Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Bronchiectases : lecture
Содержание
- 1. Bronchiectases : lecture
- 2. DefinitionBronchiectasis - uncommon disease, most often secondary
- 3. ERS guidelines for the management of adult
- 4. Classification by etiology1. Genetic disorders (cystic fibrosis,
- 5. Classification by etiology 29% idiopathic 14% post-infective
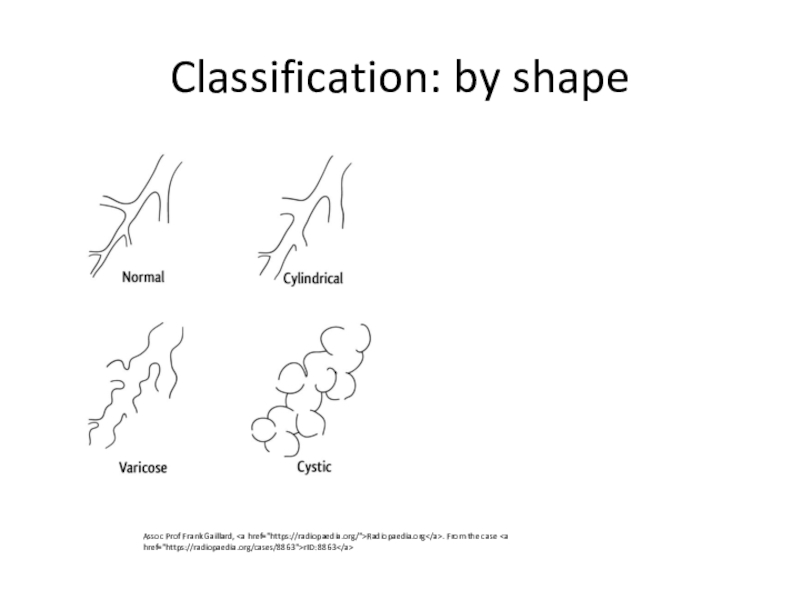
- 6. Classification: by shapeAssoc Prof Frank Gaillard, Radiopaedia.org. From the case rID: 8863
- 7. Classification by shape: Normal bronchus; no bronchoectasesAmerican
- 8. Cylindric bronchiectasis with lack of bronchial taperingAssoc
- 9. varicose bronchiectasis with string-of-pearls appearance Assoc Prof
- 10. cystic bronchiectasisAmerican Journal of Roentgenology > Volume 193,
- 11. Classification: etiology and locationFocal (congenital bronchial atresia,
- 12. Figure 1 The Lancet 2018 392, 880-890DOI: (10.1016/S0140-6736(18)31767-7)
- 13. ComponentsNeutrophilic inflammation – destruction of wall by
- 14. Inflammation: neutrophilicNeutrophils recruitment acceleration: degradation of elastins;
- 15. Importance of this mechanism for control the
- 16. Ciliary disfunction: primary and secondaryCilia Dysfunction in
- 17. Genes Encoding Major Components of Airway Motile
- 18. Secondary ciliary disfunctionViruses Bacterial mediators - H. influenzae, P.
- 19. Primary and secondary mucociliary clearance disturbance leads
- 20. Primary anatomical changes, promoting clearance disorders due
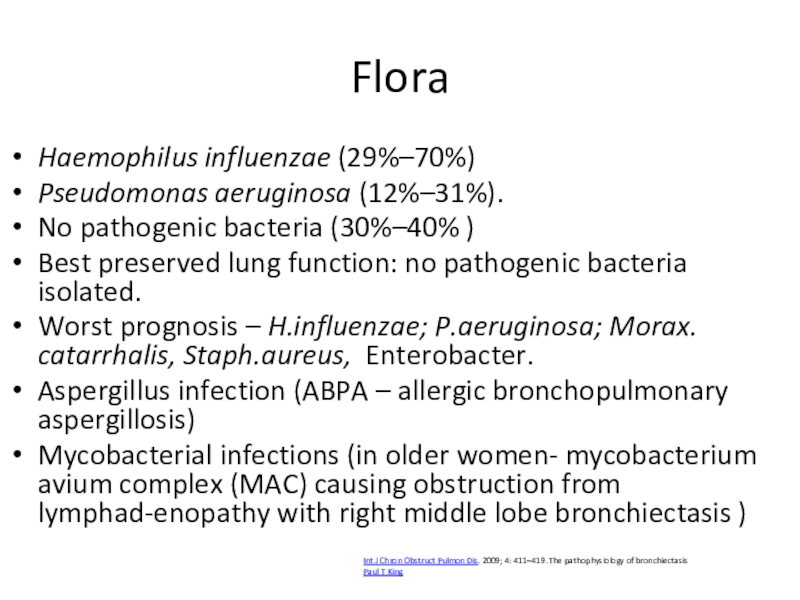
- 21. FloraHaemophilus influenzae (29%–70%) Pseudomonas aeruginosa (12%–31%). No pathogenic bacteria
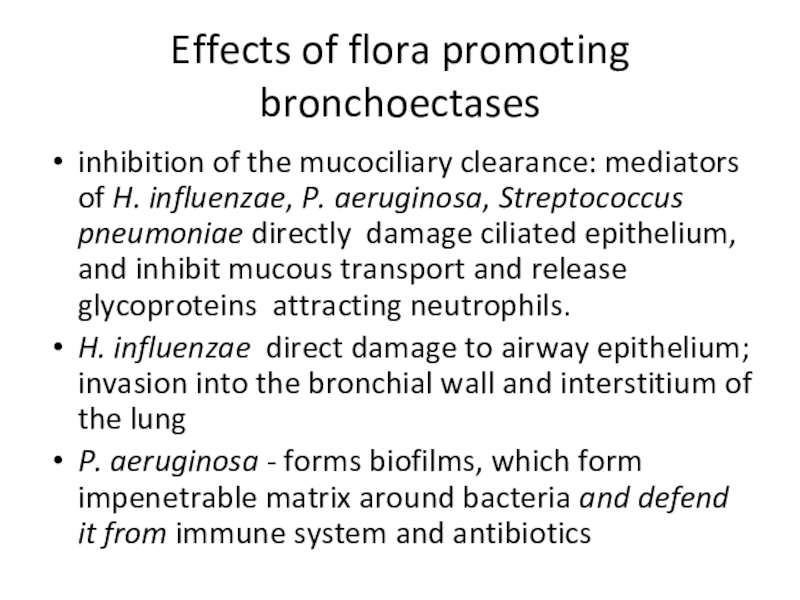
- 22. Effects of flora promoting bronchoectasesinhibition of the
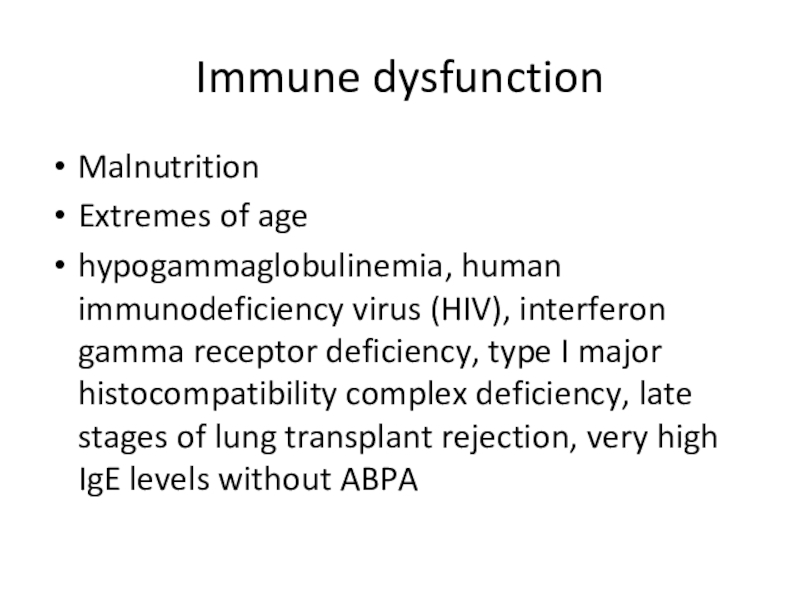
- 23. Immune dysfunctionMalnutritionExtremes of age hypogammaglobulinemia, human immunodeficiency
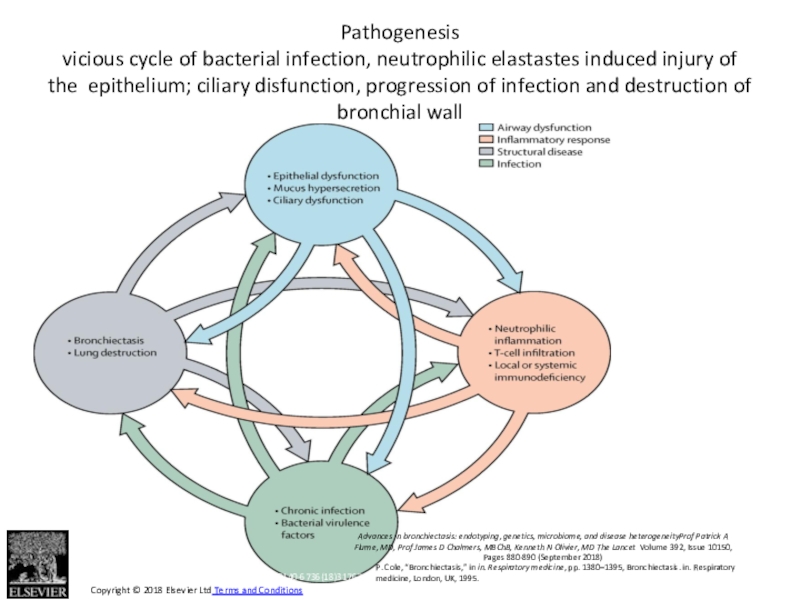
- 24. Figure 1 The Lancet 2018 392, 880-890DOI: (10.1016/S0140-6736(18)31767-7)
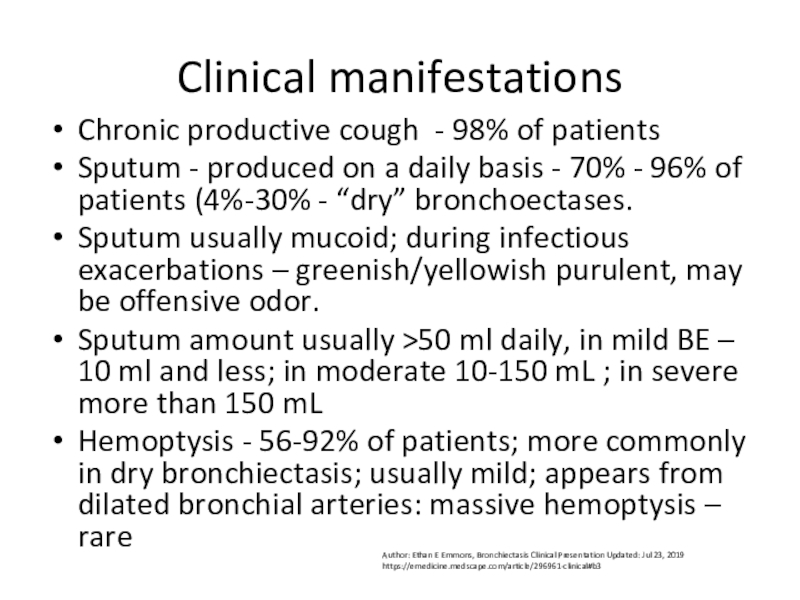
- 25. Clinical manifestations Chronic productive cough - 98%
- 26. Dyspnea – 62%-72% of patients, mixed (obstruction
- 27. In whom should be suspected?Persistent mucopurulent/purulent sputum
- 28. Diagnosis: to confirmbaseline chest X-ray in patients
- 29. CT features of bronchiectasis bronchial dilatation as
- 30. Diagnosis: general + florafull blood count incl
- 31. Diff: COPDBronchiectasesSputum >50 ml, more purulentHemopthisis common
- 32. Diff: cancerBronchiectasesSputum >50 ml, more purulentHemopthisis common
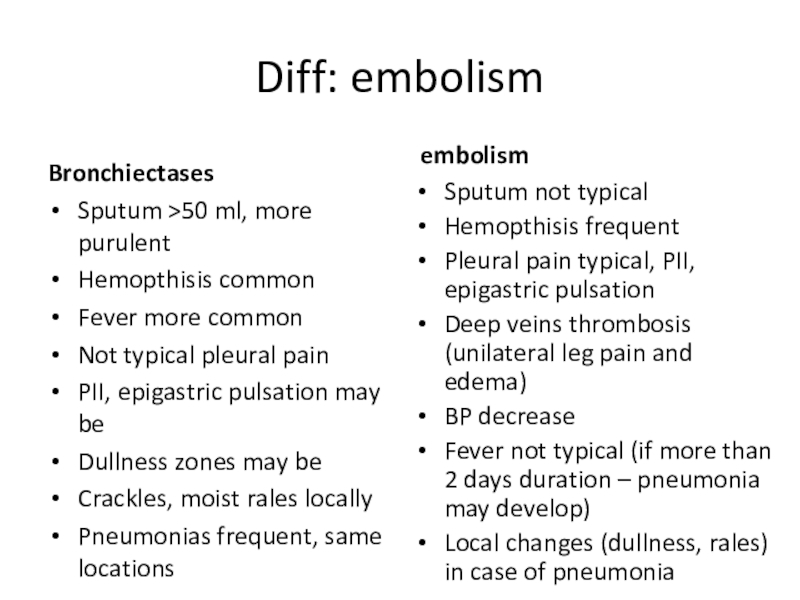
- 33. Diff: embolismBronchiectasesSputum >50 ml, more purulentHemopthisis common
- 34. Rare syndroms (ciliary disfunction, cystic fibrosis)Cystic fibrosisFetal
- 35. Cystic fibrosispredominance of cystic bronchiectasis (arrows) volume loss (fibrosis) diffuse heterogeneous attenuationenlarged lung volumes (obstruction)
- 36. Adult cystic fibrosis (milder case)cylindric bronchiectasis (white
- 37. Kartagener's syndromeDextrocardia (here + cardiomegaly) Here -
- 38. Other endotypesAlpha -1 antitripsin deficiencyPanacinar basal emphysema
- 39. SarcoidosisDiffuse fibrosis traction bronchiectasis (arrows, B) predominantly upper
