Слайд 1Pathology and complications
of
Diabetes Mellitus
Слайд 2Learning objectives
1. Understand why good diabetic control reduces the incidence
of long-term complications.
2. Differentiate between micro- and macrovascular damage, and
the diseases they cause.
3. Understand the other complications that are associated with diabetes.
4. Identify some of mechanisms by which glucose can cause long-term complication of diabetes
Слайд 3Diabetes Mellitus
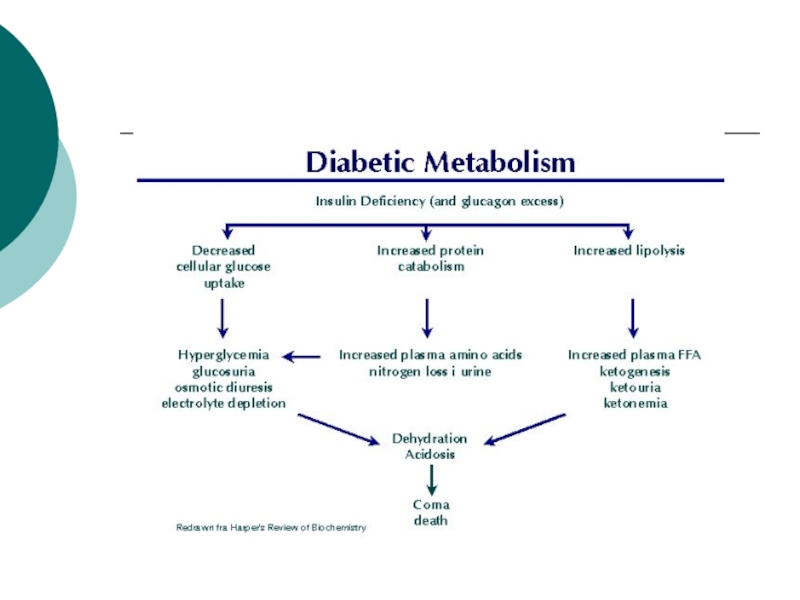
Metabolic disease affecting CHO, protein and fat metabolism due
to insulin deficiency or inefficiency.
Two types: type I (insulin dependant)
and Type II (insulin independent).
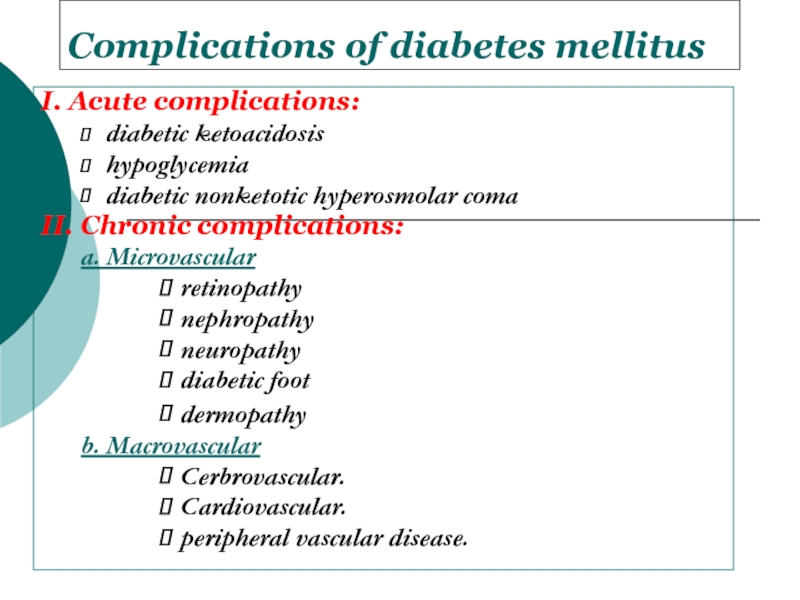
Слайд 5Complications of diabetes mellitus
I. Acute complications:
diabetic ketoacidosis
hypoglycemia
diabetic nonketotic hyperosmolar coma
II.
Chronic complications:
a. Microvascular
retinopathy
nephropathy
neuropathy
diabetic foot
dermopathy
b. Macrovascular
Cerbrovascular.
Cardiovascular.
peripheral vascular disease.
Слайд 6Diabetic ketoacidosis (DKA)
May be the 1st presentation of type 1
DM.
