Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
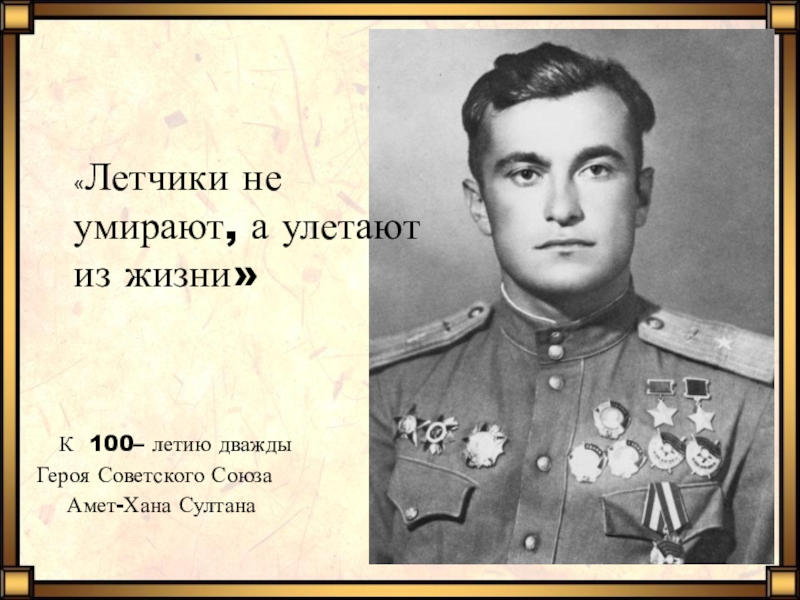
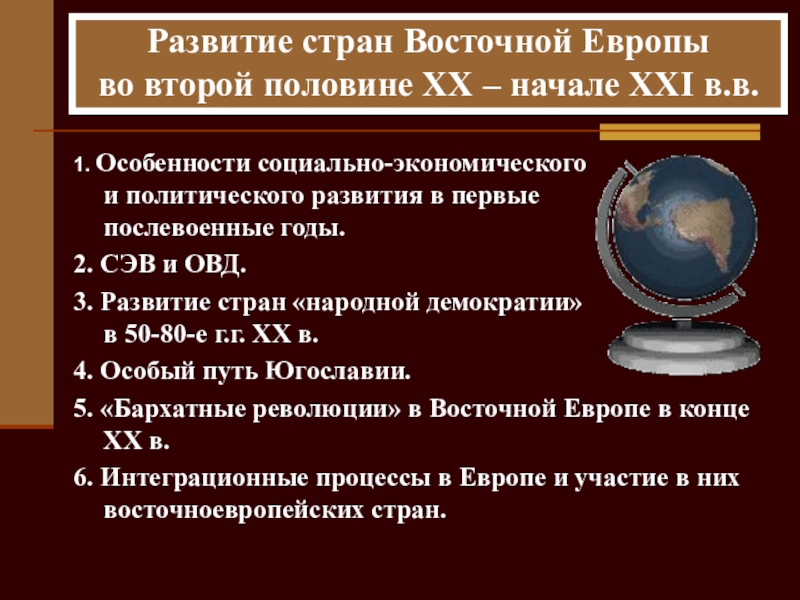
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
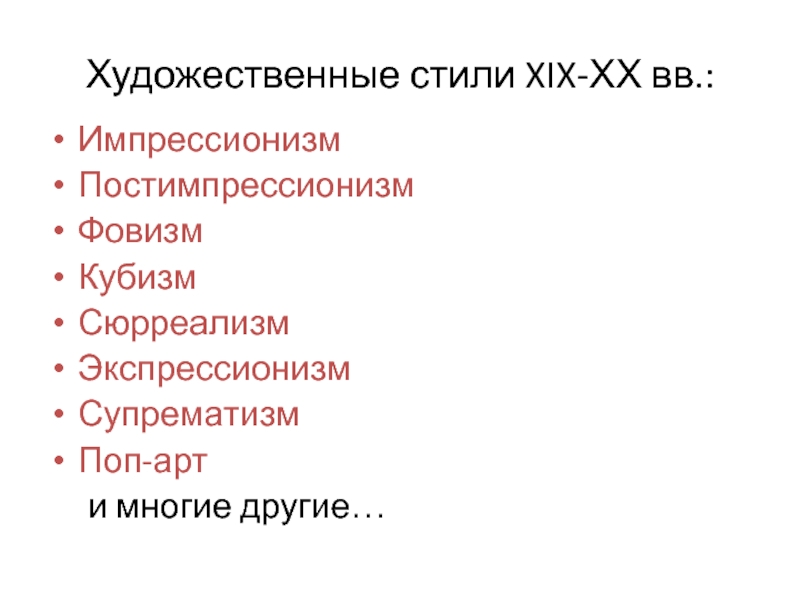
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Breech Presentation
Содержание
- 1. Breech Presentation
- 2. BackgroundIncidence20% at 28 weeks4% at termReasons for
- 3. Perinatal mortality is increased because…PrematurityCongenital malformationsBirth asphyxiaBirth
- 4. Current ControversiesManagement of term breechElective Caesarean or
- 5. Recent HistoryBy 1990The practice of ECV had
- 6. 2000 The Term Breech TrialRCT in 121
- 7. Risks to the baby & the mode
- 8. Risks to the mother & mode of
- 9. Events since the publication of the Term
- 10. Other Major StudiesA prospective study of 2526
- 11. Problems with the Term Breech Trial…Most of
- 12. Two year follow up of babies in
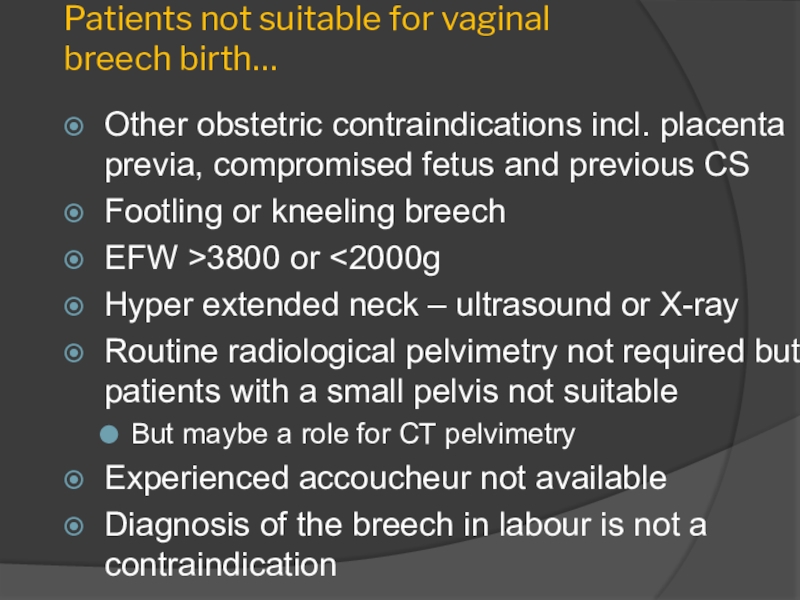
- 13. Patients not suitable for vaginal breech birth…Other
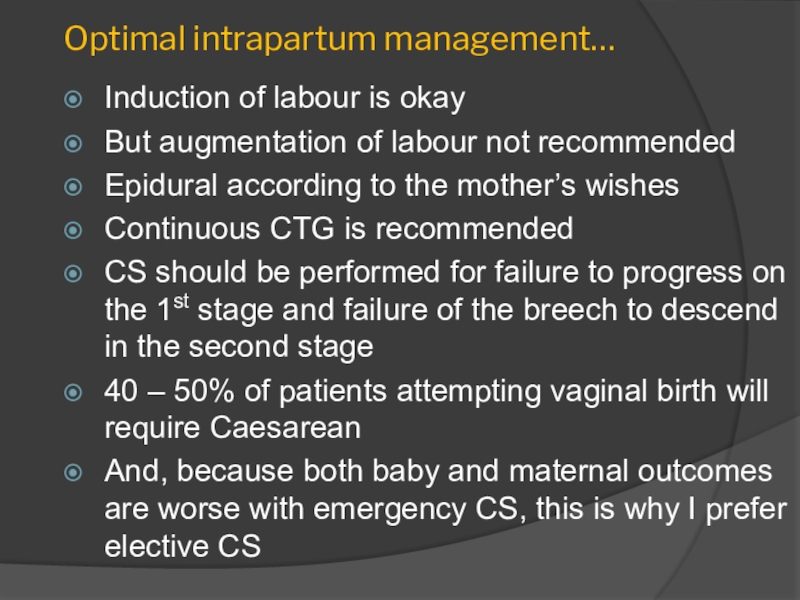
- 14. Optimal intrapartum management…Induction of labour is okayBut
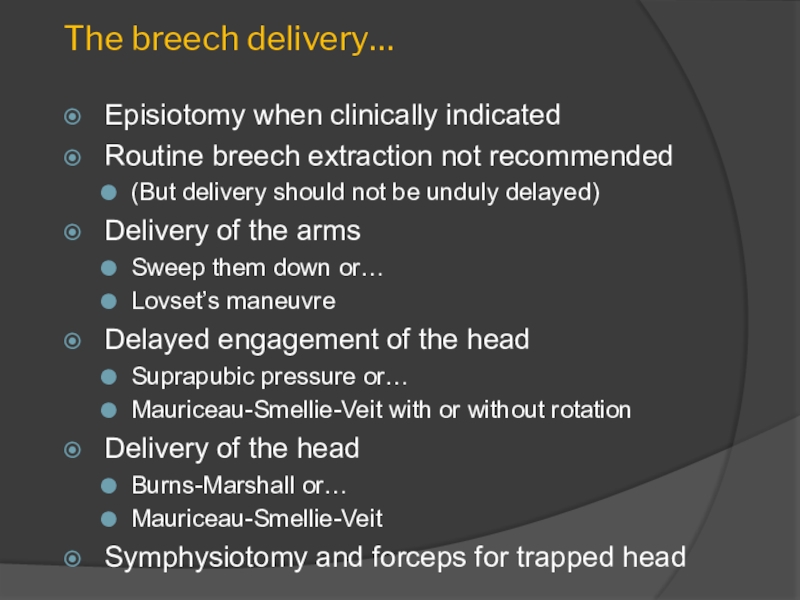
- 15. The breech delivery…Episiotomy when clinically indicatedRoutine breech
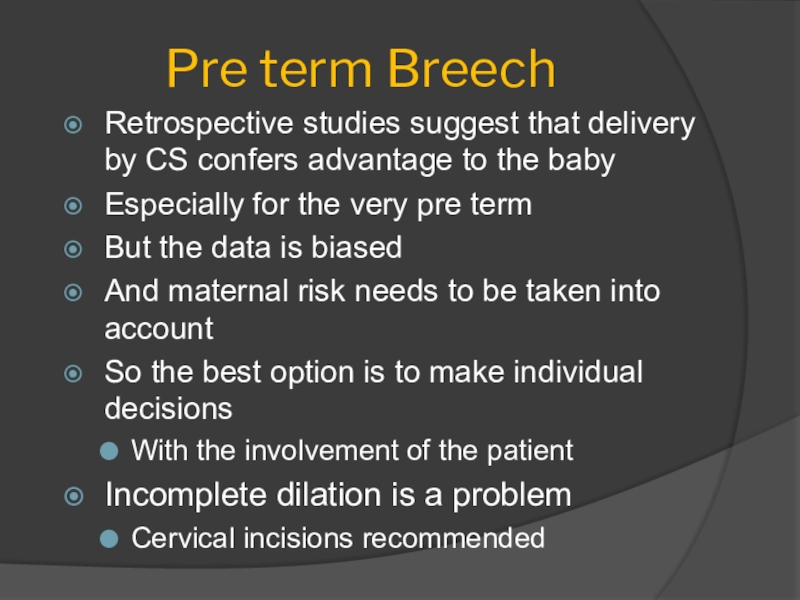
- 16. Pre term BreechRetrospective studies suggest that delivery