- 40. Usual interstitial pneumonia (idiopathic pulmonary fibrosis; rheumatoid
- 41. Scleroderma and other connective tissue diseases –
- 42. Bronchiolitis obliterans after lung transplantation. Transverse images
- 43. Other endotypesABPABlood eosinophiliathick sputum with black Bronchial
- 44. Allergic bronchopulmonary aspergillosisAsthmaPresence of transient pulmonary infiltrates
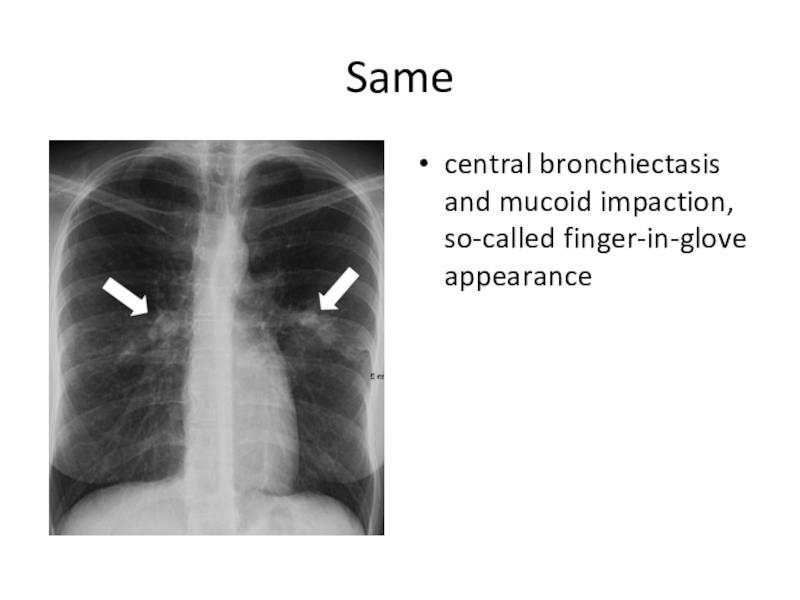
- 45. Same central bronchiectasis and mucoid impaction, so-called finger-in-glove appearance
- 46. Other investigations: endotypes assessment Co-morbidities and past
- 47. Tests for: cystic fibrosis - early onset,
- 48. Other investigationsSpirogram/functional investigation of lungs, oxygen saturation,
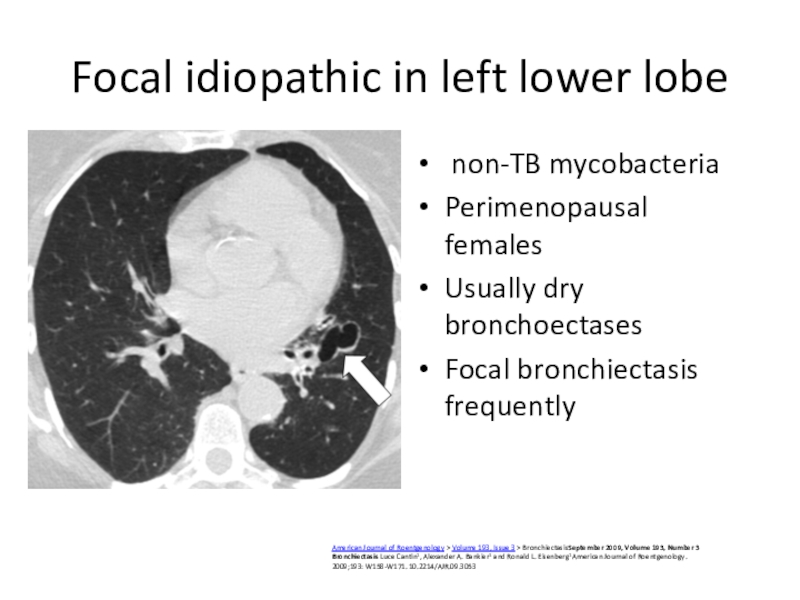
- 49. Focal idiopathic in left lower lobe non-TB mycobacteriaPerimenopausal
- 50. subtle idiopathic bibasilar cylindric bronchiectasis shows signet-ring
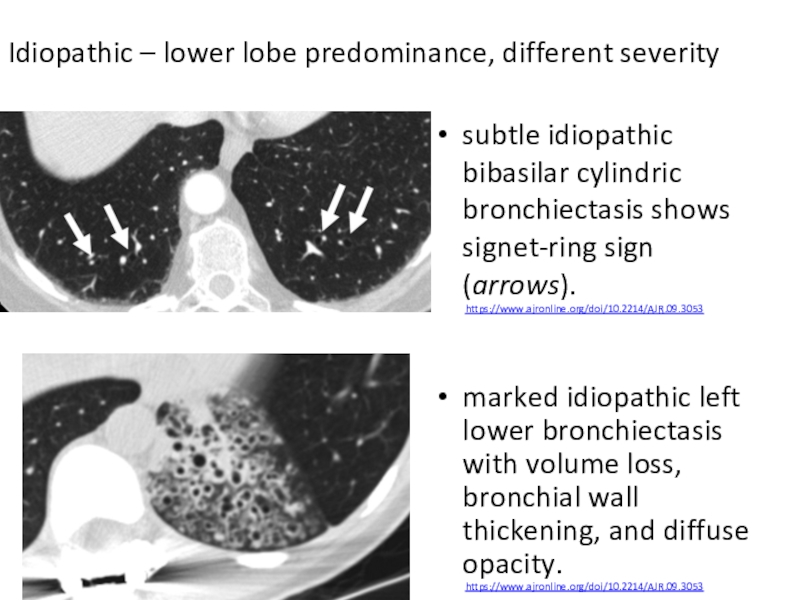
- 51. Mycobacterium avium- intracellulare infectionBronchiectasis (arrows) predominantly involves right
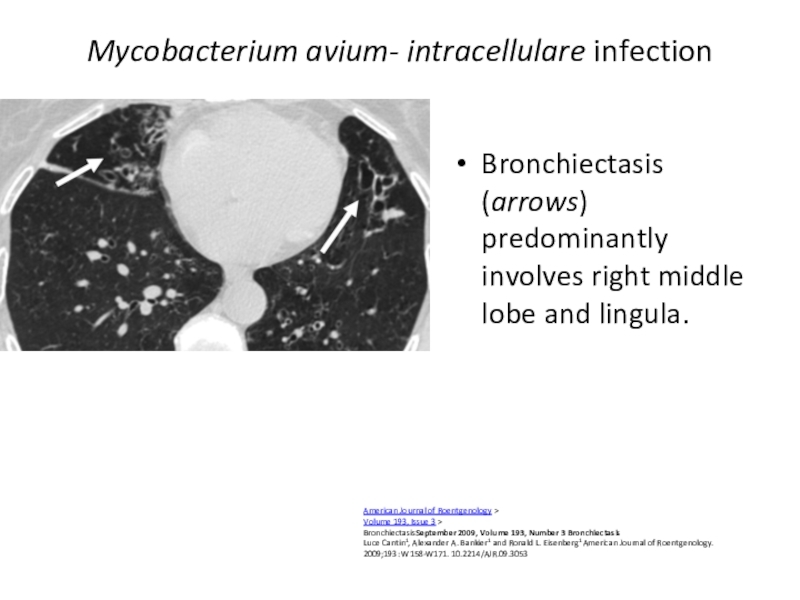
- 52. Obstruction Tumor More gradual onset (1-3 mo)Dyspnea
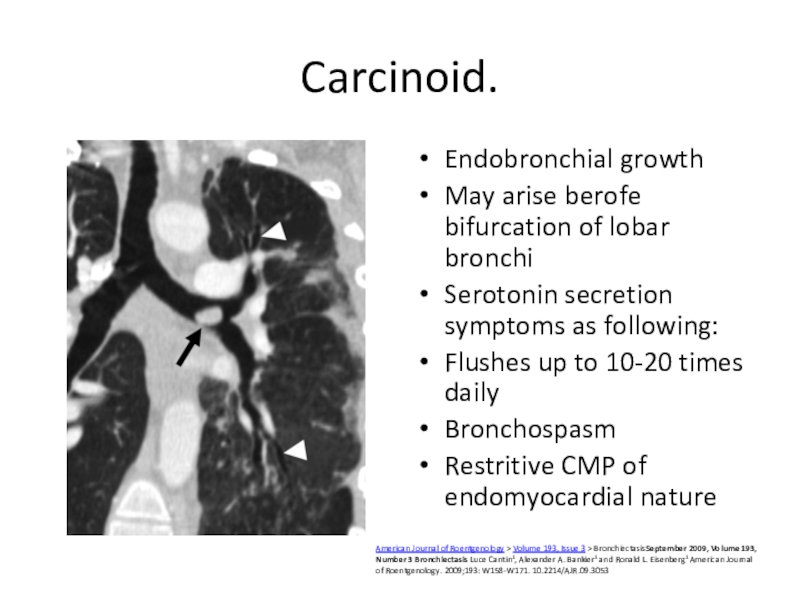
- 53. Carcinoid.Endobronchial growth May arise berofe bifurcation of
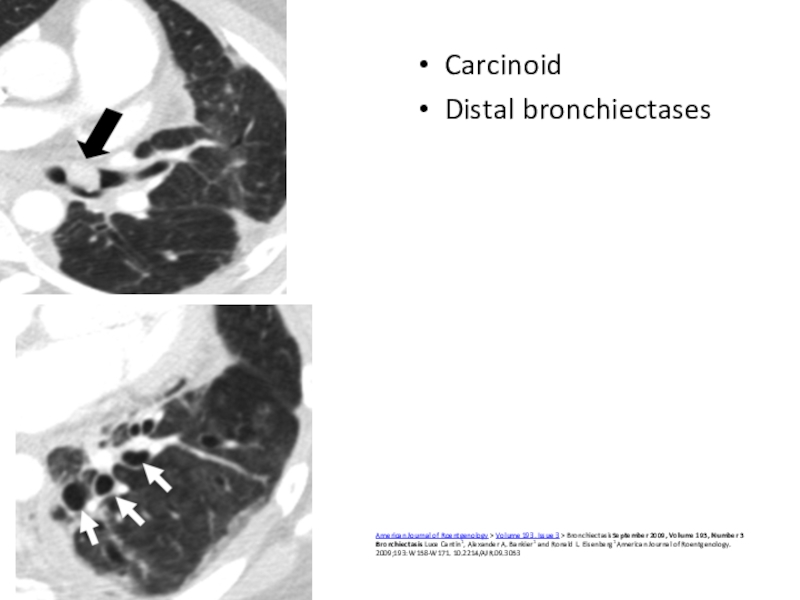
- 54. CarcinoidDistal bronchiectases American Journal of Roentgenology > Volume
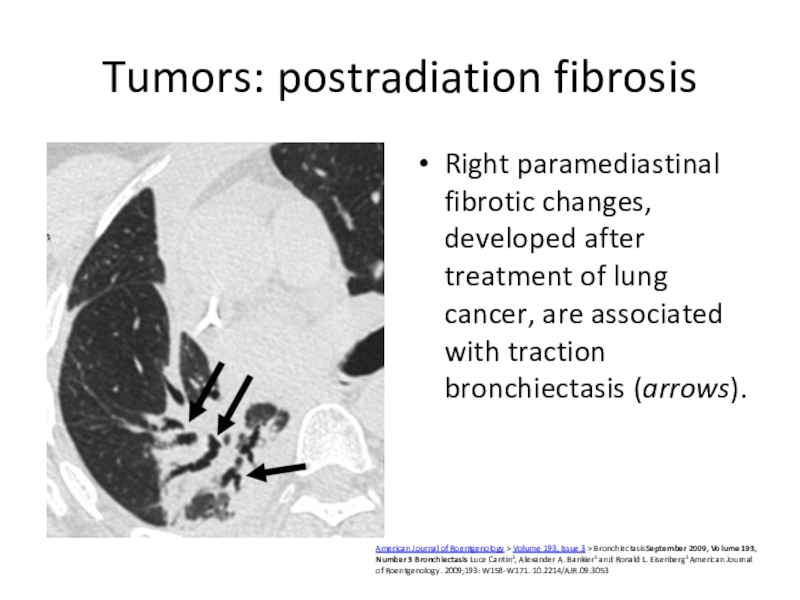
- 55. Tumors: postradiation fibrosisRight paramediastinal fibrotic changes, developed
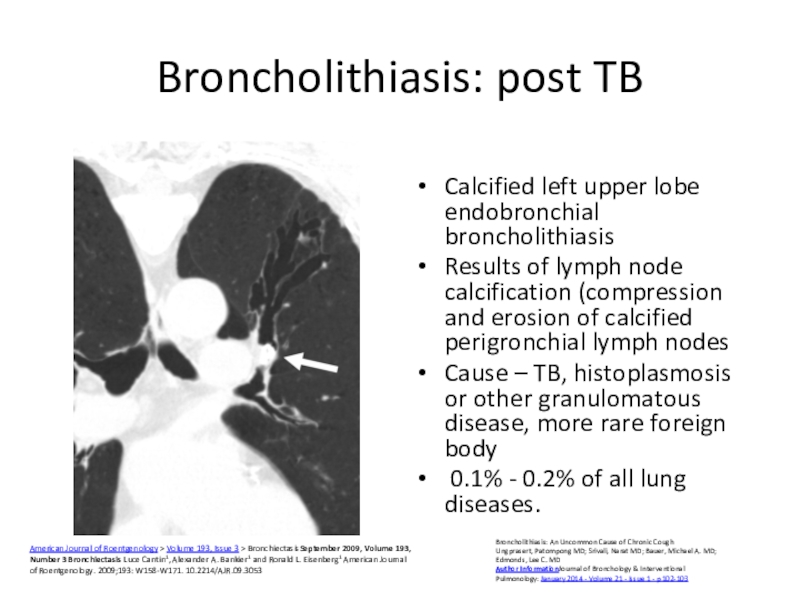
- 56. Broncholithiasis: post TBCalcified left upper lobe endobronchial
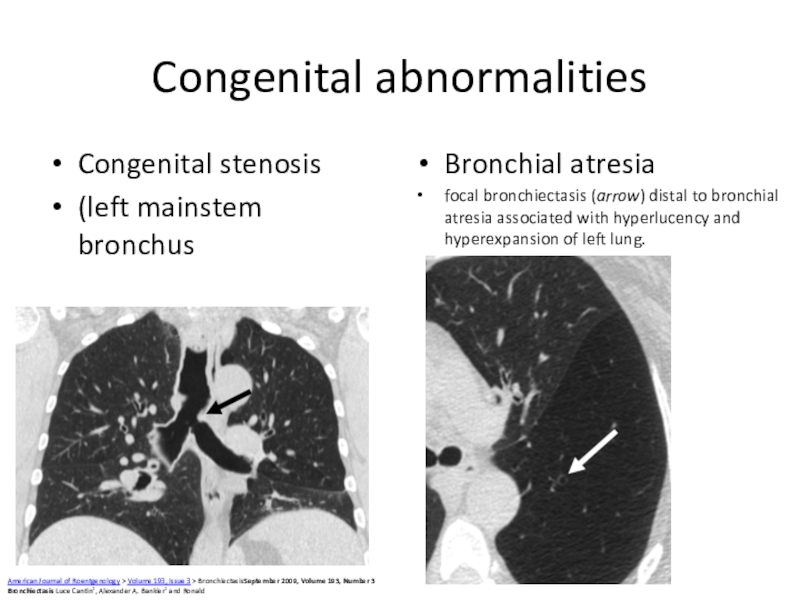
- 57. Congenital abnormalitiesCongenital stenosis(left mainstem bronchusBronchial atresia focal
- 58. Other causesMounier-Kuhn's syndrome. Enlarged trachea (arrow).Enlarged mainstem
- 59. Williams-Campbellmostly varicose and cystic central bronchiectasis (arrows).American
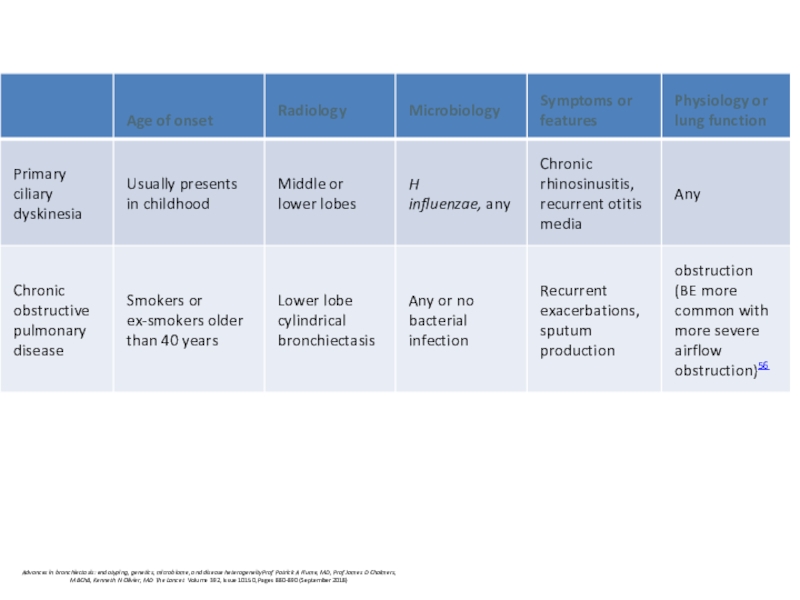
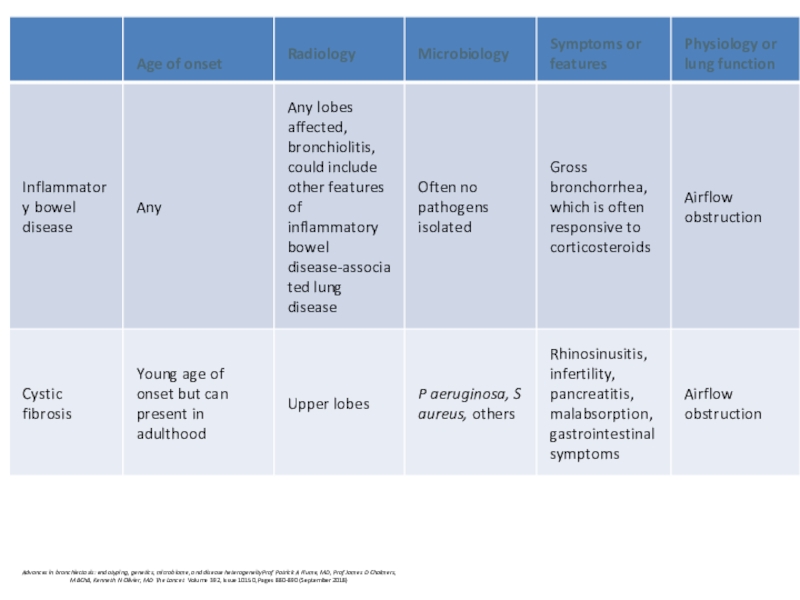
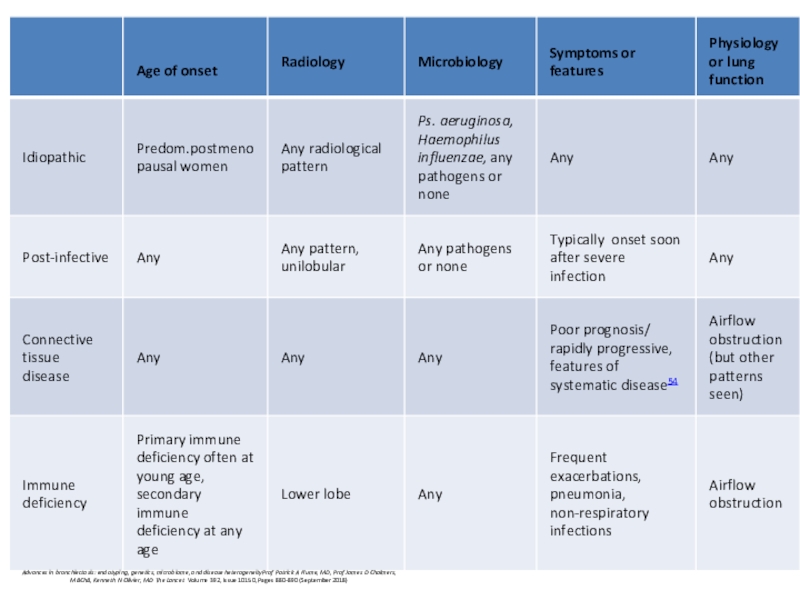
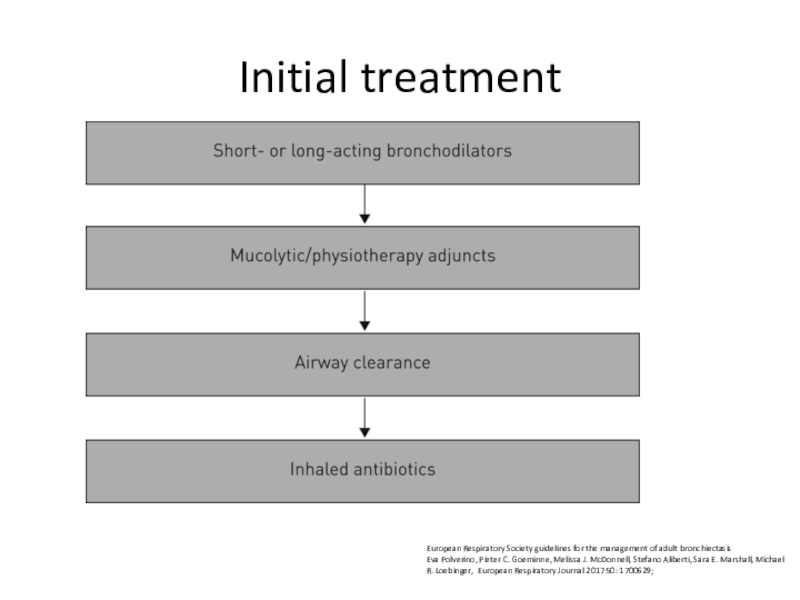
- 60. Advances in bronchiectasis: endotyping, genetics, microbiome, and
- 61. Advances in bronchiectasis: endotyping, genetics, microbiome, and
- 62. Cystic fibrosisCystic fibrosis (CF) is an autosomal
- 63. Pathogenesis: hypothesischemical shield’ hypothesis: in normal condition airway epithelium produces low salt (
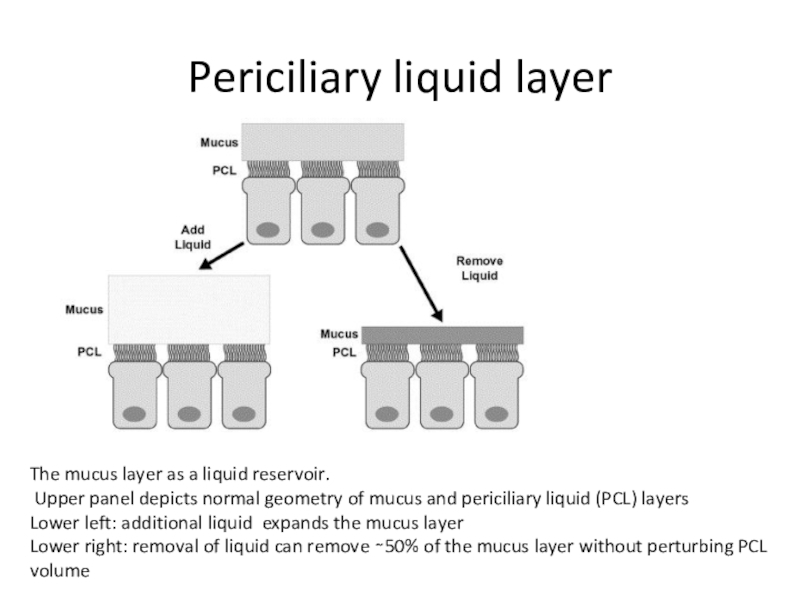
- 64. Periciliary liquid layer The mucus layer as
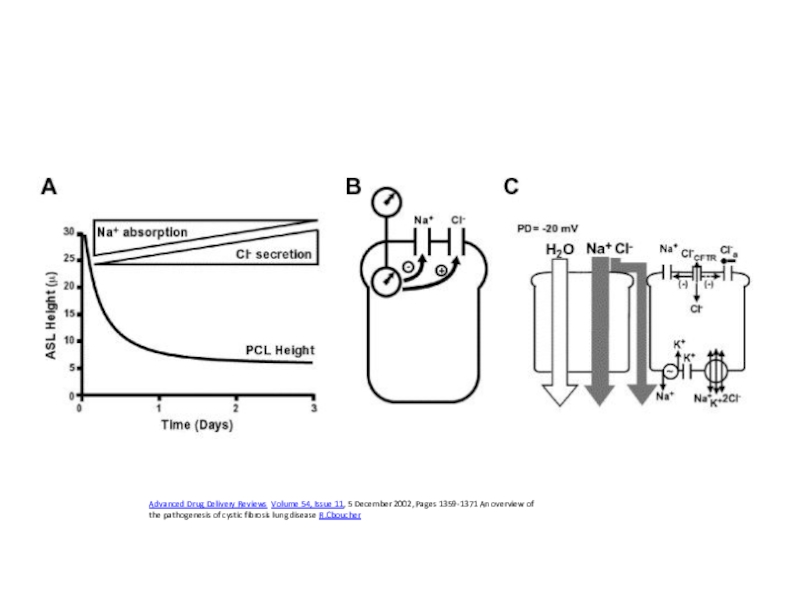
- 65. Advanced Drug Delivery Reviews Volume 54, Issue
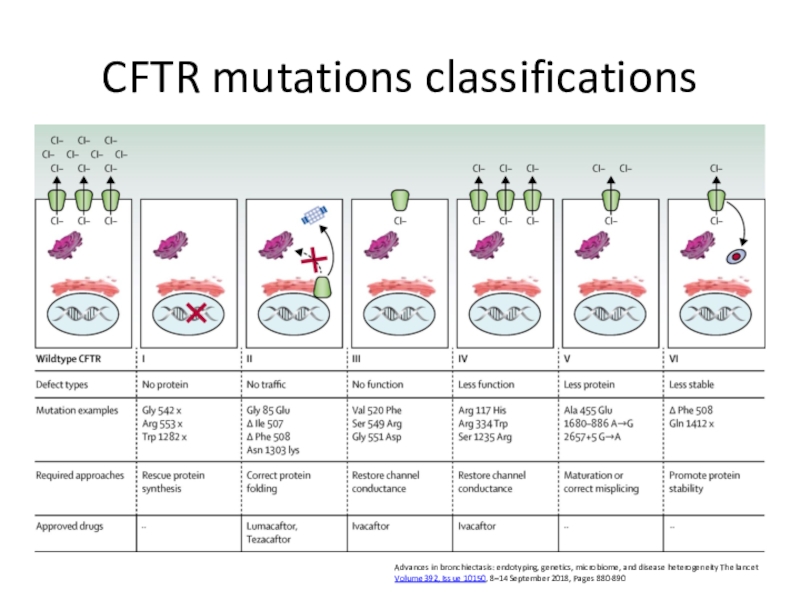
- 66. CFTR mutations classificationsAdvances in bronchiectasis: endotyping, genetics,
- 67. Median age at diagnosis- 6-8 months; two
- 68. Primary ciliary dyskinesia multiple genes
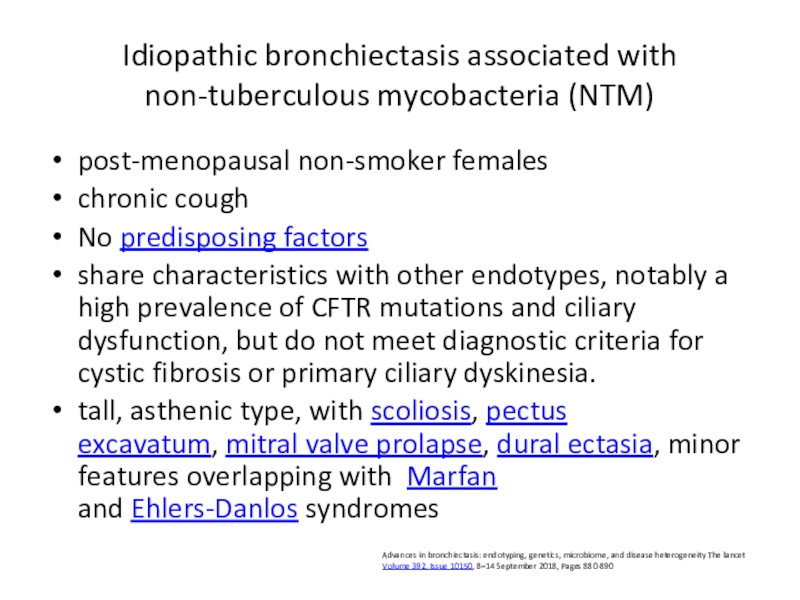
- 69. Idiopathic bronchiectasis associated with non-tuberculous mycobacteria (NTM)post-menopausal
- 70. Advances in bronchiectasis: endotyping, genetics, microbiome, and
- 71. Advances in bronchiectasis: endotyping, genetics, microbiome, and
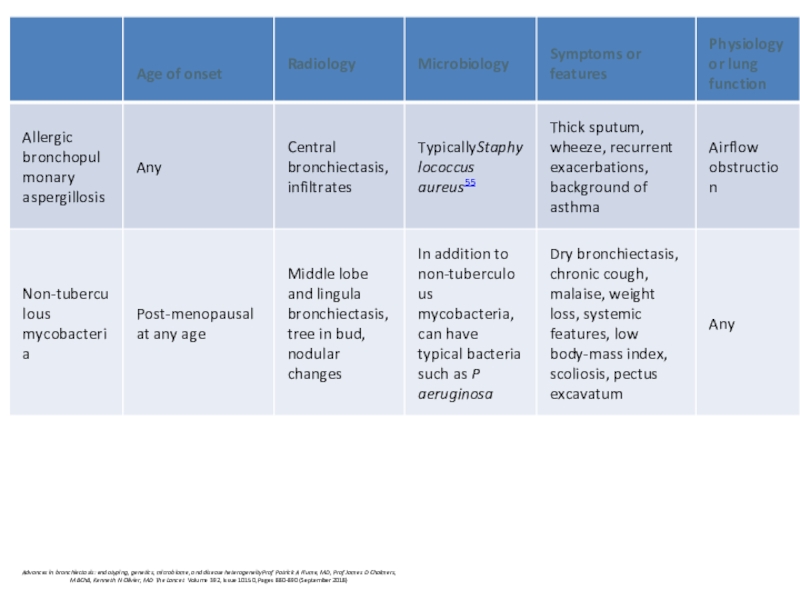
- 72. T Hill A, L Sullivan A, D Chalmers J, et alBritish Thoracic Society Guideline for bronchiectasis in adultsThorax 2019;74:1-69.
