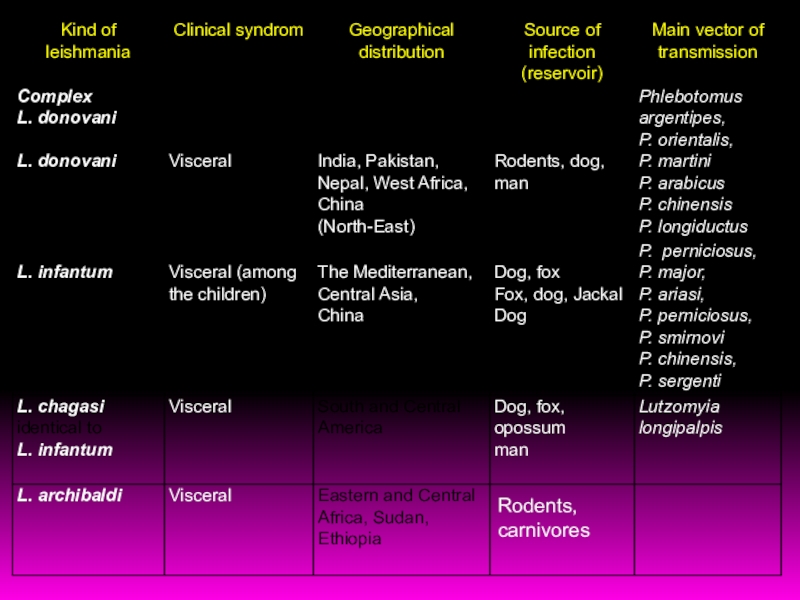
Слайд 14Visceral leishmaniasis - natural-focal transmissible protozoan infection, caused by a
special view of protozoa (Leishmania)
Disease is characterized by:
affection of reticul-endothelial
system,
clinically – prolonged course, undulating fever,
splenohepatomegaly, progressive anemia, leukopenia,
thrombocytopenia, cachexia.
Visceral leishmaniasis is a typical parasitic reticulo –
endotheliosis.
There is distinguished:
Indian visceral leishmaniasis (black illness, dumdum fever,
Indian Kala-Azar, Leishman-Donovan’s disease and other),
Mediterranean-Asian visceral leishmaniasis
(children's leishmaniasis),
East- African visceral leishmaniasis
(East- African Kala-Azar), American visceral leishmaniasis
(visceral leishmaniasis of New World).
Слайд 15 Epidemiology
Source of infection - sick man (in Africa and
other regions may be animals)
Vectors - mosquitoes type of Phlebotomus
argentipes. Vector becomes contagious in 6-8 days after blood suction, when leishmania finishes it’s life cycle.
A person infected after a mosquito bite. Beside the transmissible way there are possible non-traditional ways - blood transfusion, sexual contact.
Susceptibility of population is general, but young people (10-30 years) in rural areas are more sensitive.
Слайд 17General pathogenesis
Gates of infection - skin.
1. In a
few days (or weeks) of bite of infected mosquito
small papule or ulcer has appeared with
multiplicating leyshmania.
2. Then the parasites spread hematogenically throughout
the body and fix in the bone marrow, lymph nodes,
liver and spleen.
Clusters of leishmania, cause proliferation of connective tissue in parenhimatous organs, development of necrotic and degenerative processes.
Clinically – enlargement of liver, spleen, lymph nodes and disorder of their functions (bone marrow failure and GIT). Defeat of the blood-forming organs leads to severe leukopenia by reducing the number of granulocytes and progressive anemia.