Result from absolute insulin deficiency or increase requirement.
Mortality rate around
5%.
Слайд 7Pathophysiology of DKA
Ketosis
Dehydration
Electrolyte imbalance
Слайд 8Diagnosis of DKA
Hyperglycemia
Ketonuria and ketonemia
Acidosis (PH< 7.3 )
Слайд 9Predisposing factors for DKA
Infection
Trauma
Myocardial Infarction
Stroke
Surgery
Emotional stress
Слайд 10Clinical presentation of DKA
Polyurea and polydepsia.
Nausea and vomiting.
Anorexia and abdominal
pain.
Tachycardia.
Fruity odor of the breath.
Hypotonia, stupor and coma.
Sign of dehydration.
Слайд 11Treatment of DKA
Fluid replacement.
Insulin therapy for hyperglycemia.
Electrolyte correction.
Acidosis correction.
Treatment
of precipitating cause.
Слайд 12Complication of DKA
Cerebral edema
Vascular thrombosis
Infection
M I
Acute gastric dilatation
Respiratory distress syndrome
Слайд 13 Hypoglycemic coma
Hypoglycemia is the most frequent acute complication in
type 1 diabetes.
Hypoglycemia is the level of blood glucose
at which autonomic and neurological dysfunction begins
Слайд 14Clinical manifestations of hypoglycemia:
Autonomic dysfunctions:
1. Hunger
2. Tremor
3. Palpitation
4. Anxiety
5. Pallor
6. Sweating
Слайд 15Neurologic dysfunctions:
1. Impaired thinking
2.
Change of mood
3. Irritability
4.
Headache
5. Convulsion
6. Coma
Слайд 16Predisposing factors
Missed meal
Change in physical activity
Alterations or errors in insulin
dosage
Alcohol ingestion
Слайд 17Treatment of hypoglycemia
In mild cases oral rapidly absorbed carbohydrate
In sever
cases (comatose patient) iv hypertonic glucose 25% or 50% concentration
Glucagons
injection
Слайд 18Chronic Complications of DM
A. Macrovascular Complications:
B. Microvascular Complications:
Слайд 19Macro-vascular Complications:
Ischemic heart diseases.
Cerebrovascular diseases.
Peripheral vascular diseases.
Diabetic patients
have a 2 to 6 times higher risk for development
of these complications than the general population
Слайд 20Macro-vascular Complications:
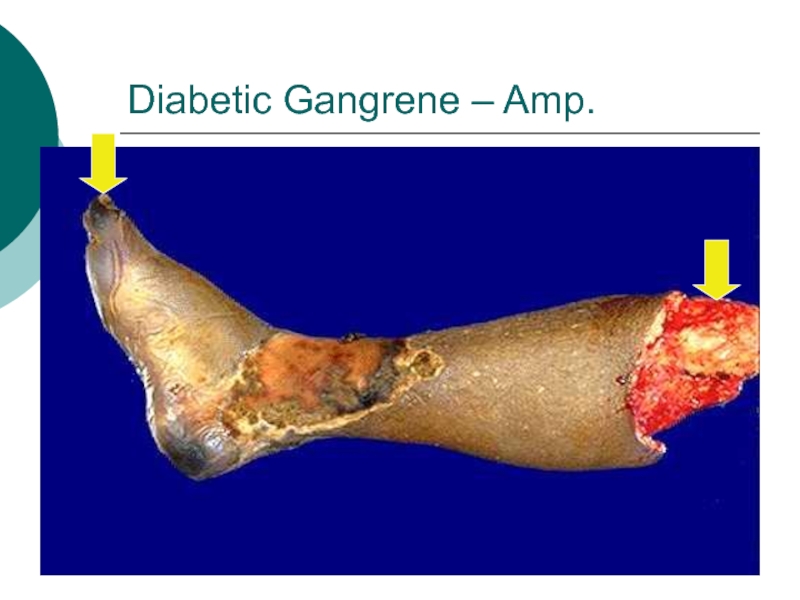
Accelerated atherosclerosis involving the aorta and large- and medium-sized
arteries.
Myocardial infarction, caused by atherosclerosis of the coronary arteries,
is the most common cause of death in diabetics.
Gangrene of the lower extremities.
Hypertension due to Hyaline arteriolosclerosis.