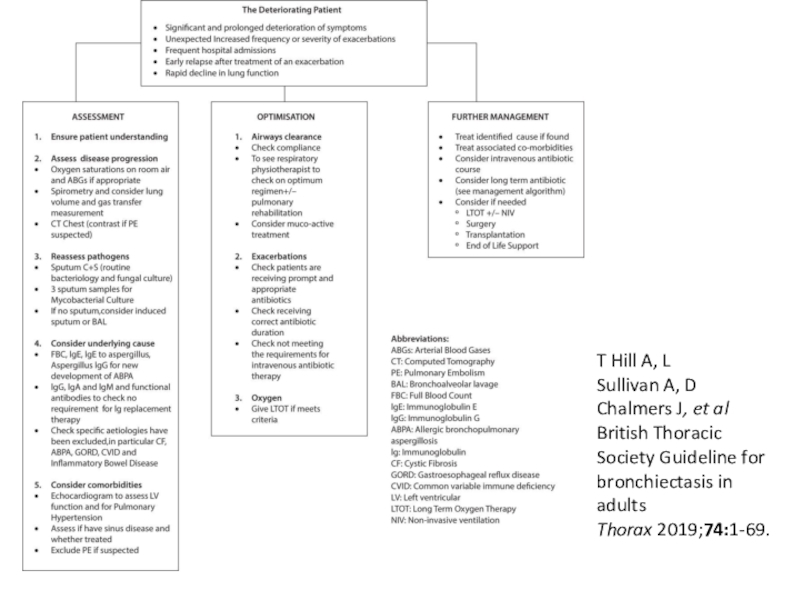
- 73. Initial treatmentEuropean Respiratory Society guidelines for the
- 74. Offer annual influenza immunisation to all patients
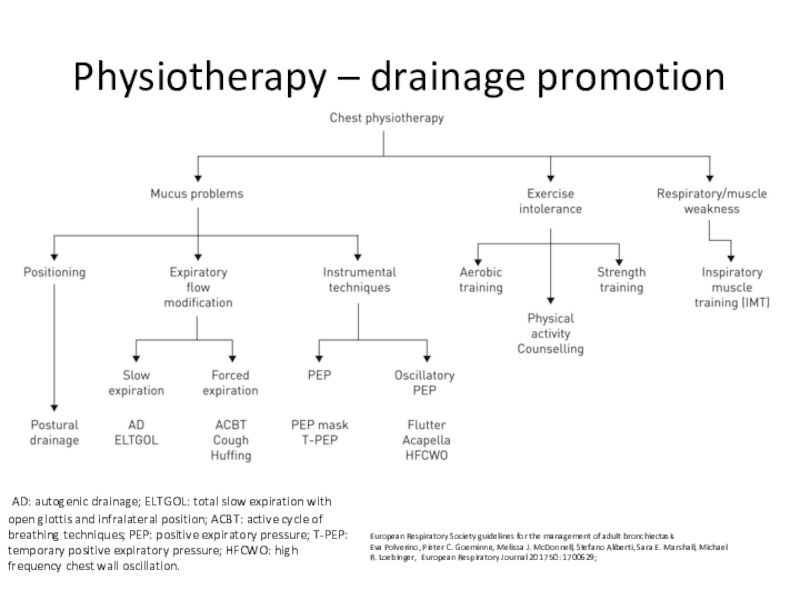
- 75. Physiotherapy – drainage promotion AD: autogenic drainage;
- 76. Airway clearance techniquesshould be taught by a
- 77. Consider autogenic drainage, positive expiratory pressure, high
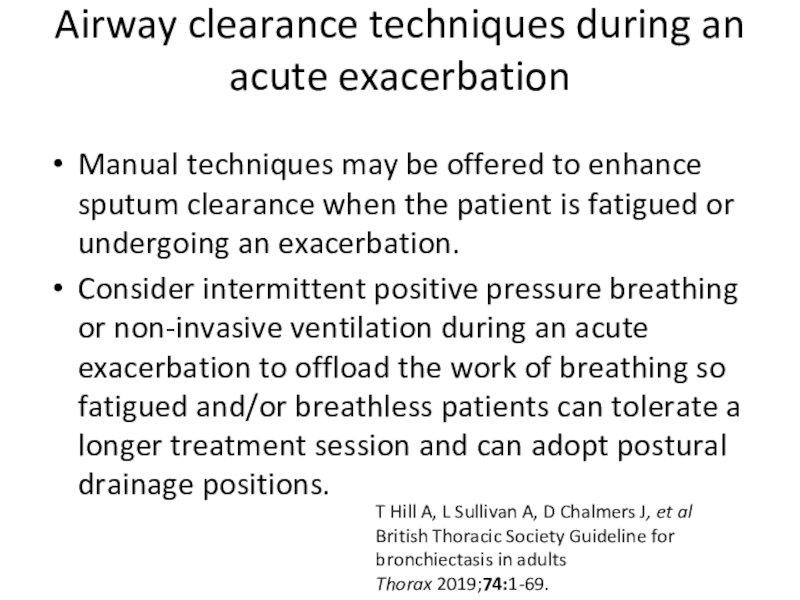
- 78. Airway clearance techniques during an acute exacerbation
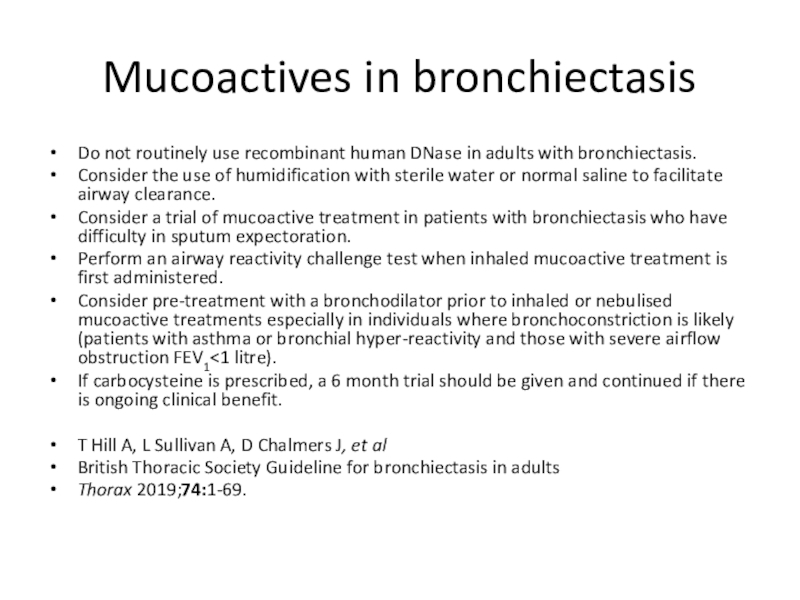
- 79. Mucoactives in bronchiectasisDo not routinely use recombinant
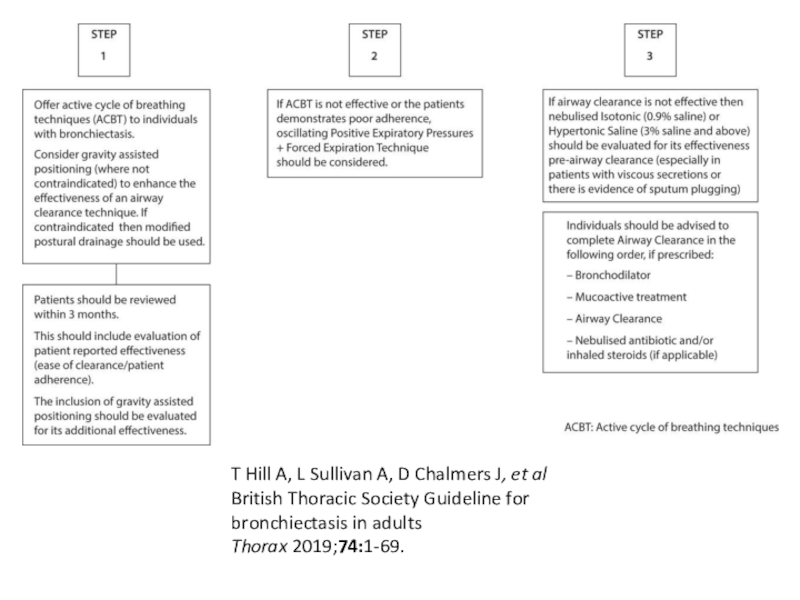
- 80. T Hill A, L Sullivan A, D Chalmers J, et alBritish Thoracic Society Guideline for bronchiectasis in adultsThorax 2019;74:1-69.
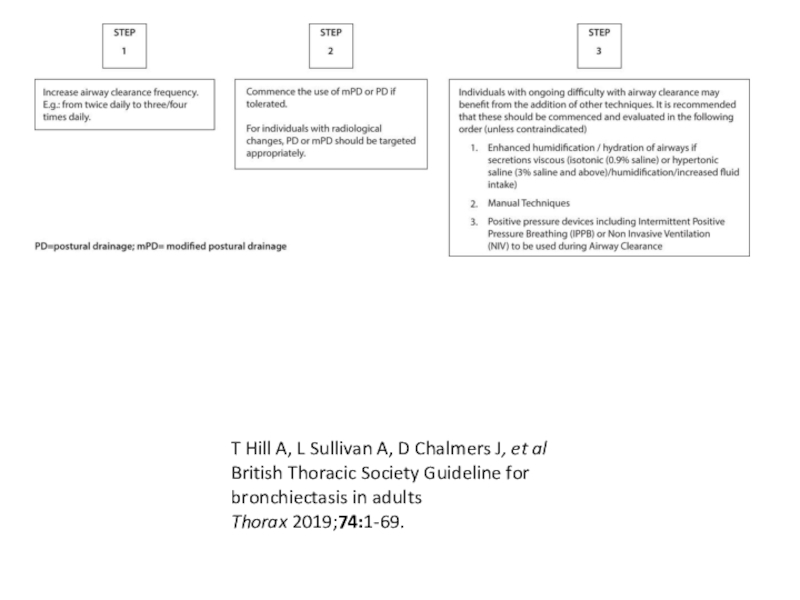
- 81. T Hill A, L Sullivan A, D Chalmers J, et alBritish Thoracic Society Guideline for bronchiectasis in adultsThorax 2019;74:1-69.
