Слайд 1мараках марван якин ножи
Department of Dermatovenerology
Piodermitis
Слайд 2Piodermitis
Lection 7
Pyodermas.
Scabies.
Слайд 3Piodermitis
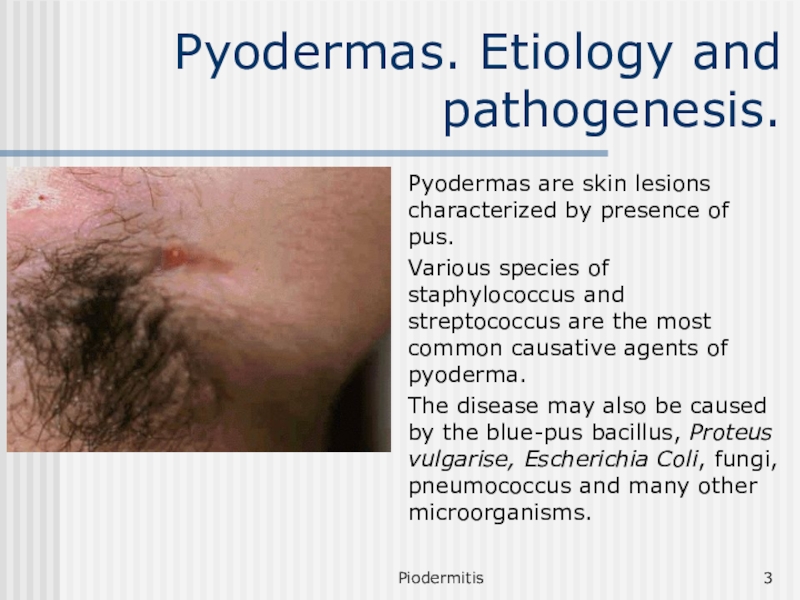
Pyodermas. Etiology and pathogenesis.
Pyodermas are skin lesions characterized by presence
of pus.
Various species of staphylococcus and streptococcus are the most
common causative agents of pyoderma.
The disease may also be caused by the blue-pus bacillus, Proteus vulgarise, Escherichia Coli, fungi, pneumococcus and many other microorganisms.
Слайд 4Piodermitis
The contributing factors
Superficial skin injuries (microtraumas), such as cuts, excoriations,
scratches, superficial burns, etc.
Soiling of the skin (occupational soiling with
coal, lime, cement etc. and soiling because of faulty hygienic care)
Over-cooling or overheating of the body
The endogenic factors are just as diverse, note should be made of disorders of carbohydrate metabolism, endocrine disorders, functional disorders of the nervous system, hypovitaminosis, acute and chronic diseases, and hereditary factors, weakening of immune of immune defense mechanisms.
Слайд 5Piodermitis
Classification
Pyodermas are classified by several items.
By Etiology
Staphylococcal
Streptococcal
Mixed
By depth of the
localization
Superficial
Deep
Слайд 6Piodermitis
Classification
By time of appearance of the lesions
Acute
Chronic
According to the course
of disease
Primary
Secondary
Слайд 7Piodermitis
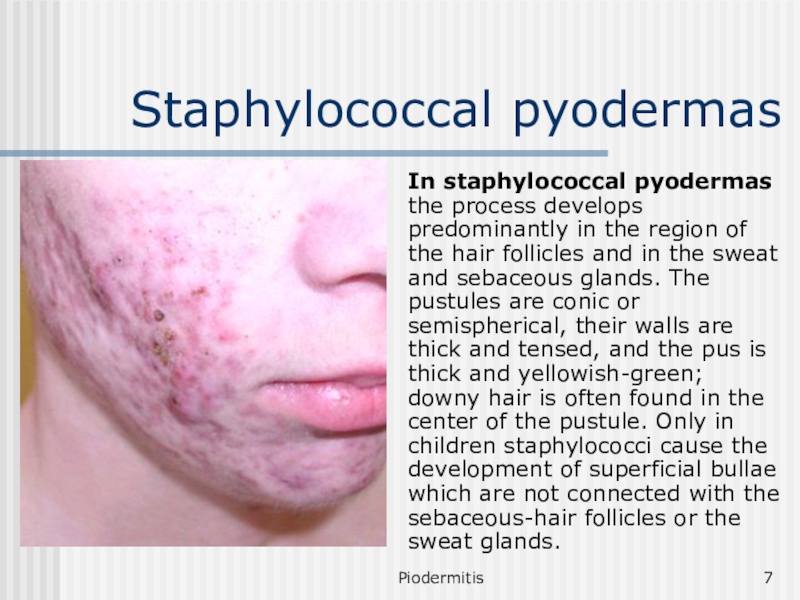
Staphylococcal pyodermas
In staphylococcal pyodermas the process develops predominantly in the
region of the hair follicles and in the sweat and
sebaceous glands. The pustules are conic or semispherical, their walls are thick and tensed, and the pus is thick and yellowish-green; downy hair is often found in the center of the pustule. Only in children staphylococci cause the development of superficial bullae which are not connected with the sebaceous-hair follicles or the sweat glands.
Слайд 8Piodermitis
Staphylococcal pyodermas
Ostial folliculitis (Bockhart’s impetigo)
Folliculitis,
Sycosis,
Furuncle,
Carbuncle,
Hydradenitis.
Слайд 9Piodermitis
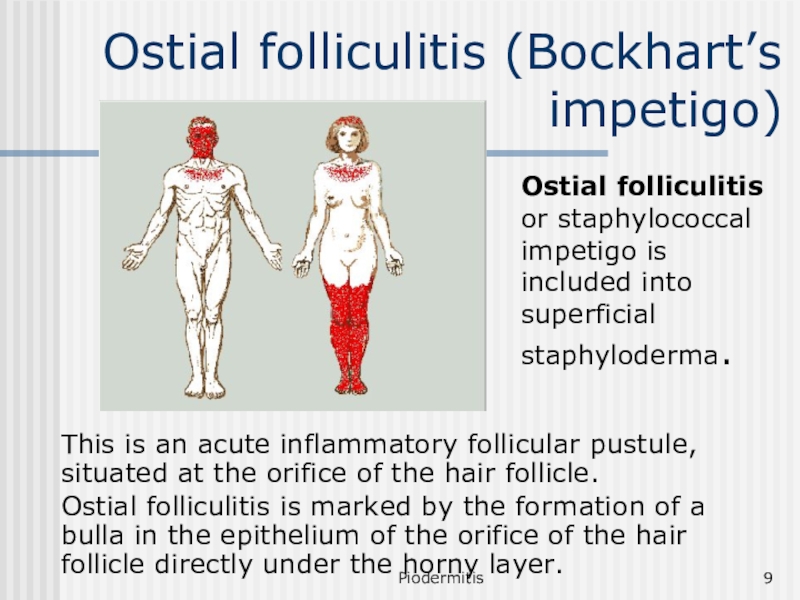
Ostial folliculitis (Bockhart’s impetigo)
Ostial folliculitis or staphylococcal impetigo is included
into superficial staphyloderma.
This is an acute inflammatory follicular pustule,
situated at the orifice of the hair follicle.