- 17. Twins and BreechMany clinicians recommend CS when
- 18. Detection of breech presentation…Antenatal diagnosis is inconsequential
- 19. Because breech delivery is a preventable condition
- 20. ECV is EffectiveRCT’s of external version at
- 21. Risks with ECVCord entanglementPost procedure monitoring by
- 22. ECV is SafeNo differences in any measure
- 23. An attempt at ECV is not contraindicated
- 24. ECV is not successively achieved by…Maternal posturing5
- 25. Unanswered Questions about ECVWhen it should be
- 26. The Early ECV Trial1543 ♀ in 21
- 27. Скачать презентанцию
BackgroundIncidence20% at 28 weeks4% at termReasons for a breechUterine abnormalitiesPlacental localisationExcessive or reduced amniotic fluidFetal abnormalitiesFetal attitude – extended legsJust chance
Слайды и текст этой презентации
Слайд 2Background
Incidence
20% at 28 weeks
4% at term
Reasons for a breech
Uterine abnormalities
Placental
localisation
chanceСлайд 3Perinatal mortality is increased because…
Prematurity
Congenital malformations
Birth asphyxia
Birth trauma
“the biggest part
of the baby is coming last”
Increased risk of long term
“handicap” even when delivered by CS Слайд 4Current Controversies
Management of term breech
Elective Caesarean or vaginal birth
Selection of
patients for breech birth
Techniques in vaginal breech delivery
Pre term breech
and the twin breechThe detection of breech presentation
