Слайд 2Why use iv fluid
•Think about why you're ordering IVF
-
NPO
- significant volume deficit
- ongoing loss
- specific
goal to fluid therapy(hydration prior to contrast dye)
• Consider appropriateness of IVF daily in each patient
•Do not use IVF if they are unnecessary, complications: fluid overload, electrolyte disturbance, line infection.
Слайд 3Outline of Talk
Fluid compartments
What can go wrong
Calculating fluid requirements
Principles of
fluid replacement
Scenarios
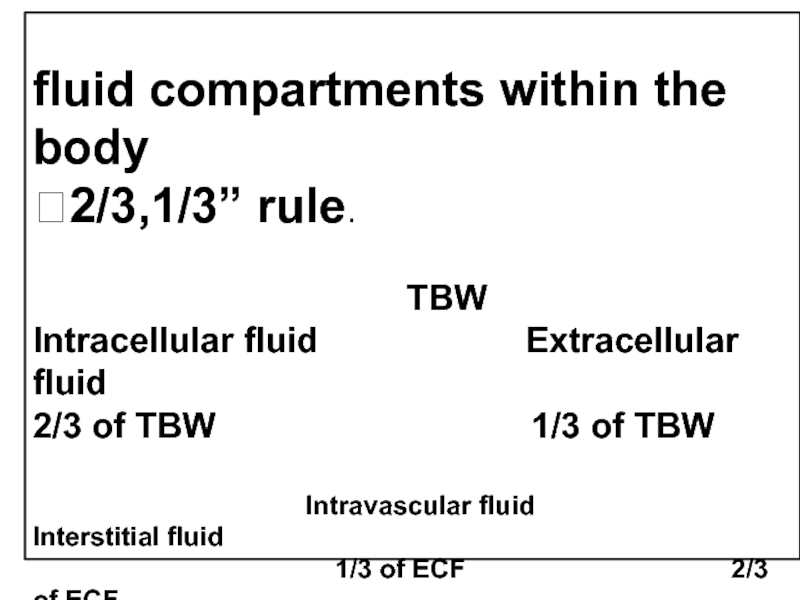
Слайд 560% of body weight is fluid
2/3 is intracellular and 1/3
extracellular
2/3 of extracellular is interstitial and 1/3 intravascular
Where is the
Fluid?
Слайд 6
fluid compartments within the body
2/3,1/3” rule.
TBW
Intracellular fluid Extracellular fluid
2/3 of TBW 1/3 of TBW
Intravascular fluid Interstitial fluid
1/3 of ECF 2/3 of ECF
F NonF
CSF + J fluid
Слайд 7Intravascular
5 litres
Interstitial
10 litres
Intracellular
30 litres
60% of body weight is fluid (55)
2/3
is intracellular and 1/3 extracellular
2/3 of extracellular is interstitial and
1/3 intravascular
So for a 70kg person…
Слайд 8
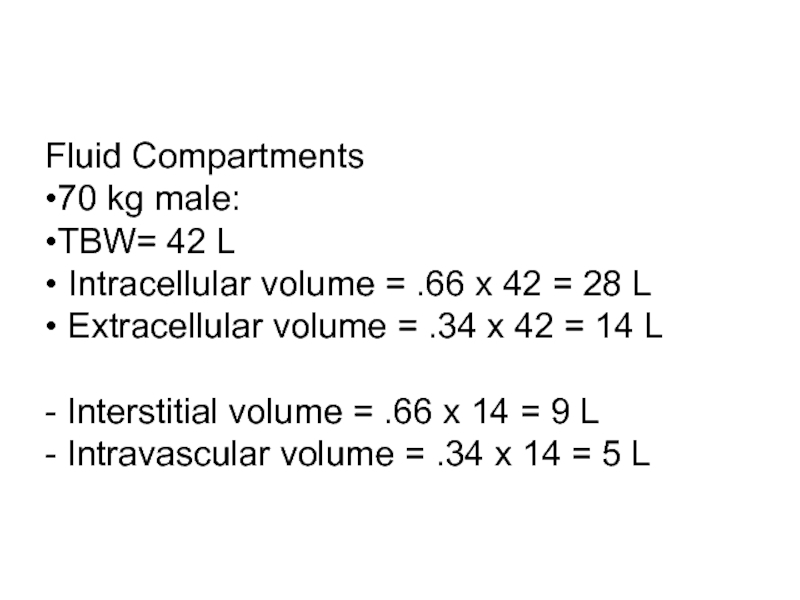
Fluid Compartments
•70 kg male:
•TBW= 42 L
• Intracellular
volume = .66 x 42 = 28 L
• Extracellular
volume = .34 x 42 = 14 L
- Interstitial volume = .66 x 14 = 9 L
- Intravascular volume = .34 x 14 = 5 L
Слайд 9What is normal fluid intake and output?