Ostial folliculitis is marked by the formation of a bulla in the epithelium of the orifice of the hair follicle directly under the horny layer.
Слайд 10Piodermitis
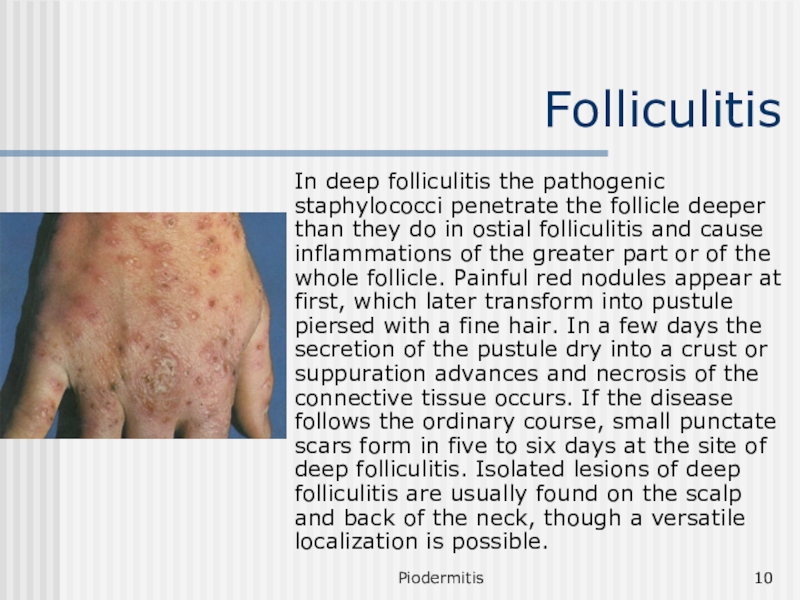
Folliculitis
In deep folliculitis the pathogenic staphylococci penetrate the follicle deeper
than they do in ostial folliculitis and cause inflammations of
the greater part or of the whole follicle. Painful red nodules appear at first, which later transform into pustule piersed with a fine hair. In a few days the secretion of the pustule dry into a crust or suppuration advances and necrosis of the connective tissue occurs. If the disease follows the ordinary course, small punctate scars form in five to six days at the site of deep folliculitis. Isolated lesions of deep folliculitis are usually found on the scalp and back of the neck, though a versatile localization is possible.
Слайд 11Piodermitis
Sycosis
Staphylogenic sycosis is a chronic, relapsing infection of hair follicles.
Males are infected more often.
At the onset of the
disease, a few lesions of ostial folliculitis appear on a relatively circumscribed skin area, which tend to spread to larger and larger areas. An inflammatory infiltrate forms around the lesions, as a result of which the affected area thickens and turns bluish-red and is sometimes painful. Involvement of new follicles in the process leads to slow growth of the focus of affection in which there may be a large number of inflamed follicular orifices forming a conglomerate of pustules. After the top of the pustules opens, the pus dries up into dirty-yellow crusts which stick to the hairs.
Слайд 12Piodermitis
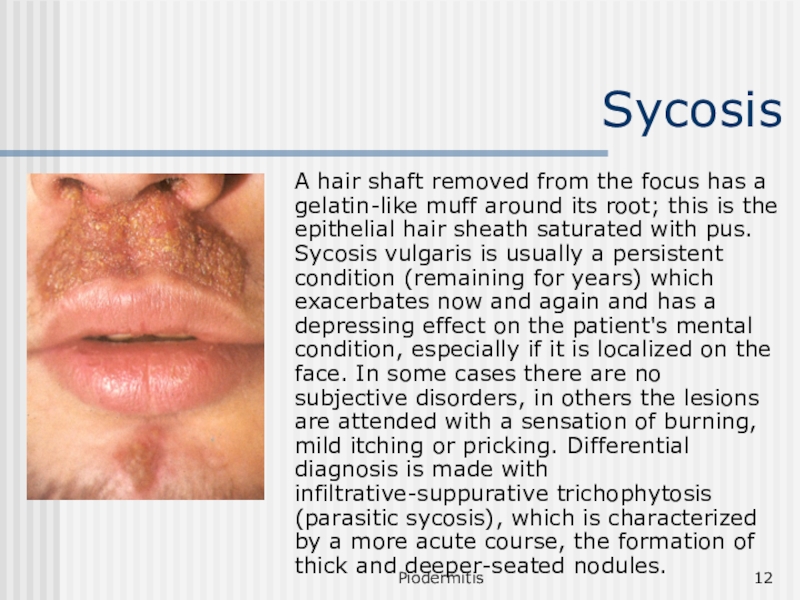
Sycosis
A hair shaft removed from the focus has a gelatin-like
muff around its root; this is the epithelial hair sheath
saturated with pus. Sycosis vulgaris is usually a persistent condition (remaining for years) which exacerbates now and again and has a depressing effect on the patient's mental condition, especially if it is localized on the face. In some cases there are no subjective disorders, in others the lesions are attended with a sensation of burning, mild itching or pricking. Differential diagnosis is made with infiltrative-suppurative trichophytosis (parasitic sycosis), which is characterized by a more acute course, the formation of thick and deeper-seated nodules.
Слайд 13Piodermitis
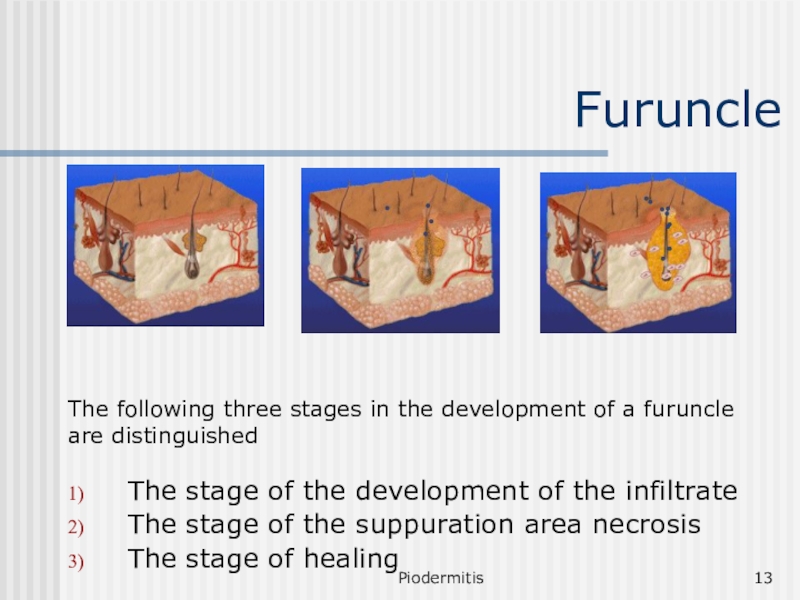
Furuncle
The stage of the development of the infiltrate
The stage of
the suppuration area necrosis
The stage of healing
The following three stages
in the development of a furuncle are distinguished
Слайд 14Piodermitis
Furuncle
A hard, elevated, bright-red infiltrate first forms around the hair
follicle. The infiltrate is not sharply circumscribed and is attended
with a pricking sensation or mild pain. The infiltrate acquires gradually the form of a firm tumor, which grows along the periphery and becomes more painful; there is swelling of the surrounding tissues (the swelling in the region of the cheeks, eyelids, and lips may be sharply pronounced). The second stage sets in on the third or fourth day: the furuncle grows to 1-3 cm in diameter and a pyo-necrotic core with a pustule on its surface forms in the center.