The Role of ECV
Is it effective
Is it safe
When should it be performed
How is it best achieved
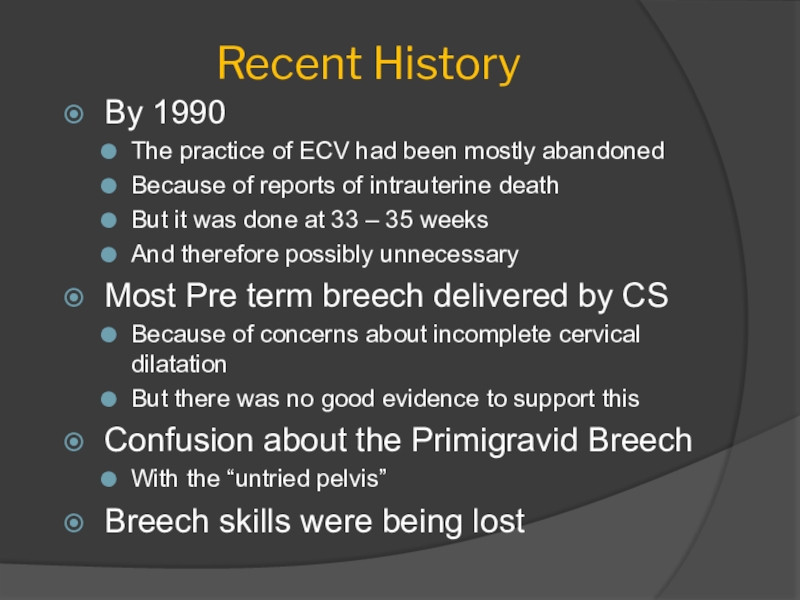
Слайд 5Recent History
By 1990
The practice of ECV had been mostly abandoned
Because
of reports of intrauterine death
But it was done at 33
– 35 weeksAnd therefore possibly unnecessary
Most Pre term breech delivered by CS
Because of concerns about incomplete cervical dilatation
But there was no good evidence to support this
Confusion about the Primigravid Breech
With the “untried pelvis”
Breech skills were being lost
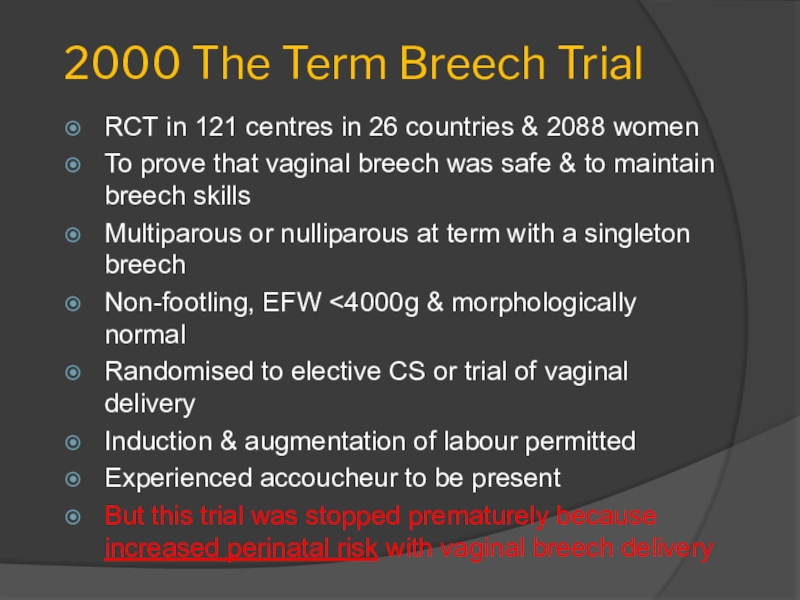
Слайд 62000 The Term Breech Trial
RCT in 121 centres in 26
countries & 2088 women
To prove that vaginal breech was safe
& to maintain breech skillsMultiparous or nulliparous at term with a singleton breech
Non-footling, EFW <4000g & morphologically normal
Randomised to elective CS or trial of vaginal delivery
Induction & augmentation of labour permitted
Experienced accoucheur to be present
But this trial was stopped prematurely because increased perinatal risk with vaginal breech delivery
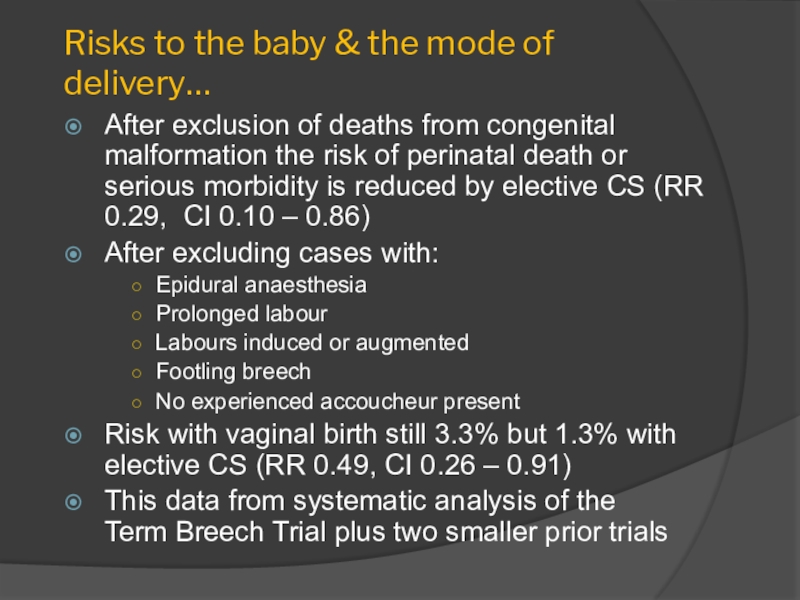
Слайд 7Risks to the baby & the mode of delivery…
After exclusion
of deaths from congenital malformation the risk of perinatal death
or serious morbidity is reduced by elective CS (RR 0.29, CI 0.10 – 0.86)After excluding cases with:
Epidural anaesthesia
Prolonged labour
Labours induced or augmented
Footling breech
No experienced accoucheur present
Risk with vaginal birth still 3.3% but 1.3% with elective CS (RR 0.49, CI 0.26 – 0.91)
This data from systematic analysis of the Term Breech Trial plus two smaller prior trials
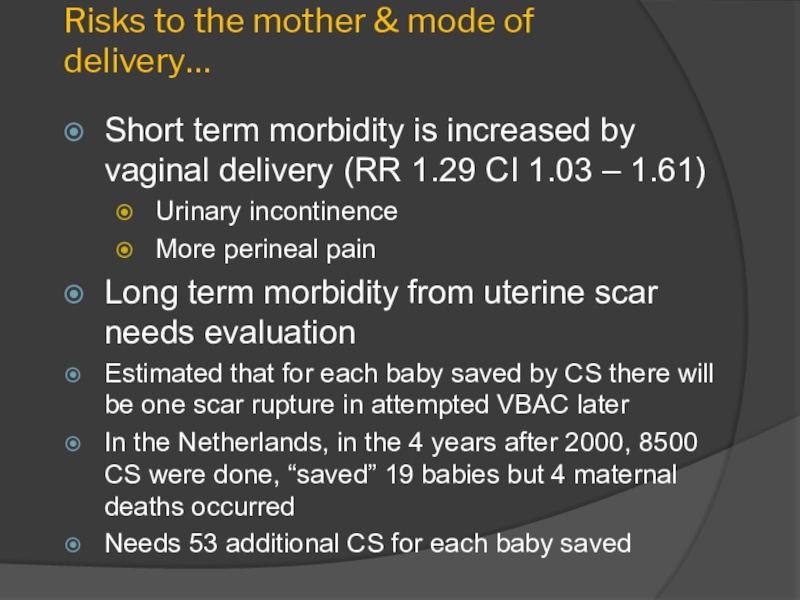
Слайд 8Risks to the mother & mode of delivery…
Short term morbidity
is increased by vaginal delivery (RR 1.29 CI 1.03 –
1.61)Urinary incontinence
More perineal pain
Long term morbidity from uterine scar needs evaluation
Estimated that for each baby saved by CS there will be one scar rupture in attempted VBAC later
In the Netherlands, in the 4 years after 2000, 8500 CS were done, “saved” 19 babies but 4 maternal deaths occurred
Needs 53 additional CS for each baby saved
Слайд 9Events since the publication of the Term Breech Trial…
Many criticisms
of the Trial
Follow up of the Term Breech Trial babies
found no long term benefit from CSA prospective study of 2526 women in France and Belgium analyzed on an intention-to-treat basis found no benefit from elective CS
RCOG, RANZCOG and Canadian guidelines state that trial of vaginal breech delivery is a safe option
All also recommend attempting ECV
Слайд 10Other Major Studies
A prospective study of 2526 women in France
and Belgium analyzed on an intention-to-treat basis found no benefit
from elective CSDutch study of 58,320 term breech 1999-2007
Elective CS rose from 24% to 60%
PNM fell from 1.3 to 0.7 per 1000
PNM for those having vaginal birth did not change
Слайд 11Problems with the Term Breech Trial…
Most of the patients recruited
in developed countries
Subgroup analysis suggests that the outcome cannot be
extrapolated to resource poor countriesMany of the centres involved had historically low rates of vaginal breech birth
Raises questions about the experience of the “skilled accoucheur”
Criteria for patients for trial of vaginal birth were too liberal
Lumping fetal mortality and morbidity was inappropriate for long term outcomes
3 deaths in the vaginal group vs none in the CS group is NS (and one death was a surviving twin)
Слайд 12Two year follow up of babies in the Term Breech
Trial…
Was conducted in those Centres thought to achieve 80% follow
upOutcomes measured were perinatal death and neurodevelopmental delay
There were no significant differences (RR 1.09 CI 0.52 – 2.30)
The smaller number of perinatal deaths in the CS group was balanced by a higher number of 2 year-olds with neuro-developmental delay
Calls into question the measures of neonatal morbidity (which were more frequent in the vaginal birth group)
Слайд 13Patients not suitable for vaginal breech birth…
Other obstetric contraindications incl.