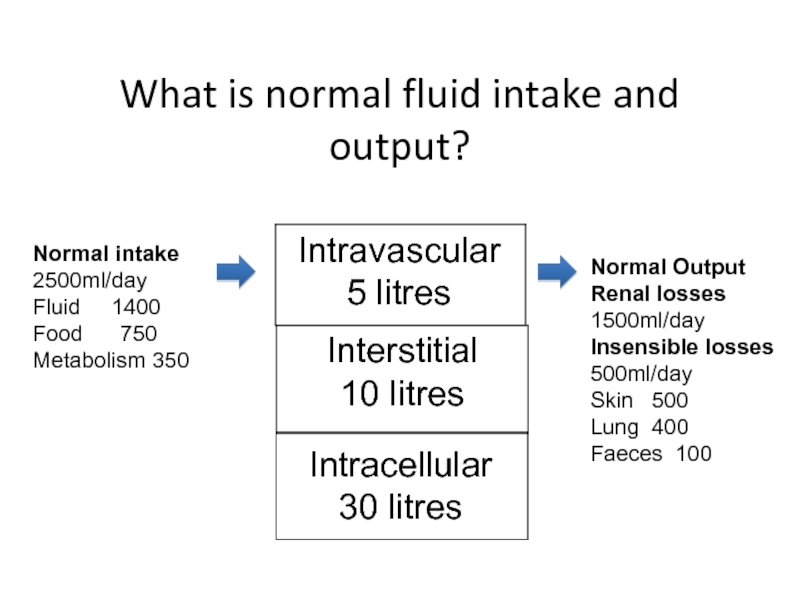
Слайд 10Intravascular
5 litres
Interstitial
10 litres
Intracellular
30 litres
Normal Output
Renal losses
1500ml/day
Insensible losses
500ml/day
Skin 500
Lung
400
Faeces 100
Normal intake
2500ml/day
Fluid 1400
Food 750
Metabolism 350
What
is normal fluid intake and output?
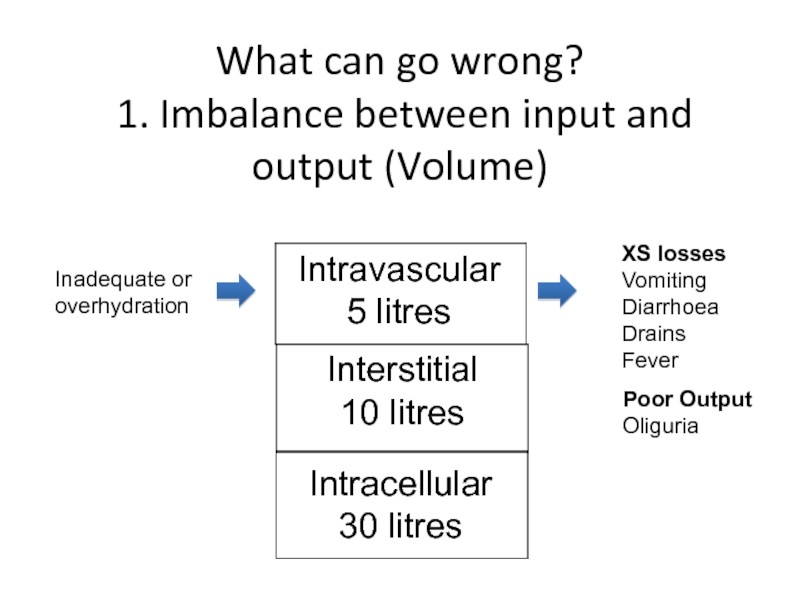
Слайд 12Intravascular
5 litres
Interstitial
10 litres
Intracellular
30 litres
XS losses
Vomiting
Diarrhoea
Drains
Fever
Poor Output
Oliguria
Inadequate or
overhydration
What can go
wrong?
1. Imbalance between input and output (Volume)
Слайд 13Intravascular
Interstitial
Intravascular
pressure
Capillary
leakage
Plasma oncotic pressure
(hypoalbiminaemia)
Peripheral +/- pulmonary oedema
What can
go wrong?
2. Redistribution
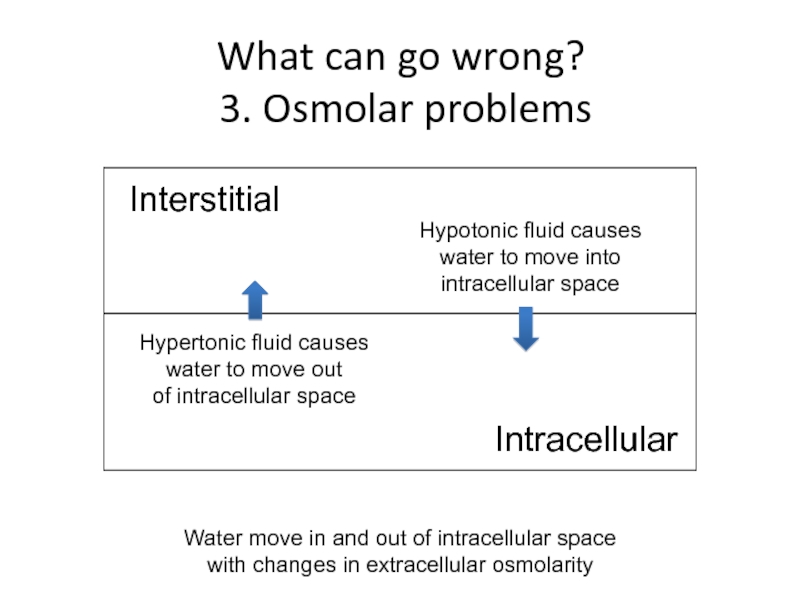
Слайд 14Interstitial
Intracellular
Hypertonic fluid causes
water to move out
of intracellular space
What
can go wrong?
3. Osmolar problems
Hypotonic fluid causes
water to
move into
intracellular space
Water move in and out of intracellular space
with changes in extracellular osmolarity
Слайд 15What can go wrong?