Слайд 15Piodermitis
Furuncle
The furuncle takes the shape of a conic tumor with
smooth, lusty blue skin. The pain is very severe in
this period, body temperature may rise to 37-38° C, and symptoms of toxicosis may develop (general indisposition, malaise, headache, etc.).
The top of the pustule opens spontaneously or is opened artificially and pus, sometimes with an admixture of blood, is discharged from the furuncle after which a yellowish-green necrotic 'plug' (necrotic core) comes out.
Слайд 16Piodermitis
Furuncle
After removal or rejection of the core, swelling, infiltration, and
pain subside, and the remaining crater of the furuncle is
filled with granulations, which are replaced by a scar in two to three days. The scar is bluish-red at first, then gradually turns white and is sometimes hardly visible. The developmental cycle of a furuncle commonly lasts eight to ten days.
Слайд 17Piodermitis
Furunculosis
Furunculosis is a condition in which there is recurrent eruption
of furuncles. Furunculosis may be localized (on a circumscribed skin
area) or diffuse, disseminated. According to the course, furunculosis may be only chronic (a small number of furuncles appearing at short intervals or uninterruptedly for months).
Слайд 18Piodermitis
Furuncle
Treatment depends on the stage of the pathological process.
In
stage of infiltration physiotherapy is placed
In stage of the suppuration
area necrosis ichthyol troche is placed.
In stage of healing - after opening - dressing with hypertonic solution is put on and keratoplastic unguentum is used.
Слайд 19Piodermitis
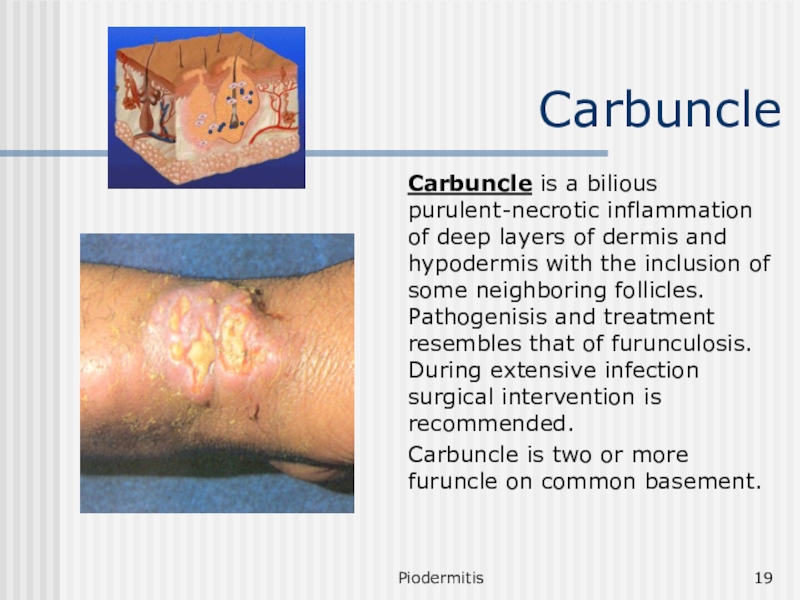
Carbuncle
Carbuncle is a bilious purulent-necrotic inflammation of deep layers of
dermis and hypodermis with the inclusion of some neighboring follicles.
Pathogenisis and treatment resembles that of furunculosis. During extensive infection surgical intervention is recommended.
Carbuncle is two or more furuncle on common basement.
Слайд 20Piodermitis
Hydradenitis
Hydradenitis is a purulent inflammation of apocrine sweat glands. The
main role in pathogenesis is played by general weakness of
the organism, increased sweating, deviation of sweat reaction towards the basic side, microtraumas, endocrinopathy.
At the onset of the disease, solitary small hard mound-like nodes are palpated in the thickness of the dermis or hypoderm. The patient experiences mild itching or pain at this time. The nodes grow rapidly in size, adhere to the skin, become pear-shaped and protrude like nipples and resemble bitch's udder.
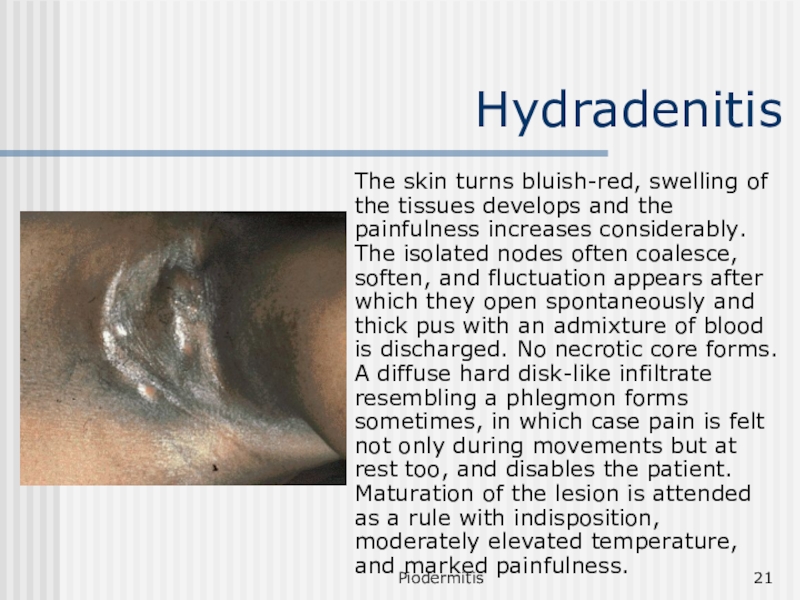
Слайд 21Piodermitis
Hydradenitis
The skin turns bluish-red, swelling of the tissues develops and
the painfulness increases considerably. The isolated nodes often coalesce, soften,
and fluctuation appears after which they open spontaneously and thick pus with an admixture of blood is discharged. No necrotic core forms. A diffuse hard disk-like infiltrate resembling a phlegmon forms sometimes, in which case pain is felt not only during movements but at rest too, and disables the patient. Maturation of the lesion is attended as a rule with indisposition, moderately elevated temperature, and marked painfulness.