placenta previa, compromised fetus and previous CS
Footling or kneeling breech
EFW
>3800 or <2000gHyper extended neck – ultrasound or X-ray
Routine radiological pelvimetry not required but patients with a small pelvis not suitable
But maybe a role for CT pelvimetry
Experienced accoucheur not available
Diagnosis of the breech in labour is not a contraindication
Слайд 14Optimal intrapartum management…
Induction of labour is okay
But augmentation of labour
not recommended
Epidural according to the mother’s wishes
Continuous CTG is recommended
CS
should be performed for failure to progress on the 1st stage and failure of the breech to descend in the second stage40 – 50% of patients attempting vaginal birth will require Caesarean
And, because both baby and maternal outcomes are worse with emergency CS, this is why I prefer elective CS
Слайд 15The breech delivery…
Episiotomy when clinically indicated
Routine breech extraction not recommended
(But
delivery should not be unduly delayed)
Delivery of the arms
Sweep them
down or…Lovset’s maneuvre
Delayed engagement of the head
Suprapubic pressure or…
Mauriceau-Smellie-Veit with or without rotation
Delivery of the head
Burns-Marshall or…
Mauriceau-Smellie-Veit
Symphysiotomy and forceps for trapped head
Слайд 16Pre term Breech
Retrospective studies suggest that delivery by CS confers
advantage to the baby
Especially for the very pre term
But the
data is biasedAnd maternal risk needs to be taken into account
So the best option is to make individual decisions
With the involvement of the patient
Incomplete dilation is a problem
Cervical incisions recommended
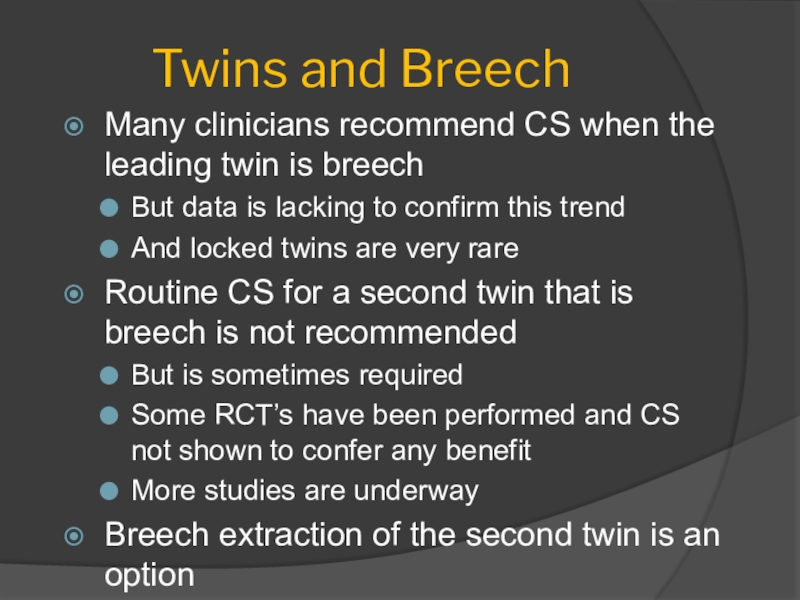
Слайд 17Twins and Breech
Many clinicians recommend CS when the leading twin
is breech
But data is lacking to confirm this trend
And locked