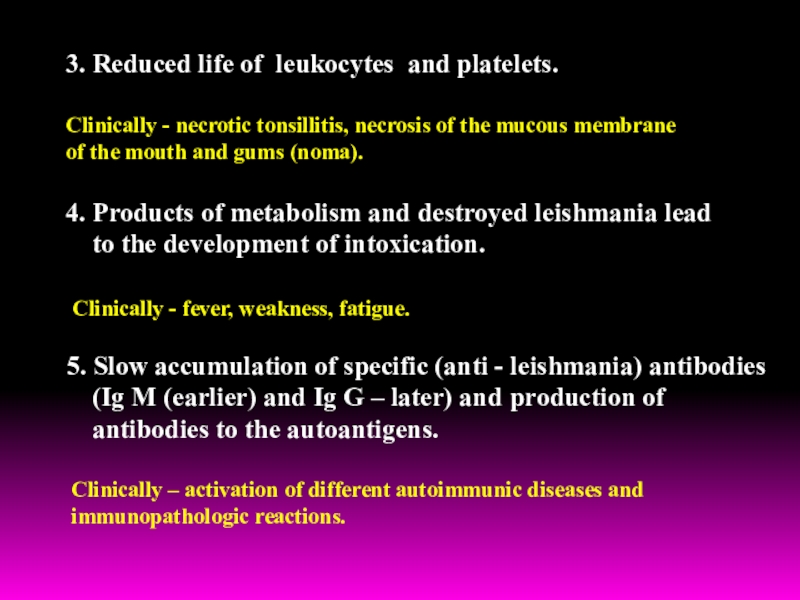
Слайд 183. Reduced life of leukocytes and platelets.
Clinically - necrotic tonsillitis,
necrosis of the mucous membrane
of the mouth and gums
(noma).
4. Products of metabolism and destroyed leishmania lead
to the development of intoxication.
Clinically - fever, weakness, fatigue.
5. Slow accumulation of specific (anti - leishmania) antibodies
(Ig M (earlier) and Ig G – later) and production of
antibodies to the autoantigens.
Clinically – activation of different autoimmunic diseases and
immunopathologic reactions.
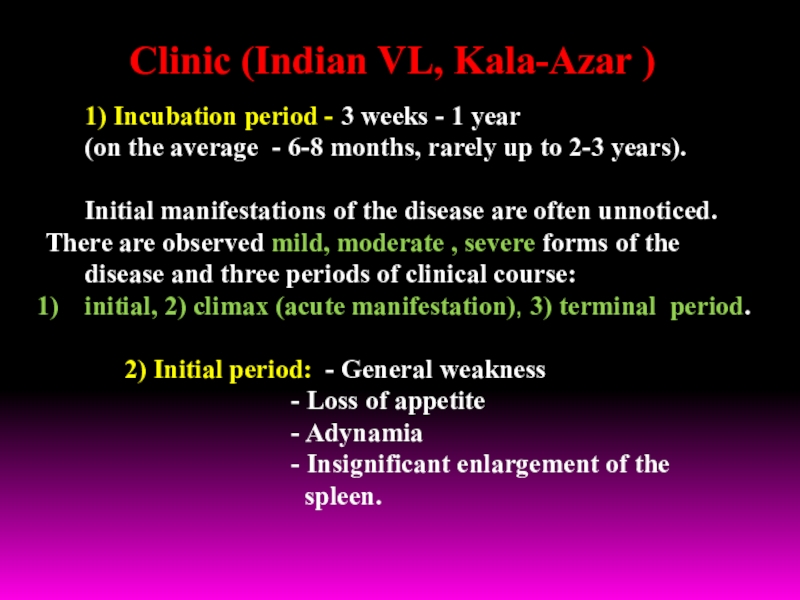
1) Incubation period - 3 weeks - 1 year
(on
the average - 6-8 months, rarely up to 2-3 years).
Initial manifestations of the disease are often unnoticed. There are observed mild, moderate , severe forms of the
disease and three periods of clinical course:
initial, 2) climax (acute manifestation), 3) terminal period.
2) Initial period: - General weakness
- Loss of appetite
- Adynamia
- Insignificant enlargement of the
spleen.