Слайд 22Piodermitis
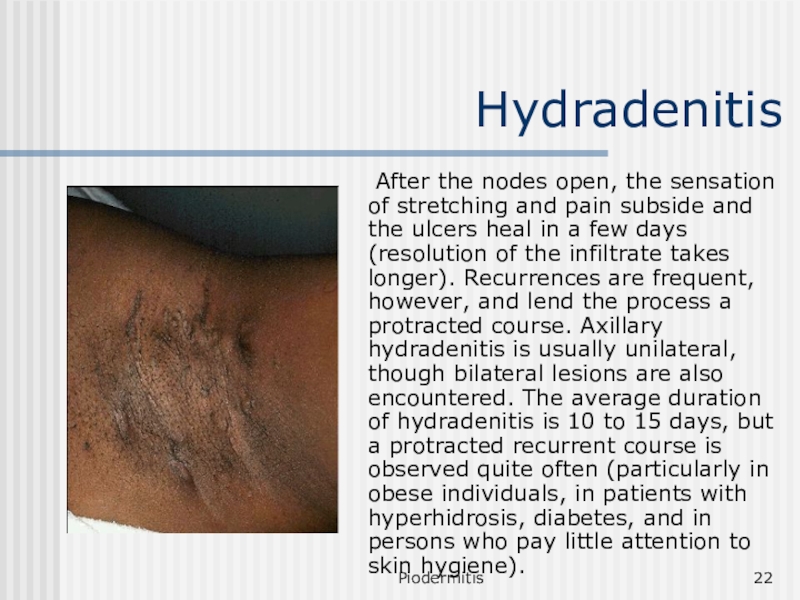
Hydradenitis
After the nodes open, the sensation of stretching and
pain subside and the ulcers heal in a few days
(resolution of the infiltrate takes longer). Recurrences are frequent, however, and lend the process a protracted course. Axillary hydradenitis is usually unilateral, though bilateral lesions are also encountered. The average duration of hydradenitis is 10 to 15 days, but a protracted recurrent course is observed quite often (particularly in obese individuals, in patients with hyperhidrosis, diabetes, and in persons who pay little attention to skin hygiene).
Слайд 23Piodermitis
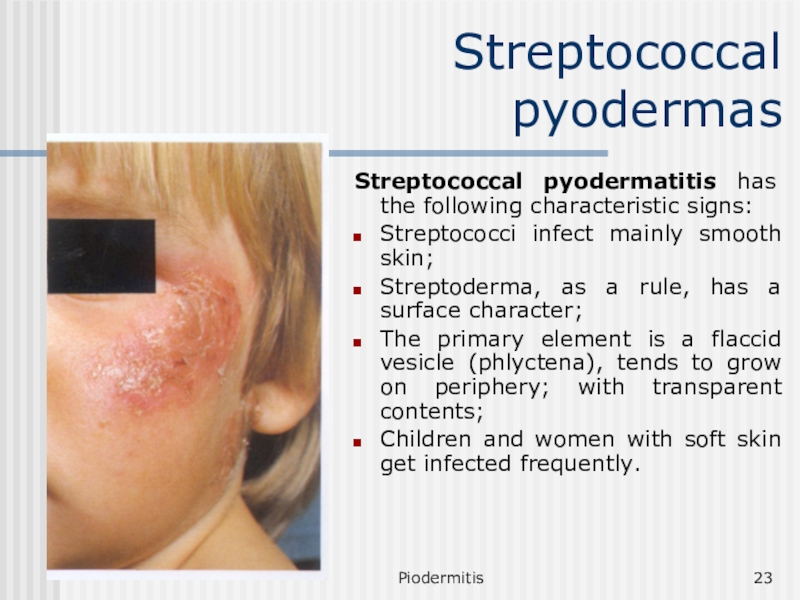
Streptococcal pyodermas
Streptococcal pyodermatitis has the following characteristic signs:
Streptococci infect mainly
smooth skin;
Streptoderma, as a rule, has a surface character;
The
primary element is a flaccid vesicle (phlyctena), tends to grow on periphery; with transparent contents;
Children and women with soft skin get infected frequently.
Слайд 24Piodermitis
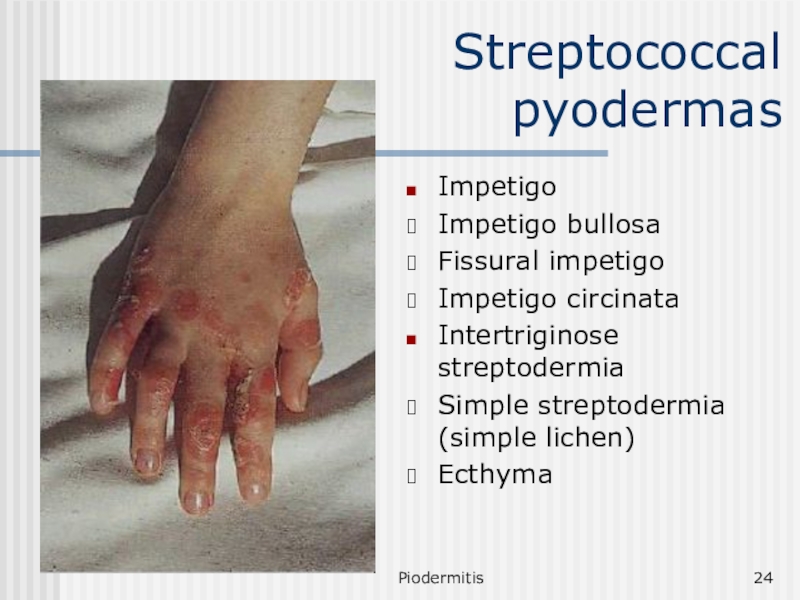
Streptococcal pyodermas
Impetigo
Impetigo bullosa
Fissural impetigo
Impetigo circinata
Intertriginose streptodermia
Simple streptodermia (simple lichen)
Ecthyma
Слайд 25Piodermitis
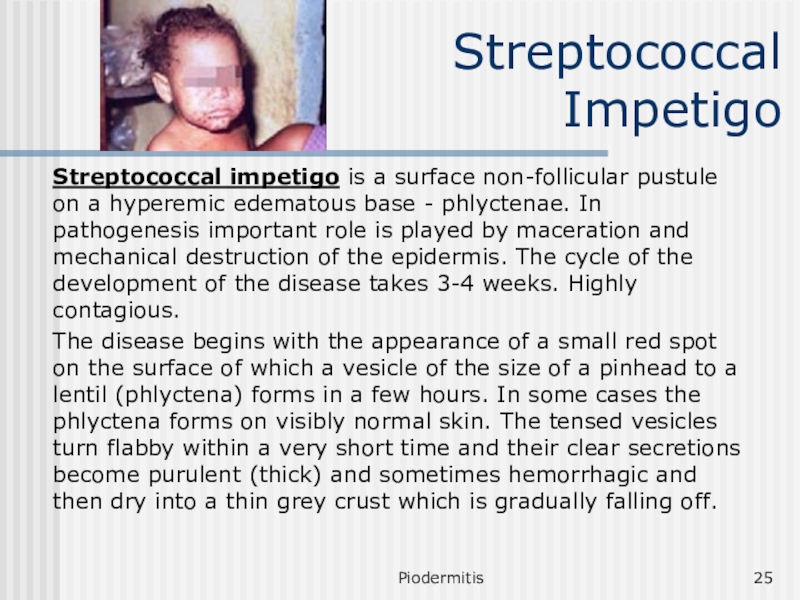
Streptococcal Impetigo
Streptococcal impetigo is a surface non-follicular pustule on a
hyperemic edematous base - phlyctenae. In pathogenesis important role is
played by maceration and mechanical destruction of the epidermis. The cycle of the development of the disease takes 3-4 weeks. Highly contagious.