4- concentration
5- composition
6- Acid Base
Balance
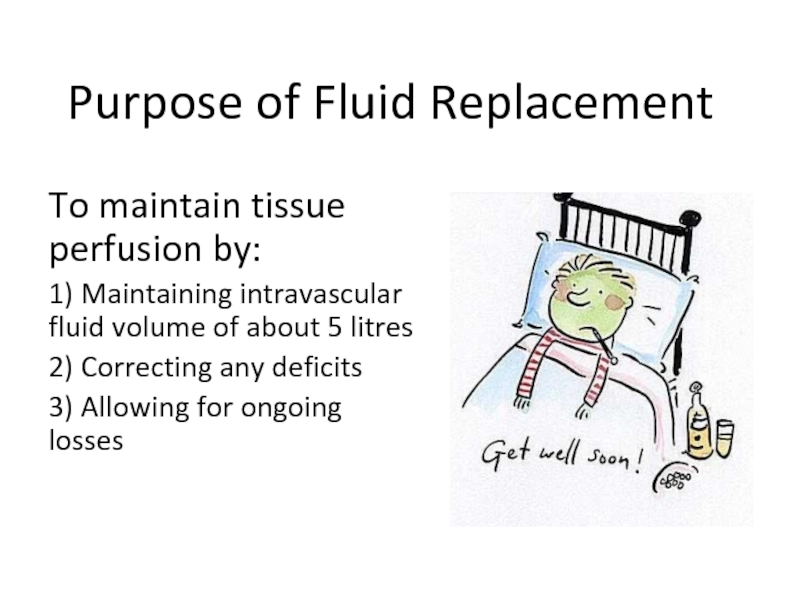
Слайд 16Purpose of Fluid Replacement
To maintain tissue perfusion by:
1) Maintaining intravascular
fluid volume of about 5 litres
2) Correcting any deficits
3) Allowing
for ongoing losses
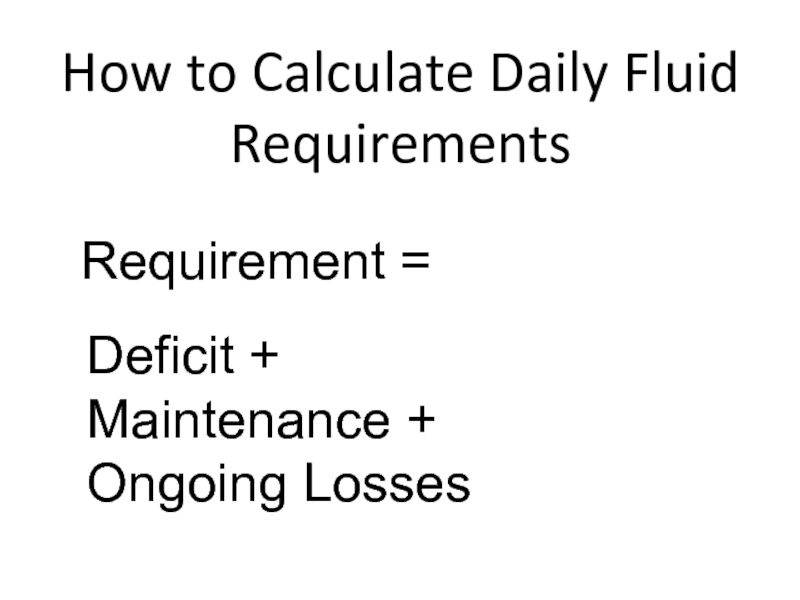
Слайд 17How to Calculate Daily Fluid Requirements
Requirement =
Deficit +
Maintenance +
Ongoing Losses
Слайд 18How to Calculate Daily Fluid Requirements?
Normal adult requires approximately 35cc/kg/d.
This assumes normal fluid loss.
- Urine
- Stool
- Insensible
Watch I/O carefully and be aware of other losses.
- Fever increases insensible loss by 200cc/day for each degree (C).
- Monitor abnormal GI loss e.g. NGT suctioning
Слайд 19
Fluid Requirements
“4,2,1” Rule
- First 10 kg= 4cc/kg/hr
-
Second 10 kg= 2cc/kg/hr
- 1cc/kg/hr thereafter
In adults remember
IVF rate = wt (kg) + 40.
- 70 + 40 = 110cc/hr
- Assumes no significant renal or cardiac disease and NPO.
This is the maintenance IVF rate, it must be adjusted for any dehydration or ongoing fluid loss.
Conversely, if the pt is taking some PO, the IVF rate must be decreased accordingly.
Daily lytes, BUN ,Cr, I/O, and if possible, weight should be monitored in patients receiving significant IVF
Слайд 20
Electrolyte Requirements
Potassium: 1 meq/kg/day
K can be added to
IV fluids. Remember this increases osm load.
20 meq/L is
a common IVF additive.
Na: 1-3 meq/kg/day
70 kg male requires 70-210 meq NaCl, 2600 cc fluid per day
Слайд 21Assessment of volume status
Hypovolaemic
(dehydrated)
Hypervolaemic
(overloaded)
Слайд 22Assessment of Volume Status
– are they dry, wet or
euvolaemic?
History
Pulse
BP incl Postural BP
Skin Turgor
Mouth Dryness
Capillary Refill
JVP
Слайд 23Assessment of Volume Status
– are they dry, wet or
euvolaemic?
Lung bases
SpO2
Body Weight
Urine Output
Fluid Balance Chart
Serum Biochem
Urine Biochem
Слайд 24Assessment of Volume Status
– are they dry, wet or
euvolaemic?
Lung bases
SpO2
Body Weight
Urine Output
Fluid Balance Chart
Serum Biochem
Urine Biochem
Слайд 25Urea:Creatinine Ratio
Normal Blood Urea = 2-7mmol/l
Normal Serum Creatinine = 40- 120umol/l
Normal Urea:Creatinine Ratio
= 60-80:1
Raised Ratio >100:1 suggests patient dehydrated. Why?