Clinic (Indian VL, Kala-Azar )
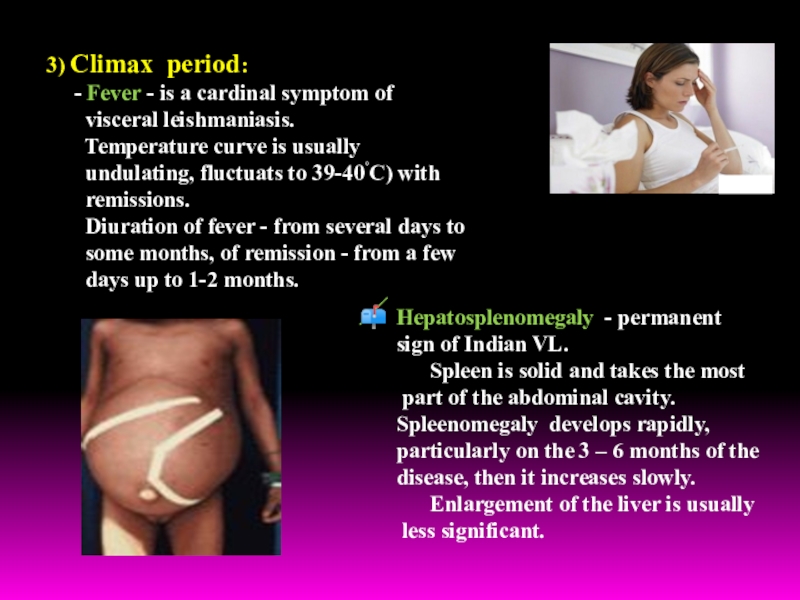
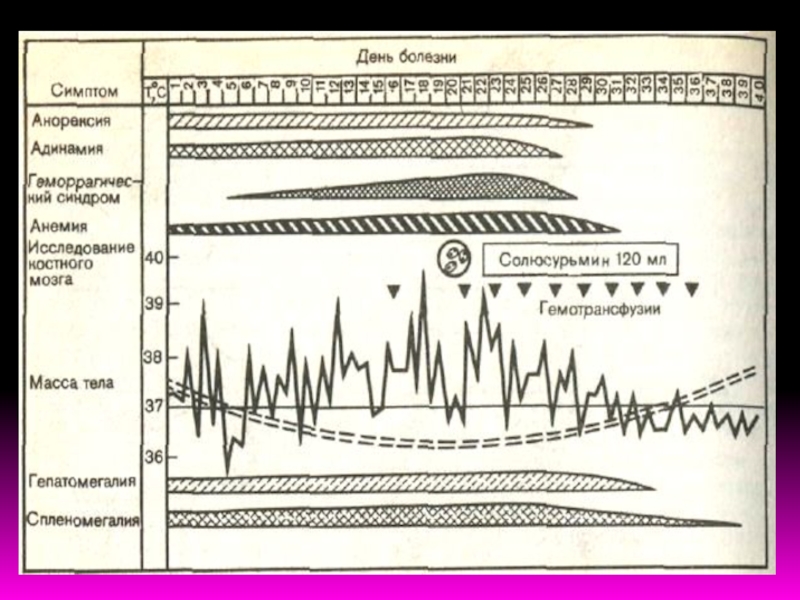
Слайд 213) Climax period:
- Fever - is a
cardinal symptom of
visceral leishmaniasis.
Temperature curve is usually
undulating, fluctuats to 39-40˚C) with
remissions.
Diuration of fever - from several days to
some months, of remission - from a few
days up to 1-2 months.
Hepatosplenomegaly - permanent
sign of Indian VL.
Spleen is solid and takes the most
part of the abdominal cavity.
Spleenomegaly develops rapidly,
particularly on the 3 – 6 months of the
disease, then it increases slowly.
Enlargement of the liver is usually
less significant.
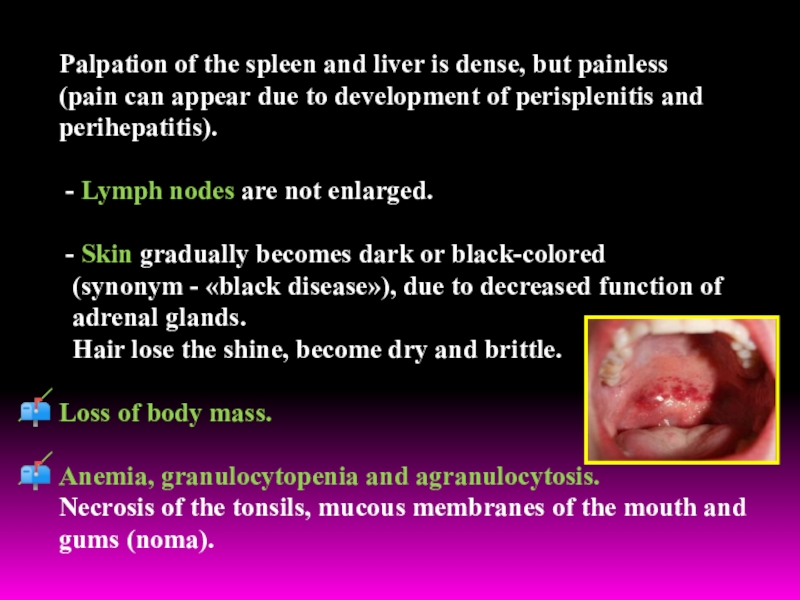
Слайд 22Palpation of the spleen and liver is dense, but painless
(pain can appear due to development of perisplenitis and
perihepatitis).
