Разделы презентаций
- Разное
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Геометрия
- Детские презентации
- Информатика
- История
- Литература
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Untitled-2
Содержание
- 1. Untitled-2
- 2. Слайд 2
- 3. Bronchiolitis is a disease of the small
- 4. PathomorphologyBronchioles derived from the tertiary bronchus and
- 5. symptomsCoughingDyspneacrackles and/or wheezingPFT - non-reversible obstructive defect,
- 6. chest radiography may be normalHRCT areas trapping
- 7. Acute bronchiolitisMostly in children of 1st yearMostly
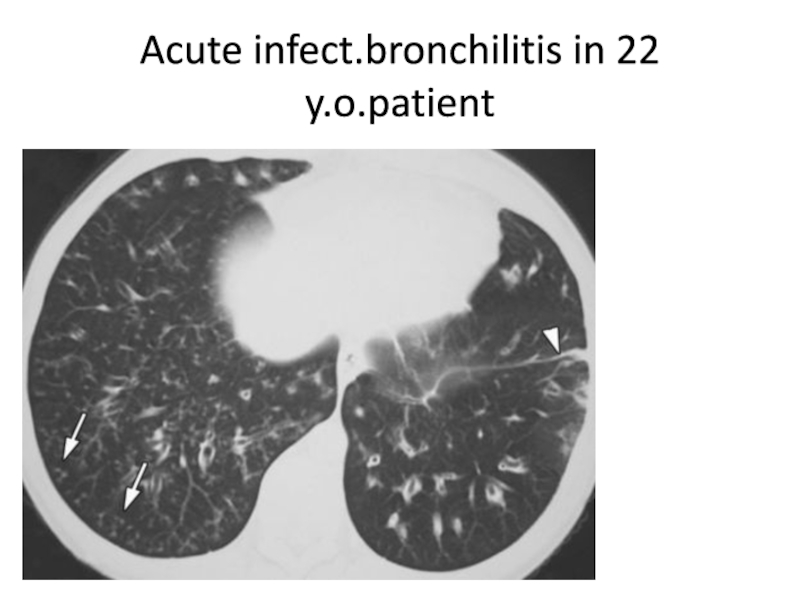
- 8. Acute infect.bronchilitis in 22 y.o.patient
- 9. Слайд 9
- 10. Proliferative bronchiolitis intra-luminal fibrotic buds, called Masson
- 11. Follicular bronchiolitis polyclonal hyperplasia of bronchiolar associated
- 12. In RA patient
- 13. Слайд 13
- 14. Respiratory bronchiolitis Frequent in young smokersusually asymptomaticclusters
- 15. Слайд 15
- 16. Airway-centered interstitial fibrosis particularly affects women
- 17. Слайд 17
- 18. Diffuse aspiration bronchiolitis poorly defined and occult
- 19. Слайд 19
- 20. Diffuse panbronchiolitis primarily affects Japanese, Korean, Chinese
- 21. Слайд 21
- 22. Obliterants bronchiolitis syndrome associated with small airways
- 23. Causes- nitrogen dioxide, nitrogen mustard, ammonia, welding
- 24. insidious onset of dyspnea and cough, especially
- 25. Слайд 25
- 26. Azithromycin has improved lung function in 50%
- 27. Скачать презентанцию
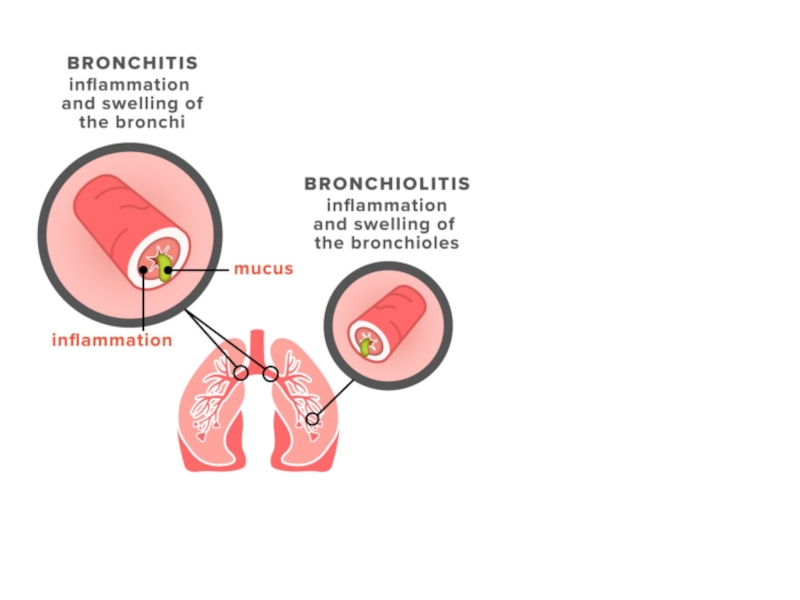
Bronchiolitis is a disease of the small airways, which are defined as airways with less than 2 mm in diameter and no cartilage
Слайды и текст этой презентации
Слайд 4Pathomorphology
Bronchioles derived from the tertiary bronchus and form a transition
area between the major airways and lung parenchyma and fundamentally