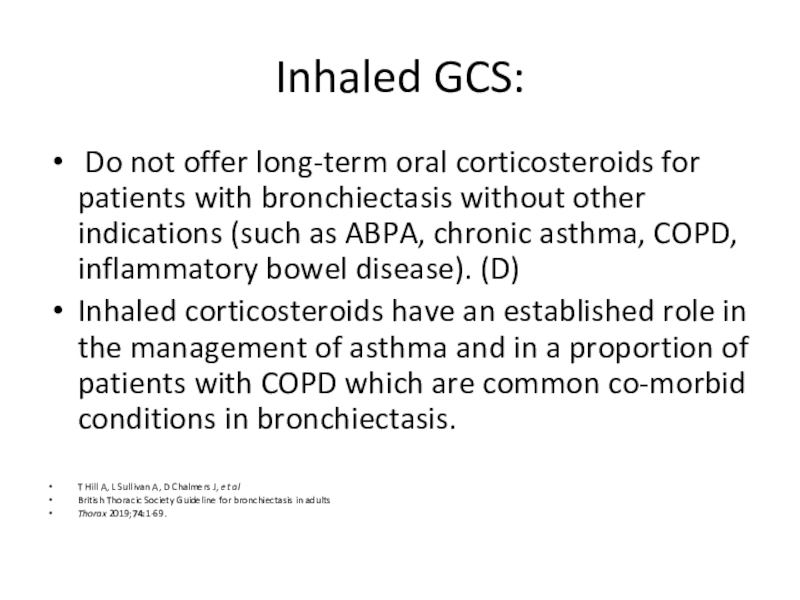
- 82. Inhaled GCS: Do not offer long-term oral
- 83. PDE inhibitors, CXCR2 antagonists, statins etcDo not
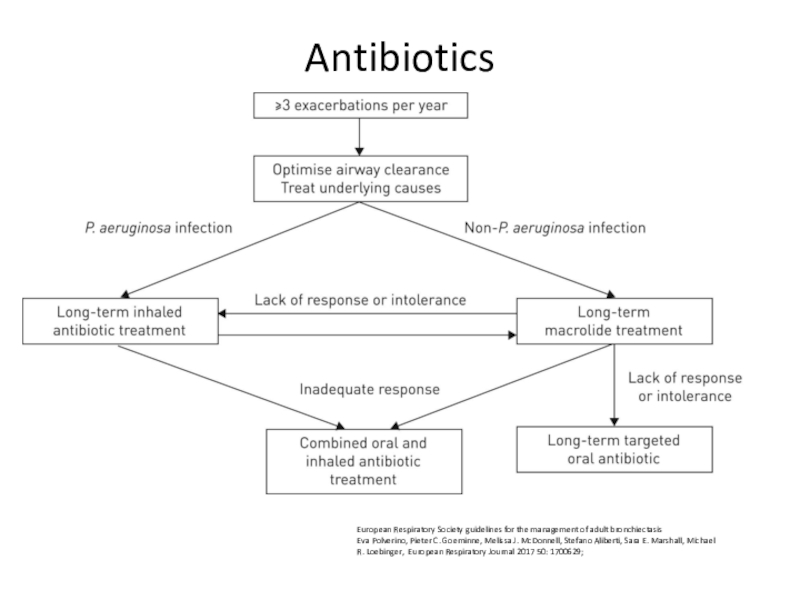
- 84. AntibioticsEuropean Respiratory Society guidelines for the management
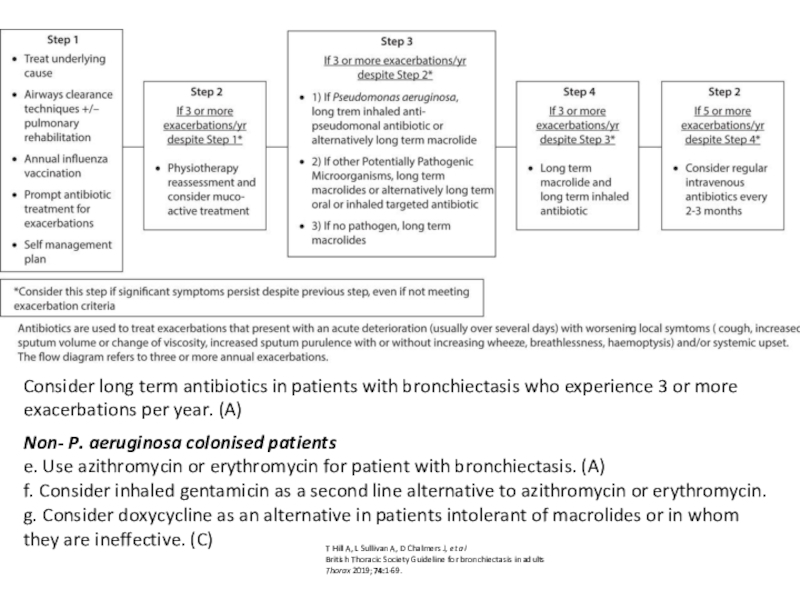
- 85. Consider long term antibiotics in patients with
- 86. SafetyPrior to starting long term macrolides, for
- 87. Ps.aeruginosaEuropean Respiratory Society guidelines for the management
- 88. Offer patients with bronchiectasis associated with clinical
- 89. Offer patients with bronchiectasis associated with clinical
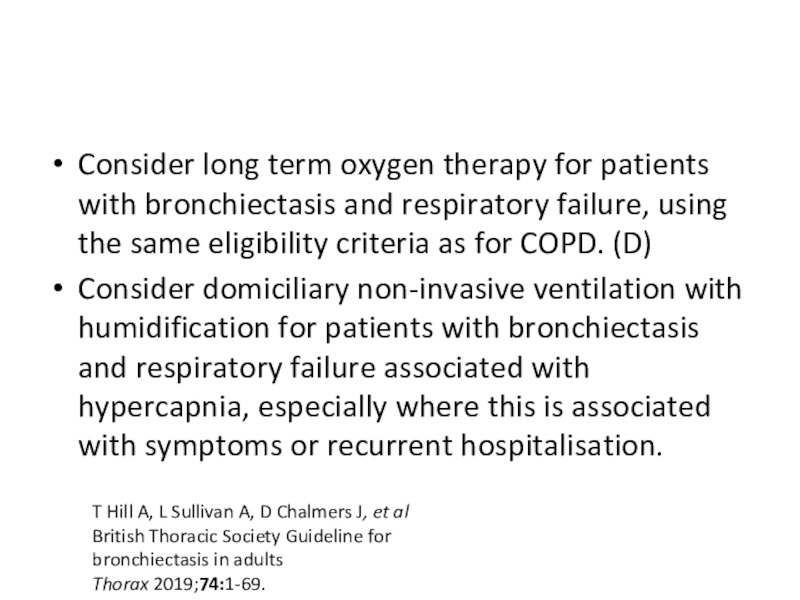
- 90. Consider long term oxygen therapy for patients
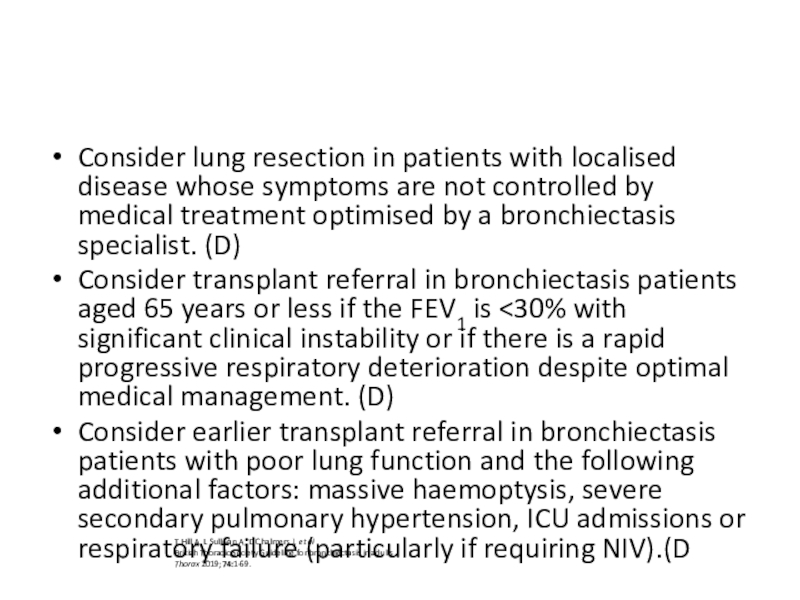
- 91. Consider lung resection in patients with localised
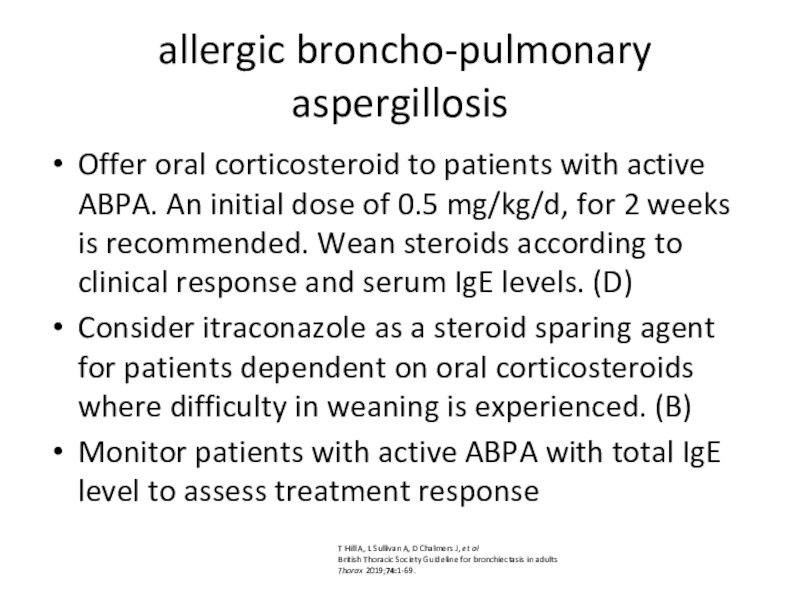
- 92. allergic broncho-pulmonary aspergillosisOffer oral corticosteroid to patients
- 93. Скачать презентанцию
Слайды и текст этой презентации
Слайд 3ERS guidelines for the management of adult bronchiectasis (Eva Polverino, Pieter C. Goeminne, Melissa
J. European Respiratory Society European Respiratory Journal 2017):
Bronchiectasis is
chronic respiratory disease
characterised by a clinical syndrome of cough, sputum production and bronchial infection
and radiologically by abnormal and permanent dilatation of the bronchi.
The objectives of treatment in bronchiectasis are to prevent exacerbations, reduce symptoms, improve quality of life and stop disease progression.
Cough and sputum production, along with breathlessness are the most frequent symptoms but rhinosinusitis, fatigue, haemoptysis and thoracic pain are also common
Слайд 4Classification by etiology
1. Genetic disorders (cystic fibrosis, primary ciliary dyskinesia,
alpha1-antitrypsin deficiency)
2. Post infectious disease (bacteria, virus, fungi, other)
3. Immunodeficiency (congenital, acquired)
4. Aspiration (gastro-oesophageal reflux, swallowing dysfunction, tracheo-esophageal fistula)
5. Congenital structural malformations (lobar emphysema, bronchomalacia, etc.)
6. Mechanical factors (foreign body, extrinsic compression, endobronchial lesions)
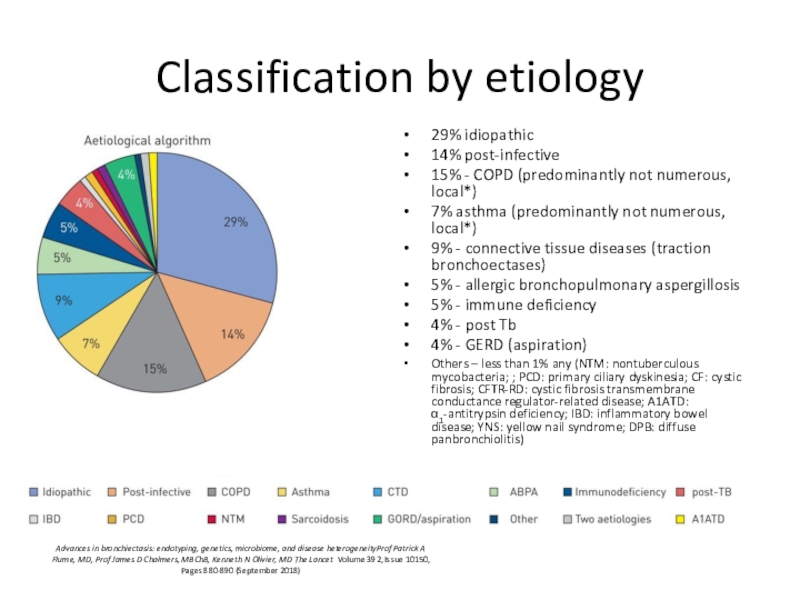
Слайд 5Classification by etiology
29% idiopathic
14% post-infective
15% - COPD
(predominantly not numerous, local*)
7% asthma (predominantly not numerous, local*)
9% -
connective tissue diseases (traction bronchoectases)5% - allergic bronchopulmonary aspergillosis
5% - immune deficiency
4% - post Tb
4% - GERD (aspiration)
Others – less than 1% any (NTM: nontuberculous mycobacteria; ; PCD: primary ciliary dyskinesia; CF: cystic fibrosis; CFTR-RD: cystic fibrosis transmembrane conductance regulator-related disease; A1ATD: α1-antitrypsin deficiency; IBD: inflammatory bowel disease; YNS: yellow nail syndrome; DPB: diffuse panbronchiolitis)
Advances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneityProf Patrick A Flume, MD, Prof James D Chalmers, MBChB, Kenneth N Olivier, MD The Lancet Volume 392, Issue 10150, Pages 880-890 (September 2018)
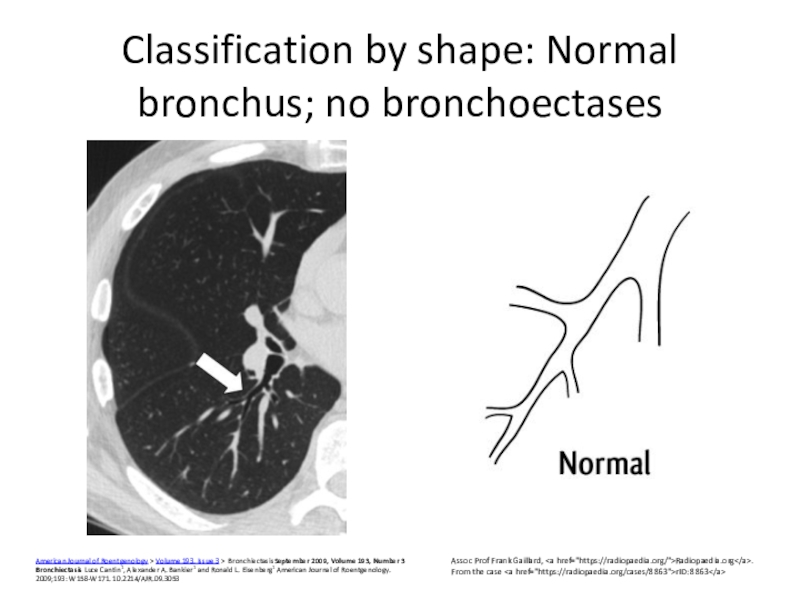
Слайд 7Classification by shape: Normal bronchus; no bronchoectases
American Journal of Roentgenology >
Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number 3
Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053Assoc Prof Frank Gaillard, Radiopaedia.org. From the case rID: 8863
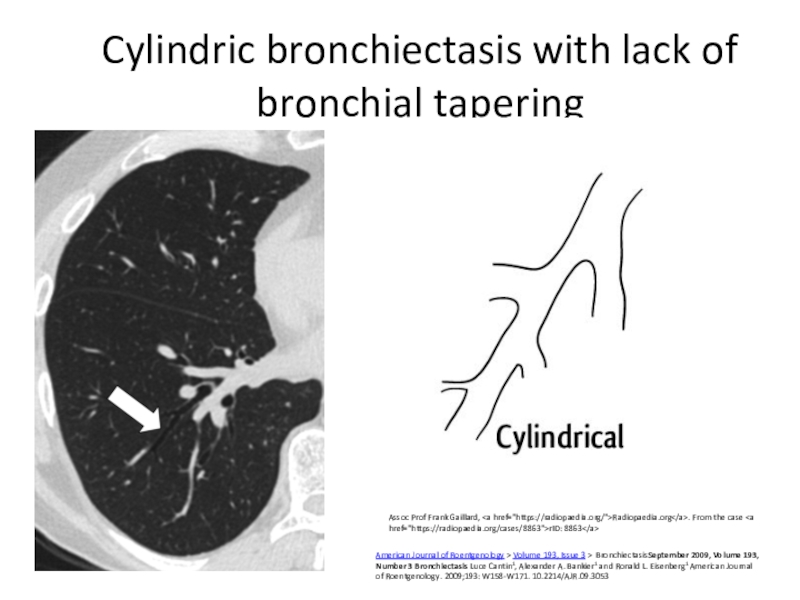
Слайд 8Cylindric bronchiectasis with lack of bronchial tapering
Assoc Prof Frank Gaillard,
Radiopaedia.org. From the case rID: 8863
American Journal of
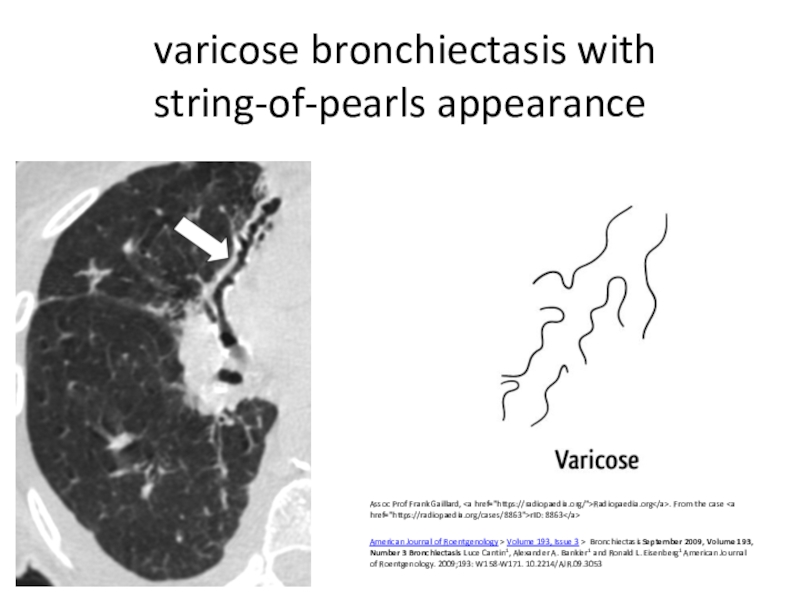
Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053 Слайд 9 varicose bronchiectasis with string-of-pearls appearance
Assoc Prof Frank Gaillard,
href="https://radiopaedia.org/">Radiopaedia.org. From the case rID: 8863
American Journal of Roentgenology >
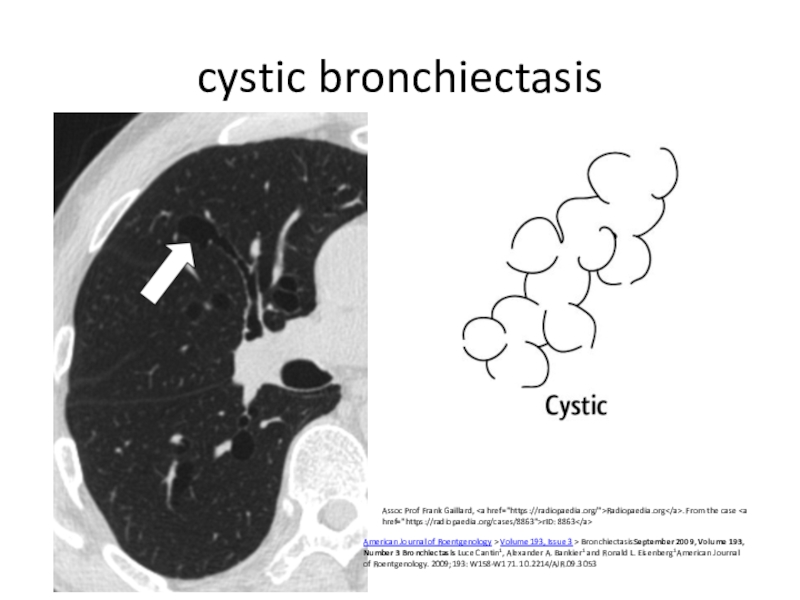
Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053 Слайд 10cystic bronchiectasis
American Journal of Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember
2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald
L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053Assoc Prof Frank Gaillard, Radiopaedia.org. From the case rID: 8863
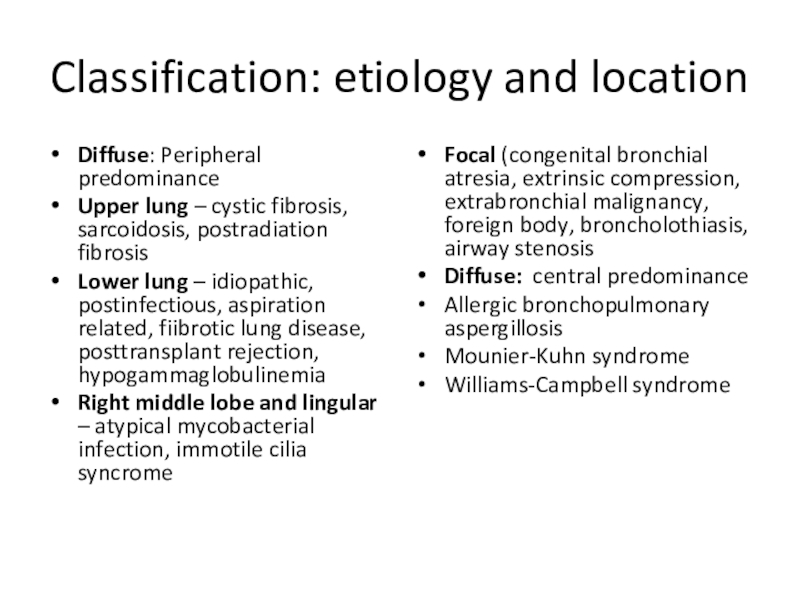
Слайд 11Classification: etiology and location
Focal (congenital bronchial atresia, extrinsic compression, extrabronchial
malignancy, foreign body, broncholothiasis, airway stenosis
Diffuse: central predominance
Allergic bronchopulmonary aspergillosis
Mounier-Kuhn
syndromeWilliams-Campbell syndrome
Diffuse: Peripheral predominance
Upper lung – cystic fibrosis, sarcoidosis, postradiation fibrosis
Lower lung – idiopathic, postinfectious, aspiration related, fiibrotic lung disease, posttransplant rejection, hypogammaglobulinemia
Right middle lobe and lingular – atypical mycobacterial infection, immotile cilia syncrome
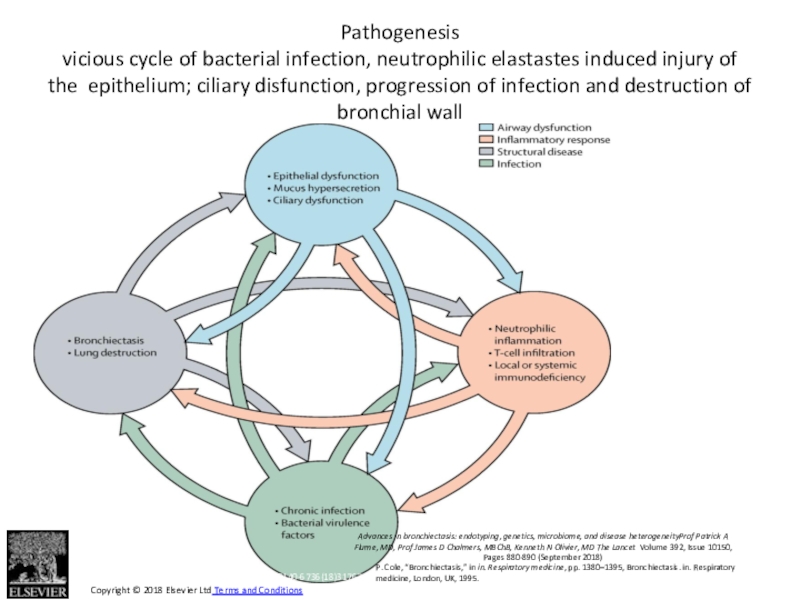
Слайд 12Figure 1
The Lancet 2018 392, 880-890DOI: (10.1016/S0140-6736(18)31767-7)
Copyright © 2018
Elsevier Ltd Terms and Conditions
Advances in bronchiectasis: endotyping, genetics, microbiome,
and disease heterogeneityProf Patrick A Flume, MD, Prof James D Chalmers, MBChB, Kenneth N Olivier, MD The Lancet Volume 392, Issue 10150, Pages 880-890 (September 2018)Pathogenesis
vicious cycle of bacterial infection, neutrophilic elastastes induced injury of the epithelium; ciliary disfunction, progression of infection and destruction of bronchial wall
P. Cole, “Bronchiectasis,” in in. Respiratory medicine, pp. 1380–1395, Bronchiectasis. in. Respiratory medicine, London, UK, 1995.