- Lymph nodes are not enlarged.
- Skin gradually becomes dark or black-colored
(synonym - «black disease»), due to decreased function of
adrenal glands.
Hair lose the shine, become dry and brittle.
Loss of body mass.
Anemia, granulocytopenia and agranulocytosis.
Necrosis of the tonsils, mucous membranes of the mouth and
gums (noma).
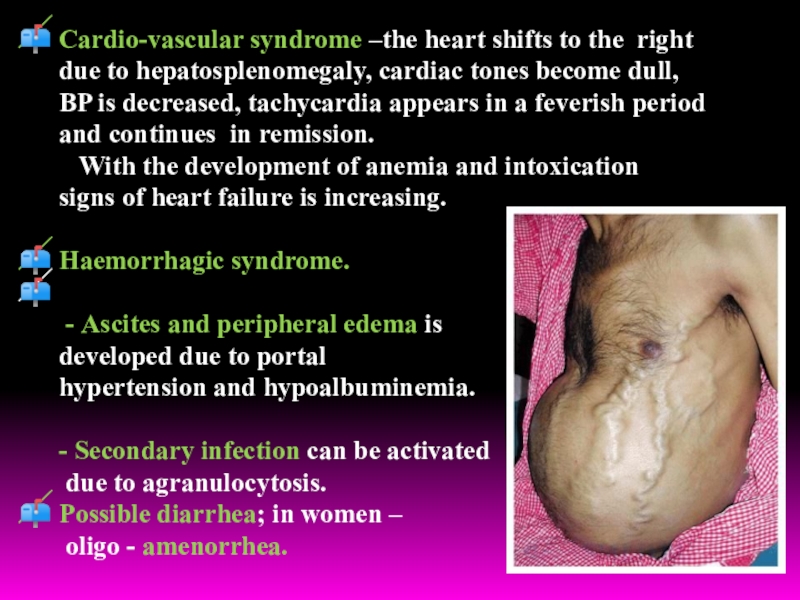
Слайд 23Cardio-vascular syndrome –the heart shifts to the right
due to hepatosplenomegaly,
cardiac tones become dull,
BP is decreased, tachycardia appears in
a feverish period
and continues in remission.
With the development of anemia and intoxication
signs of heart failure is increasing.
Haemorrhagic syndrome.
- Ascites and peripheral edema is
developed due to portal
hypertension and hypoalbuminemia.
- Secondary infection can be activated
due to agranulocytosis.
Possible diarrhea; in women –
oligo - amenorrhea.
Слайд 244) Terminal period:
- cachexia
- sharp hypotonia of muscles
-
skin is thin, through the abdominal wall can see the
border of enlarged spleen and liver.
Prognosis of mild forms of VL is favorable, but in severe
and complicated forms – serious.
In HIV-patients VL has malignant character and is
accompanied by resistance to specific therapy.
Слайд 25
In CBC: anemia (Hb – up to 40—50 g/l),
leukopenia
to 2—2,5х109/l and less, neutropenia
at relative lymphocytosis.
Uneosinophilia –
constant sign.
Coagulation of blood and erythrocyte resistance is decreased,
ESR sharply increased (till 90 mm/h).
5-10% of patients have skin leishmanoid, wich develops
in 1-2 years of effective treatment and consist of macula,
nodulus papilloma. Leishmania contained in leishmanoid
can survive many years.
Thus, a patient with skin leishmanoid – reservoir of the agent
and the source of invasion of mosquitoes for many years.