have a centrilobular location.Due to its structure (no cartilage and small diameter) they are vulnerable to infectious, inhaled, vascular, pharmacological and immunological injury
Слайд 5symptoms
Coughing
Dyspnea
crackles and/or wheezing
PFT - non-reversible obstructive defect, hyperinflation and generally
decreased diffusion (DLCO); reduced FEV1 (in less degree because it
predominantly identifies airflow obstruction in airways with diameter greater than 2 mm); may be mild restriction due to wide spread of affectionСлайд 6chest radiography may be normal
HRCT
areas trapping gas
thickening of
the bronchial wall
centrilobular nodules
air trap can be diffuse or mosaic
perfusion bronchial wall thickening occurs by cellular infiltration and / or fibrosis, and by the extension of both elements to peribronchial tissue.
Centrilobular nodules are consistent with the anatomical localization of the bronchioles; nodule size is variable.
pattern of “tree-in-bud”
Слайд 7Acute bronchiolitis
Mostly in children of 1st year
Mostly by RSV
In children
– severe life-threatening respiratory failure
In adults – not so
clear clinical presentation, mostly poorly defined; etiology may include Mycoplasma pneumoniae, RSV, measles, influenza, pertussis, parainfluenza, and adenovirusRVI symptoms may precede the bronchiolitis
Usually self-limiting
Слайд 10Proliferative bronchiolitis
intra-luminal fibrotic buds, called Masson bodies, extend beyond alveolar
ducts to alveoli.
When inflammation leads to extension of inflammatory
cells into the more distal pulmonary parenchyma, the process is called organizing pneumonia (in past COP was called BOOP – bronchiolitis obliterans organizing pneumonia)Frequent in COP, also in chronic eosinophilic pneumonia, hypersensitivity pneumonitis, idiopathic pulmonary fibrosis and nonspecific interstitial pneumonia.
may be due to exposure to nitrogen dioxide
HCRT - patchy airspace consolidation, “ground-glass” opacity and small nodular opacities in the periphery and in lower lung areas.