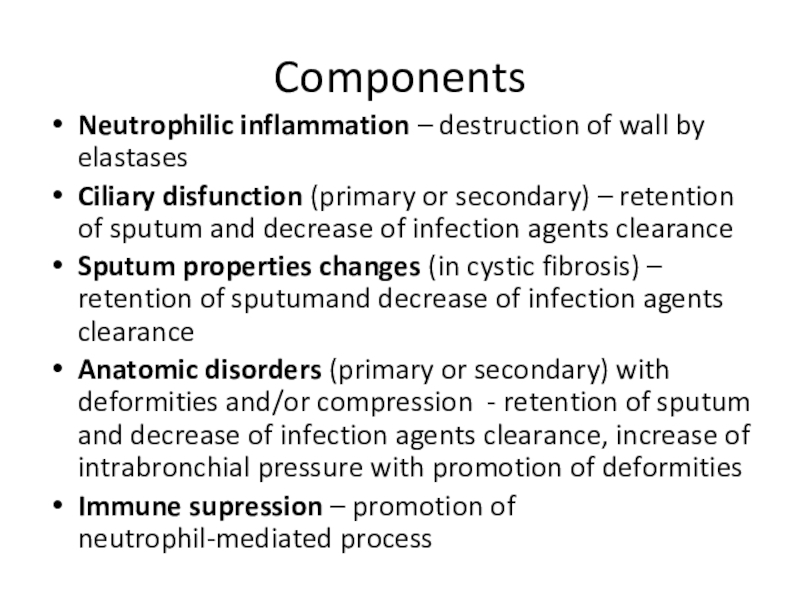
Слайд 13Components
Neutrophilic inflammation – destruction of wall by elastases
Ciliary disfunction (primary
or secondary) – retention of sputum and decrease of infection
agents clearanceSputum properties changes (in cystic fibrosis) – retention of sputumand decrease of infection agents clearance
Anatomic disorders (primary or secondary) with deformities and/or compression - retention of sputum and decrease of infection agents clearance, increase of intrabronchial pressure with promotion of deformities
Immune supression – promotion of neutrophil-mediated process
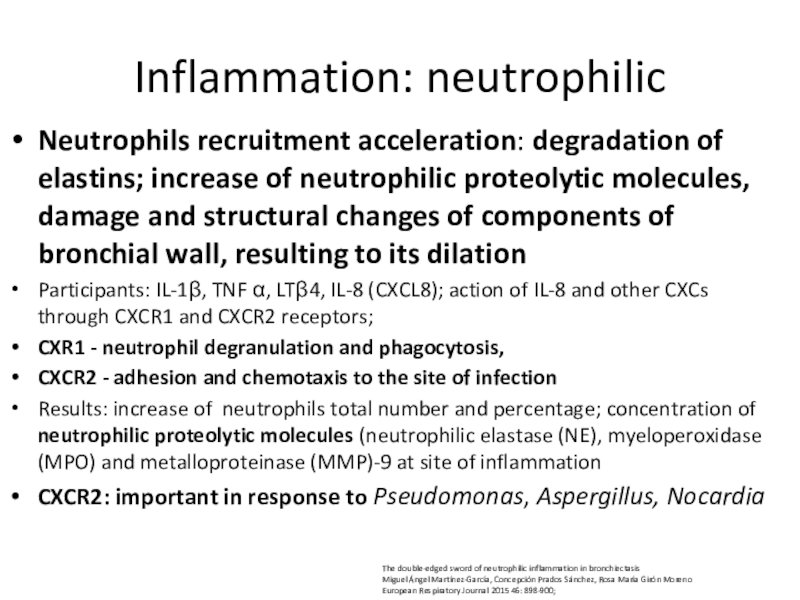
Слайд 14Inflammation: neutrophilic
Neutrophils recruitment acceleration: degradation of elastins; increase of neutrophilic
proteolytic molecules, damage and structural changes of components of bronchial
wall, resulting to its dilationParticipants: IL-1β, TNF α, LTβ4, IL-8 (CXCL8); action of IL-8 and other CXCs through CXCR1 and CXCR2 receptors;
CXR1 - neutrophil degranulation and phagocytosis,
CXCR2 - adhesion and chemotaxis to the site of infection
Results: increase of neutrophils total number and percentage; concentration of neutrophilic proteolytic molecules (neutrophilic elastase (NE), myeloperoxidase (MPO) and metalloproteinase (MMP)-9 at site of inflammation
CXCR2: important in response to Pseudomonas, Aspergillus, Nocardia
The double-edged sword of neutrophilic inflammation in bronchiectasis
Miguel Ángel Martínez-García, Concepción Prados Sánchez, Rosa María Girón Moreno
European Respiratory Journal 2015 46: 898-900;
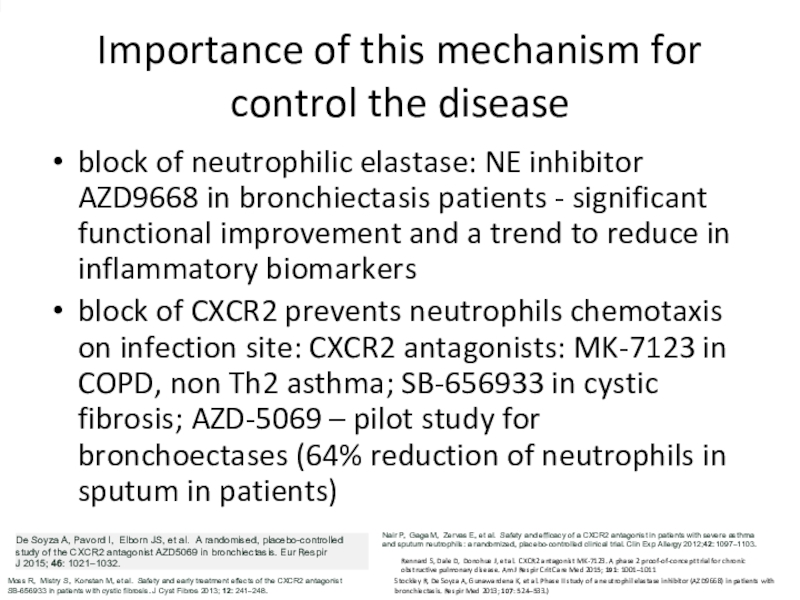
Слайд 15Importance of this mechanism for control the disease
block of neutrophilic
elastase: NE inhibitor AZD9668 in bronchiectasis patients - significant functional
improvement and a trend to reduce in inflammatory biomarkersblock of CXCR2 prevents neutrophils chemotaxis on infection site: CXCR2 antagonists: MK-7123 in COPD, non Th2 asthma; SB-656933 in cystic fibrosis; AZD-5069 – pilot study for bronchoectases (64% reduction of neutrophils in sputum in patients)
Stockley R, De Soyza A, Gunawardena K, et al. Phase II study of a neutrophil elastase inhibitor (AZD9668) in patients with bronchiectasis. Respir Med 2013; 107: 524–533.)
Rennard S, Dale D, Donohue J, et al. CXCR2 antagonist MK-7123. A phase 2 proof-of-concept trial for chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2015; 191: 1001–1011
Nair P, Gaga M, Zervas E, et al. Safety and efficacy of a CXCR2 antagonist in patients with severe asthma and sputum neutrophils: a randomized, placebo-controlled clinical trial. Clin Exp Allergy 2012;42: 1097–1103.
Moss R, Mistry S, Konstan M, et al. Safety and early treatment effects of the CXCR2 antagonist SB-656933 in patients with cystic fibrosis. J Cyst Fibros 2013; 12: 241–248.
De Soyza A, Pavord I, Elborn JS, et al. A randomised, placebo-controlled study of the CXCR2 antagonist AZD5069 in bronchiectasis. Eur Respir J 2015; 46: 1021–1032.
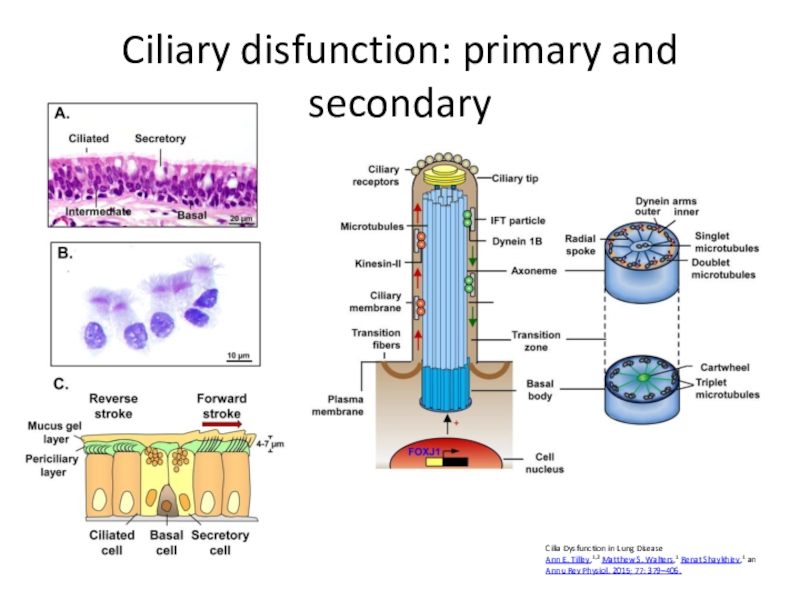
Слайд 16Ciliary disfunction: primary and secondary
Cilia Dysfunction in Lung Disease
Ann E.
Tilley,1,2 Matthew S. Walters,1 Renat Shaykhiev,1 an
Annu Rev Physiol. 2015; 77: 379–406.
Слайд 17Genes Encoding Major Components of Airway Motile Cilia
Axoneme – outer
dynein arm – Dyenin axoneal heavy/intermediate/ light chain genes (DNAH5,
DNAH9, DNAH11, DNAI1, DNAI2, DNAL1)Dynein assembly and docking (Dynein, axonemal, assembly factors 1-3 -DNAAF1-3 etc)
Tubulins and other microtubule-associated (NME/NM23 family member 8NME8 etc)
Receptors, ion channels and signaling molecules (Nitric oxide synthase 3 (endothelial cell)NOS3)
These genes changes predispose do development of primary ciliary dyskinesia
Слайд 18Secondary ciliary disfunction
Viruses
Bacterial mediators - H. influenzae, P. aeruginosa, Streptococcus pneumoniae
(direct damage)
Smoking (direct action on cilia, down-regulation of above
mentioned genes)Слайд 19Primary and secondary mucociliary clearance disturbance leads to
airway dehydration, excess
mucus volume and viscosity.
Increase of sputum content and further infection
development Слайд 20Primary anatomical changes, promoting clearance disorders due to bronchi deformities
or compression
Traction bronchoectases – advanced pulmonary fibrosis with traction of
the airwaysPostTb – advanced fibrotic changes and localized peribronchial lymphadenopathy squeezing bronchi and causing localised bronchial obstruction (particularly in the right middle and upper lobes) with secondary decrease of clearence and infection persistence
Childhood infections - whooping cough, measles, adenovirus – increase pressure in bronchiols during paroxysmal cough, mucus plugs in bronchi
Mycobacterium avium complex (MAC) in elder women cause obstruction from lymphadenopathy with right middle lobe bronchiectasis
Other causes – inborn changes, bronchial and lung dysplasia, endobronchial calcifications, foreign bodies etc
Слайд 21Flora
Haemophilus influenzae (29%–70%)
Pseudomonas aeruginosa (12%–31%).
No pathogenic bacteria (30%–40% )
Best
preserved lung function: no pathogenic bacteria isolated.
Worst prognosis –
H.influenzae; P.aeruginosa; Morax. catarrhalis, Staph.aureus, Enterobacter.Aspergillus infection (ABPA – allergic bronchopulmonary aspergillosis)
Mycobacterial infections (in older women- mycobacterium avium complex (MAC) causing obstruction from lymphad-enopathy with right middle lobe bronchiectasis )
Int J Chron Obstruct Pulmon Dis. 2009; 4: 411–419. The pathophysiology of bronchiectasis
Paul T King
Слайд 22Effects of flora promoting bronchoectases
inhibition of the mucociliary clearance: mediators
of H. influenzae, P. aeruginosa, Streptococcus pneumoniae directly damage ciliated epithelium, and inhibit
mucous transport and release glycoproteins attracting neutrophils.H. influenzae direct damage to airway epithelium; invasion into the bronchial wall and interstitium of the lung
P. aeruginosa - forms biofilms, which form impenetrable matrix around bacteria and defend it from immune system and antibiotics
Слайд 23Immune dysfunction
Malnutrition
Extremes of age
hypogammaglobulinemia, human immunodeficiency virus (HIV), interferon
gamma receptor deficiency, type I major histocompatibility complex deficiency, late
stages of lung transplant rejection, very high IgE levels without ABPAСлайд 24Figure 1
The Lancet 2018 392, 880-890DOI: (10.1016/S0140-6736(18)31767-7)
Copyright © 2018
Elsevier Ltd Terms and Conditions
Advances in bronchiectasis: endotyping, genetics, microbiome,
and disease heterogeneityProf Patrick A Flume, MD, Prof James D Chalmers, MBChB, Kenneth N Olivier, MD The Lancet Volume 392, Issue 10150, Pages 880-890 (September 2018)Pathogenesis
vicious cycle of bacterial infection, neutrophilic elastastes induced injury of the epithelium; ciliary disfunction, progression of infection and destruction of bronchial wall
P. Cole, “Bronchiectasis,” in in. Respiratory medicine, pp. 1380–1395, Bronchiectasis. in. Respiratory medicine, London, UK, 1995.
Слайд 25Clinical manifestations
Chronic productive cough - 98% of patients
Sputum -
produced on a daily basis - 70% - 96% of
patients (4%-30% - “dry” bronchoectases.Sputum usually mucoid; during infectious exacerbations – greenish/yellowish purulent, may be offensive odor.
Sputum amount usually >50 ml daily, in mild BE – 10 ml and less; in moderate 10-150 mL ; in severe more than 150 mL
Hemoptysis - 56-92% of patients; more commonly in dry bronchiectasis; usually mild; appears from dilated bronchial arteries: massive hemoptysis – rare
Author: Ethan E Emmons, Bronchiectasis Clinical Presentation Updated: Jul 23, 2019 https://emedicine.medscape.com/article/296961-clinical#b3
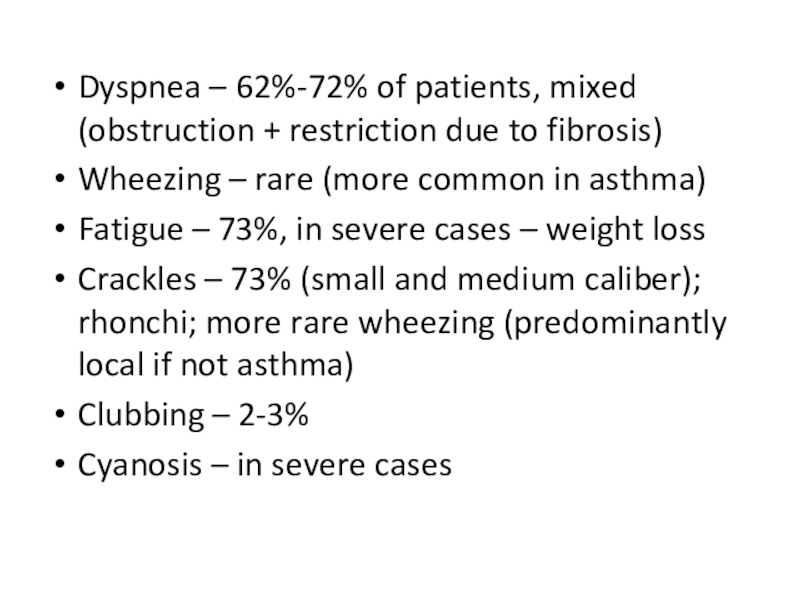
Слайд 26Dyspnea – 62%-72% of patients, mixed (obstruction + restriction due
to fibrosis)
Wheezing – rare (more common in asthma)
Fatigue – 73%,
in severe cases – weight lossCrackles – 73% (small and medium caliber); rhonchi; more rare wheezing (predominantly local if not asthma)
Clubbing – 2-3%
Cyanosis – in severe cases
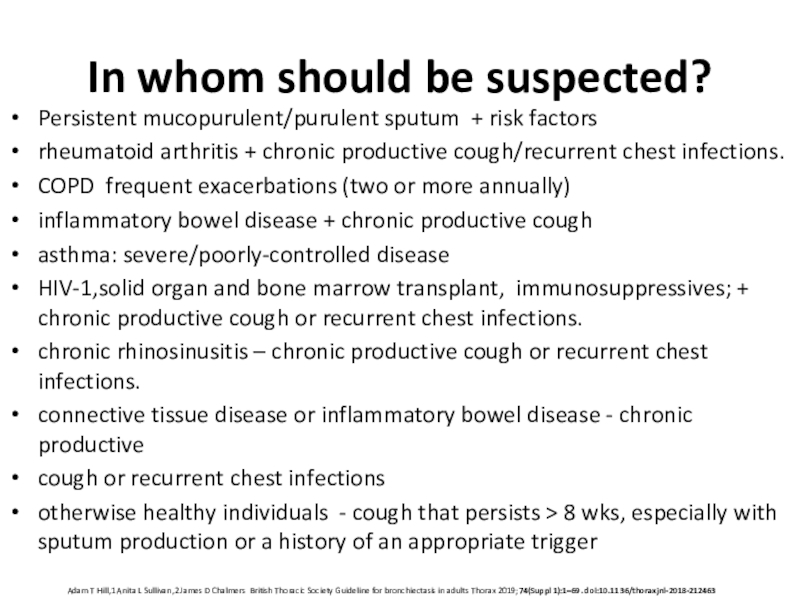
Слайд 27In whom should be suspected?