Слайд 21Hypertension in DM
Type 1
present after several years of DM
affects about
30% of patients.
Secondary to
nephropathy
Activation of the Renin angiotensin system
Type 2
Mostly
present at diagnosis
Affects about 60% of patients
Secondary to insulin resistance
Activation of the sympathetic nervous system
Слайд 22Dyslipidaemia in DM
Most common abnormality is HDL and
Triglycerides
A low HDL is the most constant predictor of Cardiovascular
disease in DM.
Слайд 23Screening for Macrovascular Complications
1. Examine pulses for cardiovascular diseases.
2. Lipogram (lipid
profile).
3. ECG.
4. Blood pressure.
Слайд 24Microvascular complications are specific to diabetes and related to longstanding
hyperglycaemia.
Both Type1 DM and Type2 DM are susceptible to microvascular
complications.
The duration of diabetes and the quality of diabetic control are important determinants of microvascular abnormalities.
Microvascular Complications
Слайд 25Pathophysiology of microvascular disease
In diabetes, the microvasculature shows both functional
and structural abnormalities.
The structural hallmark of diabetic
microangiopathy is thickening of the capillary basement membrane.
Many chemical changes in basement membrane composition have been identified in diabetes, including increased type IV collagen and its glycosylation (i.e binding of glucose to wall of blood vessels).
Слайд 26The main functional abnormalities include increased capillary permeability, viscosity, and
disturbed platelet function.
These changes occur early in the course
of diabetes and precede organ failure by many years.
Increased capillary permeability is manifested in the retina by leakage of fluorescein and in the kidney by increased urinary losses of albumin which predict eventual renal failure.
Слайд 27
Platelets from diabetic patients show an exaggerated tendency to aggregate,
perhaps mediated by altered prostaglandin metabolism.
Plasma and whole blood viscosity
are increased in diabetes.
These defects together with the platelet abnormalities may cause stasis in the microvaculature, leading to increased intravascular pressure and to tissue hypoxia.
There is abnormal production of von Willebrand factor and endothelial derived nitric oxide by endothelial cells which could contribute to tissue damage.
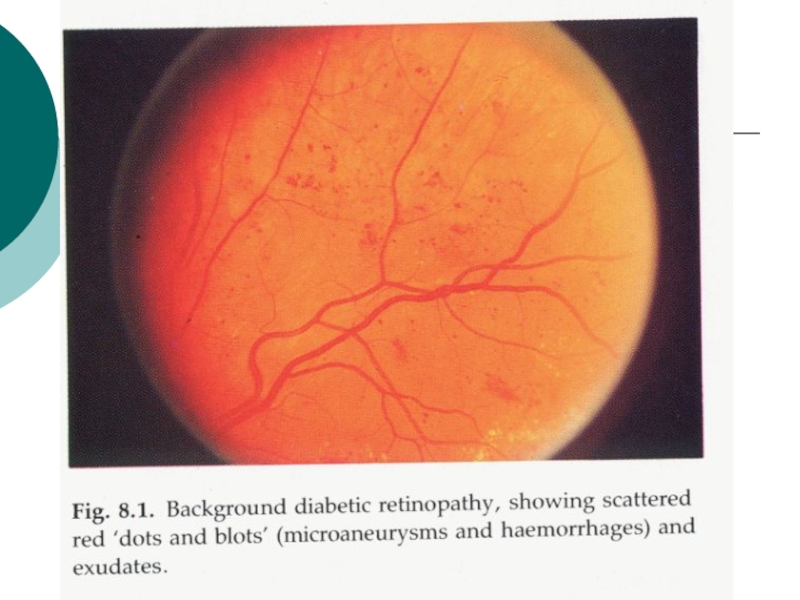
Слайд 281- Diabetic retinopathy
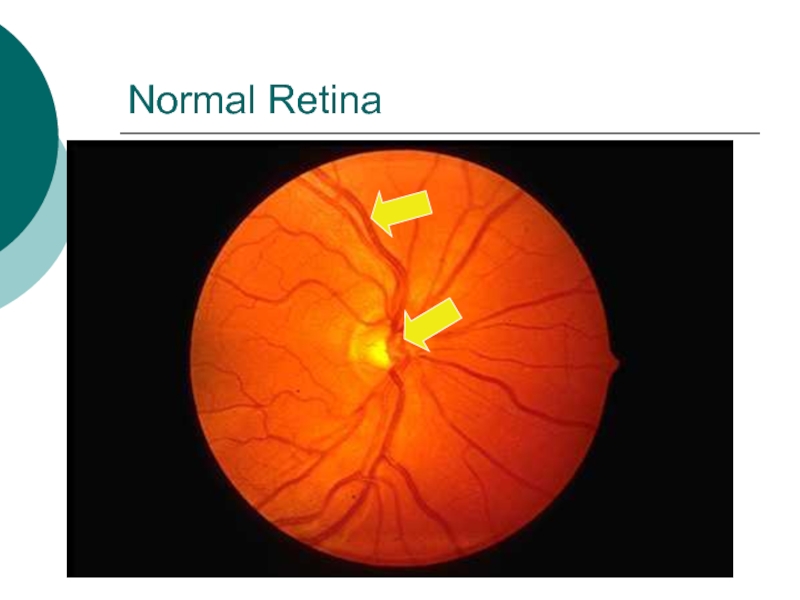
* Pathogenesis:
Histologically the earliest lesion is thickening
of the capillary basement membrane.