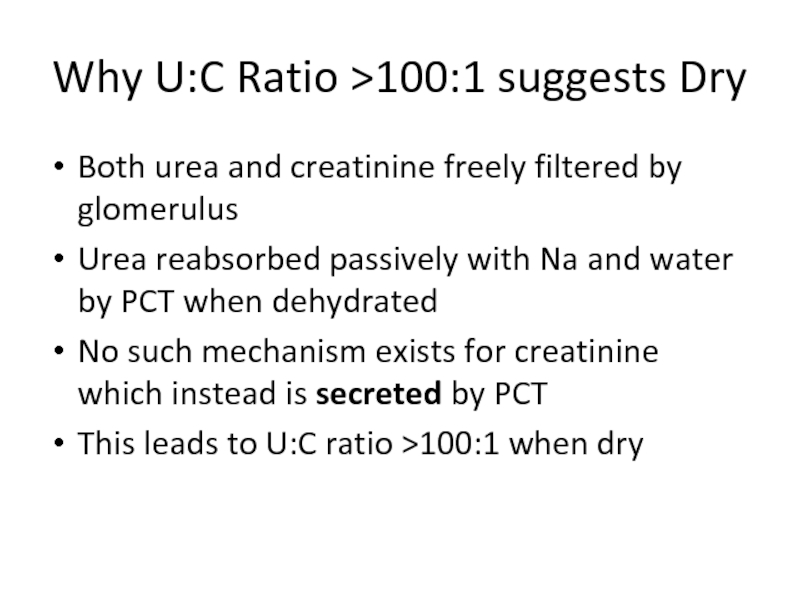
Слайд 26Why U:C Ratio >100:1 suggests Dry
Both urea and creatinine freely
filtered by glomerulus
Urea reabsorbed passively with Na and water by
PCT when dehydrated
No such mechanism exists for creatinine which instead is secreted by PCT
This leads to U:C ratio >100:1 when dry
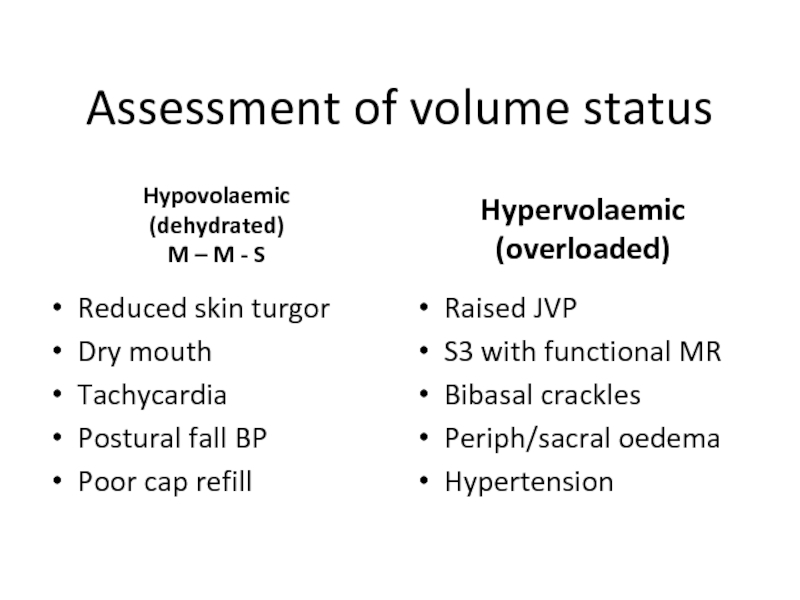
Слайд 27Assessment of volume status
Hypovolaemic
(dehydrated)
M – M - S
Reduced skin
turgor
Dry mouth
Tachycardia
Postural fall BP
Poor cap refill
Hypervolaemic
(overloaded)
Raised JVP
S3 with
functional MR
Bibasal crackles
Periph/sacral oedema
Hypertension
Слайд 28
To Determine the appropriate iv fluid you have to :
1-
Asses the volume status
maintenance , ongoing losses
2-
Determine the access
3-Select the type of fluid
4- Determine the rate
in adult rate = wt(kg)+40
Слайд 29Composition of Losses
Vomit is mostly HCl – contains very little
K and a lot of chloride (hypokalaemia is due to
renal K wasting)
Diarrhoea is more alkaline – contains quite a lot of K and no chloride
Слайд 30Two Other Things it Helps to Know when Judging Fluid
Requirements
Deficit
Maintenance
Ongoing Losses
Cardiac Status
Kidney Function
Слайд 31What Replacement Fluids are Available?
Слайд 32What Replacement Fluids are Available?
Crystalloid
Colloid
Synthetic Human
Слайд 33What Replacement Fluids are Available?
Crystalloid
Saline 0.9%
Hartmanns
Dextrose 5%
Слайд 34
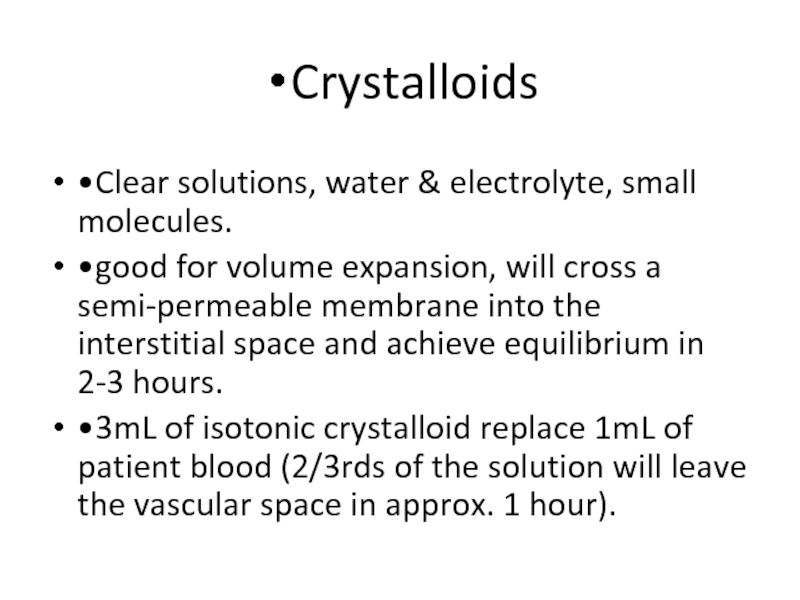
Crystalloids
•Clear solutions, water & electrolyte, small molecules.