Слайд 27Mediterranean Kala – Azar
- Most cases of co-infection are
registered among men,
aged 20-40 years.
- 25-75% of HIV-infected
and 1,5-9% of AIDS-patients
suffers from visceral leishmaniasis. That why VL in
HIV-infected - the most frequent cause of opportunistic
infections.
- Hematogenic (syringe) way is easier realized due to high
concentration of leyshmania in the blood of HIV-patients
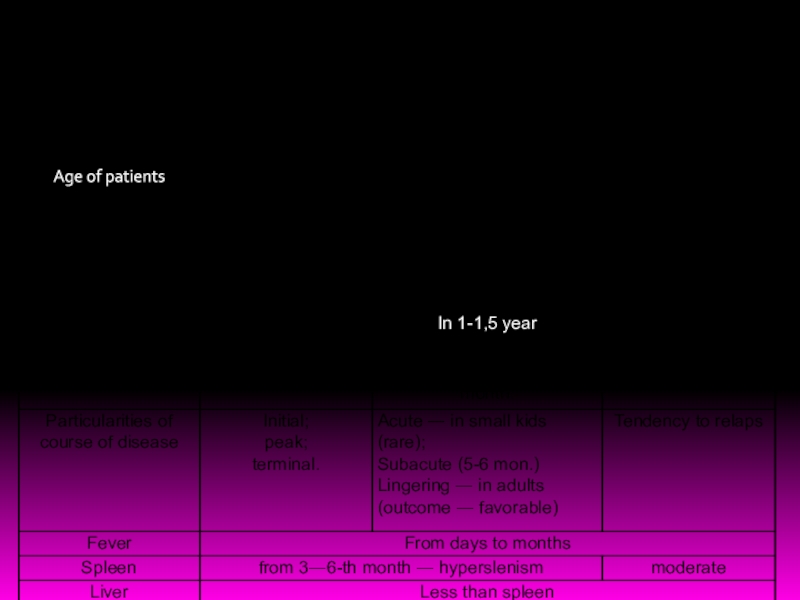
Слайд 28The most significant features of Mediterranean-Asian visceral leishmaniasis are:
1) incubation
period - within 1 month to 1 year (on an
average 3-5 months);
2) skin leishmanoid is absent;
3) involvment in pathological process peripheral and visceral lymph nodes with the development of mesadenitis;
4) frequent development of hemorrhages and bacterial pneumonia;
5) hyperpigmentation of skin is absent , skin is pale, grey-colored;
6) primary affect as papules, sometimes covered with scale before the manifestation of the disease;
7) the disease may occur in acute, subacute and chronic forms.
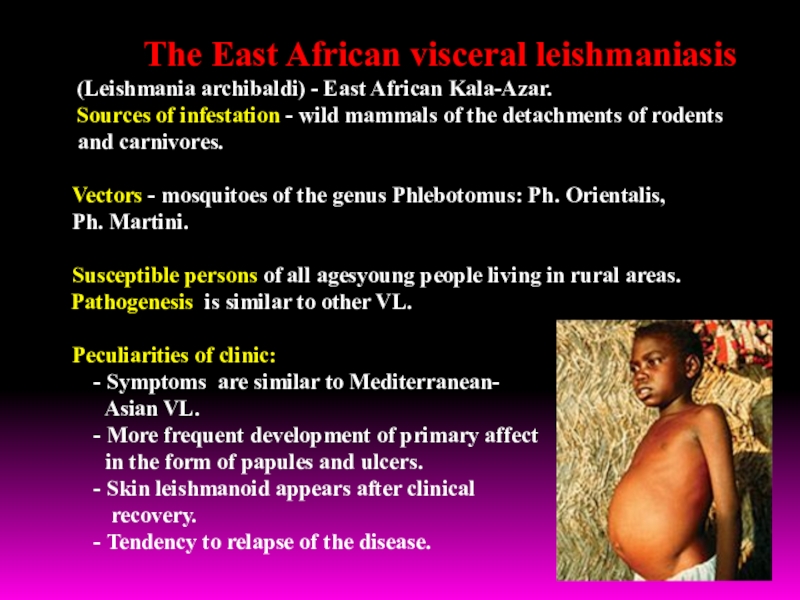
Слайд 30 The East African visceral leishmaniasis
(Leishmania archibaldi) - East African Kala-Azar.