The disease begins with the appearance of a small red spot on the surface of which a vesicle of the size of a pinhead to a lentil (phlyctena) forms in a few hours. In some cases the phlyctena forms on visibly normal skin. The tensed vesicles turn flabby within a very short time and their clear secretions become purulent (thick) and sometimes hemorrhagic and then dry into a thin grey crust which is gradually falling off.
Слайд 26Piodermitis
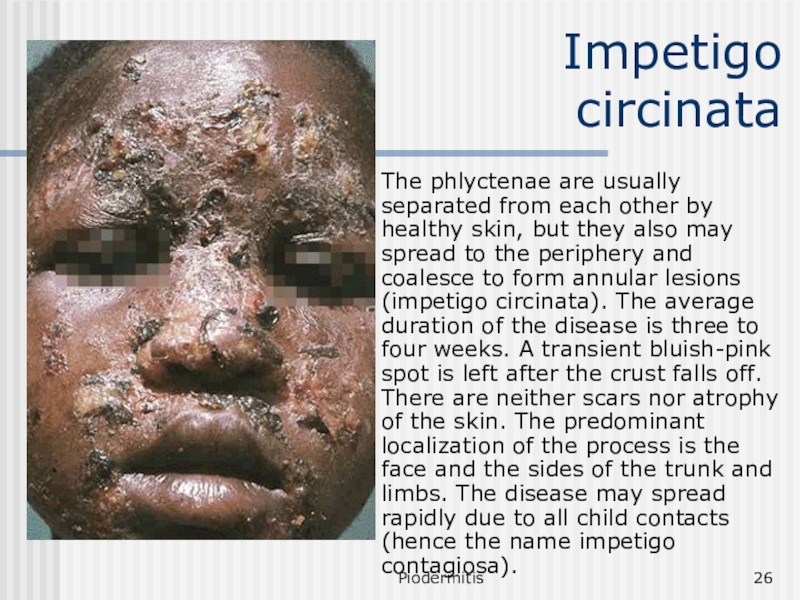
Impetigo circinata
The phlyctenae are usually separated from each other by
healthy skin, but they also may spread to the periphery
and coalesce to form annular lesions (impetigo circinata). The average duration of the disease is three to four weeks. A transient bluish-pink spot is left after the crust falls off. There are neither scars nor atrophy of the skin. The predominant localization of the process is the face and the sides of the trunk and limbs. The disease may spread rapidly due to all child contacts (hence the name impetigo contagiosa).
Слайд 27Piodermitis
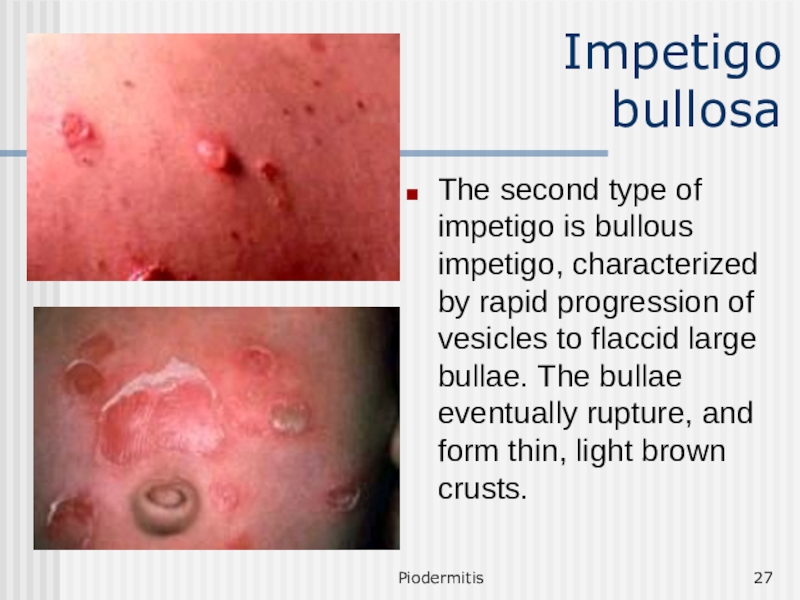
Impetigo bullosa
The second type of impetigo is bullous impetigo,
characterized by rapid progression of vesicles to flaccid large bullae.
The bullae eventually rupture, and form thin, light brown crusts.
Слайд 28Piodermitis
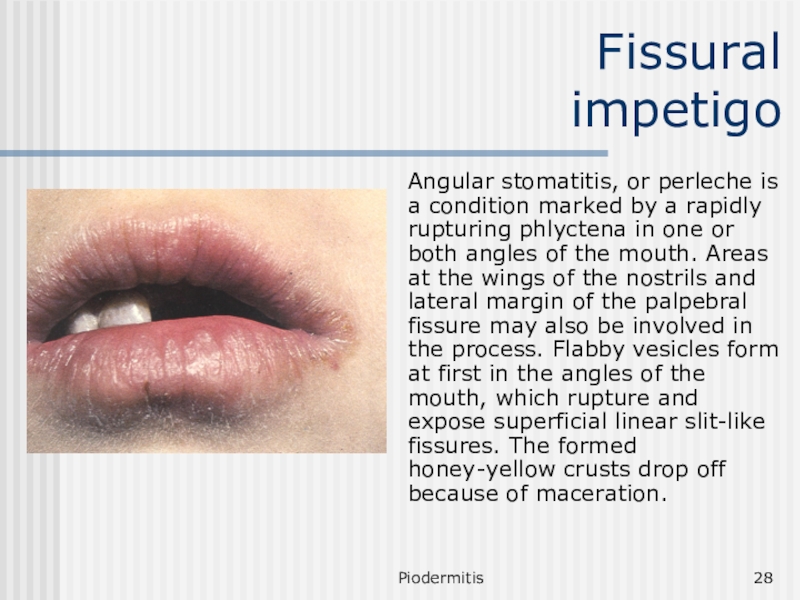
Fissural impetigo
Angular stomatitis, or perleche is a condition marked
by a rapidly rupturing phlyctena in one or both angles
of the mouth. Areas at the wings of the nostrils and lateral margin of the palpebral fissure may also be involved in the process. Flabby vesicles form at first in the angles of the mouth, which rupture and expose superficial linear slit-like fissures. The formed honey-yellow crusts drop off because of maceration.