On fluorescein angiography the first abnormality
is the capillary dilatations (microaneurysms).
Microaneurysm may give rise to haemorrhage or exudate.
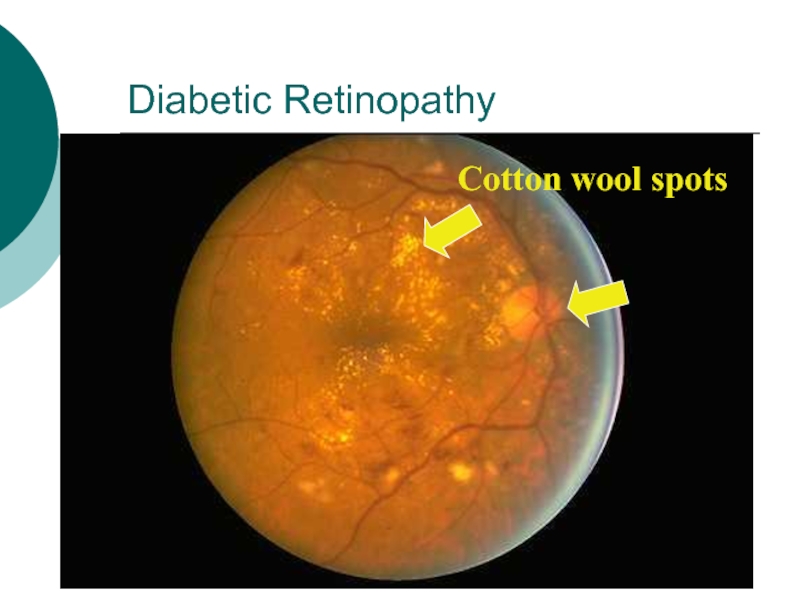
Vascular occlusion, initially of capillaries and later of arteries and veins, leads to large ischaemic areas (cotton-wool spots).
Слайд 31Diabetic Retinopathy
Cotton wool spots
Слайд 32Other Eye Complications
- Cataracts.
- Glaucoma
- Macular edema.
Ischaemic maculopathy.
Proliferative retinopathy.
Vitreous
Bleeding.