Persistent mucopurulent/purulent sputum + risk factors
rheumatoid
arthritis + chronic productive cough/recurrent chest infections.
COPD frequent exacerbations
(two or more annually)inflammatory bowel disease + chronic productive cough
asthma: severe/poorly-controlled disease
HIV-1,solid organ and bone marrow transplant, immunosuppressives; + chronic productive cough or recurrent chest infections.
chronic rhinosinusitis – chronic productive cough or recurrent chest infections.
connective tissue disease or inflammatory bowel disease - chronic productive
cough or recurrent chest infections
otherwise healthy individuals - cough that persists > 8 wks, especially with sputum production or a history of an appropriate trigger
Adam T Hill,1 Anita L Sullivan,2 James D Chalmers British Thoracic Society Guideline for bronchiectasis in adults Thorax 2019;74(Suppl 1):1–69. doi:10.1136/thoraxjnl-2018-212463
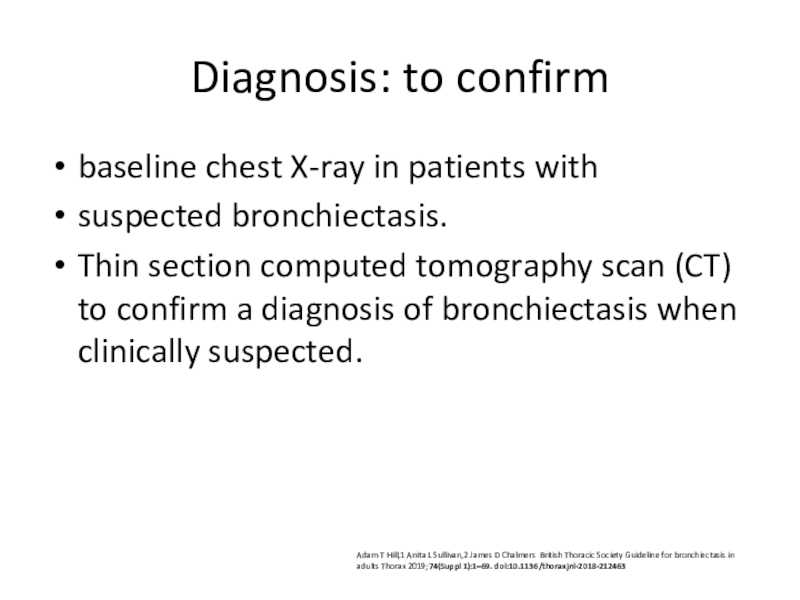
Слайд 28Diagnosis: to confirm
baseline chest X-ray in patients with
suspected bronchiectasis.
Thin section
computed tomography scan (CT) to confirm a diagnosis of bronchiectasis
when clinically suspected.Adam T Hill,1 Anita L Sullivan,2 James D Chalmers British Thoracic Society Guideline for bronchiectasis in adults Thorax 2019;74(Suppl 1):1–69. doi:10.1136/thoraxjnl-2018-212463
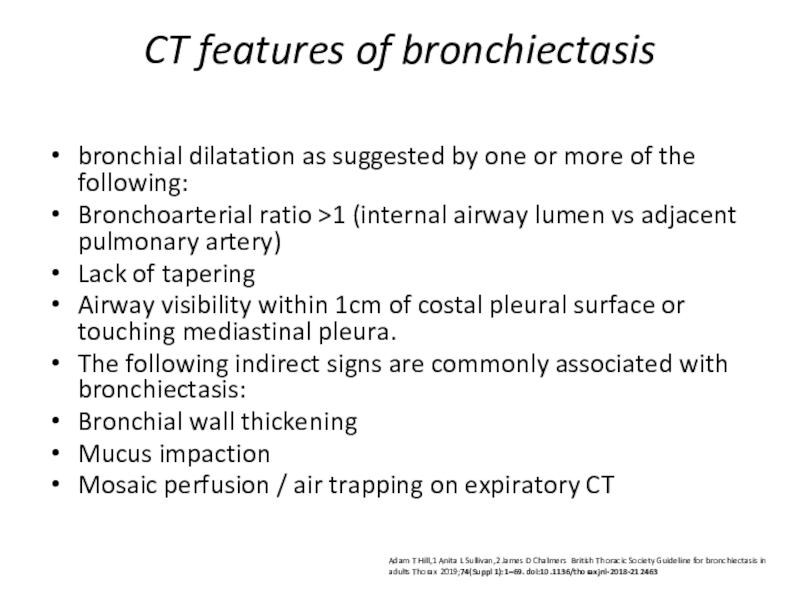
Слайд 29CT features of bronchiectasis
bronchial dilatation as suggested by one or
more of the following:
Bronchoarterial ratio >1 (internal airway lumen vs
adjacent pulmonary artery)Lack of tapering
Airway visibility within 1cm of costal pleural surface or touching mediastinal pleura.
The following indirect signs are commonly associated with bronchiectasis:
Bronchial wall thickening
Mucus impaction
Mosaic perfusion / air trapping on expiratory CT
Adam T Hill,1 Anita L Sullivan,2 James D Chalmers British Thoracic Society Guideline for bronchiectasis in adults Thorax 2019;74(Suppl 1):1–69. doi:10.1136/thoraxjnl-2018-212463
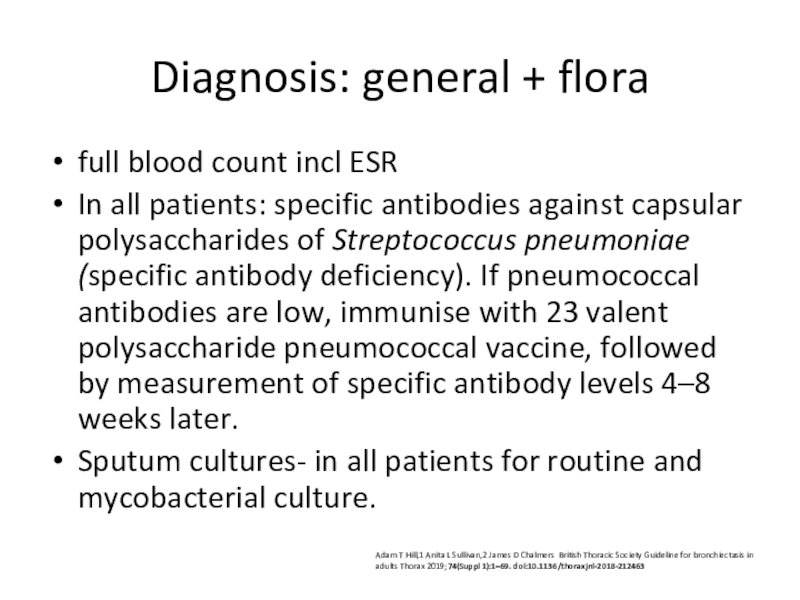
Слайд 30Diagnosis: general + flora
full blood count incl ESR
In all
patients: specific antibodies against capsular polysaccharides of Streptococcus pneumoniae (specific
antibody deficiency). If pneumococcal antibodies are low, immunise with 23 valent polysaccharide pneumococcal vaccine, followed by measurement of specific antibody levels 4–8 weeks later.Sputum cultures- in all patients for routine and mycobacterial culture.
Adam T Hill,1 Anita L Sullivan,2 James D Chalmers British Thoracic Society Guideline for bronchiectasis in adults Thorax 2019;74(Suppl 1):1–69. doi:10.1136/thoraxjnl-2018-212463
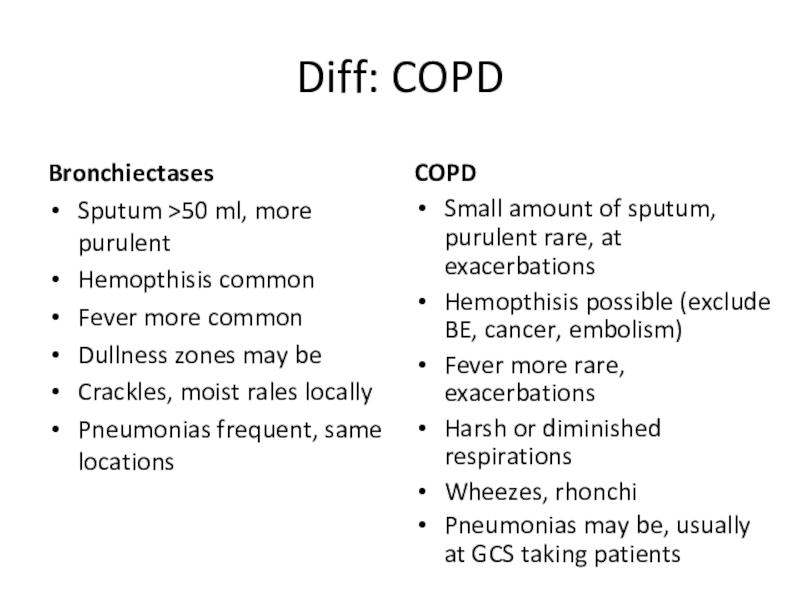
Слайд 31Diff: COPD
Bronchiectases
Sputum >50 ml, more purulent
Hemopthisis common
Fever more common
Dullness
zones may be
Crackles, moist rales locally
Pneumonias frequent, same locations
COPD
Small amount of sputum, purulent rare, at exacerbations
Hemopthisis possible (exclude BE, cancer, embolism)
Fever more rare, exacerbations
Harsh or diminished respirations
Wheezes, rhonchi
Pneumonias may be, usually at GCS taking patients
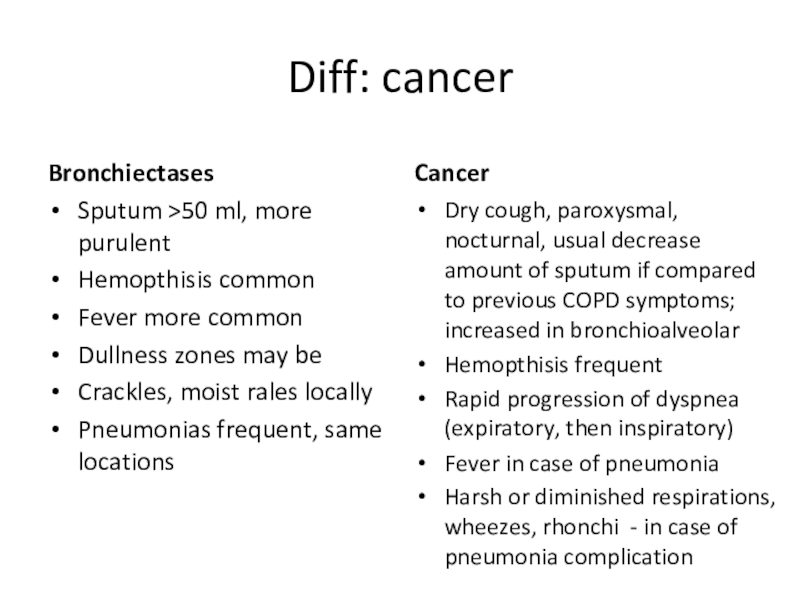
Слайд 32Diff: cancer
Bronchiectases
Sputum >50 ml, more purulent
Hemopthisis common
Fever more common
Dullness
zones may be
Crackles, moist rales locally
Pneumonias frequent, same locations
Cancer
Dry cough, paroxysmal, nocturnal, usual decrease amount of sputum if compared to previous COPD symptoms; increased in bronchioalveolar
Hemopthisis frequent
Rapid progression of dyspnea (expiratory, then inspiratory)
Fever in case of pneumonia
Harsh or diminished respirations, wheezes, rhonchi - in case of pneumonia complication
Слайд 33Diff: embolism
Bronchiectases
Sputum >50 ml, more purulent
Hemopthisis common
Fever more common
Not
typical pleural pain
PII, epigastric pulsation may be
Dullness zones may be
Crackles, moist rales locally
Pneumonias frequent, same locations
embolism
Sputum not typical
Hemopthisis frequent
Pleural pain typical, PII, epigastric pulsation
Deep veins thrombosis (unilateral leg pain and edema)
BP decrease
Fever not typical (if more than 2 days duration – pneumonia may develop)
Local changes (dullness, rales) in case of pneumonia
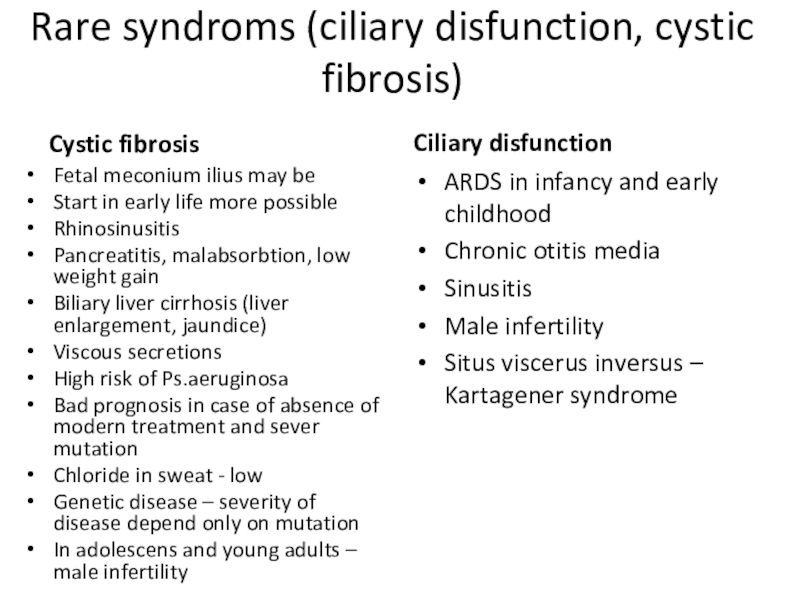
Слайд 34Rare syndroms (ciliary disfunction, cystic fibrosis)
Cystic fibrosis
Fetal meconium ilius may
be
Start in early life more possible
Rhinosinusitis
Pancreatitis, malabsorbtion, low weight gain
Biliary
liver cirrhosis (liver enlargement, jaundice)Viscous secretions
High risk of Ps.aeruginosa
Bad prognosis in case of absence of modern treatment and sever mutation
Chloride in sweat - low
Genetic disease – severity of disease depend only on mutation
In adolescens and young adults – male infertility
Ciliary disfunction
ARDS in infancy and early childhood
Chronic otitis media
Sinusitis
Male infertility
Situs viscerus inversus – Kartagener syndrome
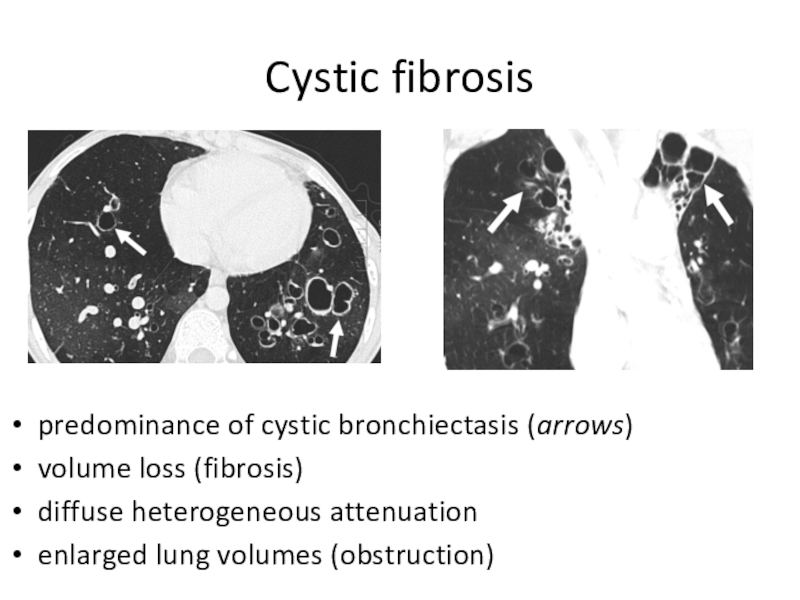
Слайд 35Cystic fibrosis
predominance of cystic bronchiectasis (arrows)
volume loss (fibrosis)
diffuse
heterogeneous attenuation
enlarged lung volumes (obstruction)
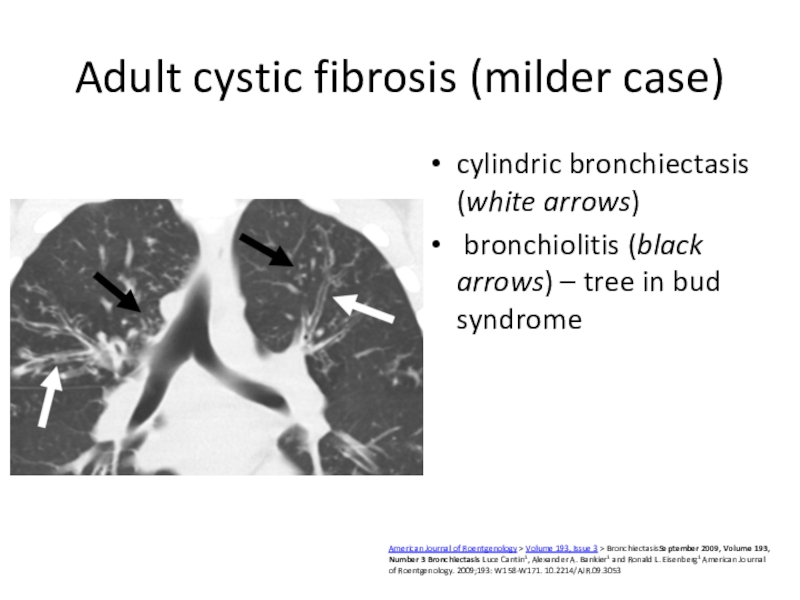
Слайд 36Adult cystic fibrosis (milder case)
cylindric bronchiectasis (white arrows)
bronchiolitis
(black arrows) – tree in bud syndrome
American Journal of Roentgenology >
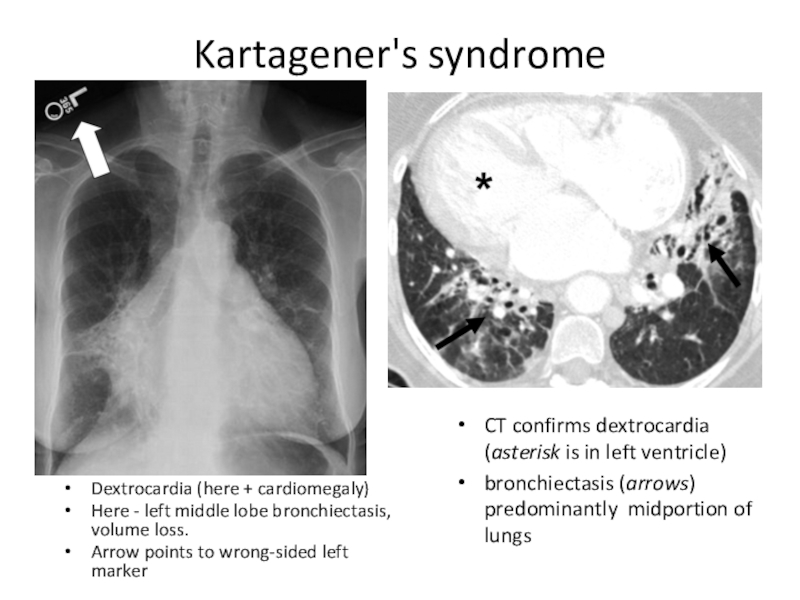
Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053 Слайд 37Kartagener's syndrome
Dextrocardia (here + cardiomegaly)
Here - left middle lobe
bronchiectasis, volume loss.