Sources of infestation - wild mammals of the detachments of rodents
and carnivores.
Vectors - mosquitoes of the genus Phlebotomus: Ph. Orientalis,
Ph. Martini.
Susceptible persons of all agesyoung people living in rural areas.
Pathogenesis is similar to other VL.
Peculiarities of clinic:
- Symptoms are similar to Mediterranean-
Asian VL.
- More frequent development of primary affect
in the form of papules and ulcers.
- Skin leishmanoid appears after clinical
recovery.
- Tendency to relapse of the disease.
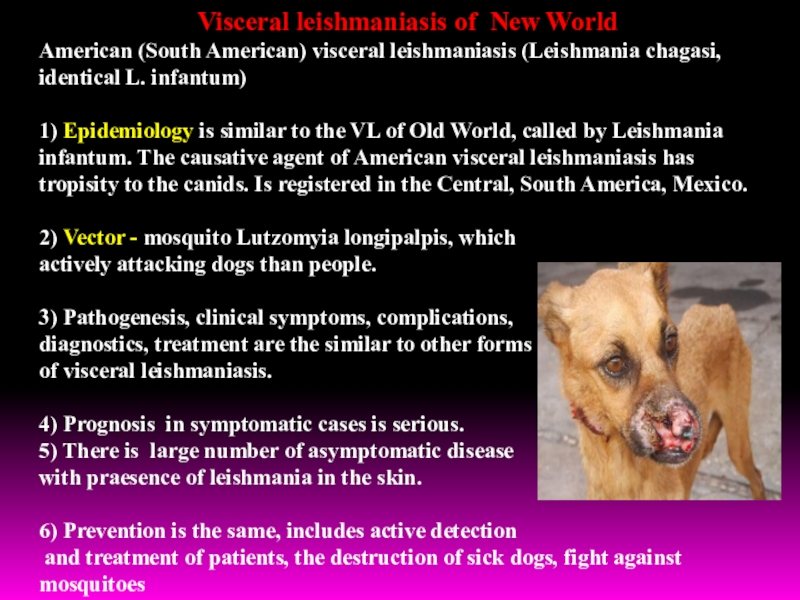
leishmaniasis of New World
American (South American) visceral leishmaniasis (Leishmania chagasi,
identical L. infantum)
1) Epidemiology is similar to the VL of Old World, called by Leishmania infantum. The causative agent of American visceral leishmaniasis has tropisity to the canids. Is registered in the Central, South America, Mexico.
2) Vector - mosquito Lutzomyia longipalpis, which
actively attacking dogs than people.
3) Pathogenesis, clinical symptoms, complications,
diagnostics, treatment are the similar to other forms
of visceral leishmaniasis.
4) Prognosis in symptomatic cases is serious.
5) There is large number of asymptomatic disease
with praesence of leishmania in the skin.