responds to glucocorticoids; the specific regimen depends on the clinical changes and the underlying cause
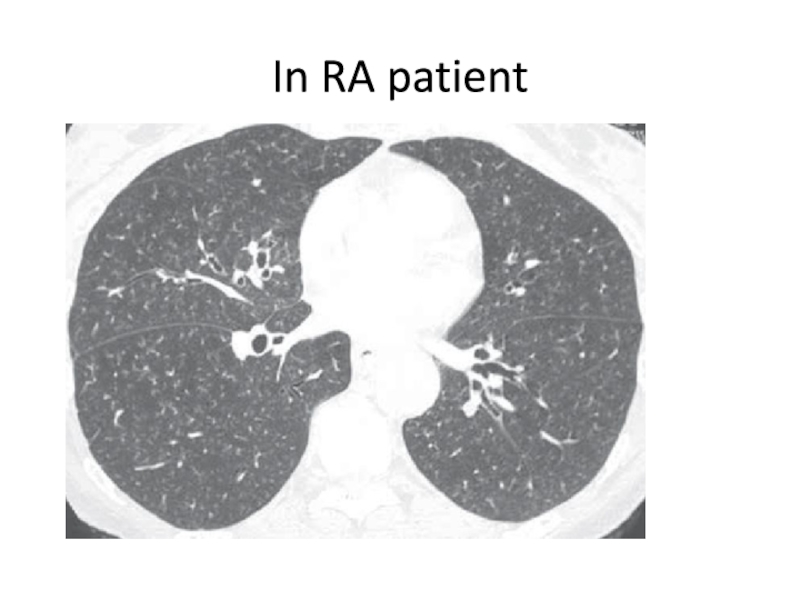
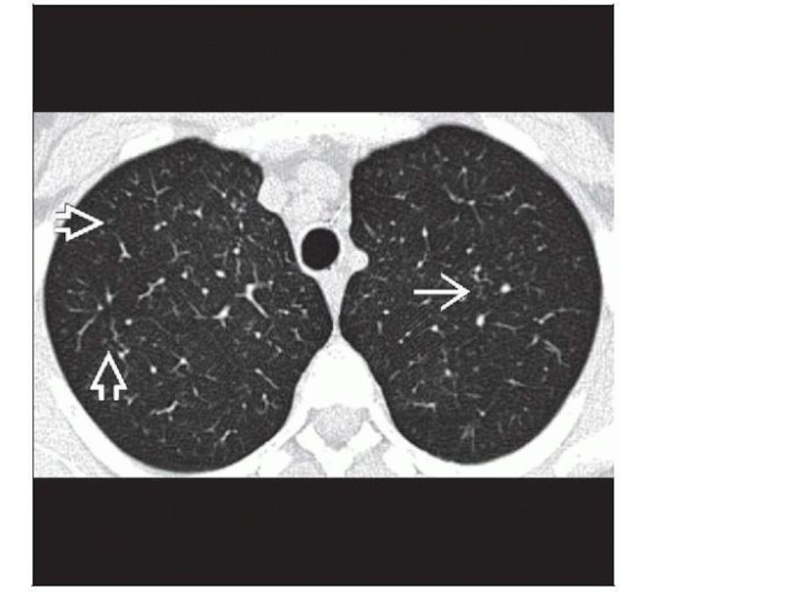
Слайд 11Follicular bronchiolitis
polyclonal hyperplasia of bronchiolar associated lymphoid tissue (BALT) produced
by antigen stimulation
Well-structured lymphoid follicles are located between the bronchioles
and pulmonary arteries and hyperplasia following compress the light of the bronchioles causing obstruction or complete obliterationis part of the "lymphoproliferative pulmonary diseases" (LPDs) and is associated with connective tissue diseases (rheumatoid arthritis, Sjögren's syndrome), interstitial lung diseases (ILDs), disorders of mixed collagen-vascular, obstructive diseases of airways and states immunodeficiency including HIV and common variable immunodeficiency (CVID) (secondary FB) , also in lymphoproliferative malignant parenchymal lesions (lymphoma MALT, diffuse large B-cell lymphoma)
CT:
small centrilobular nodules associated, sometimes to peribronchiolar nodules and “ground-glass” areas
"tree-in-bud" pattern, representing impaction with secondary bronchiolar exudate material infection or inflammation
peribronchiolar inflammation and formation of peribronchiolar lymphoid follicles may appear as a “tree-in-bud” on HRCT; which is described as "cotton-in-bud“
Treatment - underlying disease (IVIG, Rituximab, azathioprine), someties macrolides
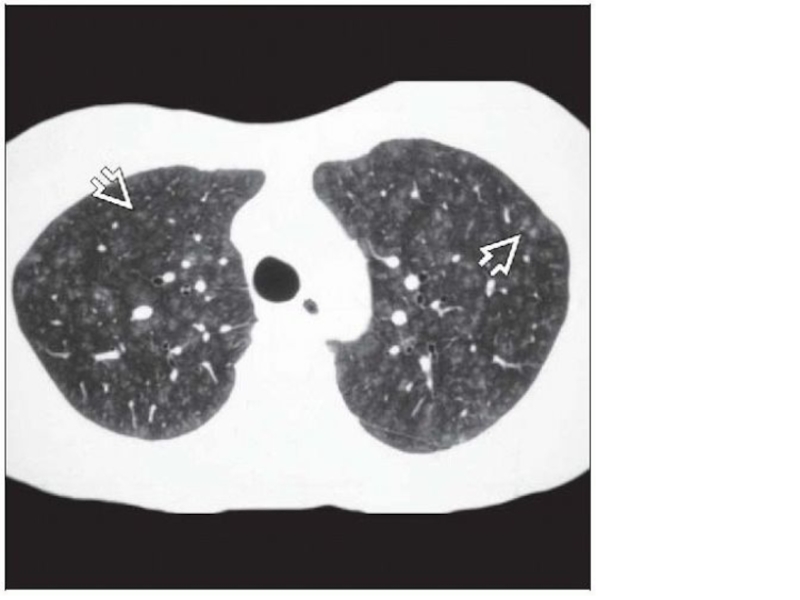
Слайд 14Respiratory bronchiolitis
Frequent in young smokers
usually asymptomatic
clusters of tan-pigmented macrophages in
the respiratory bronchioles; intraluminal macrophages are accompanied by a patchy
submucosal and peribronchiolar infiltrate of lymphocytes and histiocytes; peribronchiolar fibrosis extends in a stellate pattern into contiguous alveolar wallsinflammatory profile in normal smokers is very similar to that of patients with chronic obstructive pulmonary disease (COPD), but less prominent.