•good for
volume expansion, will cross a semi-permeable membrane into the interstitial
space and achieve equilibrium in 2-3 hours.
•3mL of isotonic crystalloid replace 1mL of patient blood (2/3rds of the solution will leave the vascular space in approx. 1 hour).
Слайд 35
Crystalloids
•Advantages :
1-They are inexpensive.
2-Easy to store with
long shelf life.
3-Readily available with a very low incidence
of adverse reactions.
4-There are a variety of available formulations that are effective for use as replacement fluids or maintenance fluids.
•Disadvantage:
1-It takes approximately 2-3 x volume of a crystalloid to cause the same intravascular expansion as a single volume of colloid.
2-Causes peripheral edema.
3-Dilute plasma proteins.
Слайд 38
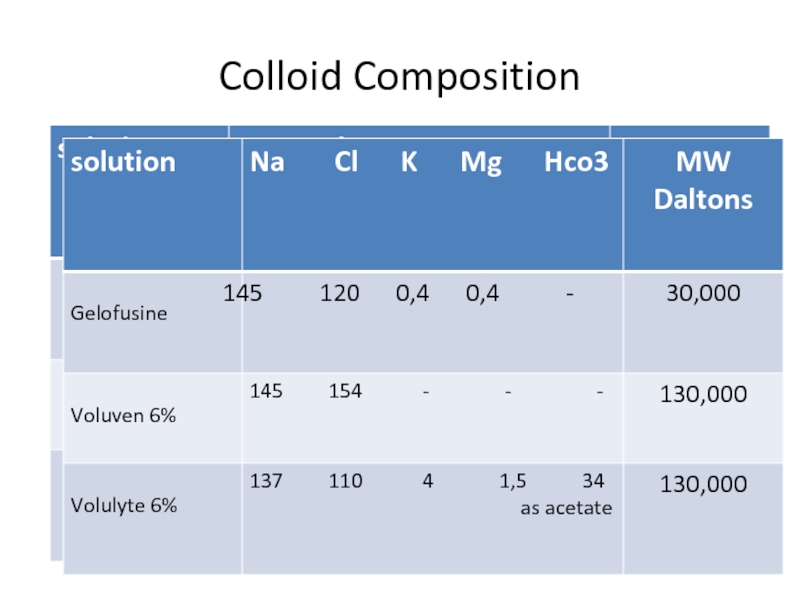
Colloids
•Solutions that contain high molecular weight proteins as well
as electrolytes, MW > 30,000 daltons.
•Unable to diffuse through
normal capillary membranes
•stay almost entirely in the intravascular space for a prolonged period of time compared to crystalloid.
Слайд 39
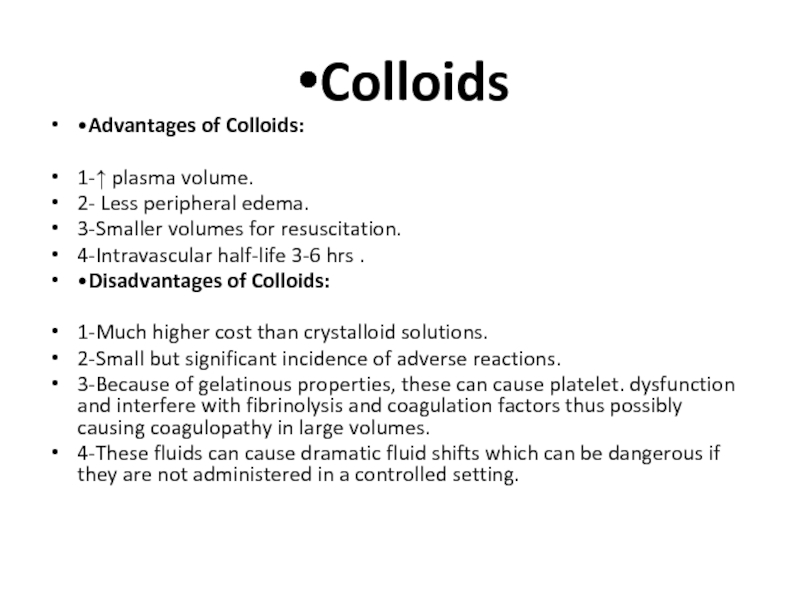
Colloids
•Advantages of Colloids:
1-↑ plasma volume.
2- Less peripheral
edema.
3-Smaller volumes for resuscitation.
4-Intravascular half-life 3-6 hrs .
•Disadvantages of Colloids:
1-Much higher cost than crystalloid solutions.
2-Small but significant incidence of adverse reactions.
3-Because of gelatinous properties, these can cause platelet. dysfunction and interfere with fibrinolysis and coagulation factors thus possibly causing coagulopathy in large volumes.
4-These fluids can cause dramatic fluid shifts which can be dangerous if they are not administered in a controlled setting.