6) Prevention is the same, includes active detection
and treatment of patients, the destruction of sick dogs, fight against mosquitoes
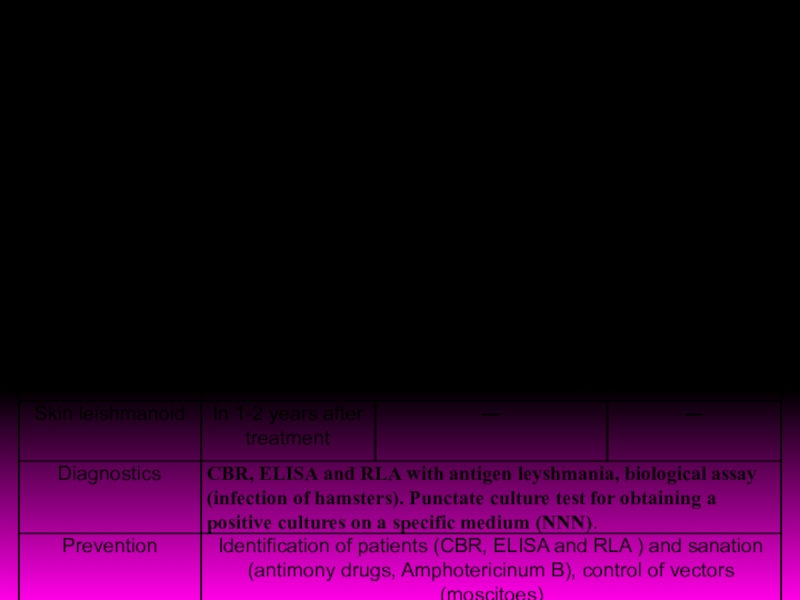
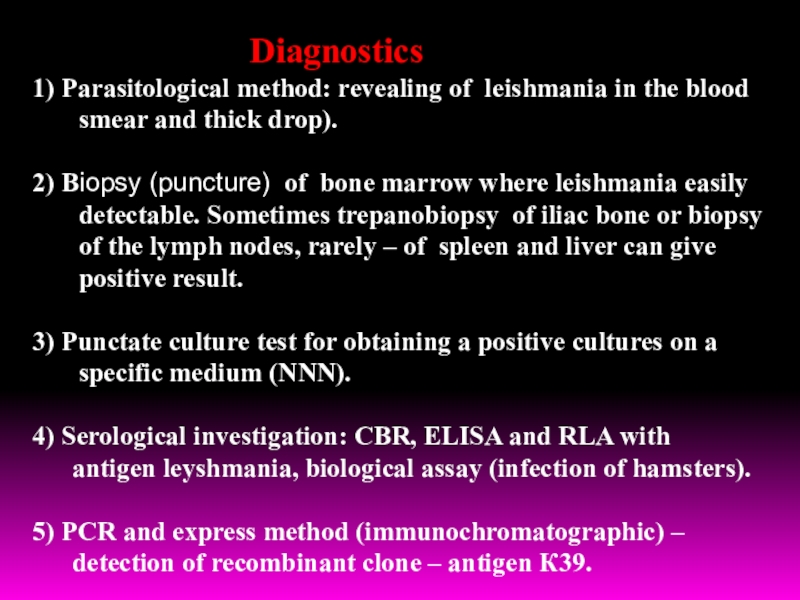
Parasitological method: revealing of leishmania in the blood
smear and
thick drop).
2) Biopsy (puncture) of bone marrow where leishmania easily
detectable. Sometimes trepanobiopsy of iliac bone or biopsy
of the lymph nodes, rarely – of spleen and liver can give
positive result.
3) Punctate culture test for obtaining a positive cultures on a
specific medium (NNN).
4) Serological investigation: CBR, ELISA and RLA with
antigen leyshmania, biological assay (infection of hamsters).
5) PCR and express method (immunochromatographic) –
detection of recombinant clone – antigen К39.
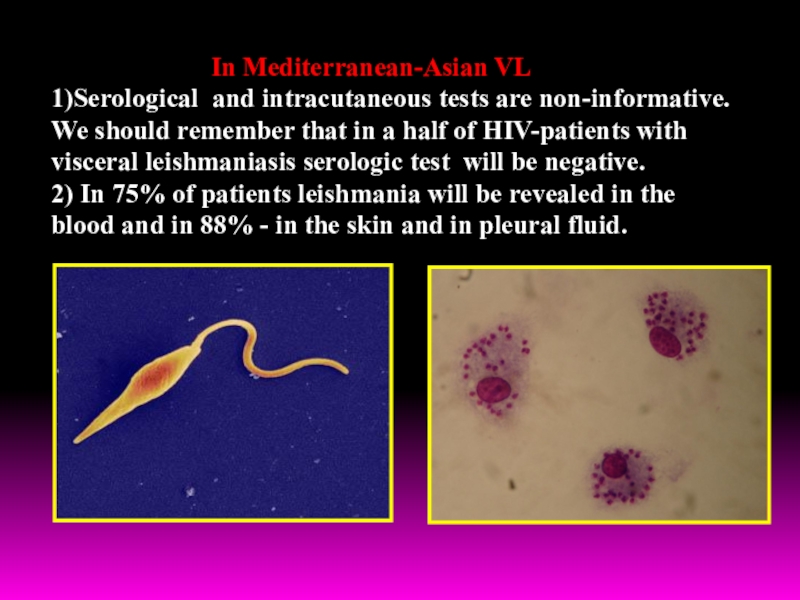
Mediterranean-Asian VL
1)Serological and intracutaneous tests are non-informative.