twins are very rareRoutine CS for a second twin that is breech is not recommended
But is sometimes required
Some RCT’s have been performed and CS not shown to confer any benefit
More studies are underway
Breech extraction of the second twin is an option
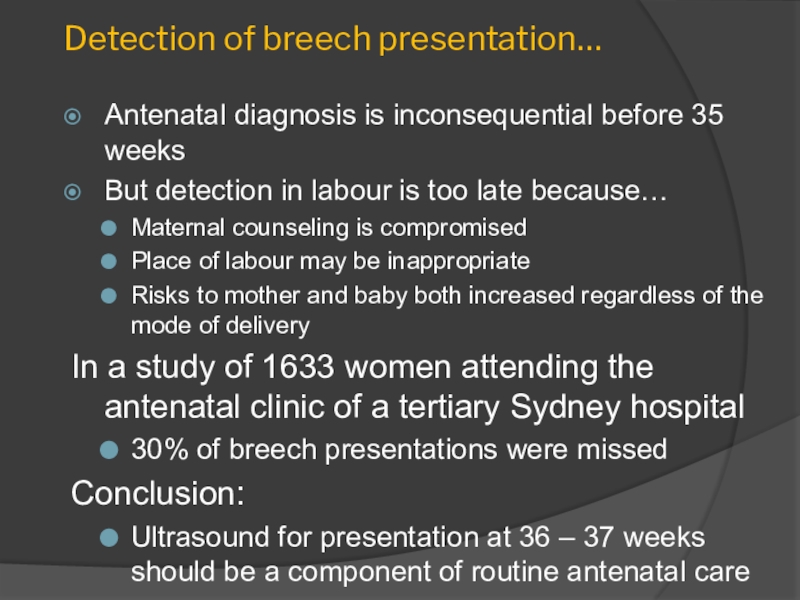
Слайд 18Detection of breech presentation…
Antenatal diagnosis is inconsequential before 35 weeks
But
detection in labour is too late because…
Maternal counseling is compromised
Place
of labour may be inappropriateRisks to mother and baby both increased regardless of the mode of delivery
In a study of 1633 women attending the antenatal clinic of a tertiary Sydney hospital
30% of breech presentations were missed
Conclusion:
Ultrasound for presentation at 36 – 37 weeks should be a component of routine antenatal care
Слайд 19Because breech delivery is a preventable condition that meets all
the criteria for a screening procedure
The Role of External Cephalic
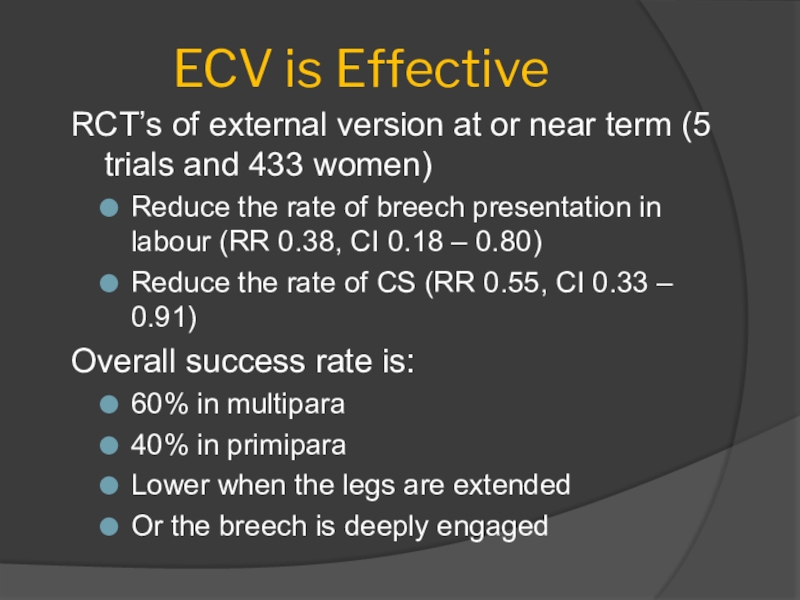
VersionСлайд 20ECV is Effective
RCT’s of external version at or near term
(5 trials and 433 women)
Reduce the rate of breech presentation
in labour (RR 0.38, CI 0.18 – 0.80)Reduce the rate of CS (RR 0.55, CI 0.33 – 0.91)
Overall success rate is:
60% in multipara
40% in primipara
Lower when the legs are extended
Or the breech is deeply engaged
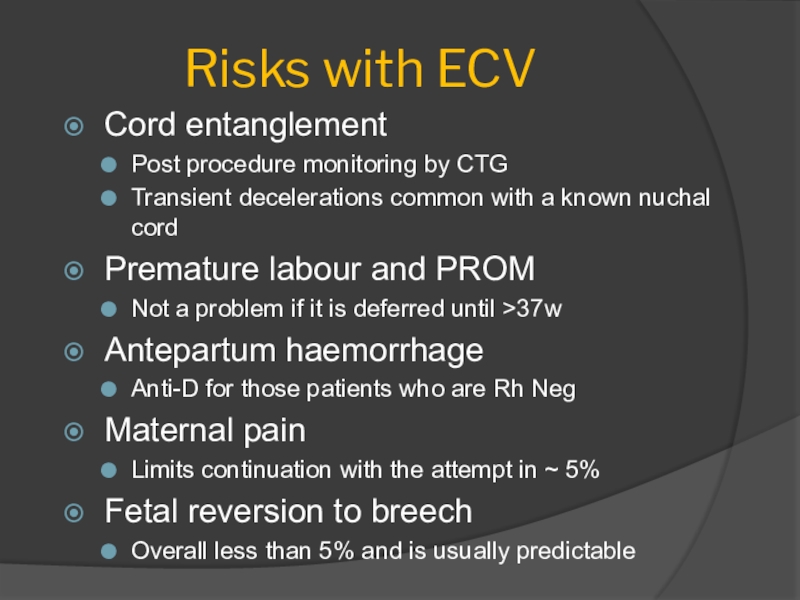
Слайд 21Risks with ECV
Cord entanglement
Post procedure monitoring by CTG
Transient decelerations common
with a known nuchal cord
Premature labour and PROM
Not a problem
if it is deferred until >37wAntepartum haemorrhage
Anti-D for those patients who are Rh Neg
Maternal pain
Limits continuation with the attempt in ~ 5%
Fetal reversion to breech
Overall less than 5% and is usually predictable
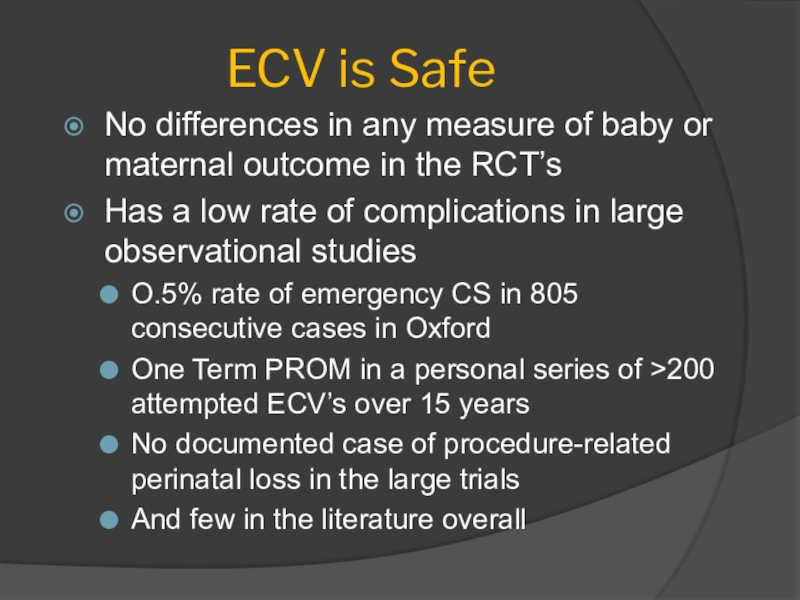
Слайд 22ECV is Safe
No differences in any measure of baby or