Слайд 29Piodermitis
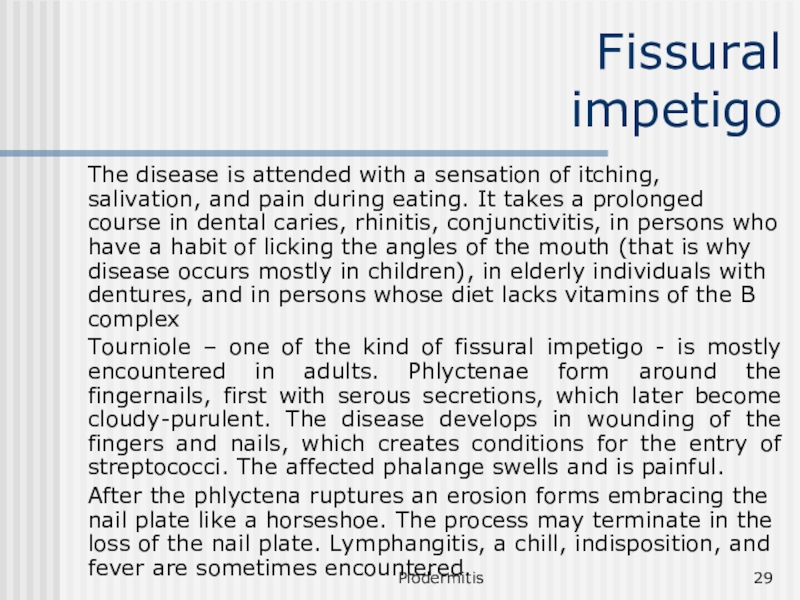
Fissural impetigo
The disease is attended with a sensation of itching,
salivation, and pain during eating. It takes a prolonged course
in dental caries, rhinitis, conjunctivitis, in persons who have a habit of licking the angles of the mouth (that is why disease occurs mostly in children), in elderly individuals with dentures, and in persons whose diet lacks vitamins of the B complex
Tourniole – one of the kind of fissural impetigo - is mostly encountered in adults. Phlyctenae form around the fingernails, first with serous secretions, which later become cloudy-purulent. The disease develops in wounding of the fingers and nails, which creates conditions for the entry of streptococci. The affected phalange swells and is painful.
After the phlyctena ruptures an erosion forms embracing the nail plate like a horseshoe. The process may terminate in the loss of the nail plate. Lymphangitis, a chill, indisposition, and fever are sometimes encountered.
Слайд 30Piodermitis
Simple streptodermia
Simple streptodermia is considered to be a dry variety
of impetigo streptogenes. It is particularly widespread in children and
is characterized by round or oval, strictly circumscribed whitish or pink foci, which are abundantly covered with small scales. The foci are especially conspicuous in individuals with pigmented skin. The disease may be cured by exposure to sunrays, but the affected areas are tanned weakly so that mottling of the skin surface occurs. The favored localization is the skin around the mouth, the cheeks, and the region of the lower jaw, sometimes the lesions occur on the skin of the trunk and limbs.
The disease usually occurs in spring or autumn. In children's collectives pityriasis simplex may acquire the character of epidemics. There is sometimes a sensation of mild itching.
Слайд 31Piodermitis
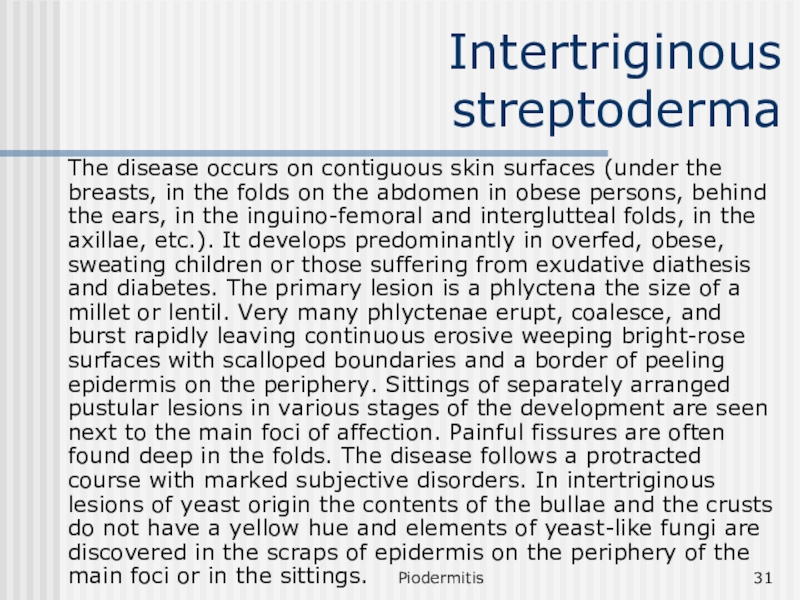
Intertriginous streptoderma
The disease occurs on contiguous skin surfaces (under
the breasts, in the folds on the abdomen in obese
persons, behind the ears, in the inguino-femoral and interglutteal folds, in the axillae, etc.). It develops predominantly in overfed, obese, sweating children or those suffering from exudative diathesis and diabetes. The primary lesion is a phlyctena the size of a millet or lentil. Very many phlyctenae erupt, coalesce, and burst rapidly leaving continuous erosive weeping bright-rose surfaces with scalloped boundaries and a border of peeling epidermis on the periphery. Sittings of separately arranged pustular lesions in various stages of the development are seen next to the main foci of affection. Painful fissures are often found deep in the folds. The disease follows a protracted course with marked subjective disorders. In intertriginous lesions of yeast origin the contents of the bullae and the crusts do not have a yellow hue and elements of yeast-like fungi are discovered in the scraps of epidermis on the periphery of the main foci or in the sittings.
Слайд 32Piodermitis
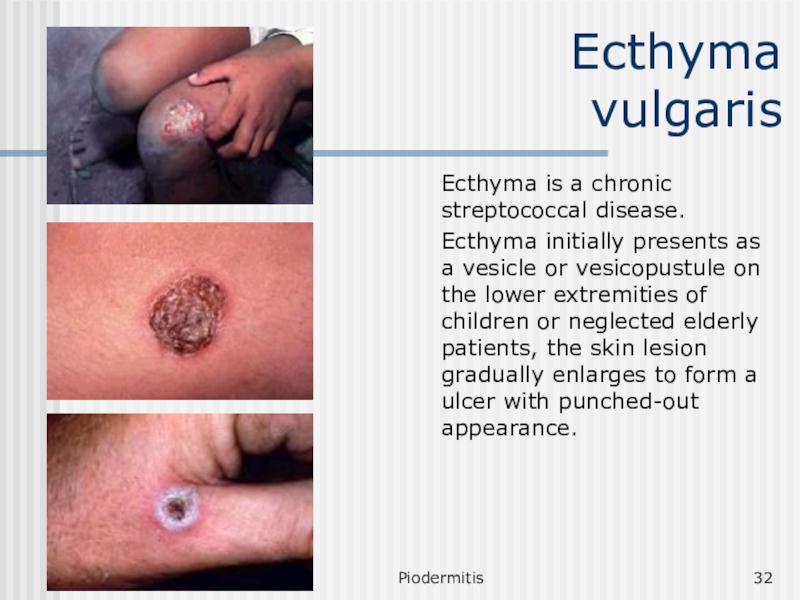
Ecthyma vulgaris
Ecthyma is a chronic streptococcal disease.
Ecthyma initially presents
as a vesicle or vesicopustule on the lower extremities of
children or neglected elderly patients, the skin lesion gradually enlarges to form a ulcer with punched-out appearance.