We should remember that
in a half of HIV-patients with
visceral leishmaniasis serologic test will be negative.
2) In 75% of patients leishmania will be revealed in the
blood and in 88% - in the skin and in pleural fluid.
Слайд 36Treatment
For the treatment of visceral leishmaniasis,
used drugs of 5-valent antimony:
1. Solusurmine
2. Pentostame – sodium stibogluconatis
3.Glucantime - synonyms: Meglumini stibias
Contraindications: pneumonic tuberculosis, severe violations of the liver
and kidney function.
Side-reactions: fever, cough, vomiting, polyneuritis, myocarditis.
Intradaction: Intramuscularly deeply.
Daily dose - 0,06 g/kg of body mass.
On the first day ¼ of necessary dose, on the second – a half of necessary
dose, on the 3rd day - ¾ of daily dose, 4-day - full dose.
The course of treatment is 10-15 injection.
Repeat a course through the 4-6 weeks.
At non effective therapy with antimony drugs appoint Amphotericin B and paromicyne!
Aminozidine can be administered simultaneously with drugs 5-valent antimony in two syringes in different places.
Слайд 37For the treatment of VL also can be applied:
Pentamidine
- 4 mg/kg/day – during 11 weeks
Amphotericin B, full dose
for a course –
20-30 mg/kg – during 10-20 days.
In addition to specific treatment, is necessary
pathogenic therapy and prevention of secondary
bacterial infection.
It is necessary to widely use restorative therapy, drugs iron and phosphorus (per os), vitamin B12, diet, rich in animal proteins and vitamins.
- Treatment of post-Kala-Azar skin leishmanoid is the same as visceral leishmaniasis, but the course of treatment continuances to 4 months.
The first oral medication for the treatment of VL – miltefosine had been registered in India.
It is suggested that miltefosine will replace drugs of 5-valent antimony and amphotericin as the drugs of first line.
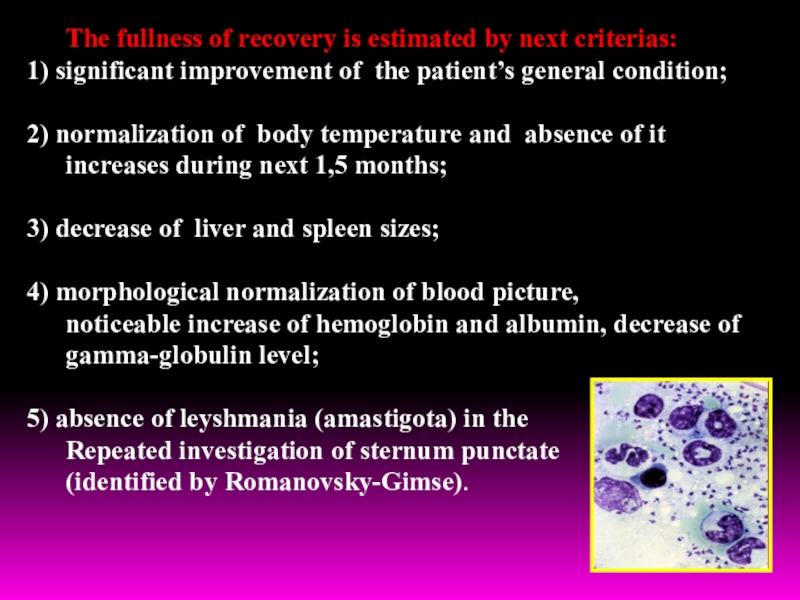
Слайд 38The fullness of recovery is estimated by next criterias:
1) significant
improvement of the patient’s general condition;
2) normalization of body temperature
and absence of it
increases during next 1,5 months;
3) decrease of liver and spleen sizes;
4) morphological normalization of blood picture,
noticeable increase of hemoglobin and albumin, decrease of
gamma-globulin level;
5) absence of leyshmania (amastigota) in the
Repeated investigation of sternum punctate
(identified by Romanovsky-Gimse).