Arrow points to wrong-sided left marker
CT
confirms dextrocardia (asterisk is in left ventricle)bronchiectasis (arrows) predominantly midportion of lungs
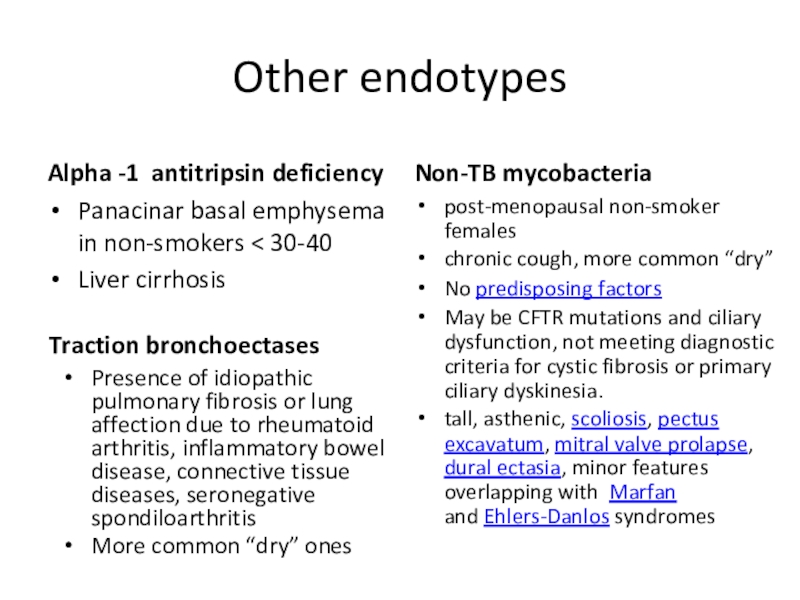
Слайд 38Other endotypes
Alpha -1 antitripsin deficiency
Panacinar basal emphysema in non-smokers
30-40
Liver cirrhosis
Non-TB mycobacteria
post-menopausal non-smoker females
chronic cough, more common “dry”
No
predisposing factors May be CFTR mutations and ciliary dysfunction, not meeting diagnostic criteria for cystic fibrosis or primary ciliary dyskinesia.
tall, asthenic, scoliosis, pectus excavatum, mitral valve prolapse, dural ectasia, minor features overlapping with Marfan and Ehlers-Danlos syndromes
Presence of idiopathic pulmonary fibrosis or lung affection due to rheumatoid arthritis, inflammatory bowel disease, connective tissue diseases, seronegative spondiloarthritis
More common “dry” ones
Traction bronchoectases
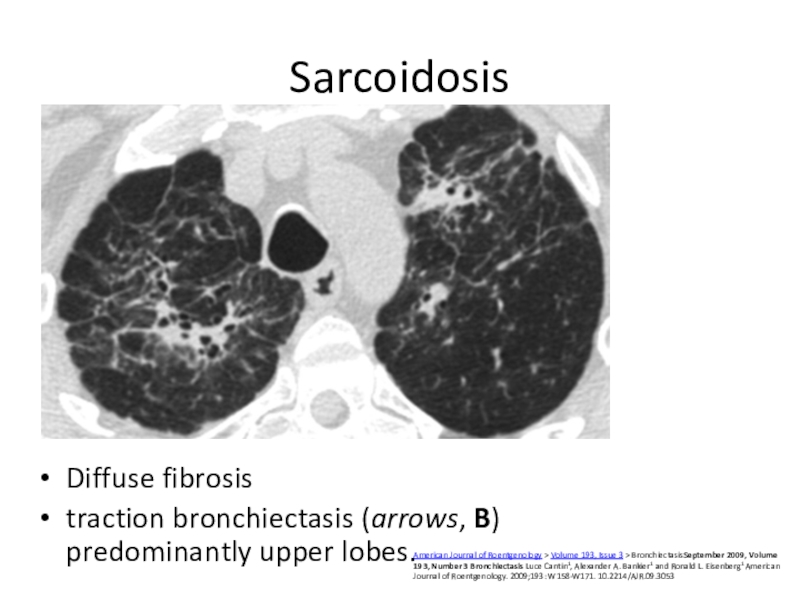
Слайд 39Sarcoidosis
Diffuse fibrosis
traction bronchiectasis (arrows, B) predominantly upper lobes.
American Journal of
Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number
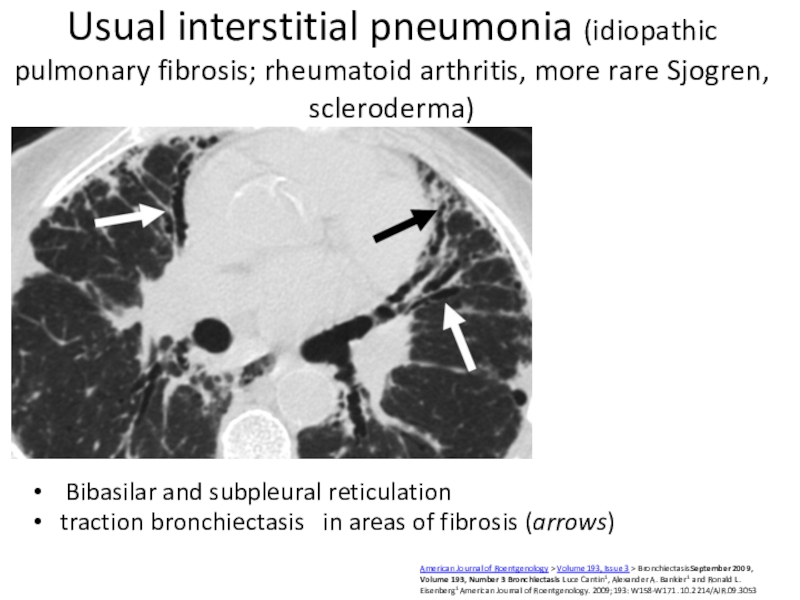
3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053Слайд 40Usual interstitial pneumonia (idiopathic pulmonary fibrosis; rheumatoid arthritis, more rare
Sjogren, scleroderma)
Bibasilar and subpleural reticulation
traction bronchiectasis in
areas of fibrosis (arrows)American Journal of Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053
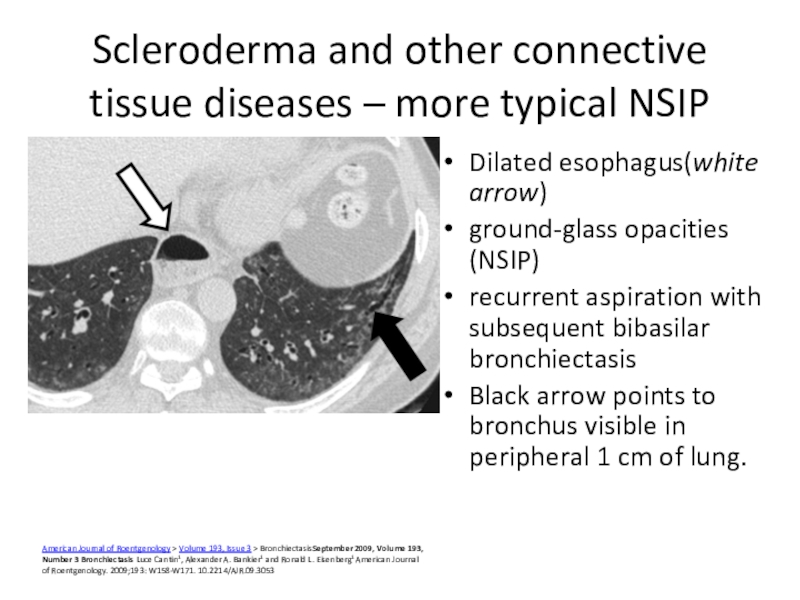
Слайд 41Scleroderma and other connective tissue diseases – more typical NSIP
Dilated
esophagus(white arrow)
ground-glass opacities (NSIP)
recurrent aspiration with subsequent bibasilar bronchiectasis
Black arrow
points to bronchus visible in peripheral 1 cm of lung.American Journal of Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053
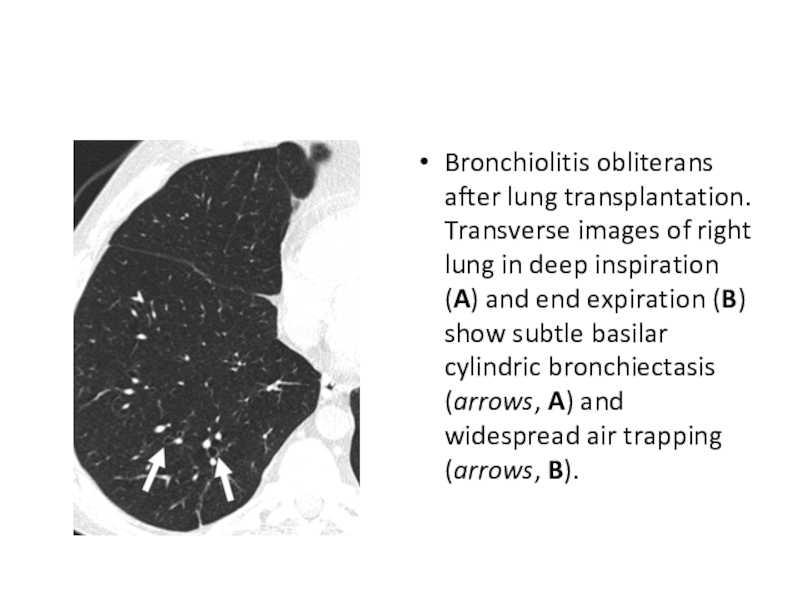
Слайд 42Bronchiolitis obliterans after lung transplantation. Transverse images of right lung
in deep inspiration (A) and end expiration (B) show subtle
basilar cylindric bronchiectasis (arrows, A) and widespread air trapping (arrows, B).Слайд 43Other endotypes
ABPA
Blood eosinophilia
thick sputum with black
Bronchial obstruction with wheeze,
Asthma in case history
recurrent exacerbations
Post-infective
ulilateral, localized
Severe infection in case
history Start at early age
Infections from childhood/infancy if inborn
Frequent exacerbations
Pneumonias
non-respiratory infections
Immune deficiency
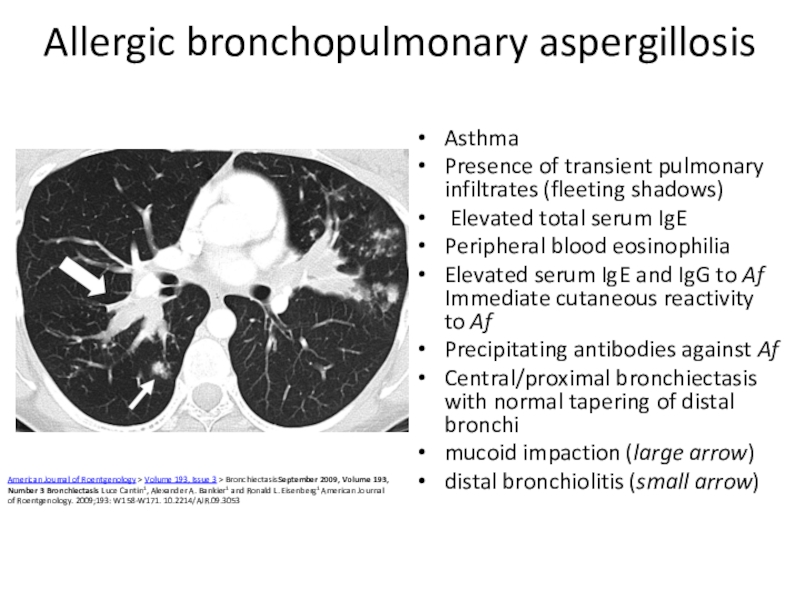
Слайд 44Allergic bronchopulmonary aspergillosis
Asthma
Presence of transient pulmonary infiltrates (fleeting shadows)
Elevated
total serum IgE
Peripheral blood eosinophilia
Elevated serum IgE and IgG
to Af
Immediate cutaneous reactivity to AfPrecipitating antibodies against Af
Central/proximal bronchiectasis with normal tapering of distal bronchi
mucoid impaction (large arrow)
distal bronchiolitis (small arrow)
American Journal of Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053
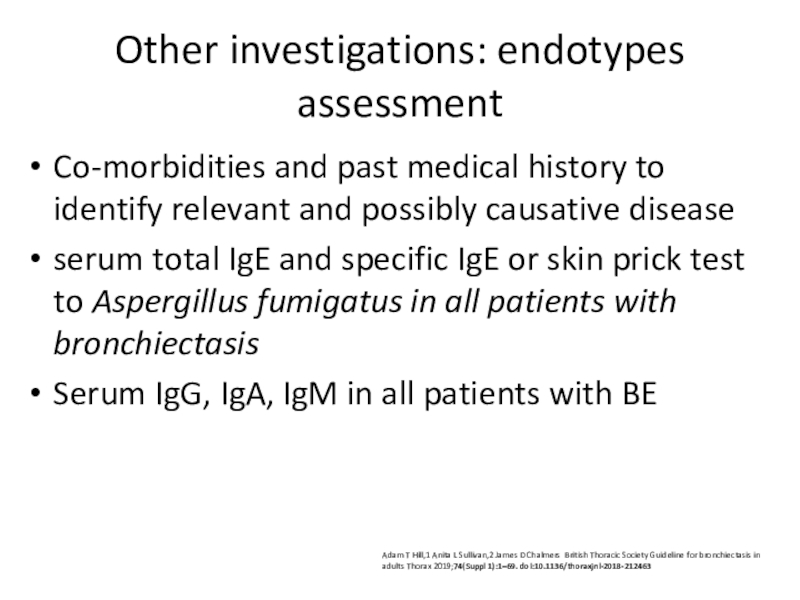
Слайд 46Other investigations: endotypes assessment
Co-morbidities and past medical history to
identify relevant and possibly causative disease
serum total IgE and specific
IgE or skin prick test to Aspergillus fumigatus in all patients with bronchiectasisSerum IgG, IgA, IgM in all patients with BE
Adam T Hill,1 Anita L Sullivan,2 James D Chalmers British Thoracic Society Guideline for bronchiectasis in adults Thorax 2019;74(Suppl 1):1–69. doi:10.1136/thoraxjnl-2018-212463
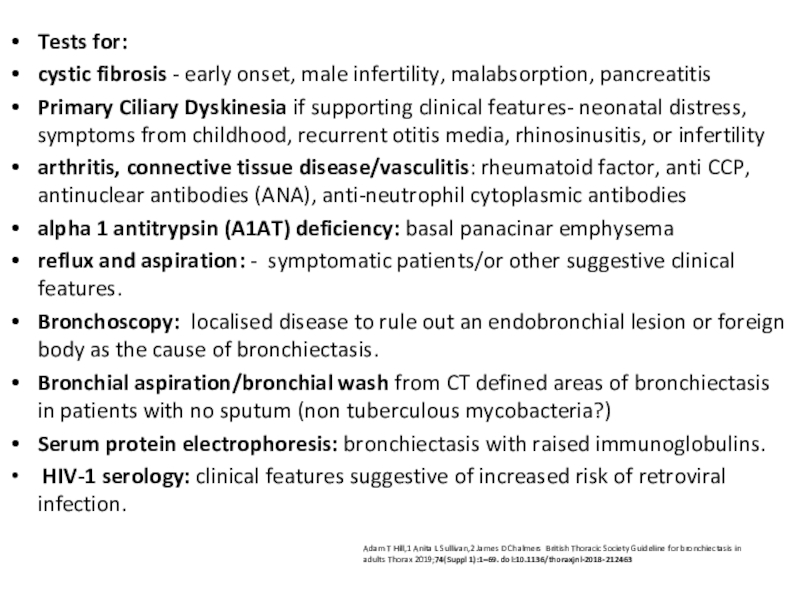
Слайд 47Tests for:
cystic fibrosis - early onset, male infertility, malabsorption,
pancreatitis
Primary Ciliary Dyskinesia if supporting clinical features- neonatal distress, symptoms
from childhood, recurrent otitis media, rhinosinusitis, or infertilityarthritis, connective tissue disease/vasculitis: rheumatoid factor, anti CCP, antinuclear antibodies (ANA), anti-neutrophil cytoplasmic antibodies
alpha 1 antitrypsin (A1AT) deficiency: basal panacinar emphysema
reflux and aspiration: - symptomatic patients/or other suggestive clinical features.
Bronchoscopy: localised disease to rule out an endobronchial lesion or foreign body as the cause of bronchiectasis.
Bronchial aspiration/bronchial wash from CT defined areas of bronchiectasis in patients with no sputum (non tuberculous mycobacteria?)
Serum protein electrophoresis: bronchiectasis with raised immunoglobulins.
HIV-1 serology: clinical features suggestive of increased risk of retroviral infection.
Adam T Hill,1 Anita L Sullivan,2 James D Chalmers British Thoracic Society Guideline for bronchiectasis in adults Thorax 2019;74(Suppl 1):1–69. doi:10.1136/thoraxjnl-2018-212463
Слайд 48Other investigations
Spirogram/functional investigation of lungs, oxygen saturation, blood gases
Daily
protein loss, GFR, urine analysis – for early diagnosis of
inflammatory (SAA) amyloidosisOther investigations if necessary
Слайд 49Focal idiopathic in left lower lobe
non-TB mycobacteria
Perimenopausal females
Usually dry bronchoectases
Focal
bronchiectasis frequently
American Journal of Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember
2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053Слайд 50subtle idiopathic bibasilar cylindric bronchiectasis shows signet-ring sign (arrows).
https://www.ajronline.org/doi/10.2214/AJR.09.3053
marked
idiopathic left lower bronchiectasis with volume loss, bronchial wall thickening,
and diffuse opacity. https://www.ajronline.org/doi/10.2214/AJR.09.3053Idiopathic – lower lobe predominance, different severity
Слайд 51Mycobacterium avium- intracellulare infection
Bronchiectasis (arrows) predominantly involves right middle lobe and
lingula.
American Journal of Roentgenology >
Volume 193, Issue 3 >
BronchiectasisSeptember 2009, Volume 193,
Number 3 BronchiectasisLuce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053
Слайд 52Obstruction
Tumor
More gradual onset (1-3 mo)
Dyspnea progression from expiratory
to inspiratory
Dry cough, hemopthisis
More see “lung cancer”
Foreign body
Usually in children
May
be acute suffocation episode in case history with stridor Relapsing pneumonias
Слайд 53Carcinoid.
Endobronchial growth
May arise berofe bifurcation of lobar bronchi
Serotonin secretion
symptoms as following:
Flushes up to 10-20 times daily
Bronchospasm
Restritive
CMP of endomyocardial natureAmerican Journal of Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053
Слайд 54Carcinoid
Distal bronchiectases
American Journal of Roentgenology > Volume 193, Issue 3 >
BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A.
Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053Слайд 55Tumors: postradiation fibrosis
Right paramediastinal fibrotic changes, developed after treatment of
lung cancer, are associated with traction bronchiectasis (arrows).
American Journal of
Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053Слайд 56Broncholithiasis: post TB
Calcified left upper lobe endobronchial broncholithiasis
Results of lymph
node calcification (compression and erosion of calcified perigronchial lymph nodes
Cause
– TB, histoplasmosis or other granulomatous disease, more rare foreign body 0.1% - 0.2% of all lung diseases.