May lead to subtle functional alterations in young smokers and may precede the development of emphysema in genetically predisposed patients.
HRCT: diffuse or patchy “ground-glass” opacities, fine nodules, and air trapping, predominantly in the upper lobes.
Слайд 16Airway-centered interstitial fibrosis
particularly affects women between 40-60 years of
age
Same name as as idiopathic bronchiolocentric interstitial pneumonia or chronic
bronchiolitis with fibrosiscentrilobular and bronchiolocentric inflammatory infiltrate with peribronchiolar fibrosis and an absence of granulomas; prominent epithelial hyperplasia affecting alveolar septa; squamous metaplasia, goblet cell metaplasia and necrosis have been described
May be related to hypersensitivity pneumonitis
clinical picture: chronic nonproductive cough, progressing faster than HP, no specific interstitial pneumonia (NSIP) or RB-ILD, the other diagnoses have a similar presentation.
PFT - obstructive or restrictive patterns
HRCT - combination of “ground-glass” opacities, traction bronchiectasis, and bronchial wall thickening; latter is a result most advanced peribronchiolar fibrosis
Diff with HP - percentage of lymphocytes in the bronchoalveolar lavage (BAL) is less than 40%.
diagnosis is based on lung biopsy.
treatment is not known. Some patients improve with inhaled or systemic glucocorticoids, but the disease progresses generally in at least half of the patients reported, although ACIF has better prognosis than idiopathic pulmonary fibrosis
Слайд 18Diffuse aspiration bronchiolitis
poorly defined and occult entity
most often in young
or middle-aged patients with identifiable risk factors such as gastroesophageal
reflux disease (GERD), drug abuse and dysphagiacough, sputum production, dyspnea, and fever in patients with a history of recurrent pneumonia that did not respond to antimicrobial therapy were the most common manifestations
Chest CT findings are micro-nodules and opacities “tree-in-bud”.
management of these patients should focus on the prevention of recurrent aspiration and treatment of GERD.
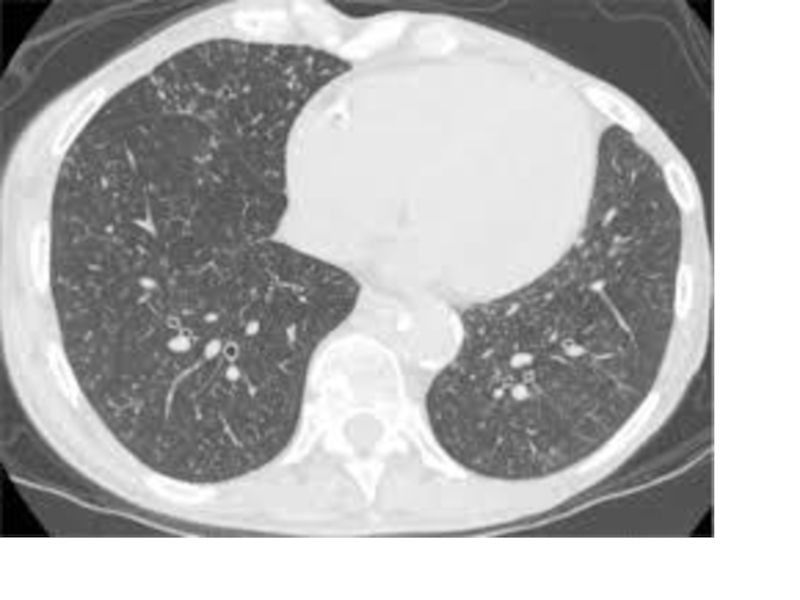
Слайд 20Diffuse panbronchiolitis
primarily affects Japanese, Korean, Chinese and Thai middle age
men and rarely reported outside South-East Asia
affects the lower and
upper respiratory tract, leading to progressive evolution bronchiectasis, recurrent infections and generally sinusitis Histological injury - respiratory bronchioles, transmural infiltrate of lymphocytes, plasma cells and distinctive lipid-laden “foamy” macrophages, with extension to peribronchiolar tissue. In advanced stages, there´s obstruction and constriction of lumen, proliferation of lymphoid follicles and secondary ectasia of terminal bronchioles. The functional pattern is essentially obstructive.