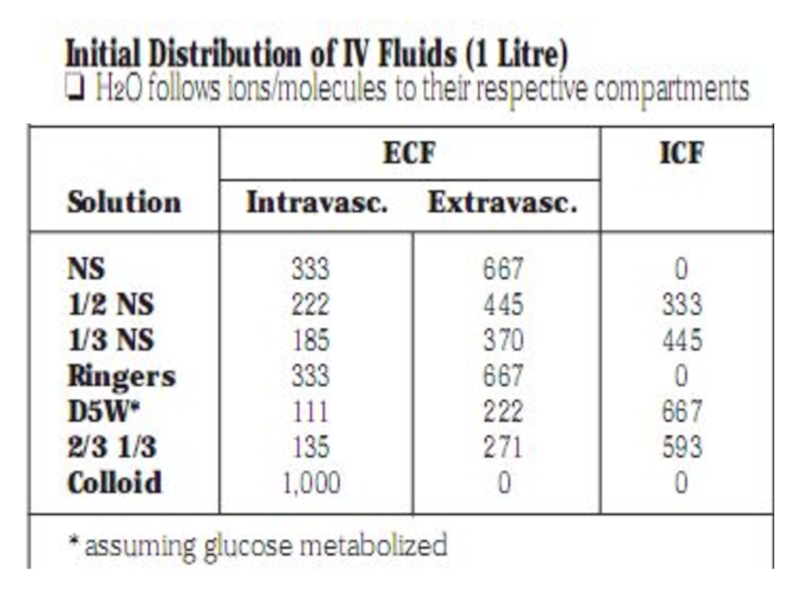
Слайд 41
Distribution of IV fluids
colloid
Saline
Dextrose
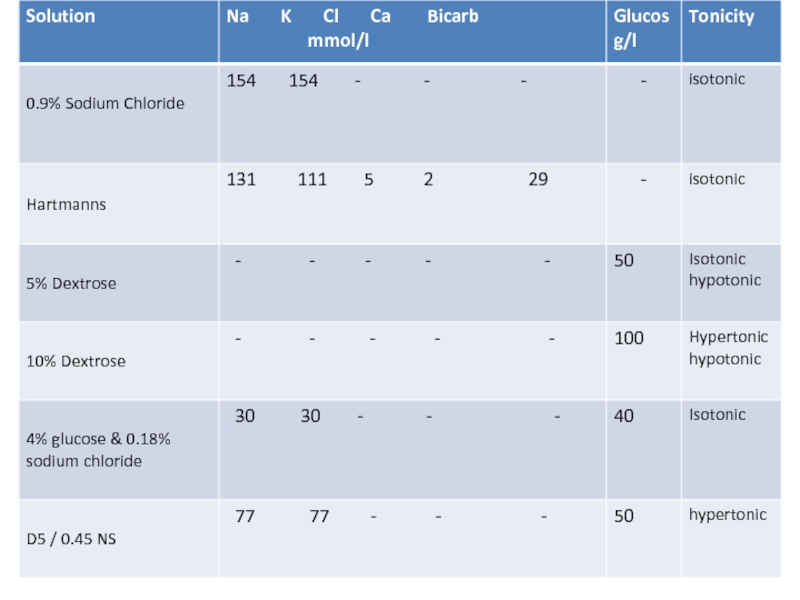
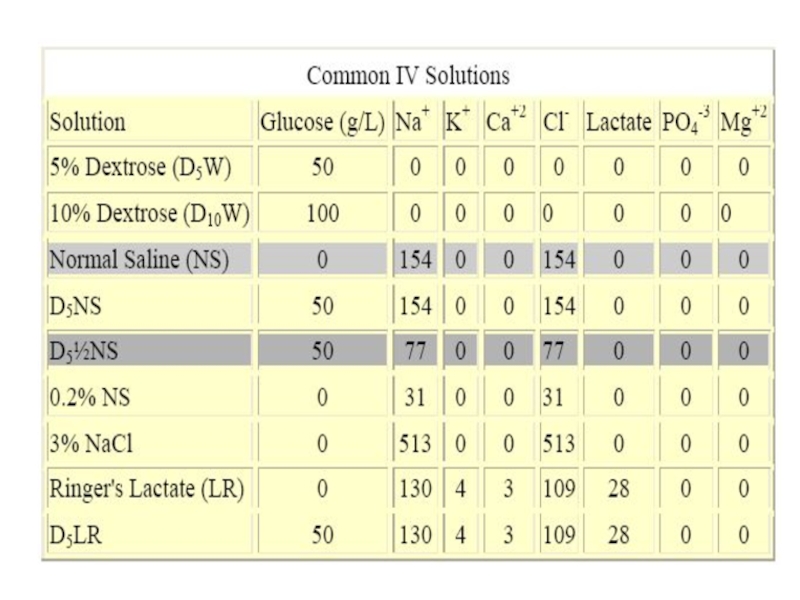
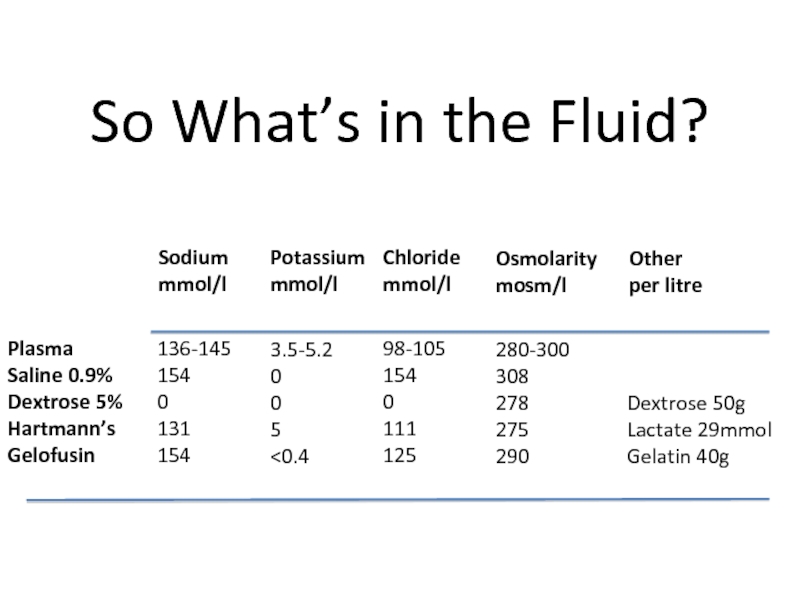
Слайд 43So What’s in the Fluid?