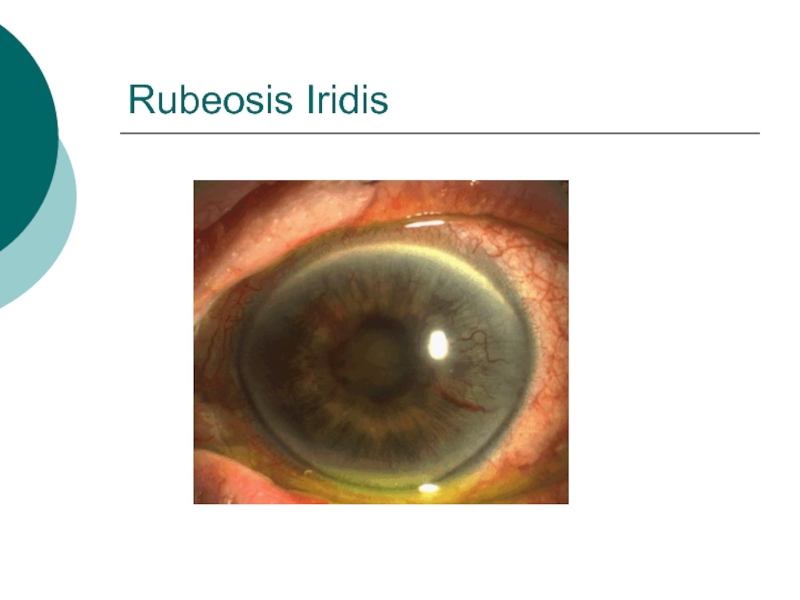
Rubeosis Iridis
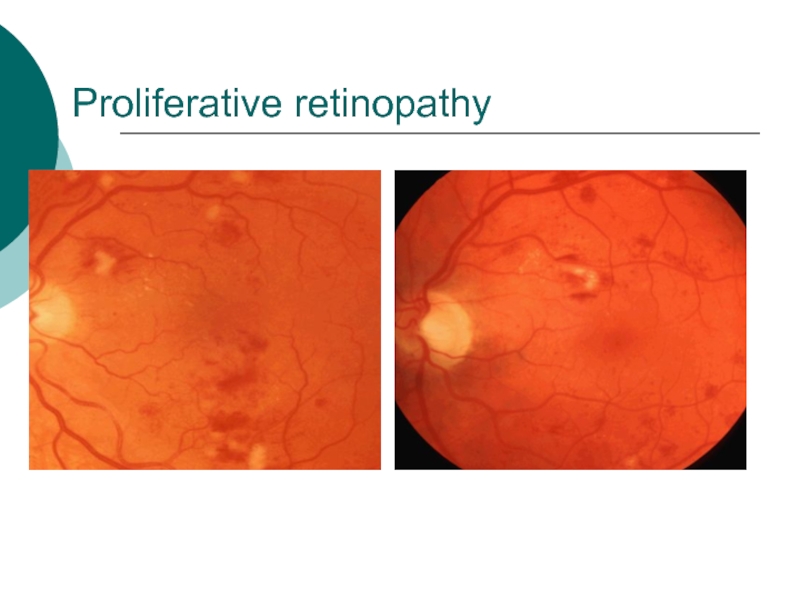
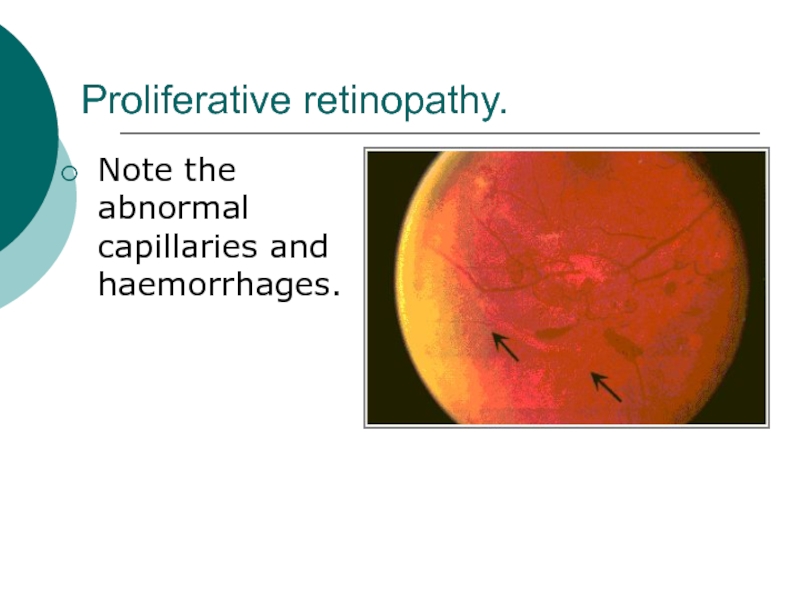
Слайд 36Proliferative retinopathy.
Note the abnormal capillaries and haemorrhages.
Слайд 372- Diabetic Nephropathy (DN)
- Diabetic nephropathy is defined by persistent
albuminuria (>300 mg/day), decrease glomerular filtration rate and rising blood
pressure.
- About 20 – 30% of patients with diabetes develop diabetic nephropathy
Слайд 38Risk factors of DN
Duration of DM.
Family History of hypertension. Cardiovascular
disease, nephropathy.