Слайд 33Piodermitis
Mixed strepto-staphylococcal pyodermatitis. Classification
Impetigo vulgaris
Epidemic pemphigus of the newborn
Chancriform pyoderma
Chronic ulcerous and ulcero-vegetative pyoderma
Granuloma pyogenicum (batriomycoma)
Слайд 34Piodermitis
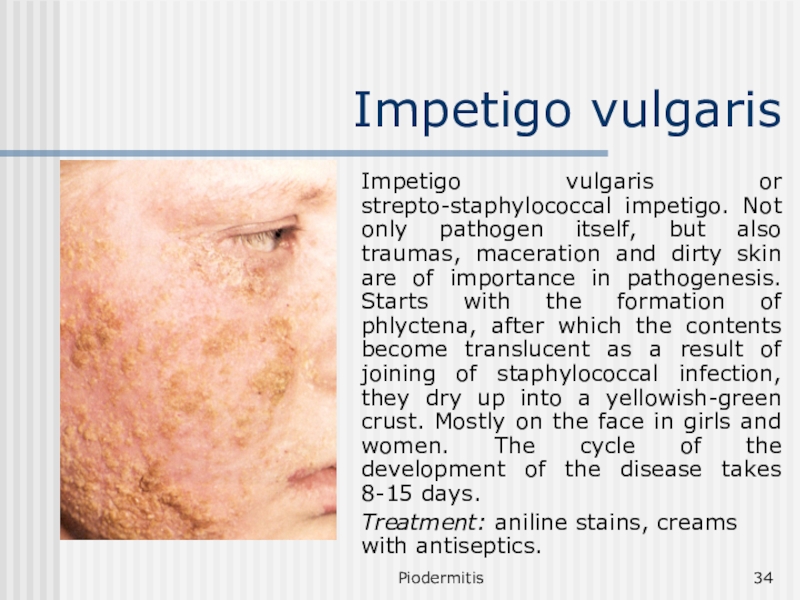
Impetigo vulgaris
Impetigo vulgaris or strepto-staphylococcal impetigo. Not only pathogen itself,
but also traumas, maceration and dirty skin are of importance
in pathogenesis. Starts with the formation of phlyctena, after which the contents become translucent as a result of joining of staphylococcal infection, they dry up into a yellowish-green crust. Mostly on the face in girls and women. The cycle of the development of the disease takes 8-15 days.
Treatment: aniline stains, creams with antiseptics.
Слайд 35Piodermitis
Epidemic pemphigus of the newborn
It is an acute contagious disease
of staphylococcal nature. Pathogenesis: the main pathogenic factor is sensitivity
of the skin to infections, prematurity, pregnancy toxicosis, birth injury. The source of infection is often the medical staff, mother and the patients themselves.
Clinical features. Emergence of small vesicles with thin tensed cover and serous-yellow contents, tendency towards fusion and formation of large vesicles. Fever is possible. Vesicles are converted into pustules, open, erosion slowly epithilizes. It is necessary to differentiate epidemic pemphigus form syphilitic pemphigus. The latter arises on palms and soles, on an infiltrated base, characterized by the presence of T. palladium in the contents of the vesicles, positive compliment fixation test (CFT) in child and mother.
Treatment. Antibiotics, antistaphylococcal serum, transfusion of plasma, locally: aniline stains, creams with antibodies.
Слайд 36Piodermitis
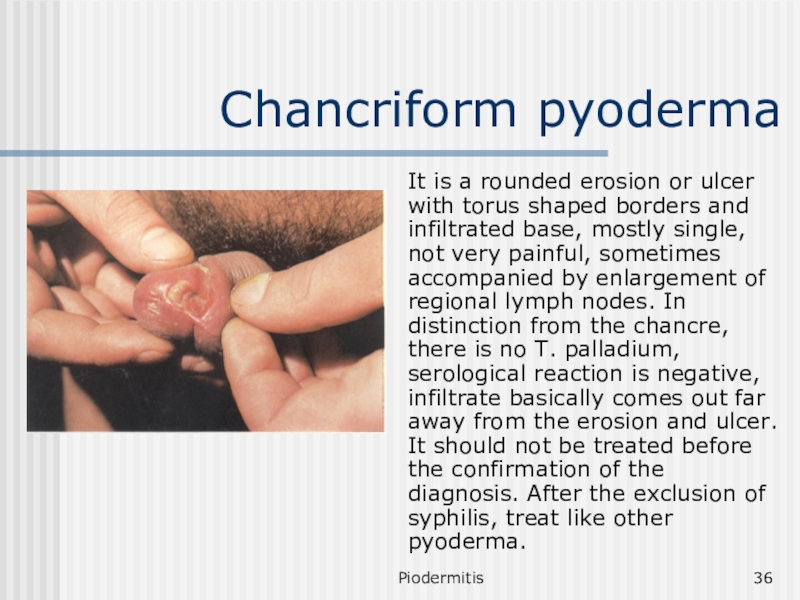
Chancriform pyoderma
It is a rounded erosion or ulcer with torus
shaped borders and infiltrated base, mostly single, not very painful,
sometimes accompanied by enlargement of regional lymph nodes. In distinction from the chancre, there is no T. palladium, serological reaction is negative, infiltrate basically comes out far away from the erosion and ulcer. It should not be treated before the confirmation of the diagnosis. After the exclusion of syphilis, treat like other pyoderma.
Слайд 37Piodermitis
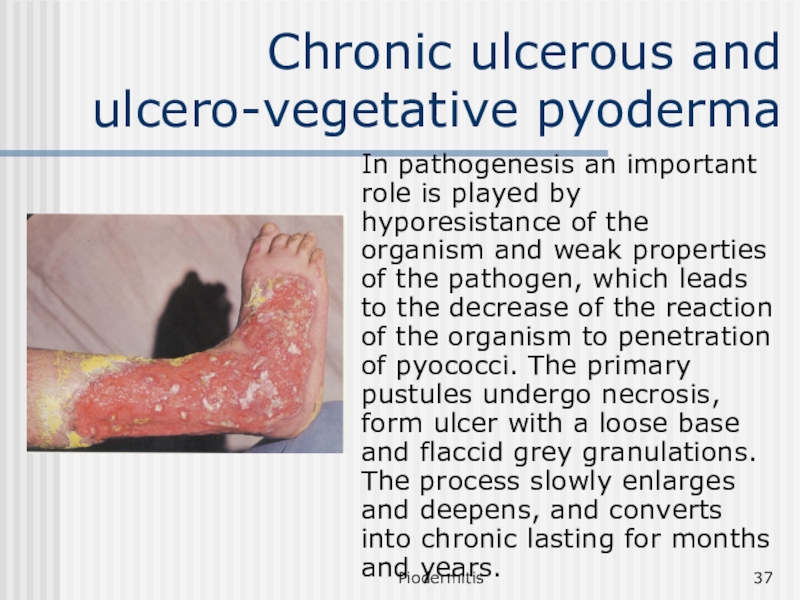
Chronic ulcerous and ulcero-vegetative pyoderma
In pathogenesis an important role
is played by hyporesistance of the organism and weak properties
of the pathogen, which leads to the decrease of the reaction of the organism to penetration of pyococci. The primary pustules undergo necrosis, form ulcer with a loose base and flaccid grey granulations. The process slowly enlarges and deepens, and converts into chronic lasting for months and years.