Sodium
mmol/l
Potassium
mmol/l
Chloride
mmol/l
Osmolarity
mosm/l
Other
per litre
Plasma
Saline 0.9%
Dextrose 5%
Hartmann’s
Gelofusin
136-145
154
0
131
154
3.5-5.2
0
0
5
Слайд 44Intravascular
5 litres
Interstitial
10 litres
Intracellular
30 litres
Dextrose 5%
Saline
Hartmanns
Gelofusine
Where does the Fluid Go?
(Volume
of Distribution)
Слайд 45Blood
Indicated to correct hypovolaemia due to blood loss
NB Aggressive correction
of anemia in critically ill patients does not improve outcome
– target Hb 70-90g/l gives same outcomes as target Hb 100-120g/l
Слайд 46
Types:
There are Three main types of IVF:
•Isotonic fluids.
•Hypotonic fluids.
•Hypertonic Fluids.
Слайд 47Isotonic
Isotonic fluids Have a total osmolality close to that
of extra cellular fluids (ECF) and don't cause RBCs to
shrink or swell.
•Isotonic have a tonicity equal to the body plasma. When administered to a normally hydrated patient, isotonic crystalloids do not cause a significant shift of water between the blood vessels and the cells. Thus, there is no (or minimal) osmosis occurring
•Helpful with patients who are hypotensive or hypovolemic.
•Examples: NS, RL, D5W(isotonic in the bag, once infused the glucose is utilized leaving just water)
Слайд 48
Hypotonic Fluids
•Less osmolarity than serum. (meaning: in general less
sodium ion concentration than serum)
•These fluids DILUTE serum thus
decreasing osmolarity.
•Water moves from the vascular compartment into the interstitial fluid compartment interstitial fluid becomes diluted osmolarity descreases water is drawn into adjacent cells.
•Caution with use because sudden fluid shifts from the intravascular space to cells can cause cardiovascular collapse and increased ICP in certain patients.
•Examples: half normal saline0.45%, 1/3 NS 0.33%, dextrose 2.5% (D2.5W)
Слайд 49
Hypertonic Fluids
•These have a higher osmolarity than serum.
•These
fluids pull fluid and sometimes electrolytes from the intracellular/interstitial compartments
into the intravascular compartments.
•Useful for stabilizing blood pressure, increasing urine output, correcting hypotonic hyponatremia and decreasing edema.
•These can be dangerous in the setting of cell dehydration.
•Examples: 5% dextrose in 0.9% NaCl (D5NS),D5RL,D5 ½ NS, 3% NaCl,10% dextrose in water (D10W)
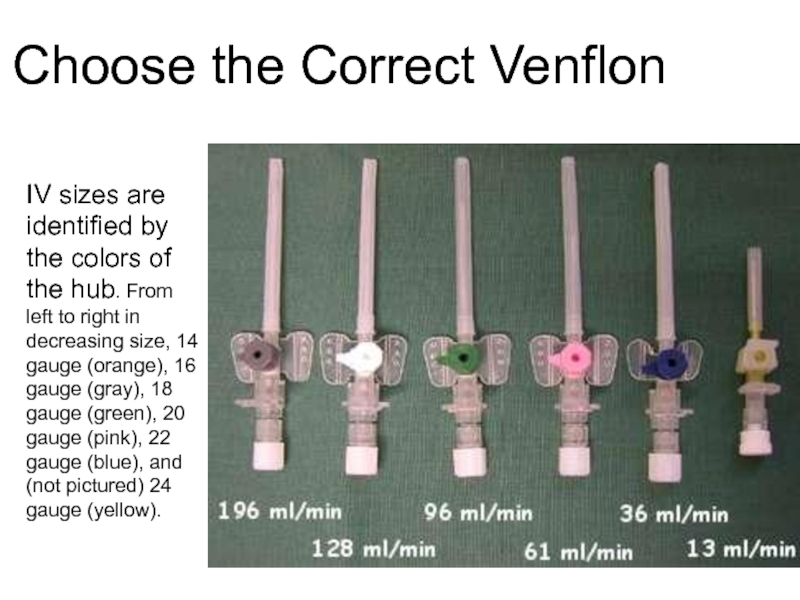
Слайд 50Choose the Correct Venflon
IV sizes are identified by the colors
of the hub. From left to right in decreasing size,
14 gauge (orange), 16 gauge (gray), 18 gauge (green), 20 gauge (pink), 22 gauge (blue), and (not pictured) 24 gauge (yellow).
Слайд 51
Theory of Fluid Flow
•Flow = diameter4 / length
–Larger
catheters = higher flow
–Short catheters = somewhat higher flow
•Other factors affecting flow
–Tubing length
–Size of Vein
–Temperature and viscocity of fluid
•Warm fluids flow better than cold
Слайд 52
There are 4 types of patients:
1-Hypovolemic Patient:
Pneumonia, Sepsis,
Hemorrhage,Gastroenteritis.
2-Hypervolemic Patient:
CHF, renal failure, cirrhosis.
3-NPO Patient, surgical
patient, euvolemic:
Awaiting surgery, unsafe swallow.