Hyperglycemia.
Hypertension.
Microalbuminuria.
Male gender.
Cigarette smoking.
Слайд 39Pathogenesis:
The glomerular and vascular lesions are linked to hyperglycemia.
Nonenzymatic glycosylation
to glomerular proteins results in accumulation of irreversible advanced glycosylation
end products in the glomerular mesangium and glomerular basement membrane.
This alteration leads to proteinuria and eventually glomerulosclerosis
Слайд 40Pathological pattern of DN
Diffuse form (more common): consist of thickining
of glomerular basement membrane with generalized mesangial thickenings.
The nodular form
(the Kimmelstiel-Wilson lesion): (accumulation of periodic acid schiff positive material are deposit in the periphery of glomerular tufts.
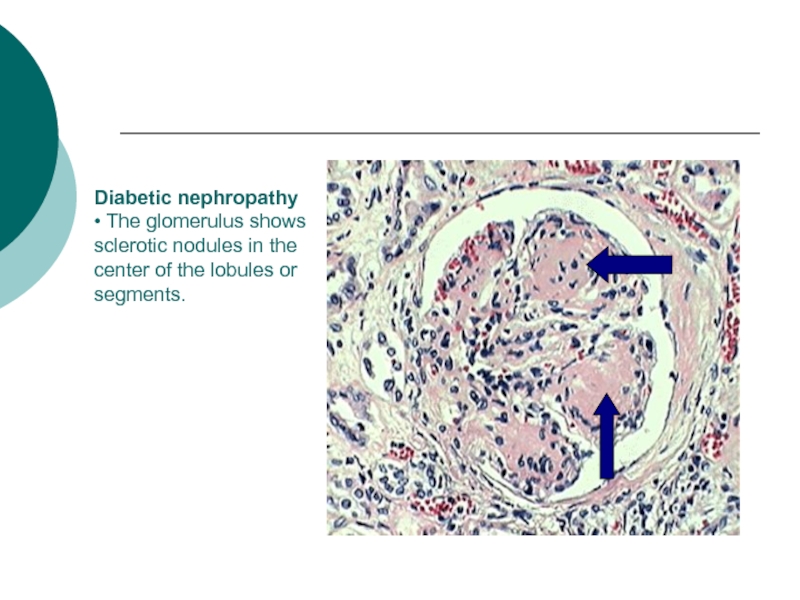
Слайд 41Diabetic nephropathy
• The glomerulus shows sclerotic nodules in the center of
the lobules or segments.
Слайд 42Treatment to prevent progression to DN
Glycaemic control.
ACE inhibitor .
Blood pressure
control.
Smoking cessation.
Proteins restriction.
Lipid reduction.
Слайд 434. Diabetic Neuropathy
1. Sensorimotor neuropathy.
2. Autonomic neuropathy.
Слайд 44Sensorimotor Neuropathy
Numbness, paresthesias.
Feet are mostly affected, hands are seldom affected.
Complicated
by ulceration (painless), charcot arthropathy.
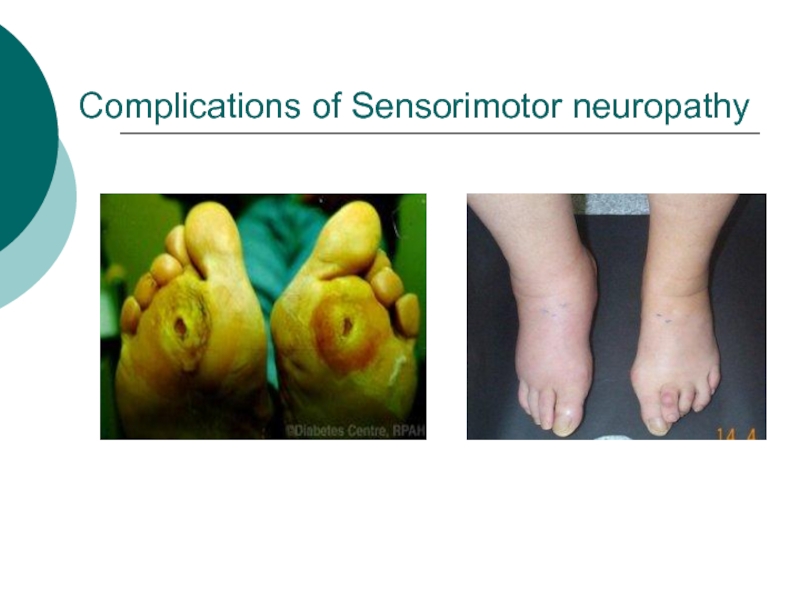
Слайд 45Complications of Sensorimotor neuropathy
Слайд 46Autonomic Neuropathy
Postural hypotension.