maternal outcome in the RCT’s
Has a low rate of complications
in large observational studiesO.5% rate of emergency CS in 805 consecutive cases in Oxford
One Term PROM in a personal series of >200 attempted ECV’s over 15 years
No documented case of procedure-related perinatal loss in the large trials
And few in the literature overall
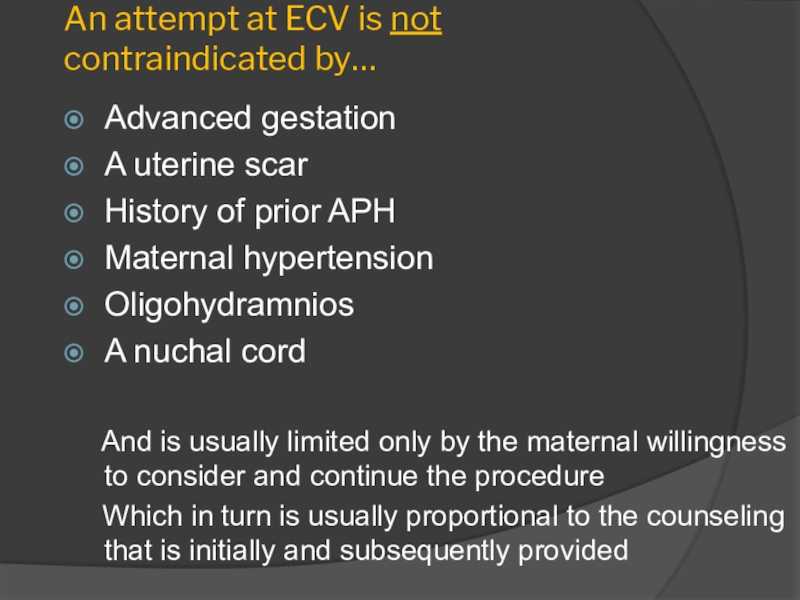
Слайд 23An attempt at ECV is not contraindicated by…
Advanced gestation
A uterine
scar
History of prior APH
Maternal hypertension
Oligohydramnios
A nuchal cord
And is
usually limited only by the maternal willingness to consider and continue the procedureWhich in turn is usually proportional to the counseling that is initially and subsequently provided
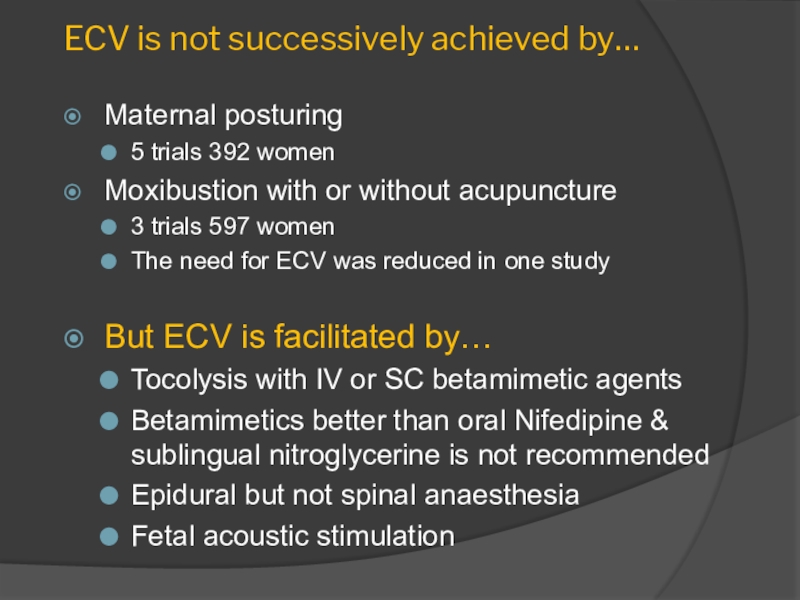
Слайд 24ECV is not successively achieved by…
Maternal posturing
5 trials 392 women
Moxibustion
with or without acupuncture
3 trials 597 women
The need for
ECV was reduced in one studyBut ECV is facilitated by…
Tocolysis with IV or SC betamimetic agents
Betamimetics better than oral Nifedipine & sublingual nitroglycerine is not recommended
Epidural but not spinal anaesthesia
Fetal acoustic stimulation
Слайд 25Unanswered Questions about ECV
When it should be attempted
Beginning earlier at
34 – 36w may be okay
Should attempts be repeated
How many
timesHow often
Role in the fetus who has an unstable lie
Role with amnioreduction and amnioinfusion
Teaching and maintaining skills
Слайд 26The Early ECV Trial
1543 ♀ in 21 countries randomised to:
ECV
at 34 – 36 weeks or
>37 weeks
Fewer breeches at term
from early ECVRR 0.84 CI 0.75 – 0.94 (41% vs 48%)
But rate of Caesarean not reduced
Inexplicable
Early ECV appears safe
No difference in fetal/neonatal morbidity
But a meta analysis suggests increased risk of preterm labour
Discuss benefits and risks and choose