4-Eating/drinking normally.
Слайд 53
Hypovolemic patients:
-True volume depletion (hypovolemia):
•usually refers to a
state of combined salt and water loss exceeding intake which
leads to ECF volume contraction.
•ECF volume contraction is manifested as a decreased plasma volume and hypotension.
•Signs of intravascular volume contraction include decreased jugular venous pressure, postural hypotension, and postural tachycardia.
•Larger and more acute fluid losses lead to hypovolemic shock and manifest as hypotension, tachycardia, peripheral vasoconstriction, & hypoperfusion.
Слайд 54
Treatment of Hypovolemia:
•The goals of treatment is to restore
normovolemia with fluid similar in composition to that lost and
replace ongoing losses.
•Mild volume losses can be corrected via oral rout.
•More severe hypovolemia requires IV therapy.
•Isotonic or Normal Saline (0.9%NaCl) is the choice in normonatremic and mildly hyponatremic patients and should be administered initially in patients with hypotension or shock.
Слайд 55
In Hypernatremic patient, there is a proportionately greater deficit of
water than sodium, therefore to correct this patient you will
use a Hypotonic solution like ½ NS (0.45% NaCl) or D5W. For The Hypernatremic Patient: STOP THE ONGOING LOSS!
To Calculate Water Deficit:
Estimate TBW: 50-60% body weight (KG) depending on body composition (W vs M)
Calculate Free-Water deficit: [(Na+ - 140)/140] x TBW
Administer deficit over 48-72 hrs
Insensible Losses:
Approximately 10mL/kg per day: less if ventilated, more if febrile.
Слайд 56
Hypervolemic Patient:
-Avoid additional IVF
-Maintain access IV access with Hep-Lock
( A small tube connected to a catheter in a
vein in the arm for easy access. It is an alternative in some cases to using an IV. Its called heplock because of the order of medicating using it which is saline, medication, saline then heparin)
Слайд 57
NPO Patient now euvolemic
-Administer maintenance fluids. Goal is to
maintain input of fluids to keep up with ongoing losses
and normal fluid needs
-For average adult NPO for more than 6-12 hours, consider D5 1/2NS at 75-100cc/hr
-Constantly reassess, at least 2x day or with any change
-Don’t give fluids blindly ie: if the patient is pre-procedure but has history of CHF, be CAREFUL!
-The reason for giving dextrose (D5) is to prevent catabolism
-Normal PO Intake:
-No need for fluids if they are taking PO without problems! Avoid IVF
Слайд 58
Post-operative patients:
- Pain and narcotics can be powerful stimulants
of inappropriate ADH secretion (SIADH)
- Giving hypotonic fluids in
this setting can (but usually does not) cause dangerous hyponatremia.
- This makes 0.9 % saline a safer fluid but realize that it will also deliver free water in the setting of SIADH. (stay tuned for a future lecture).
Слайд 59
Examples
• 35 y/o female NPO for elective lap
chole. Afebrile HR 72 BP 120/80 Wt 85 kg. Na
140 K 4.0. Fluid Orders:
•D5 0.45% saline with 20meq KCl @ 125 cc/hr.
Слайд 60
Examples
• 89 y/o nursing home pt. admitted for diverticulitis.
T 38.0 HR 90 BP 145/85. wt 70 kg Na:
140, K: 3.7. Not eating. Fluid Orders:
• Basal needs 70 + 40 = 110cc/hr
•Additional loss from fever = approx. 10 cc/hr
• Total rate = 120 cc/hr: IVF?
•(D5) 0.45% saline with 20 meq KCl
Слайд 61
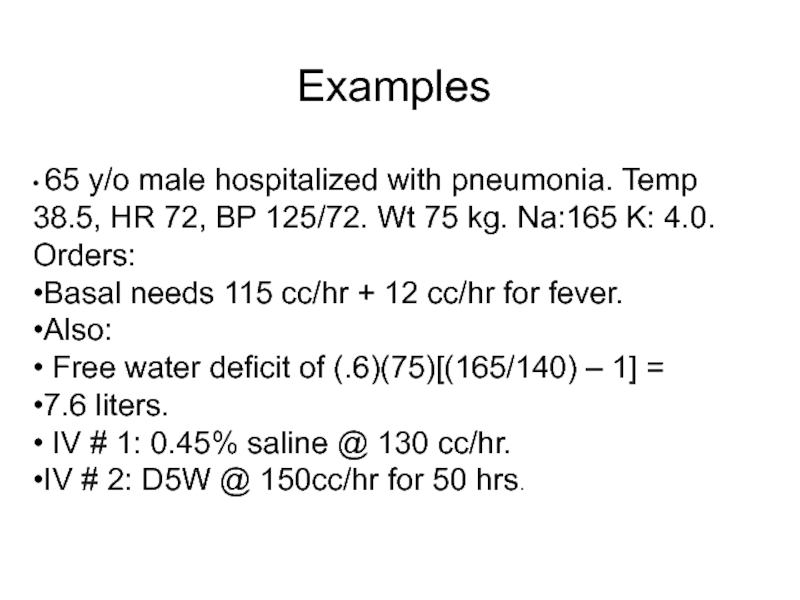
Examples
• 65 y/o male hospitalized with pneumonia. Temp 38.5,
HR 72, BP 125/72. Wt 75 kg. Na:165 K: 4.0.
Orders:
•Basal needs 115 cc/hr + 12 cc/hr for fever.
•Also:
• Free water deficit of (.6)(75)[(165/140) – 1] =
•7.6 liters.
• IV # 1: 0.45% saline @ 130 cc/hr.
•IV # 2: D5W @ 150cc/hr for 50 hrs.