Слайд 38Piodermitis
Chronic ulcerous and ulcero-vegetative pyoderma
Differential diagnosis should be made from
warty, ulcerous and ulcero-vegetative tuberculosis, tertiary syphilis and deep mycosis.
During TB of the skin the inflammatory reaction is less dominant, skin tuberculin test is positive. During tertiary syphilis characteristic feature is the copper-red colour and dense consistency, absence of tendency towards fusion, positive immobilization reaction of T. palladium. Deep mycosis is differentiated through bacteriological and cultural diagnosis.
Слайд 39Piodermitis
Treatment
All of the superficial and acute pyodermas are to be
treated by aniline dyes. Deep and chronic pyodermas may be
treated by antibiotics and immune modulators such as:
Specific immune modulators (immunoglobulines etc.)
Non-specific immune modulators (Timus drugs, Vitamins, Splenin and others).
Слайд 40Piodermitis
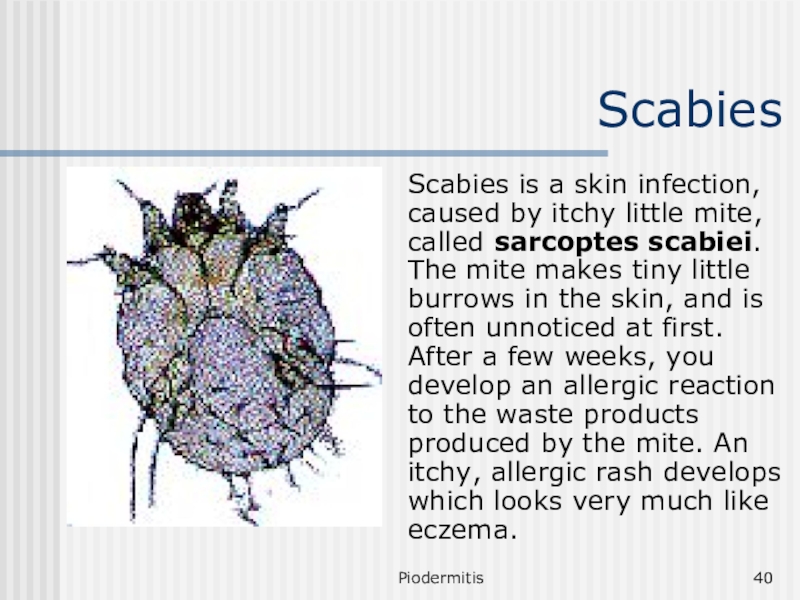
Scabies
Scabies is a skin infection, caused by itchy little mite,
called sarcoptes scabiei. The mite makes tiny little burrows in
the skin, and is often unnoticed at first. After a few weeks, you develop an allergic reaction to the waste products produced by the mite. An itchy, allergic rash develops which looks very much like eczema.
Слайд 41Piodermitis
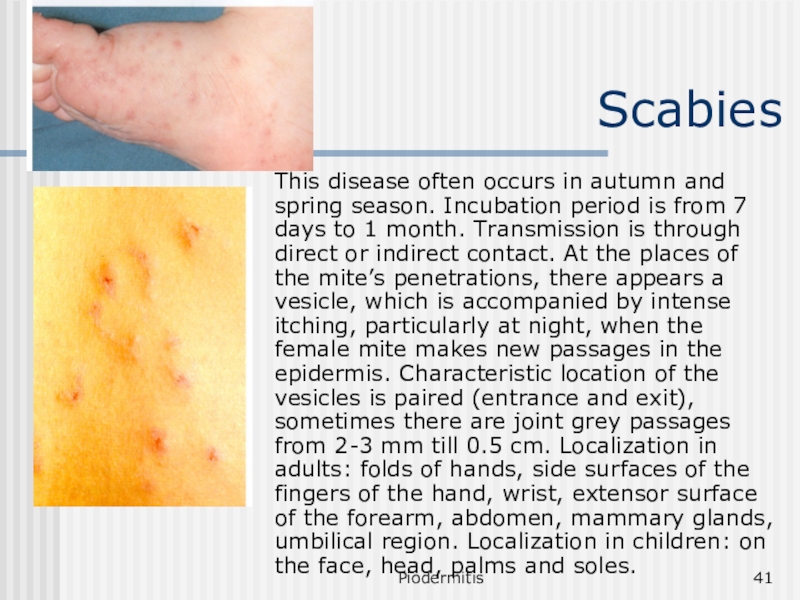
Scabies
This disease often occurs in autumn and spring season. Incubation
period is from 7 days to 1 month. Transmission is
through direct or indirect contact. At the places of the mite’s penetrations, there appears a vesicle, which is accompanied by intense itching, particularly at night, when the female mite makes new passages in the epidermis. Characteristic location of the vesicles is paired (entrance and exit), sometimes there are joint grey passages from 2-3 mm till 0.5 cm. Localization in adults: folds of hands, side surfaces of the fingers of the hand, wrist, extensor surface of the forearm, abdomen, mammary glands, umbilical region. Localization in children: on the face, head, palms and soles.
Слайд 42Piodermitis
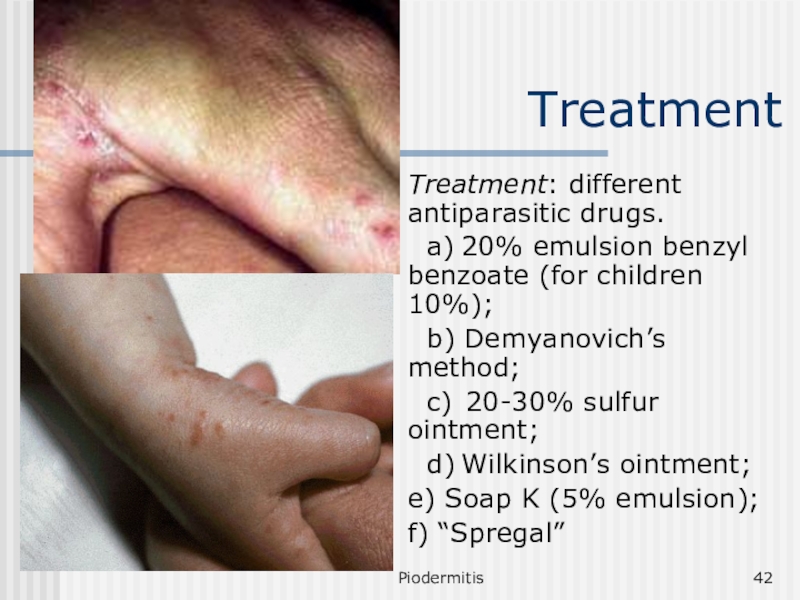
Treatment
Treatment: different antiparasitic drugs.
a) 20% emulsion benzyl benzoate (for
children 10%);
b) Demyanovich’s method;
c) 20-30% sulfur ointment;
d) Wilkinson’s
ointment;
e) Soap K (5% emulsion);
f) “Spregal”
Слайд 43Piodermitis
Prophylaxis
Before starting the treatment and after it: hot shower,
change of clothes.
Prophylaxis: simultaneous treatment of all the patients at
the place of infection, examination of families and children, where it was found. Thorough disinfecting of bedding.