Broncholithiasis: An Uncommon Cause of Chronic Cough
Ungprasert, Patompong MD; Srivali, Narat MD; Bauer, Michael A. MD; Edmonds, Lee C. MD
Author InformationJournal of Bronchology & Interventional Pulmonology: January 2014 - Volume 21 - Issue 1 - p 102-103
American Journal of Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053
Слайд 57Congenital abnormalities
Congenital stenosis
(left mainstem bronchus
Bronchial atresia
focal bronchiectasis (arrow) distal
to bronchial atresia associated with hyperlucency and hyperexpansion of left
lung.American Journal of Roentgenology > Volume 193, Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald
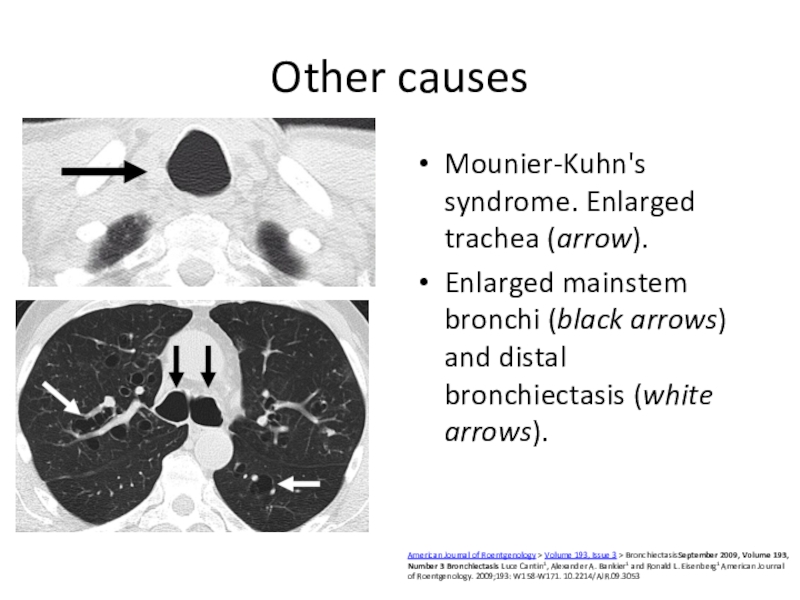
Слайд 58Other causes
Mounier-Kuhn's syndrome. Enlarged trachea (arrow).
Enlarged mainstem bronchi (black arrows)
and distal bronchiectasis (white arrows).
American Journal of Roentgenology > Volume 193,
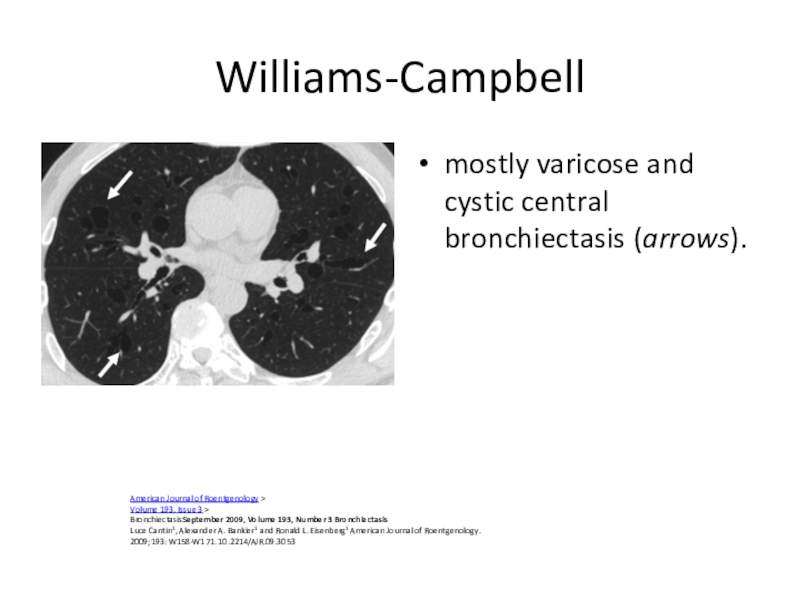
Issue 3 > BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis Luce Cantin1, Alexander A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053Слайд 59Williams-Campbell
mostly varicose and cystic central bronchiectasis (arrows).
American Journal of Roentgenology >
Volume
193, Issue 3 >
BronchiectasisSeptember 2009, Volume 193, Number 3 Bronchiectasis
Luce Cantin1, Alexander
A. Bankier1 and Ronald L. Eisenberg1 American Journal of Roentgenology. 2009;193: W158-W171. 10.2214/AJR.09.3053Слайд 60Advances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneityProf Patrick
A Flume, MD, Prof James D Chalmers, MBChB, Kenneth N
Olivier, MD The Lancet Volume 392, Issue 10150, Pages 880-890 (September 2018)Слайд 61Advances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneityProf Patrick
A Flume, MD, Prof James D Chalmers, MBChB, Kenneth N
Olivier, MD The Lancet Volume 392, Issue 10150, Pages 880-890 (September 2018)Слайд 62Cystic fibrosis
Cystic fibrosis (CF) is an autosomal recessive disease
Loss of
function of the cystic fibrosis transmembrane conductance regulator (CFTR) at
the apical membrane of airway epithelial cellsAdvances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneity The lancet Volume 392, Issue 10150, 8–14 September 2018, Pages 880-890
American Journal of Respiratory and Critical Care Medicine
Vol. 187, No. 7 | Apr 01, 2013
Cystic Fibrosis Pulmonary Guidelines Chronic Medications for Maintenance of Lung Health
Peter J. Mogayzel Jr.1, Edward T. Naureckas 2,
Слайд 63Pathogenesis: hypothesis
chemical shield’ hypothesis: in normal condition airway epithelium produces
low salt (
antimicrobial activities are performedimportance of isotonic (i.e. ∼150 mM NaCl) airway surface liquid volume normally performs efficient mucus clearance
Слайд 64Periciliary liquid layer
The mucus layer as a liquid reservoir.
Upper panel depicts normal geometry of mucus and periciliary liquid
(PCL) layersLower left: additional liquid expands the mucus layer
Lower right: removal of liquid can remove ∼50% of the mucus layer without perturbing PCL volume
Слайд 65Advanced Drug Delivery Reviews Volume 54, Issue 11, 5 December 2002,
Pages 1359-1371 An overview of the pathogenesis of cystic fibrosis
lung disease R.CboucherСлайд 66CFTR mutations classifications
Advances in bronchiectasis: endotyping, genetics, microbiome, and disease
heterogeneity The lancet Volume 392, Issue 10150, 8–14 September 2018, Pages
880-890Слайд 69Idiopathic bronchiectasis associated with non-tuberculous mycobacteria (NTM)
post-menopausal non-smoker females
chronic cough
No
predisposing factors
share characteristics with other endotypes, notably a high prevalence
of CFTR mutations and ciliary dysfunction, but do not meet diagnostic criteria for cystic fibrosis or primary ciliary dyskinesia. tall, asthenic type, with scoliosis, pectus excavatum, mitral valve prolapse, dural ectasia, minor features overlapping with Marfan and Ehlers-Danlos syndromes
Advances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneity The lancet Volume 392, Issue 10150, 8–14 September 2018, Pages 880-890
Слайд 70Advances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneityProf Patrick
A Flume, MD, Prof James D Chalmers, MBChB, Kenneth N
Olivier, MD The Lancet Volume 392, Issue 10150, Pages 880-890 (September 2018)Слайд 71Advances in bronchiectasis: endotyping, genetics, microbiome, and disease heterogeneityProf Patrick
A Flume, MD, Prof James D Chalmers, MBChB, Kenneth N
Olivier, MD The Lancet Volume 392, Issue 10150, Pages 880-890 (September 2018)Слайд 72T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for
bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 73Initial treatment
European Respiratory Society guidelines for the management of adult
bronchiectasis
Eva Polverino, Pieter C. Goeminne, Melissa J. McDonnell, Stefano Aliberti, Sara E. Marshall, Michael R. Loebinger, European Respiratory Journal 2017 50: 1700629;
Слайд 74Offer annual influenza immunisation to all patients with bronchiectasis. (D)
Offer
polysaccharide pneumococcal vaccination to all patients with bronchiectasis.
T Hill A, L Sullivan A, D
Chalmers J, et alBritish Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 75Physiotherapy – drainage promotion
AD: autogenic drainage; ELTGOL: total slow
expiration with open glottis and infralateral position; ACBT: active cycle
of breathing techniques; PEP: positive expiratory pressure; T-PEP: temporary positive expiratory pressure; HFCWO: high frequency chest wall oscillation.European Respiratory Society guidelines for the management of adult bronchiectasis
Eva Polverino, Pieter C. Goeminne, Melissa J. McDonnell, Stefano Aliberti, Sara E. Marshall, Michael R. Loebinger, European Respiratory Journal 2017 50: 1700629;
Слайд 76Airway clearance techniques
should be taught by a respiratory physiotherapist.
Patients admitted
with an exacerbation of bronchiectasis should be seen daily by
a respiratory physiotherapist until their airway clearance is optimised.CT imaging should be reviewed to complement the physiotherapy assessment. Where indicated, this information could be used in order to teach the patient the appropriate postural drainage position(s) for their affected bronchopulmonary segment(s).
T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 77Consider autogenic drainage, positive expiratory pressure, high frequency chest wall
oscillation and intrapulmonary percussive ventilation as an alternative airway clearance
technique if other techniques are not effective or acceptable to the patient.Patients should be encouraged to perform regular physical exercise (plus the forced expiration technique/huff) to promote airway clearance.
If there is ongoing haemoptysis, refer back to the respiratory physiotherapist to determine the optimum airways clearance technique.
Advise individuals to perform their airway clearance technique for a minimum of 10 minutes (up to a maximum of 30 minutes). After this time they should continue until two clear huffs or coughs are completed, or until the patient is starting to become fatigued.
T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 78Airway clearance techniques during an acute exacerbation
Manual techniques may be
offered to enhance sputum clearance when the patient is fatigued
or undergoing an exacerbation.Consider intermittent positive pressure breathing or non-invasive ventilation during an acute exacerbation to offload the work of breathing so fatigued and/or breathless patients can tolerate a longer treatment session and can adopt postural drainage positions.
T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 79Mucoactives in bronchiectasis
Do not routinely use recombinant human DNase in
adults with bronchiectasis.
Consider the use of humidification with sterile
water or normal saline to facilitate airway clearance. Consider a trial of mucoactive treatment in patients with bronchiectasis who have difficulty in sputum expectoration.
Perform an airway reactivity challenge test when inhaled mucoactive treatment is first administered.
Consider pre-treatment with a bronchodilator prior to inhaled or nebulised mucoactive treatments especially in individuals where bronchoconstriction is likely (patients with asthma or bronchial hyper-reactivity and those with severe airflow obstruction FEV1<1 litre).
If carbocysteine is prescribed, a 6 month trial should be given and continued if there is ongoing clinical benefit.
T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 80T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for
bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 81T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for
bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 82Inhaled GCS:
Do not offer long-term oral corticosteroids for patients
with bronchiectasis without other indications (such as ABPA, chronic asthma,
COPD, inflammatory bowel disease). (D)Inhaled corticosteroids have an established role in the management of asthma and in a proportion of patients with COPD which are common co-morbid conditions in bronchiectasis.
T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 83PDE inhibitors, CXCR2 antagonists, statins etc
Do not routinely offer phosphodiesterase
type 4 (PDE4) inhibitors, methylxanthines or leukotriene receptor antagonists for
bronchiectasis treatment. (D)Do not routinely offer CXCR2 antagonists, neutrophil elastase inhibitors or statins for bronchiectasis treatment. (B)
T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 84Antibiotics
European Respiratory Society guidelines for the management of adult bronchiectasis
Eva Polverino, Pieter
C. Goeminne, Melissa J. McDonnell, Stefano Aliberti, Sara E. Marshall, Michael R. Loebinger, European Respiratory Journal 2017 50: 1700629;
Слайд 85Consider long term antibiotics in patients with bronchiectasis who experience
3 or more exacerbations per year. (A)
Non- P. aeruginosa colonised
patientse. Use azithromycin or erythromycin for patient with bronchiectasis. (A)
f. Consider inhaled gentamicin as a second line alternative to azithromycin or erythromycin.
g. Consider doxycycline as an alternative in patients intolerant of macrolides or in whom they are ineffective. (C)
T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
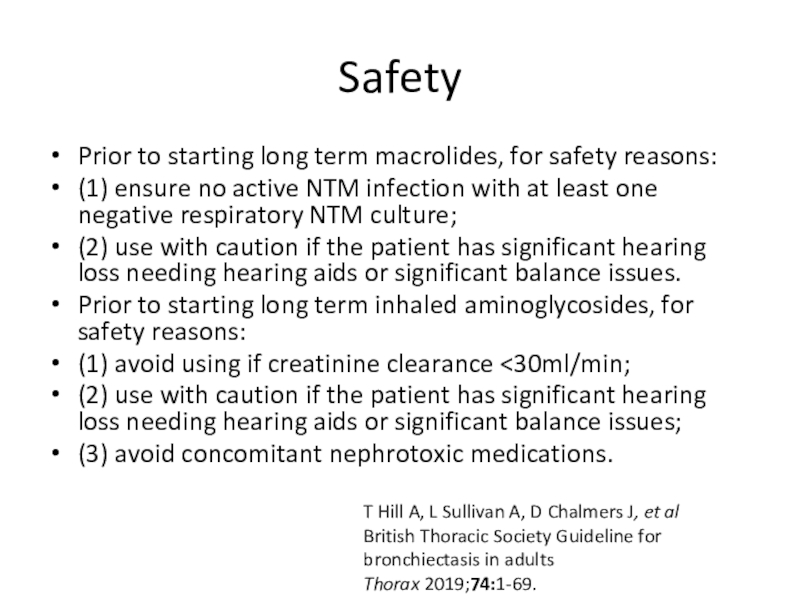
Слайд 86Safety
Prior to starting long term macrolides, for safety reasons:
(1)
ensure no active NTM infection with at least one negative
respiratory NTM culture;(2) use with caution if the patient has significant hearing loss needing hearing aids or significant balance issues.
Prior to starting long term inhaled aminoglycosides, for safety reasons:
(1) avoid using if creatinine clearance <30ml/min;
(2) use with caution if the patient has significant hearing loss needing hearing aids or significant balance issues;
(3) avoid concomitant nephrotoxic medications.
T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
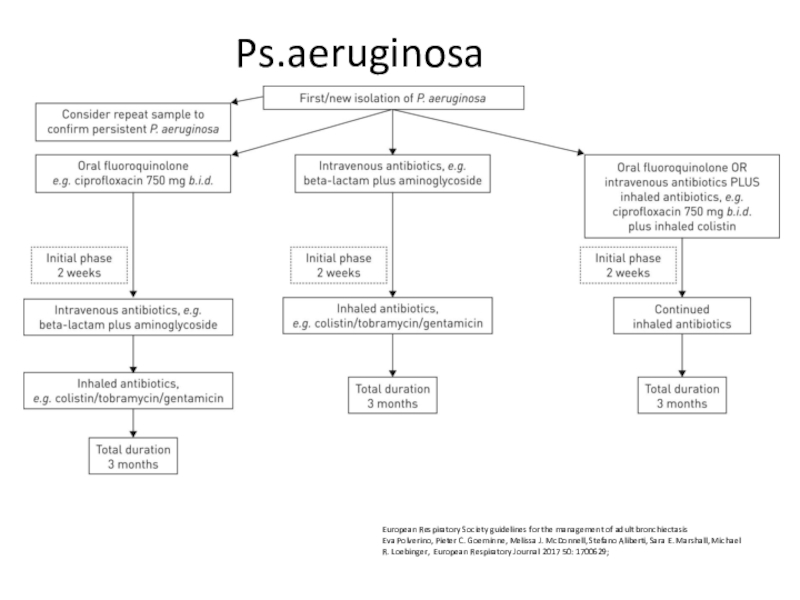
Слайд 87Ps.aeruginosa
European Respiratory Society guidelines for the management of adult bronchiectasis
Eva Polverino, Pieter
C. Goeminne, Melissa J. McDonnell, Stefano Aliberti, Sara E. Marshall, Michael R. Loebinger, European Respiratory Journal 2017 50: 1700629;
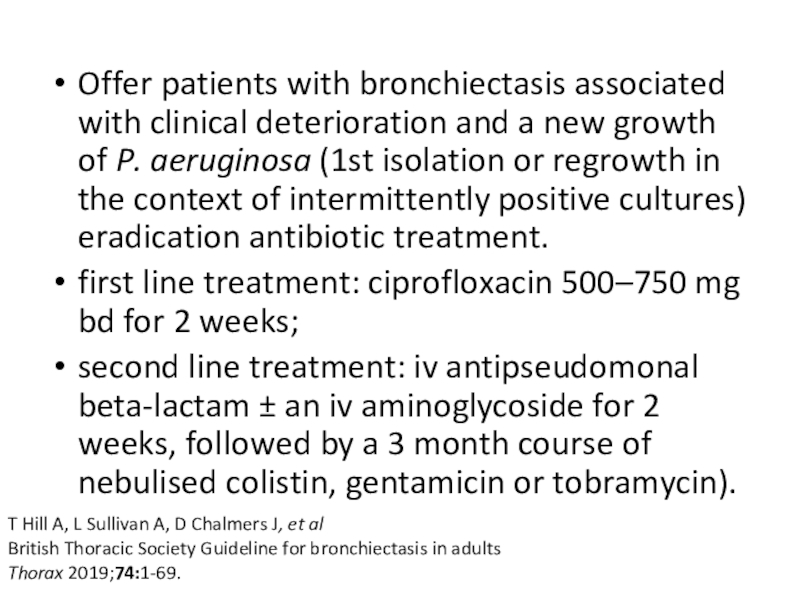
Слайд 88Offer patients with bronchiectasis associated with clinical deterioration and a
new growth of P. aeruginosa (1st isolation or regrowth in the context
of intermittently positive cultures) eradication antibiotic treatment.first line treatment: ciprofloxacin 500–750 mg bd for 2 weeks;
second line treatment: iv antipseudomonal beta-lactam ± an iv aminoglycoside for 2 weeks, followed by a 3 month course of nebulised colistin, gentamicin or tobramycin).
T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 89Offer patients with bronchiectasis associated with clinical deterioration and a
new growth of methicillin-resistant S. aureus (MRSA) (1st isolation or regrowth in
the context of intermittently positive cultures) eradication. This should be attempted especially in view of infection control issueT Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 90Consider long term oxygen therapy for patients with bronchiectasis and
respiratory failure, using the same eligibility criteria as for COPD.
(D)Consider domiciliary non-invasive ventilation with humidification for patients with bronchiectasis and respiratory failure associated with hypercapnia, especially where this is associated with symptoms or recurrent hospitalisation.
T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 91Consider lung resection in patients with localised disease whose symptoms
are not controlled by medical treatment optimised by a bronchiectasis
specialist. (D)Consider transplant referral in bronchiectasis patients aged 65 years or less if the FEV1 is <30% with significant clinical instability or if there is a rapid progressive respiratory deterioration despite optimal medical management. (D)
Consider earlier transplant referral in bronchiectasis patients with poor lung function and the following additional factors: massive haemoptysis, severe secondary pulmonary hypertension, ICU admissions or respiratory failure (particularly if requiring NIV).(D
T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.
Слайд 92 allergic broncho-pulmonary aspergillosis
Offer oral corticosteroid to patients with active ABPA.
An initial dose of 0.5 mg/kg/d, for 2 weeks is
recommended. Wean steroids according to clinical response and serum IgE levels. (D)Consider itraconazole as a steroid sparing agent for patients dependent on oral corticosteroids where difficulty in weaning is experienced. (B)
Monitor patients with active ABPA with total IgE level to assess treatment response
T Hill A, L Sullivan A, D Chalmers J, et al
British Thoracic Society Guideline for bronchiectasis in adults
Thorax 2019;74:1-69.