appears to be a genetic predisposition (HLA-B54 is associated with PBD in Japanese while HLA-A11 in Korean)
H. influenzae and Pseudomonas auroginosa may be present
CT - small nodular shadows to 2 mm in diameter, diffusely scattered in both lungs that can be invisible by hyperinflation of alveoli and the sign of “tree-in-bud”
treatment – erythromycin, roxithromycin and for extended time and at low doses, mainly for its immunomodulatory effect
survival rate at 10 years of PBD is about 90%
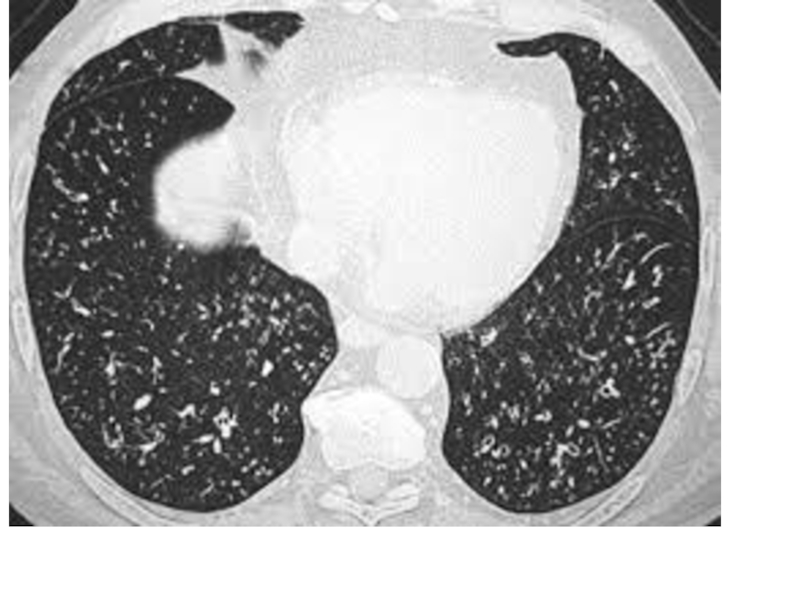
Слайд 22Obliterants bronchiolitis
syndrome associated with small airways damage caused by a
spectrum of exposure to drugs, inhalation, or infection and also
to transplantation of the lung and hematopoietic cells (HSCT)Injury to the bronchial epithelium seems to initiate the process that may involve the alveoli adjacent to the small pathways, excessive proliferation of granulation tissue that causes obstruction or obliteration of the bronchiolar lumen (constrictive bronchiolitis)
dyspnea, non-reversible airflow limitation with bronchodilators, and normal chest x-ray or pulmonary hyperinflation.
Слайд 23Causes
- nitrogen dioxide, nitrogen mustard, ammonia, welding vapors, ash, food
flavoring fumes (diacetyl and 2,3-pentanedione), SRV infection, adenovirus, orMycoplasma pneumoniae,
busulfan, gold or penicillamine treatment, and exposure to combustion air wells in the desert in soldiers, have been described as causesRheumatoid arthritis and other rheumatic diseases; inflammatory bowel disease.
graft vs host disease (GVHD) in patients undergoing lung transplantation or HSCT - 6% of allogeneic HSCT and in this group of patient’s survival is only 13% to 5 years; typically develops within the first 2 years of transplantation, although it can occur several years later.
calcineurin inhibitors (cyclosporin, tacrolimus and everolimus), inhibitors of purine synthesis (azathioprine or mycophenolate mofetil) and glucocorticoids
Слайд 24insidious onset of dyspnea and cough, especially when the symptoms
and signs do not follow a typical pattern of asthma
or COPDor if the patient has a predisposing exposure or condition; for example, symptoms of viral infection, exposure to toxic vapors, history of organ transplantation, or concomitant connective tissue disease.
PFT – initially normal or obstructive pattern with gas trapping and no reversibility with inhaled bronchodilators; then – restrictive and decrease of DLCO