Diabetic diarrhea.
Neuropathic bladder.
Erectile dysfunction.
Слайд 475. Infections
Community acquired pneumonia
Acute bacterial cystitis
Acute pyelonephritis
Pyelonephritis
Perinephric abscess
Fungal cystitis.
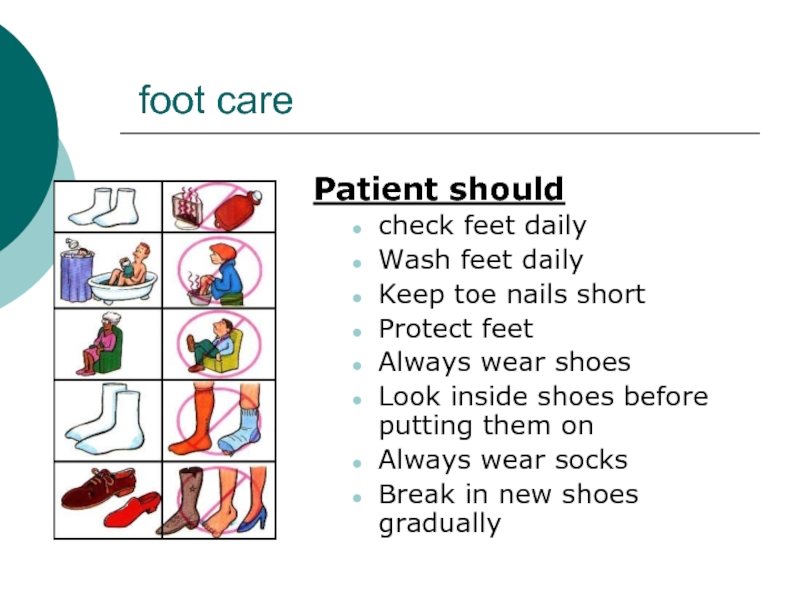
Слайд 48 foot care
Patient should
check feet daily
Wash feet daily
Keep toe
nails short
Protect feet
Always wear shoes
Look inside shoes before putting them
on
Always wear socks
Break in new shoes gradually
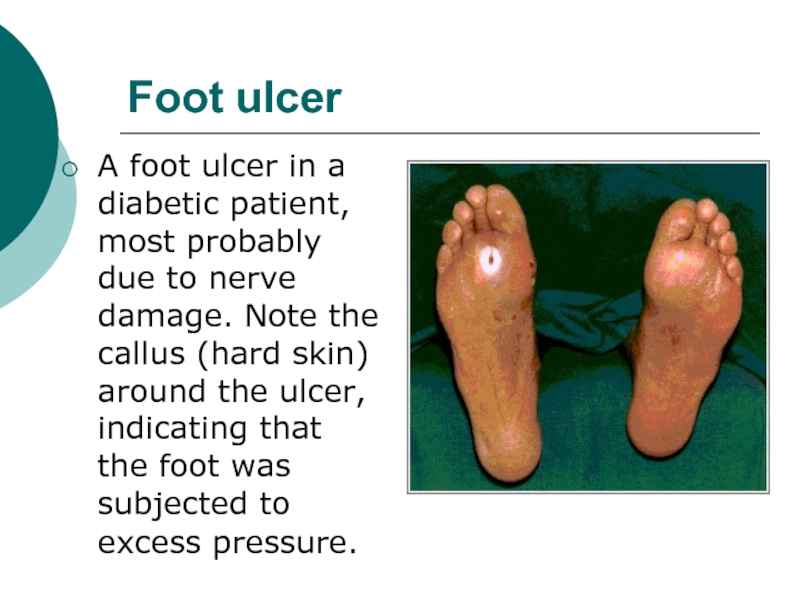
Слайд 49Foot ulcer
A foot ulcer in a diabetic patient, most probably
due to nerve damage. Note the callus (hard skin) around
the ulcer, indicating that the foot was subjected to excess pressure.